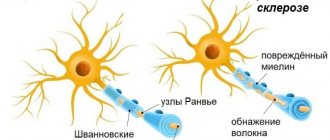
Demyelinating diseases are diseases of the nervous system in which the myelin sheath of neurons is damaged. This damage impairs the conduction of signals in the affected nerves. In turn, a decrease in conductivity ability causes a decrease in sensitivity, motor activity, perception, etc. - depending on the level and location of the lesion.
Some demyelinating diseases are genetic, some are caused by infectious agents, autoimmune reactions, or completely unknown factors. Special mention should be made about chemical agents - industrial, household and even medicinal. Organic phosphites, a class of chemicals that are the active ingredients in commercial insecticides, herbicides, pet flea medications, etc., are also known to demyelinate nerves. Even some psychotropic drugs, such as antipsychotics, can also lead to demyelination.
Demyelinating diseases are traditionally classified into two types: myelinopathies and myelinoclastics. In the first group, normal and healthy myelin is destroyed by toxic, chemical or autoimmune substances. The second group includes diseases that are based on abnormal structure and degeneration of myelin. The diseases of the second group were called dysmyelin diseases according to the “poseur criteria” (diagnostic criteria for multiple sclerosis).
In the case of a well-known example, multiple sclerosis, there is good evidence that the body's own immune system is at least partially responsible and involved in the pathological process. Representatives of the acquired immune system, the so-called T cells, are known to be present at the site of injury. Other immune system cells called macrophages (and possibly mast cells too) also contribute to the damage.
It is also known that vitamin B12 deficiency can lead to demyelination.
Evolutionary theories of pathogenesis
The role of prolonged cortical myelination in human evolution has been recognized as a contributing factor to several demyelinating diseases. Unlike other primates, humans have a unique pattern of postpubertal myelination that may contribute to the development of psychiatric disorders and neurodegenerative diseases present in early adulthood and beyond. The long period of myelination of the human cerebral cortex may provide a greater opportunity for myelination failures, resulting in the onset of demyelinating diseases. In addition, it has been noted that humans have a significantly larger volume of prefrontal white matter than other primate species and have a greater myelin density. Increased myelin density in humans as a result of prolonged myelination may cause a structural risk for myelin degeneration and dysfunction. Evolutionary considerations about the role of long-term cortical myelination as a risk factor for demyelinating diseases are particularly important given that hypotheses that emphasize genetics and autoimmune deficiency fail to explain many cases of demyelinating diseases. As already noted, diseases such as multiple sclerosis cannot be caused solely by autoimmune deficiency, but are highly sensitive to developmental defects in the pathogenesis of the disease. Thus, the role of the human-specific long period of cortical myelination is an important evolutionary factor in the pathogenesis of demyelinating diseases.
Demyelinating diseases of the nervous system
Diseases of the nervous system (ICD-10 according to the international classification), which are united by a similar method of damage to myelin, are caused by several causes - from allergic to viral agents. This group of pathologies is characterized by the fact that demyelinating diseases of the central nervous system often affect able-bodied men and women, who subsequently become disabled. As a rule, demyelination of the brain leads to a persistent decrease in intelligence. The most common demyelinating diseases of the brain are:
- multiple sclerosis;
- multifocal leukoencephalopathy;
- acute encephalomyelitis.
Multiple sclerosis
Recently, young people from 15 to 40 years old have often learned what multiple sclerosis is. A feature of this disease is the simultaneous damage to several parts of the central nervous system, which leads to different symptoms in patients. The disease alternates between periods of remission and exacerbation. The basis of multiple sclerosis is the occurrence of foci of myelin destruction in the spinal cord and brain, which are called plaques. Their sizes are small, but sometimes large compounds are formed. Often this pathology leads to Marburg disease or atherosclerosis.
Progressive multifocal leukoencephalopathy
The disease refers to a viral infection of the nervous system, which develops when the patient is in an immunodeficient state. The pathology progresses rapidly and can lead to death within a year. Often the cause of multifocal leukoencephalopathy is a reactivated virus, which enters the body in childhood and is in the kidneys or tissues in a latent state. A disease develops when a person falls into a risk zone: AIDS, organ transplantation, lymphoma, leukemia, Wiskott-Aldrich syndrome and other diseases.
- 7 Best Garden Tractors
- Searching for ads by phone number - step-by-step instructions for checking the seller
- What medications are prescribed for menopause?
Acute encephalomyelitis
Disseminated encephalomyelitis is a disease in which a variety of inflammatory processes occur in the spinal cord and brain. The pathology is characterized by lesions scattered throughout the nervous tissue. The name itself (encephalitis and myelitis) indicates the severity of the disease, and the patient’s prognosis for recovery depends on the activity of the process, the adequacy and timeliness of treatment, and the initial state of the body. The outcome of acute encephalomyelitis can be either recovery, disability or even death of the patient.
Signs and symptoms
The symptoms and signs that are present in demyelinating diseases are different for each condition. But the main ones are the following:
- blurred and double vision
- neurological "focal" symptoms
- ataxia
- clonus
- dysarthria
- fatigue, weakness
- clumsiness of movements
- incoordination (impaired coordination of movements)
- mono paresis or monoplegia of the upper limbs
- hemiparesis
- spastic para paresis
- genital anesthesia
- paresthesia
- incoordination (impaired coordination of movements)
- mono paresis or monoplegia of the upper limbs
- hemiparesis
- spastic para paresis
- genital anesthesia
- paresthesia
- gaze paralysis
- visual impairment
- loss of sensation
- urinary incontinence
- hearing problems
- speech problems
Binswanger's disease on MRI
Binswanger's disease. This is a subcortical encephalopathy, sometimes called high blood pressure dementia. With this pathology, small vessels rupture due to constant increased pressure, and diapedetic hemorrhage leads to lacunae in the brain. On an MRI of the brain, the white matter of a person with Binswanger syndrome will look like cheese with multiple perforated lesions. With this demyelinating process, a person’s cognitive functions are impaired, memory suffers, changes in movement occur - a so-called “magnetic gait” occurs. The patient's feet are always stuck to the floor. Because the subcortical area of the brain is affected, he cannot lift his leg and move freely. Such people also suffer from an overactive bladder and often have to live with urinary incontinence.
Diagnosis
Various diagnostic techniques and approaches are used to diagnose demyelinating diseases.
- Exclusion of other diseases with similar symptoms (Differential diagnosis)
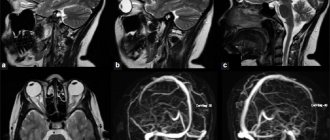
- Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to visualize the internal structures of the body in detail. MRI uses the properties of nuclear magnetic resonance (NMR) to image the nuclei of atoms inside the body. This method is reliable because MRI evaluates changes in proton density. Image changes may result from changes in the water-containing structures of the brain.
- An evoked potential is the electrical potential recorded from the nervous system after the presentation of a stimulus, as detected by electroencephalography (EEG), electromyography (EMG), or other electrophysiological recording methods.
- Cerebrospinal fluid (CSF) analysis can be extremely useful in diagnosing central nervous system infections. Culture and microscopic examination of the CMR can reveal the microorganism that caused the infection.
- Proton magnetic resonance spectroscopy (MRS) is a non-invasive analysis method that has been introduced to study metabolic changes in brain tumors, strokes, epilepsy, Alzheimer's disease, depression and other brain diseases, as well as to study the metabolism of other organs such as .muscles.
- Diagnostic criteria take into account certain combinations of signs, symptoms, and test results that a physician uses in an attempt to determine the correct diagnosis.
Diagnostics
The first sign that may be detected during the initial examination is a violation of the speech apparatus, impaired coordination of movements and sensitivity.
Magnetic resonance imaging (MRI) is used for definitive diagnosis. Only on the basis of this study can the doctor make a final diagnosis. MRI is the most accurate method for diagnosing many diseases.
The most accurate diagnostic method is MRI with the introduction of a contrast agent.
It is with the help of such a study that it is possible to identify both a single focus of demyelination and multiple lesions of the brain and nerve tissue.
An example of foci of demyelination in multiple sclerosis
If foci are detected during the first pass of magnetic resonance imaging, and on a subsequent pass it is noted that one of the foci has disappeared, then this is characteristic of multiple sclerosis.
On the MRI screen, lesions are displayed as white spots, from which it is impossible to determine the inflammatory process, demyelination, remyelination, or what other process is occurring in the tissues.
If the lesion disappears upon repeated examination, this indicates that deep tissue damage has not occurred, which is a good sign.
The demyelinating process of the brain requires a careful diagnosis:
- MRI - magnetic tomography shows hypersignal lesions in the white matter of the brain and spinal cord on T2 images and hyposignal lesions on T1 (the number correlates with the severity of the disease);
- examination of cerebrospinal fluid - intrathecal synthesis of IgG, the presence of at least 2 oligoclonal bands in the alkaline part of the spectrum not present in serum, pleocytosis of mononuclear cells (up to 100/3), prevalence of lymphocytes;
- study of evoked potentials (visual and somatosensory) – increase in wave latency;
- ophthalmological examination (in the case of retrobulbar neuritis) - in the acute stage there is swelling of the papilla, later - its temporary fading (manifestation of atrophy);
- histology - indicates the presence of inflammatory changes in the head, dystrophic processes, neuronal degeneration (gliosis).
Treatment
Treatment usually involves improving the patient's quality of life. This is achieved by treating symptoms or slowing the rate of demyelination. Treatment may include medications, lifestyle changes (eg, stopping smoking, adjusting daily routine to increase rest periods, changing diet), relaxation, exercise, patient education, and, in some cases, thalamic deep stimulation (for intractable tremor). . Also, depending on the phase and course of the disease, treatment is used that affects the innate immunity.
Treatment is specific to the patient and depends on the symptoms that are present with the disorder, as well as the phase of the disease.
Forecast
The prognosis depends on the disease itself. So, with multiple sclerosis, the prognosis depends on the subtype of the disease and the characteristics of the patient: age, gender, initial symptoms and degree of disability. Life expectancy in patients with multiple sclerosis (according to the Lancet.) is 5-10 years less than in healthy people. Multiple sclerosis is an inflammatory demyelinating disease of the central nervous system (CNS) that develops in genetically predisposed individuals after exposure to unknown environmental factors. The reasons are still not known exactly, but there is a scientifically based suspicion of the involvement of immune reactions directed against self-antigens, in particular myelin.
Demyelination of the brain and central nervous system is often a matter of life and death
Author Alexandra Balan-Senchuk
04.11.2019 09:01
Health
Demyelination of the brain and central nervous system is a pathology characterized by damage to the sheath of nerve fibers and disruption of their conductivity.
0 shared
Any disorder that results in the destruction of the myelin covering is called a demyelinating disease. Damage to the myelin sheath destabilizes nerve signal conduction, leading to neurological symptoms such as decreased sensation, cognition, and movement that rely on nerve “signaling.”
The mechanisms underlying demyelination are not well understood by medical professionals, but factors that may be involved include:
- Genetic predisposition.
- Certain infections.
- Some autoimmune disorders.
- Exposure to toxic chemicals.
Demyelinating diseases
Several conditions lead to demyelination, and one of the most well-known neurodegenerative diseases is multiple sclerosis. Here, the immune system targets the myelin sheath or the cells that form and support it. This disease occurs twice as often among women than among men. Residents of central Russia and Siberia suffer the most from the disease.
The course of the disease in multiple sclerosis is usually relapsing, but it can also progress from the onset of the disease or become progressive after periods of remission. The latent phase between the initial onset of a symptom and the first relapse is variable.
- Transverse myelitis, in which there is inflammation of the spinal cord.
- Optic neuritis, which refers to inflammation of the optic nerve.
- Acute disseminated encephalomyelitis, in which there is inflammation of the spinal cord and brain
- Adrenomyeloneuropathy, or adrenoleukodystrophy, which are rare types of metabolic disorders.
Symptoms of demyelinating diseases
Demyelinating disease usually results in muscle weakness and stiffness, loss of vision, sensation and coordination, pain and bowel and bladder dysfunction. A more complete list of symptoms and signs consistent with demyelinating diseases:
Motor symptoms: gait disturbance, limb weakness, spasticity, imbalance, hyperreflexia.
Visual: diplopia (double vision), blurred vision, loss of vision and fluctuations in objects in the field of view.
Sensory: parasthesia (tingling sensation), dysesthesia (abnormal sense of touch), numbness, pain in the trunk, trigeminal neuralgia (severe facial pain), hyperpathia (increased sensitivity and pain threshold), allodynia (pain from non-painful stimuli) and abnormal movement due to abnormal perception.
Genitourinary: constipation, impotence, urinary incontinence, frequent urination, anorgasmia and dyspareunia (pain during sex).
Nervous: anxiety, depression, irritability, impaired attention, concentration and memory impairment.
Treatment of demyelinating diseases
Demyelination of the brain is often a matter of life and death. There is no cure for demyelinating diseases or to prevent their progression, but early intervention can help minimize the impact of attacks, manage symptoms and modify the course of the disease.
Depending on the specific disorder, a number of treatments are available, which may include drugs that reduce the incidence of new lesions. Approaches to treating symptoms include muscle relaxants, physical therapy, and medications to relieve fatigue and pain.
Photo: labroots.com
Discuss
Topics central nervous system brain sclerosis bladder multiple sclerosis
Epidemiology
The incidence of demyelinating diseases varies depending on the disorder. Some conditions, such as spinal tuberculosis (tertiary syphilis affecting the nervous system, neurosyphilis) appear predominantly in men, and begin in midlife. Optic neuritis, on the other hand, occurs predominantly in women, usually between 30 and 35 years of age. Other conditions such as multiple sclerosis vary in prevalence depending on country and population, and can affect both children and adults.
Types
Demyelinating diseases can be divided into those that affect the central nervous system and the peripheral nervous system, presenting different variants of demyelination. They can also be divided according to other criteria into inflammatory and non-inflammatory (by the presence or absence of inflammation), and finally, the division can also be made depending on the main cause of demyelination into myelinopathies and myelinoclastics (damage to myelin by substances from outside and myelin degenerations without external reasons)
Demyelinating diseases of the central nervous system
Demyelinating diseases of the central nervous system include:
- Myelinoclastic diseases, in which the myelin is attacked by external substances (standard multiple sclerosis, neuromyelitis optica (Devic's disease) and other disorders involving the immune system, are called inflammatory demyelinating diseases.
- Leukodystrophies (myelinopathies) are diseases in which “wrong” myelin is produced: CNS- Neuropathies are caused by vitamin B12 deficiency
Demyelinating diseases of the peripheral nervous system
- Guillain-Barre syndrome
- Anti-MAG peripheral neuropathy
- Charcot-Marie-Tooth disease
- Copper deficiency and related conditions that cause: peripheral neuropathy, myelopathy, and rarely neuroopticopathy.
- Progressive inflammatory neuropathies
Article 22. Inflammatory, demyelinating diseases of the central nervous system and their consequences
| Disease schedule article | Name of diseases, degree of dysfunction | Category of suitability for military service |
| Article 22. | Inflammatory, demyelinating diseases of the central nervous system and their consequences: | |
| a) with significant impairment of functions | "D" | |
| b) with moderate dysfunction; | "IN" | |
| c) with minor dysfunction; | "IN" | |
| d) in the presence of objective data without dysfunction | "B-4" |
The article covers infectious and parasitic diseases of the central nervous system, lesions of the brain or spinal cord in general infections, acute and chronic intoxications, demyelinating diseases of the central nervous system.
Point “a” includes diseases of the nervous system, accompanied by deep paralysis or paresis, severe secondary parkinsonism, severe widespread hyperkinesis, frequent (5 or more per year) epileptic seizures, ataxic disorders, hydrocephalus, increased intracranial pressure syndrome with pronounced clinical manifestations.
Persons suffering from multiple sclerosis are examined under point “a”, regardless of the degree of dysfunction.
Point “b” includes residual effects and consequences of diseases that, due to the degree of dysfunction of the central nervous system, limit the possibility of military service, but do not exclude it completely (residual effects of encephalitis with moderate hemiparesis in the form of decreased muscle strength, increased muscle tone, hydrocephalus with a syndrome of increased intracranial pressure with moderate clinical manifestations), as well as with frequent (2 or more times a year) and long (at least 4 months) periods of decompensation of painful disorders (in military personnel - subject to treatment in a hospital setting, while on vacation due to illness or complete release).
Point “c” includes the consequences and residual effects of damage to the central nervous system with minor dysfunction, individual organic signs, combined with autonomic-vascular instability and asthenoneurotic manifestations if treatment is unsuccessful. If the condition improves and the ability to perform the duties of military service is restored, the examination is carried out under point “d”.
Point “d” includes the consequences and residual effects of damage to the nervous system, in which there is a slight asthenic syndrome, vegetative-vascular instability and individual persistent scattered organic signs that are not accompanied by a disorder of the motor, sensory, coordinating and other functions of the nervous system.
The presence of the disorders specified in this article must be confirmed by medical documents, information from characteristics from the place of work, study or military service about the impact of such disorders on the ability to work or perform the duties of military service, and the diagnosis must be confirmed by the results of clinical and special studies. In this case, a conclusion on the category of suitability for military service of citizens upon initial registration or conscription for military service (military training) is made after an examination in stationary conditions.
When assessing the severity of the syndrome of increased intracranial pressure, the clinical manifestations of the disease are taken into account (headache, vomiting, oculomotor disorders, cognitive impairment, gait disturbance, dysfunction of the pelvic organs), indicators of cerebrospinal fluid pressure during lumbar puncture, the presence of congestive changes in the fundus, secondary atrophy of the optic discs nerves, the presence of hydrocephalus according to computer (magnetic resonance) tomography.
In the presence of emotional-volitional or intellectual-mnestic disorders resulting from organic brain damage, infectious disease or intoxication, the examination is carried out according to Article 14 of the schedule of diseases.
The expansion of the ventricular system of the brain is assessed using computed tomography (magnetic resonance) imaging. Signs of hydrocephalus are considered to be the ratio of the maximum width of the anterior horns to the distance between the internal plates of the frontal bones at this level of more than 0.5 (less than 0.4 is normal, 0.4 - 0.5 is a borderline value, more than 0.5 is hydrocephalus), index Evans (ratio of the width of the anterior horns to the maximum distance between the internal plates of the parietal bones) over 26, index of the third ventricle (up to 20 years - over 3.0, up to 50 years - over 3.9, 50 years and older - over 4.5) . The presence of periventricular edema is assessed according to computed tomography (decrease in the density of periventricular white matter), magnetic resonance imaging (high-intensity signal on T2 images).
The criteria for pronounced clinical manifestations of increased intracranial pressure syndrome are:
- the presence of headache, vomiting, oculomotor disturbances, cognitive impairment, gait disturbances, pelvic organ dysfunction, congestive optic discs or secondary optic disc atrophy;
- CSF pressure during lumbar puncture is over 300 mmH2O. Art.;
- periventricular edema.
The criteria for moderate clinical manifestations of increased intracranial pressure syndrome are:
- presence of headache, initial symptoms of congestion in the fundus;
- CSF pressure during lumbar puncture is over 200 mmH2O. Art.
You may also want to know:
- Do they take into the army with asthma?
- Do they take into the army with flat feet?
- Do they take you into the army with gastritis?
- How to get a military card after 27 years?
Go back to main page
Do you understand everything in this article on Disease Schedules?
If there are even minimal doubts, then it is better to consult a doctor - this will help you save a lot of time and effort, and, probably, will save you from the army. You can ask a doctor a question for free using this LINK
OR
in CHAT FOR CONTRACTS
Research
Research is being conducted in various specific areas. The main focus of this study is to obtain more detailed information about demyelinating disorders affecting the central nervous system and peripheral nervous system, how they develop and how these disorders are influenced by various external influences. Most research is aimed at studying the mechanisms, development of diseases and dysfunctions in order to develop treatments.
Ideas
N-cadherin is now believed to play an important role in the process of myelination. Experiments have shown that N-cadherin plays an important role in creating remyelination-favorable conditions. this has been shown in animal models.
Influence of somatic factors
Experiments have shown that managing thyroid hormone levels may be considered as a strategy to improve remyelination and prevent irreversible damage in patients with multiple sclerosis. N-cadherin agonists have been identified and studied as stimulators of cell growth and migration, axon development, and remyelination after injury or disease. It has been shown that intranasal administration of ATP (transferrin) can protect myelin and stimulate remyelination.
Causes
The etiology of demyelinating diseases is based on a combination of hereditary predisposition and environmental influences.
Of the external factors, the greatest influence is exerted by:
- viral diseases (rubella, measles, herpes, etc.);
- bacterial infections;
- campylobacter infections;
- intoxication of the body with chemicals;
- poor diet (too much fat and protein);
- severe stress;
- poor environmental conditions.
Pathologies of the following genes can be inherited by a person:
- histocompatibility;
- cytokines;
- immunoglobulins;
- myelin proteins.
The mechanisms of development of this group of diseases are similar and consist in the development of autoimmune reactions to neuroantigens (a number of proteins, as well as lipids of the myelin sheath).
Autoreactive lymphocytes then enter the nervous system and release proinflammatory cytokines.
Due to the fact that the number of inflammatory mediators in the brain sharply increases, the microenvironment quickly changes, and anti-myelin antibodies are formed.
The primary form can be stopped, but secondary degeneration leads to persistent neurological disorders.
Demyelinating diseases in animals
Demyelinating diseases/disorders have been diagnosed in mice, pigs, cattle, hamsters, rats, sheep, Siamese kittens, a number of dog breeds (including Chow Chow, Spaniel, Dalmatian, Golden Retriever, St. Bernard, Hungarian Vizsla, Weimaraner, Australian silky terrier, and mixed breeds.
This type of disease has been diagnosed not only in land animals, but also in marine animals. The most famous of the cases is Ziggy Star, a female northern fur seal who was treated at the Marine Mammal Center beginning in March 2014. This was the first recorded case of such a disease in a marine mammal. She was later transported to the Mystic Aquarium & Institute for Exploration for lifelong care.