Recently, the world has seen an increase in such a serious disease as multiple sclerosis. Often people with multiple sclerosis turn to doctors for help very late, since the onset of this disease is easy to miss. Early symptoms of multiple sclerosis are usually not cause for concern. Therefore, we want to draw your attention to the main symptoms of multiple sclerosis in its early stages, which should not be ignored.
canva.com
Diagnostic signs
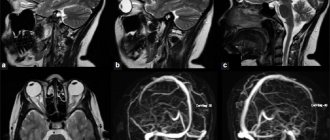
When making a diagnosis, neurologists at the Yusupov Hospital take into account objective data and the results of MRI, which reveals the dissemination of lesions. The pathological process can be confirmed if two or more lesions are detected on MRI, as well as if the symptoms progress over time (in the presence of subsequent attacks, new lesions or excessive accumulation of the injected contrast agent). In addition, specialists examine the patient’s cerebrospinal fluid, in which oligoclonal bands of immunoglobulins are detected.
The clinic's ophthalmologists determine visual fields, assess the contrast sensitivity of the eye, retinal thickness, and the condition of the fundus. One of the most important diagnostic methods used by our neurologists is a study that tests the somatosensory, auditory and visual evoked potentials of the brain.
Our Moscow center for the treatment of multiple sclerosis uses modern equipment from leading medical equipment manufacturers from the USA and Europe to conduct examinations.
Expert opinion
Author: Boyko Alexey Nikolaevich
Neurologist, Head of the Research Center for Demyelinating Diseases, Doctor of Medical Sciences, Professor
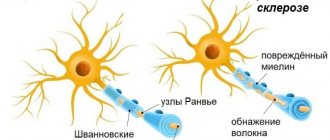
There are many autoimmune diseases, one of them is multiple sclerosis. This is a pathology in which immune cells attack the myelin sheath of a neuron. In simple words, a neuron is like a wire, and the myelin sheath is its insulation, and lymphocytes remove it.
The appearance of multiple sclerosis is associated not only with weakened immunity, but also with vitamin D deficiency - the disease is more common in the north than in the south. Previously, MS was associated with race, but studies have shown that members of the Caucasian race (usually living in northern latitudes) who change their place of residence to a sunnier one get sick less often.
Multiple sclerosis has many symptoms; American neurologists have described more than 500. The diagnosis can only be made by a specialist after a full examination, including MRI and punctures. The disease is rapidly getting younger, women need to be especially attentive to general neurological symptoms and undergo regular examinations, especially if there are risk factors - heredity, vitamin D deficiency, bad habits.
Multiple sclerosis misdiagnosis
The following diagnoses may cause neurological symptoms similar to those caused by multiple sclerosis (MS). To confirm a diagnosis of MS, your healthcare provider must be able to rule out other possible diagnoses that could explain the symptoms you are experiencing.
Some of these diagnoses can be easily ruled out with a simple blood test (such as vitamin B12 deficiency), while others, such as sarcoidosis, may require a biopsy. Some are much rarer than others. It is important to work with a healthcare professional who is familiar with these conditions to get the correct diagnosis and appropriate treatment as quickly as possible, whether you have MS or not.
Central nervous system (CNS) infections
Lyme disease is an infection caused by the organism Borrelia burgdorferi, which is transmitted to humans by the deer tick. Syphilis is a sexually transmitted infection caused by the active substance Treponema pallidum, which can cause neurological symptoms many years after the initial infection. Progressive multifocal leukoencephalopathy (PML) is a potentially fatal infection of the white matter of the brain caused by the JC virus (a virus common and dormant in the general population), which can be reactivated in people with MS who take Tysabri® (natalizumab), a human immunodeficiency virus ( HIV is a virus that can lead to acquired immunodeficiency syndrome or AIDS. Human T-cell lymphotropic virus-1 (HTLV-1) myelopathy/tropical spastic paraparesis is a chronic progressive disease of the nervous system.
Inflammatory diseases of the central nervous system
Sjögren's syndrome is a chronic autoimmune disease that affects the glands that produce moisture, causing dry eyes and mouth, general fatigue, joint pain and sometimes neurological symptoms. Vasculitis is an autoimmune disease that affects the blood vessels that supply the brain and spinal cord, causing neurological symptoms. Systemic lupus erythematosus is a chronic inflammatory autoimmune disease that can affect the skin, joints, kidneys, lungs, nervous system and other organs of the body. Sarcoidosis is a chronic, possibly autoimmune disease that causes collections of inflammatory cells (granulomas) in the lungs, skin, lymph nodes, liver, and central nervous system, usually causing respiratory symptoms and sometimes neurological symptoms. Behçet's disease is an autoimmune disease that damages blood vessels, especially veins. In addition to mouth ulcers, genital pain, eye inflammation and skin problems, Behcets may affect the white matter in the brain.
Genetic disorders
Hereditary myelopathies are a number of inherited diseases involving the spinal cord, including hereditary cerebellar degeneration, leukodystrophy, and motor neuron disorders (including nerve pathways in the spinal cord). Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) is an inherited disease that primarily affects small blood vessels in the white matter of the brain, causing numerous progressive neurological symptoms. Leukodystrophies are rare, inherited, progressive disorders that damage myelin in the central nervous system and cause neurological symptoms. Hereditary cerebellar degeneration is a group of inherited disorders that cause slowly progressive loss of motor coordination, as well as poor hand, speech and eye coordination. Mitochondrial disease is a disorder of mitochondria (structures in cells that produce energy) that affects various body functions and can cause neurological symptoms.
Brain tumors
Metastases. Cancer that has spread from its original location to another is considered metastatic. Some types of cancer—breast, lung, kidney, and skin (melanoma)—are more likely to spread to the central nervous system and cause neurological symptoms. Lymphoma is a blood cancer involving the rapid replication of abnormal T or B lymphocytes (types of white blood cells) that form tumors - which sometimes begins in the central nervous system (CNS) or spreads to the brain from other places.
Nutrient deficiencies
Copper deficiency is a relatively rare deficiency seen with excessive zinc intake or certain types of gastric surgery, which can cause neurological symptoms. Vitamin B12 deficiency – Deficiency of this vitamin, which is critical for neurological function, can occur due to dietary restrictions or absorption problems and is a common cause of neurological symptoms.
Structural damage to the brain or spinal cord
Cervical spondylosis is a spinal degeneration associated with normal aging that can put pressure on the spinal cord and cause neurological symptoms. A herniated disc is a disc that acts as a cushion between the vertebrae (bones) of the spine that can deteriorate with age by moving or slipping out of place (called a herniation). A herniated disc puts pressure on the nerves in the area, causing neurological symptoms. Chiari malformation is an abnormality in the position of the cerebellum, a brain structure responsible for balance and coordination. When the cerebellum sits too low, it puts pressure on the spinal cord or brain stem, causing neurological symptoms.
Treatment
If research results suggest that a patient has multiple sclerosis, doctors at the Yusupov Hospital prescribe symptomatic treatment and betaferon. If a reliable diagnosis was established for the first time (at the onset of multiple sclerosis), it is necessary to influence the primary link of the pathological process. The main goals are to reduce activity and prevent disease progression. To achieve them, the use of one of the drugs is prescribed: betaferon, glatiramer acetate or rebif.
Relapsing-remitting multiple sclerosis in the acute stage requires taking measures aimed at reducing the activity of the pathological process and eliminating the exacerbation (reducing the severity of neurological deficit) or achieving regression of new neurological symptoms. For this purpose, patients at the Yusupov Hospital are prescribed the following medications:
- glucocorticosteroids (methylprednisolone, Solu-Medrol, dexamethasone);
- ACTH (synacthen depot);
- cyclosporine A.
If the patient does not have the opportunity or desire to receive drug therapy, neurologists at the Yusupov Hospital use plasmapheresis to relieve an exacerbation. In addition, patients are prescribed immunoglobulin β-1b or β-1a, intravenous immunoglobulin or glatiramer acetate.
Treatment of remitting-recessive multiple sclerosis in the remission stage is aimed at reducing the activity of degenerative and immunopathological processes, increasing the duration of remission and the severity of the next exacerbation.
For one to two years, patients require intravenous administration of maintenance doses of immunoglobulin (at a dosage of 50 ml per month). Reparative medications, symptomatic therapy, and rehabilitation using modern techniques are prescribed.
Patients with secondary progressive multiple sclerosis at the Yusupov Hospital are prescribed therapy aimed at eliminating neurovegetative changes, improving immunoregulation and preventing exacerbations. In this case, interferons 1-β or cytostatics (azathioprine, cyclophosphamide, cladribine) and reparative drugs are effective. Symptomatic treatment and rehabilitation are also carried out.
Primary progressive multiple sclerosis is the most difficult to treat. The efforts of doctors in these cases are aimed at slowing down the course of the disease, slowing down neurodegenerative processes, and stabilizing the pathological process. This task can be accomplished through the use of interferons, cytostatic and symptomatic drugs, and intravenous administration of immunoglobulin.
Rehabilitation measures carried out by specialists at the Yusupov Hospital are also effective: massage, physical therapy, physiotherapy and acupuncture.
Make an appointment
Multiple sclerosis is characterized by:
The onset of the disease is at the age of 15-50 years;
alternation of exacerbation and remission (situation “doctor, I had these sensations, but then they passed”);
thermosensitivity (even if the patient has undergone a course of treatment, and it was effective, the discomfort resumes when heated - hot bath, solarium, beach);
a feeling of “current running along the spine”;
Laboratory diagnostics
A blood test is a fairly informative study that allows you to exclude or confirm the diagnosis. To do this, neurologists analyze the following indicators:
- level of anti-inflammatory cytokinins in peripheral blood;
- lymphocyte transformation reaction upon contact with myelin basic protein;
- indicator of antibodies to myelin.
With a confirmed diagnosis in patients with multiple sclerosis, a blood test demonstrates the dynamics of the process.
Diagnostic and treatment methods at the Yusupov Hospital are selected individually for each patient. When selecting drugs and their dosages, the clinical symptoms of the disease and its course are taken into account. The therapy can significantly improve the quality of life of patients.
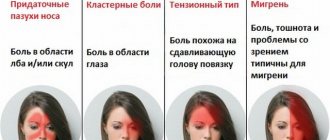
Early symptoms
According to the Multiple Sclerosis Foundation, early signs and symptoms include:
- numbness and tingling in the legs, feet, arms, hands, or face.
- vision problems such as blurred or double vision, loss of vision or color contrast, and pain when moving the eyes.
- fatigue
- difficult walking
- bladder diseases
- sexual problems, such as decreased sex drive
- problems with memory or speech
- depression and emotional changes
- muscle spasms and tremors
However, symptoms vary from person to person and may change over the course of the disease. They may also depend on the location of the nerves affected by the disease.
Forecast
The life expectancy of patients with multiple sclerosis is closely related to the form of the disease, its course and the adequacy of treatment. In extremely rare cases, the disease is fatal.
The prognosis of the disease improves significantly in the presence of the following favorable prognostic signs:
- onset of the disease in childhood – (2-3 years);
- the presence of precursors of diabetes mellitus, occurring immediately before diabetes and in the long-term history;
- rapid and simultaneous formation of neurological symptoms at the onset of the disease;
- monosyndromic nature;
- debuts of short or medium duration;
- mild or moderate onset of the disease;
- absence of sphincter disorders at the onset;
- no need to use glucocorticoids at the onset and the first 6 years from the onset of the disease, or high efficiency of therapy with these drugs.
Favorable prognostic MRI criteria include:
- periventricular zones of luminescence in the region of the posterior horns of the lateral ventricles, if other MRI signs of multiple sclerosis are absent;
- visible foci of demyelination, signs of external and internal hydrocephalus are absent.
Clinical prognostic criteria are considered unfavorable if the disease appeared before the age of 15 or after 40 years, especially in men, as well as with a slow rate of formation of the clinical picture at the onset of the disease and polysyndromic, severe and protracted onset of the disease.
We can talk about an unfavorable prognosis for multiple sclerosis if the MRI revealed pronounced atrophic changes with a small number of foci, “black holes,” significant atrophic changes in the early stages of the disease, and also if there are no periods of “decay” of MRI signs.
Hospitalization at the Yusupov Hospital is possible even for those patients who were refused in other specialized clinics. Treatment is carried out using innovative therapeutic methods that significantly improve the prognosis. If the patient wishes and if necessary, a stem cell transplant may be recommended at partner clinics.
You can make an appointment for a consultation with a neurologist at the Yusupov Hospital by telephone 24 hours a day.
Author
Alexey Vladimirovich Vasiliev
Head of the Department of Neurology, neurologist, Ph.D.
Characteristics of the procedure
This is an examination related to invasive interventions. As part of this procedure, cerebrospinal fluid (CSF) is taken from the cavity of the spinal canal in the area of the lower lumbar spine. At this level, the spinal cord is absent - it ends at levels 1-2 of the lumbar vertebrae. Therefore, there is no risk of damage to it. The study of cerebrospinal fluid is an irreplaceable diagnostic procedure that has no alternatives.
CSF is typically a clear, slightly yellowish fluid produced in the ventricles. It flows through them, surrounding the brain and ultimately being absorbed into the venous nodes.
CSF is also present in the spinal canal around the spinal cord, providing it with similar protection.
Another type of puncture is a puncture biopsy. It is performed to examine soft tissues, in particular glands (prostate, thyroid, etc.), kidneys, and liver.
The puncture site is between the 4th and 5th (L4-L5) or between the 3rd and 4th vertebrae (L3-L4). This is approximately below the point where the lower back crosses the imaginary line between the crests of the femurs. The spinal cord usually ends at the level of the L 1-2 vertebra, slightly lower in women. The sac of spinal membranes containing the spinal cord ends at the 2nd sacral vertebra (S2), so the puncture is made between L3-L5 without the risk of damaging it.
When performing a spinal puncture in children (newborns, infants and infants), the puncture is usually made as low as possible, since the child’s spinal cord extends almost to the sacral region.
Executing the procedure
A spinal tap is an operation performed in a clinic. An important prerequisite for a successful examination is the correct position of the patient being examined.
- During the procedure, the patient wears a hospital gown that is tied at the back.
- The patient takes the recommended position.
- The puncture site is disinfected (with antiseptic soap or iodine) to prevent infection.
How to take a spinal cord puncture:
- Local anesthesia is applied to the lower back to numb the puncture site before the needle is inserted.
- A thin hollow needle is inserted between the 2 lower vertebrae (lumbar region) and reaches the target area. The patient is not in pain, but there may be a feeling of pressure in the back.
- Once the needle reaches the target area, the doctor may ask the patient to change position slightly. Otherwise, you can’t move, it’s dangerous!
- The doctor measures the CSF pressure, takes a small sample, and measures the pressure again. If necessary, a medicine or other substance is administered.
- The needle is removed and the puncture site is covered with a sterile bandage.
- The procedure usually takes about 45 minutes. After the examination, the patient rests for several hours in the clinic.
During a lumbar puncture, the Queckenstedt test is performed. It involves applying finger pressure to one or both internal jugular veins. If the spinal canal is patent, the pressure increases. With obstruction, there is a slight increase in pressure or no increase in indicators.
- Calmness and relaxation are important for the patient. On the day of the puncture, performing any strenuous activities is prohibited.
- If a headache or back pain occurs, take a pain reliever (eg Paracetamol).
- The doctor evaluates the results of a laboratory analysis of a sample of cerebrospinal fluid along with other information obtained during the puncture. According to the findings, the presence of the disease is confirmed or refuted.
Limitations in normal lifestyle and ability to work are individual for each patient. They are determined taking into account the nature of the disease, recovery, social and professional involvement after the procedure. Individual restrictions are set immediately after the puncture.