0
Author of the article: Marina Dmitrievna
2017.10.30
40
Vessels
Vegetovascular dystonia (VSD) is a set of disorders of the autonomic nervous system caused by mental illness. VSD is an outdated term that is used extremely rarely. Panic disorder is considered to be the correct synonym for VSD.
Attention! Frequent symptoms of VSD are a feeling of suffocation, weakness, lack of air and hyperventilation. In some cases, studies have shown that an increase in CO2 levels in the blood can cause a panic attack.
CO2
Is the feeling of lack of air during VSD due to increased CO2 dangerous?
Chronic or spontaneous hyperventilation is associated with various physical illnesses and a number of mental disorders. Proponents of the panic disorder theory believe that hyperventilation either causes dangerous symptoms of hypocapnia or protects against attacks of suffocation. Although the evidence for both theories is inconclusive, observational, experimental, and therapeutic studies suggest an important role for high carbon dioxide (CO2) levels in the pathogenesis of VSD.
Likewise, hypocapnia and hypercapnia are associated with bronchoconstriction, worsening symptoms, and decreased quality of life in patients with asthma. Reducing CO2 levels has proven beneficial in both disorders.
Bronchial asthma
Abnormalities in breathing have been suggested to play a central role in the development and maintenance of VSD. The clinical literature is replete with observations of panicked patients presenting with various physical complaints for which there is no organic origin.
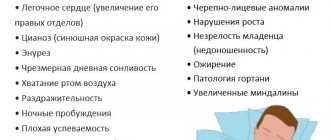
Some of the most common and alarming symptoms reported by panic patients include shortness of breath (the inability to breathe deeply), rapid heartbeat and weakness. Other symptoms include dizziness, pain or pressure in the chest, sore throat, waking up at night due to nightmares, excessive yawning, tingling in the extremities (knee, for example). Some patients shake (tremors), make awkward movements, or grab objects. A child may start crying during an attack of VSD.
Respiratory symptoms best characterize people with VSD. However, it has been suggested that respiratory parameters (PCO2, vital volume, respiratory rate) are more likely to correlate with anxiety compared to other physiological functions, including heart rate.
Anxiety
It has been suggested that the underlying origin of these respiratory symptoms in various patient groups is related to acid-base imbalance. In earlier studies, "hyperventilation syndrome" became a generic term for the constellation of complaints of these patients, and the diagnosis was reported to be present in at least 5-10% of outpatients.
The breathing pattern of these patients was described as disorganized, with lower than normal PCO2 levels, rapid breathing rates, rapid sighing, and predominantly thoracic rather than abdominal breathing. At the same time, patients often spoke of feelings of anxiety and depression.
These observations led to the formulation of two respiratory theories proposing a causal relationship between respiratory regulation, particularly that associated with PCO2, and panic: Lay's hyperventilation theory (1986) and Klein's suffocation false alarm theory (1993).
In the first of these, the main assumption is that panic attacks cause acute states of hypocapnia. In addition, hyperventilation may not be limited to the attack itself, but may precede and follow it, resulting in moderate, sustained hypocapnia. According to this hypothesis, the cause of seemingly spontaneous panic attacks is maintained through episodic periods of hyperventilation, which often occur outside the patient's awareness.
Hypocapnia also plays a significant role in Klein's hypothesis, but not as a leading cause of panic. Hyperventilation is seen as a compensatory or secondary response to an overly sensitive "choking alarm system" in these patients.
When a patient's PCO2 rises, the system begins to respond from an abnormally low threshold. This leads to disproportionate shortness of breath (a feeling of lack of air, suffocation), which, due to its terrible nature, initiates a cascade of panic symptoms. In this context, chronic hyperventilation is interpreted as an adaptation to a lower suffocation threshold.
VSD
Important! From a cognitive perspective, bodily sensations, including symptoms of hyperventilation, are thought to trigger panic attacks. It is the fearful interpretation of these sensations that arises, rather than the sensation itself that initiates the panic attack (for example, “shortness of breath means I have asthma and am dying”).
According to Clark (1986), relief of physical symptoms is not sufficient for treatment success unless it is accompanied by a reduction in catastrophic interpretations. Consequently, patients undergoing cognitive therapy training are told that hyperventilation, like a number of other sources of physiological symptoms, is harmless and does not pose a threat to human health.
Exercises
Perform the exercises twice a day ten times, in this case the body will get used to different types of breathing. You need to practice consistently, gradually complicating the complex.
- Rhythmic nasal breathing at a normal pace. Repeat through one nostril. To make it more difficult, inhale in three bursts and exhale through your mouth.
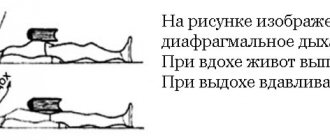
- Practice abdominal breathing - inhale through your nose with a stationary chest, sticking out your stomach, and when exhaling, hide your stomach inside. To control the correctness of the exercise, place one hand on your stomach, the other on your chest.
- Chest breathing - do not move your stomach, breathe through your nose, inhale to expand your chest as much as possible, and as you exhale, “deflate” it as much as possible. Place your hands on your waist, so you can feel the stillness of your stomach.
- Breathe fully through your nose. Inhale, expand your chest and stick out your belly. As you exhale, first release your stomach, then compress your chest. Use your hands to control your chest and stomach. This ventilation gymnastics becomes more complicated if you not only exercise control with your hands, but also apply slight resistance.
- If the attack of VSD is very strong, you can breathe for two minutes using a paper bag (breathe into a paper bag), which is pressed to the cheeks and nose.
- Exercise by doctor Kurpatov - with inhalation a person mobilizes his efforts, with exhalation he relaxes. Fear forms the third phase, between inhalation and exhalation, this stage must be shortened. Exercise - slowly inhale for five seconds, hold your breath for five seconds, exhale for five seconds. Then we inhale for five seconds, hold for four seconds, exhale for six. Gradually remove a second from the pause and add it to the exhalation. At the end of the exercise, the person inhales for five seconds and exhales for ten. In this way, you need to breathe for three minutes, both during training and during an attack, breathing will normalize.
Of course, proper breathing is good, but to treat VSD you also need a regimen, proper nutrition, hardening, and regular restorative exercises. The nutrition needed is the same as for hypertensive patients. And if properly tempered, the vessels will become stronger, their elasticity will improve, the blood arteries will be able to expand and contract in time - their main quality, which suffers from VSD. But still, in order to fill the body with a sufficient amount of oxygen, you need to have a good respiratory system, so that it starts working “like a young one,” you need to train your breathing. Breathing exercises will help, but you also need to use regular exercises to increase physical endurance, and you may need to change your lifestyle to a more active one.
Source: gimnastikasport.ru
Does increased CO2 cause suffocation during VSD?
As noted previously, accurate assessment of chronic hyperventilation conditions requires assessment of acid-base status by analyzing blood samples. Very few studies have made this assessment in VSD, and the results have been mixed.
Evidence of chronic hyperventilation using acid-base balance measurements was found in the studies of Gorman and Papp, but not Zandbergen. Studies assessing the end-point effects of PCO2 are more numerous and show differences in baseline levels between patients suffering from VSD compared to patients without panic.
In Papp's study, respiratory psychophysiology was examined in patients with panic disorder. The authors also examined baseline respiratory characteristics between the two groups. They found that baseline final PCO2 levels were significantly lower in sick patients.
Other respiratory parameters (respiratory rate, vital volume and minute ventilation) also showed elevated PCO2 levels in patients.
Basic Breathing Principles
It is better, of course, not to pay attention to breathing and live a full life. But if there are malfunctions in the human respiratory system, and even against the background of VSD, then you need to learn the basic principles of proper inhalation of air:
- not only the chest breathes, but also the diaphragm, as well as the muscles of the anterior abdominal wall; when a person inhales air, first the lungs expand, then the chest increases, and then the abdominal wall moves forward; accordingly, exhalation occurs in the reverse order;
- If possible, you need to breathe only through your nose - this way the air is moistened, purified and warmed; only in case of heavy physical exertion is mouth breathing possible;
- you need to breathe according to the movement - the body instinctively exhales when squatting, when the arms go down, inhalation is done when straightening the torso, weights are lifted as you inhale.
If, in case of breathing problems that affect the well-being of VSD, you correctly synchronize breathing and the physical state of the body, then you can achieve relief by strengthening the body and coherence of vital processes. Simply put, exercise will prepare you for an improved quality of life.
Breathing tests in patients who have difficulty breathing with VSD
Respiratory theories, as described above, suggest a direct link between changes in PCO2 and a panic attack. This has led researchers to use various experimental tests to study the effects of artificially induced hypo- or hypercapnia.
Induction of hypocapnia is achieved through voluntary hyperventilation (VH). Despite its widespread use in panic disorder research, there is little consensus regarding the standards of the DH test.
Patients are asked to breathe faster than normal over a period of time, but beyond this general function, studies vary widely in procedural parameters and outcome measures. It is often unclear whether PCO2 is actually reduced to moderate to severe hypocapnia levels (30 to 20 mmHg) because capnographic assessment is not performed.
Hypocapnia
Some studies have used solely respiratory rate measurements or even simple observational respiration counts, but this does not guarantee that a patient will develop hypocapnia.
Exogenous CO2 can serve as an anxiogenic substance and its effect has been extensively studied in patients with panic disorder. Here, the experimental procedure involves inhalation of an increased concentration of CO2 (usually in the range of 5-65%). Depending on the inhalation concentration, the test can induce choking and mild to severe states of anxiety or panic, the latter often resembling natural panic attacks.
The normal response to inhalation of elevated CO2 levels also includes significant increases in minute ventilation, respiratory rate, and vital volume. Studies are equivocal regarding the ventilatory response in patients with panic, with some demonstrating a greater increase in minute ventilation.
In addition to minor ventilation, studies have shown differences between panic patients and healthy controls in aspects of airway adaptation to the CO2 challenge, such as a greater increase in respiratory rate.
Some studies have also documented a reduced respiratory response in patients with panic. A number of factors may explain this pattern of evidence and discrepancies between observations. The response of healthy patients to CO2 has been shown to be more variable, with a minority also responding with panic symptoms and greater ventilatory changes.
The strong reaction of panic patients to increased CO2 appears to have a hereditary cause. Relatives of panic patients also expressed symptoms of anxiety when inhaling CO2.
A hypersensitive response to hypercapnia has been documented in patients with panic disorder, but the nature of the specific respiratory abnormalities in panic disorder remains controversial. Several reports have questioned the causal role of hypercapnia in detecting panic or distinguishing panic patients from other anxious patients. A common criticism of these studies is that the reported CO2 concentrations are higher than natural values. Data on chemoreflex hypersensitivity in VSD also remained ambiguous.
It has been suggested that cognitive errors, rather than biological responses, are the main reason why patients panic during these procedures. For example, patients were given single inhalations of 50% CO2 without any explanation or detailed information about the psychophysiological symptoms associated with the inhalation. Since the patients did not respond to the increase in CO2, scientists began to believe that the cause of panic was cognitive errors rather than organic disorders.
Sanderson gave patients a dial that showed the wrong amount of CO2 in the patients' blood. Patients in this condition were less likely to panic than those who were not given the illusion of control. However, other studies have failed to replicate the finding that panic tendencies depend on patients' cognitive errors.
Welkowitz developed a stronger test of the putative control hypothesis by presenting patients with a dial with high (incorrect) blood CO2 readings. The patients began to have a panic attack each time, and their condition worsened significantly. Welkowitz proved the cognitive nature of VSD.
Panic
Abelson found that cognitive psychotherapy reduced the intensity of panic attacks in response to doxapram administration and significantly reduced the respiratory response. However, minor changes in respiration and increases in PCO2 were noted.
Basics of breathing exercises
- You need to breathe deeply. When breathing, it is important to engage the chest and anterior abdominal muscles. The inhalation process should begin with the expansion of the chest as oxygen enters, then the abdominal muscles expand. And the exhalation cycle occurs in the opposite direction with retraction of the abdomen and compression of the chest.
- Breathe through your nose. It does not matter whether it is inhalation or exhalation, the air must pass through the nose, thus it is moistened, warmed and cleared of dust. In this case, breathing should be smooth, without jerks, without tension. It is allowed to exhale through the mouth during serious cardio exercises and running.
- Adaptation of breathing. If a person is in motion, then the process of inhalation and exhalation must be adapted to the nature of the actions. It is better to accompany the inhalation by straightening the chest, spreading the arms to the sides, or raising them up, and the exhalation by bending, bringing the arms together, squatting, which compress the chest. This helps the body not get so tired and realize more. Learn to synchronize your movements with your breathing and you will feel much better.
Correct breathing exercises will help you feel much better, alleviate your physical condition, strengthen the immune system, and improve the body’s vital processes.
Breathing exercises for vegetative-vascular dystonia are an excellent remedy that does not require much time for treatment, does not put a strain on the family budget and gives rise to a healthy quality of life.
It’s hard to breathe with VSD: what to do?
As mentioned above, choking occurs due to cognitive errors rather than physical causes. There is a whole list of methods that will help relieve the VSD crisis:
- Muscle relaxation according to Jacobson;
- Autotraining according to Schultz;
- Slow walking;
- Artificial coughing or yawning (stimulate the vagus nerve);
- “Thought stopping” technique;
- Yoga and meditation.
In many ways, the semiotics of suffocation during VSD depends on the patient’s perception of his illness. During attacks of “choking,” it is not recommended to use medications (tablets, drops) or traditional methods (infusions, herbs). If you constantly swallow pills, addiction will form. This reinforces the patient's belief that he has a physical illness and is capable of suffocating from VSD.
Meditation
The reason for suffocation lies in constant fear. There were no deaths associated with a panic attack. Contrary to popular belief, coma is not caused by attacks of VSD.
Advice! The feeling of “deficiency” of oxygen, tachycardia, and “false” dyspnea are not life-threatening for the patient. Calming down and distracting yourself from the attack is the most effective way to get rid of symptoms. In case of serious overload at work, it is recommended to take a vacation and go to a sanatorium or provide peace for a long time.
Exercises
The main task of breathing exercises is to focus on exhalation. You need to accustom yourself to exhale as much air as possible and clear your lungs so that clean air can enter when you inhale. Having learned this rule, it will be easier for you to perform physical therapy and your well-being will noticeably improve.
Static classes
Exercises for VSD are performed in a sitting or horizontal position; it should not be confused with exercise therapy. Poses in which it will be convenient and correct to do gymnastics:
- lying on your back;
- sitting on a chair;
- sitting on the floor in the “lotus” position or simply with crossed legs;
- sitting on the floor with your heels tucked under you. If it is uncomfortable, you can place something soft under your heels, such as a pillow.
All exercises for VSD are quite simple, they are easy to perform, and they are accessible to everyone. You need to exercise regularly, gradually increasing the load and complicating the process. After two weeks, the body will get used to it and this will become a daily ritual on the way to a healthy body and spirit.
Exercise 1
Rhythmic breathing. This exercise is performed through the nose: at a normal pace, you need to rhythmically inhale and exhale air. You can gradually complicate the task, for example, inhale air in jerks for three counts and exhale through your mouth. You can also do gymnastics with one nostril, alternating them one by one.
Exercise 2
Chest breathing: hands are placed on the waist and control the immobility of the abdomen. The air is inhaled through the nose, expanding the chest as much as possible, and the air is exhaled in as large a volume as possible.
Exercise 3
Abdominal breathing. For this exercise, the chest remains motionless, inhalation and exhalation occurs with the help of the abdomen: when inhaling, it contracts inward, and when exhaling, it protrudes. To control both the chest and abdomen, you need to place both hands on them.
Exercise 4
Nasal breathing. The chest and abdomen are involved in the breathing process. You can complicate the process and press on the involved parts of the body with your hands in order to increase resistance. As you inhale, the chest expands and the stomach protrudes, and as you exhale, the stomach hides and the chest drops. This kind of gymnastics is also called ventilation and cleanses the lungs well.
Exercise 5
Breathing into a paper bag. This exercise is suitable for those who experience severe attacks of vegetative-vascular dystonia. The paper bag must be pressed tightly to the nose and cheeks and breathing rhythmically into it for two minutes or until the attack stops.
Exercise 6
Breathing according to Kurpatov. The exercise begins with three phases: inhalation, breath-holding and exhalation, each of which is 5 seconds. Gradually, we remove every second from the pause in favor of exhalation, i.e. inhale – 5, pause – 4, exhale – 6 seconds. By the end of the exercise, the breath hold should be reduced to zero, the inhalation will remain for 5 seconds, and the exhalation will last up to 10. During the exercise, breathing normalizes and the attack passes.
Breathing exercises are a very accessible and effective relief for the symptoms of VSD, but in addition to it, proper nutrition, adherence to a regimen, hardening and exercise therapy are necessary.
Respiratory complex Strelnikova
The author of this gymnastics is the famous teacher and singer Alexandra Nikolaevna Strelnikova. This complex helps restore voice and breathing, and also generally heals the body. It is used by professional opera singers and actors to treat speech disorders such as stuttering. The enormous importance of Strelnikova’s respiratory system was repeatedly noted in the Soviet years by such famous personalities as: Boris Telvin (conservatory professor), Vladimir Etush, Margarita Terikhova, Armen Dzhigarkhanyan.
The Strelnikova complex will also be useful for vegetative-vascular dystonia. Exercises normalize previously disturbed breathing through the nose, provide pulmonary drainage, improve autonomic reactions, strengthen the heart and blood vessels, increase the overall tone of the body and immunity.
Strelnikova’s complex includes many different exercises, here are just a few of them:
- “ Pump ”: stand straight with your arms down and your feet shoulder-width apart, relaxing the muscles of your arms and shoulder girdle. Bend slightly forward, lowering your head, arms and shoulders. When bending over, take a quick breath, and when bending back, exhale. After every 8 breaths, pause for 5 seconds.
- “ Cat ”: squats are performed with simultaneous turns from the position: arms pressed at the seams, legs wider than shoulders. Do a squat with a torso turn, while raising your arms to your waist, and inhale quickly. Then, exhaling, shake the hands and turn in the other direction. After every 8 turns, pause for 8 seconds.
- “ Big pendulum ”: a slight inclination is made towards the floor, which is accompanied by inhalation. Then you need to straighten up and lean back a little, put your arms around your shoulders and bend at the lower back. After this, a calm, long exhalation is done.
You can read more about this complex in the book by I.N. Kochetkova “Strelnikova’s paradoxical gymnastics”:
As can be seen from the above exercises, Strelnikova’s gymnastics contains some paradoxical movements: inhalation is performed in a position where the chest area, diaphragm and lungs are maximally compressed, and exhalation is performed when they are straightened. Due to this, a therapeutic effect is achieved. This gymnastics was invented by Strelnikova to help herself in a difficult situation: one day she felt ill when she was alone at home and there was no one to call her an ambulance. To alleviate her condition, she intuitively began to make body movements that helped her.
Physiotherapy
What is exercise therapy for vegetative-vascular dystonia? This is, first of all, regular morning exercises and light physical activity. They could be simple exercises that you did at school or college, that you know or have done before.
It is very important during exercise therapy to follow the correct breathing technique: rhythmic, coordinated with actions, direct breathing with a wide chest as you inhale and straightening as you exhale.
In addition to physical exercise, you can do jogging, swimming, cycling, skiing in winter or kayaking in summer. Don’t set the bar too high right away, because classes should bring not only benefits, but also positive emotions. Jumping, sudden movements (boxing, karate, wrestling) and weightlifting should be avoided.
Amosov technique
Floor exercises by Nikolai Amosov are very effective for normalizing blood pressure and strengthening the vegetative-vascular system.
The main requirements of this exercise therapy are endurance and strength. Each exercise is performed with 10 repetitions and gradually increased to 100. This complex is recommended to be combined with jogging, jogging and be sure to focus on the last 100 km.
The entire complex is performed at the most accelerated pace; Amosov took only half an hour for 1000 movements, and its main components were outdoor exercise in any weather.
According to Amosov, no heart disease, even chronic, is an obstacle to gymnastics. However, classes require regularity and maximum effort.
Its complex for VSD strengthens blood vessels, makes them more elastic, and helps blood arteries quickly change their state from compression to expansion. But in order to train the body with the help of physical therapy, you need to develop your respiratory system well and constantly work on proper breathing techniques.
Develop physical endurance, willpower, fortitude and respiratory system so as not to suffer from the unpleasant symptoms of dystonia.
Source: NashiNervy.ru