- Features of the disease 1
- Types of flow 2
- The insidiousness of the disease 3
- Destruction in nerve fiber 4
- Symptoms of Multiple Sclerosis 5
- Classic symptoms 5.1
- Rare symptoms 5.2
Author: Larisa Vladimirovna, higher medical, neurologist.
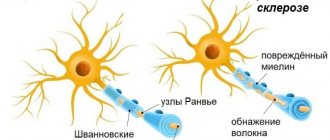
Neurologists call multiple sclerosis a disease of exposed nerves. A common expression reflects the main pathogenetic process of this suffering - the destruction of the myelin sheath.
There are also unmyelinated nerve fibers in the body; they are located in the peripheral autonomic nervous system. The axial cylinders or axons are surrounded by neurolemmocytes; one nerve may have several axial cylinders, as in a cable.
All structures that provide voluntary movements are innervated by myelin-covered nerves. They are located in the somatic nervous system, their axons are thicker, and myelin is laid in 2 layers. The structure of such nerves can be compared to an electrical wire when the rod is braided. In an undamaged wire, the electrical impulse flows strictly along its intended path. In the same places where the braid is destroyed, the impulse goes wherever it pleases. Hence the difficulty of diagnosing the variety of symptoms.
A nerve impulse travels along a myelinated fiber at a speed of 5 - 120 m/sec, and along a non-myelinated fiber - 1-2 m/sec.
Types of disease progression
The development of the disease depends on the changes that have already occurred in the myelin sheath during the period when there were no obvious signs. Depending on the stage of the disease, there are 5 main types:
- Benign MS. The onset of the disease is unnoticed, with rare and mild exacerbations, or they may not exist at all. There are already areas of damage to the myelin sheath, which during the period of remission manages to recover, if not completely, then partially. Benign MS does not lead to disability, and patients may well consider themselves healthy. This type of disease occurs in 20% of patients.
- Relapsing-remitting MS. Alternation of attacks of deterioration and periods of complete recovery. During remission, partial or complete restoration of the affected organs may occur. The period of exacerbation takes from several days to several weeks. It may take several months to recover from an attack. This type of course is typical for the initial period of the disease.
- Primary progressive MS. The patient's health can be described as gradually deteriorating. There are no clearly defined exacerbations, but there is a gradual decrease in ability to work. It is typical for those who developed the disease after 40 years of age and occurs in 10% of patients.
- Secondary progressive (progressive) MS. The initial symptoms are the same as in the remitting stage, with alternating phases of exacerbation and remission. Gradually enters a stage of rapid and constant progress. Within 5 years it can lead to complete loss of ability to work (disability).
- Progressive-remitting MS. One of the rarest forms of the disease. Against the background of a gradually worsening condition, acute attacks occur from time to time. They are followed by some improvement in well-being. The initial stage of the disease occurs as a type of primary progressive MS.
Depending on the area of damage to the nerve endings, various forms of multiple sclerosis are distinguished:
- cerebral - occurs when the brain is damaged;
- spinal – with damage to the spinal cord;
- cerebrospinal – simultaneous damage to the spinal cord and brain;
- cerebellar – damage to the cerebellum, which is responsible for coordination of movements;
- optical – damage to the optic nerve;
- stem – damage to the cells of the brain stem responsible for speech and the ability to swallow.
Some researchers adhere to a different classification and consider them to be stages of the disease that occur in the patient during the course of the disease.
Diagnostics
The disease is diagnosed after the occurrence of a damaging factor, which is associated with damage to the nerves. Common complaints include severe impairment of vision, hearing, limb weakness and loss of sensation. Diagnostic procedures that detect sclerosis with maximum accuracy include MRI and spinal puncture.
But the diagnosis has negative nuances:
- The time between the start of the examination and the diagnosis can take from 15 to 45 days.
- The telling of the clinical picture. This term refers to the vagueness of the symptoms of the disease. Sclerosis is a very long-term disease, so diagnosis may not be made immediately even after symptoms are identified.
The first signs of occurrence are confirmed by the appearance of secondary symptoms of sclerosis - this is the main characteristic feature of an accurate diagnosis. The age category currently ranges from 20 to 50 years.
Treatment of multiple sclerosis.
The main task is to reduce the activity of the pathological process during the period of exacerbation and in the acute stage of the disease.
- For this purpose, corticosteroids (prednisolone, dexamethasone) and ACTH are used in large doses. Prednisolone is prescribed orally in intensive or suppressive doses, depending on the activity and depth of the pathological process. The intensive dose of prednisolone is 0.75 mg/kg per day. The entire daily dose is given in 1 or 2 doses in the early morning hours. Glucocorticoids are prescribed either daily or every other day; The duration of treatment is 2-3 weeks, then the amount of the drug taken is gradually reduced over 2'/g-3 months.
- At the same time, anabolic hormones are prescribed (Nerobol, Retabolil),
- potassium and calcium preparations, ascorbic acid, veroshpiron.
Retabolil is administered intramuscularly at 50 mg 1-2 times a week, for a course of 25-30 injections. Nerabol is prescribed 1-2 tablets 2 times a day, daily dose 10-20 mg; veroshpiron - 25 mg 2 times a day, daily dose 50 mg.
Suppressive doses of prednisolone are prescribed according to a continuous (daily) or intermittent (every other day) regimen in a gradually increasing or immediately suppressive dose, depending on the severity and severity of the process. According to a continuous regimen, the maximum daily dose of prednisolone is up to 1.5 mg/kg. Once the therapeutic effect is achieved, the dose is gradually reduced under the control of the patient’s general condition. In an intermittent regimen, prednisolone is prescribed every other day. The daily dose is divided into two equal parts. The first half is given in the morning after breakfast, the second half an hour later. In recent years, very high doses of methylprednisolone (10-15 mg/kg per day) by intravenous administration 3-4 times a day for 3-5 days have been used with good effect, followed by switching to taking a tablet drug every other day (1 mg/kg ). Once the therapeutic effect is achieved, the dose of the drug is gradually reduced. Regardless of the size of the doses of prednisolone used, the amount of the drug is reduced until complete withdrawal.
Treatment with ACTH is carried out at the rate of 1000 units per course, the daily dose for intramuscular administration is 40-60 units.
In case of exacerbation of the disease, it is also possible to use etimizol 100 mg 3 times a day for 1.5-2 months
Patients with a steadily progressive course of the disease are prescribed levamisole 150 mg per day for 3 days every week for 3-4 months. In connection with the discovery of impaired cellular immunity in patients with multiple sclerosis, immunomodulators have begun to be used for therapeutic purposes in recent years: T-activin (100 mcg subcutaneously daily for 5 days, subsequently for a long time, 1-3 injections every 10 days) and thymalin (10 mg intramuscularly 2 times a day for 5 days, subsequently for a long time every 10 days by injection for 1-3 days). At all stages of the disease, the following are widely used: B vitamins, desensitizing agents, ATP, Trasylol, Cerebrolysin.
Among symptomatic drugs, drugs that reduce muscle tone occupy an important place: baclofen, seduxen.
In the presence of hyperkinesis, dynesin and narokin are indicated.
Physical methods of treatment mainly include dosed gymnastics and selective massage. Balneo- and mud therapy, as well as solar insolation, are contraindicated. Patients may be recommended sanatorium-resort treatment of a restorative type, not associated with a sharp change in usual climatic conditions.
Treatment should be intensive not only during exacerbation of the disease, but also in remission. In the latter case, it must be carried out 2 times a year (spring and autumn), conducting courses of vitamin therapy and biostimulants. This treatment, together with a set of measures to prevent infections, intoxications, overwork, etc. in patients, is to a certain extent a prevention of exacerbation.
Forecast.
The prognosis for life is favorable, with the exception of cases with acute pallor disorders, which sometimes lead to death. There are cases with a long-term favorable course, when patients can remain able to work for quite a long time. However, many patients become disabled during the first 3-5 years after the onset of the disease
In this regard, when employing them, it is important to correctly and timely determine the disability group, which can contribute to a longer working capacity of patients
Infectious diseases
The clinical picture of PPMS can be imitated by various infectious diseases of the central nervous system, including chronic borreliosis encephalomyelitis, which often develops after non-erythematous and subclinical forms of the primary stage of Lyme disease. Many patients do not indicate tick bites when interviewed. Changes in MRI of the brain and spinal cord also do not allow a differential diagnosis between chronic borreliosis encephalomyelitis and PPMS. If a patient with suspected PPMS has epidemiological data indicating ixodid infection (history of tick bites, erythema migrans), a combination of symptoms of damage to the central and peripheral nervous system, damage to various organs, including joints and the heart, and there are no focal changes on MRI spinal cord, then to exclude chronic borreliosis encephalomyelitis it is necessary to determine antibodies to B. burgdorferi using enzyme-linked immunosorbent assay and/or immunoblotting or bacterial DNA using polymerase chain reaction.
Given the high incidence of HIV infection, which in Russia and the CIS countries exceeds that in some other regions of the world, PPMS often has to be differentiated from neurological complications of HIV infection. According to morphological studies, the frequency of damage to the nervous system during HIV infection reaches 70–80%, and 40–60% of patients have clinical manifestations in the form of a variety of neurological, mental and cognitive disorders. Most often, a differential diagnosis must be made with HIV-associated minimal cognitive-motor disorders, which are described in more than 80% of patients, HIV encephalopathy and HIV-associated myelopathy. Changes on MRI and in the cerebrospinal fluid are nonspecific, therefore, to confirm the diagnosis of HIV infection, it is necessary to conduct a virological study and determine the patient’s immune status.
Neurosyphilis occurs in approximately 3–5% of patients with syphilis and occurs at any stage of infection, including primary, secondary and tertiary syphilis. In the Russian Federation, the number of reported cases of neurosyphilis increased from 19 cases in 1992 to 987 in 2011; while most of them were late forms. From the point of view of the relevance of the differential diagnosis with PPMS, parenchymal forms of neurosyphilis, including tabes dorsalis, progressive paralysis, or a combination thereof, are of greatest importance. Damage to the spinal cord most often occurs at the stage of tertiary syphilis and has the character of tabes dorsalis, which is a progressive degenerative process characterized by demyelination and inflammatory changes in the spinal cord. Develops in 3–5% of patients with neurosyphilis 10–20 years after infection. Demyelination is especially pronounced in the posterior columns of the spinal cord and dorsal ganglia, but over time, cells of the anterior horns of the spinal cord may also be involved. MRI of the spinal cord reveals atrophy of the posterior columns and prolonged T2 hyperintense lesions. Isolated cases of focal damage to the spinal cord with syphilitic meningomyelitis, vascular myelitis or mechanical compression by gumma have been described. Clinical manifestations include gradually increasing paresthesia and “dagger” pain in the legs, absence of tendon reflexes, impaired muscle-joint sense and vibration sensitivity in the legs, sensory ataxia, erectile dysfunction, dysfunction of the bladder and large intestine, neurodystrophic changes in the joints (joints) Charcot). In parallel, symptoms of brain damage (seizures, headaches, hearing loss, etc.) may be observed.
Progressive paralysis appears 20–40 years after the initial lesion. It is based on a predominant lesion of the brain substance, often in the area of the frontal cortex. The clinical picture is dominated by cognitive and mental disorders.
Due to the absence of pathognomonic clinical variants, serological testing of blood and cerebrospinal fluid is of leading importance in the diagnosis of neurosyphilis. The diagnosis can be established if three criteria are met:
Healthy lifestyle
Particular attention must be paid to maintaining a healthy lifestyle. This includes moderate physical activity and proper nutrition. These factors lead to increased tone, improved well-being and improved health.
In conclusion, I would like to say that it is necessary to pay careful attention to your well-being, while not neglecting periodic examinations and diagnostics of the general condition of the body. These simple rules of life will help you avoid complications and stop the disease at the earliest stages of its manifestation.
If you have information about the disease, share your experience in the comments - your knowledge is very important for other patients and their loved ones. Information is the main weapon in the fight against disease.
Secondary progressive MS
Multiple sclerosis is a slowly progressive chronic disease. Most people diagnosed with MS are in a relapsing-remitting course of the disease, which is characterized by alternating states of exacerbations and remissions with partial or complete recovery. Most of the patients with this course of MS have a secondary progressive type of the disease, namely about 80% go into the secondary stage. The disease begins a gradual progression, even taking into account the fact that exacerbations appear less and less often or do not appear at all.
Recognizing the secondary course of the disease is not so easy. To date, there are no special studies and tests that could be used to distinguish the course of primary progressive MS from secondary one. The process of transition to the secondary progressive type of MS is determined by neurologists based on the results of clinical observations of the patient. It is noted that recovery after exacerbations does not begin to occur completely; symptoms remain. As a rule, the transition to a new type of disease occurs 10-20 years after the onset of MS. There is evidence that after 5 years of having multiple sclerosis, almost 10% with the primary progressive form have reached the secondary progressive type. This ratio increased to 25% in ten years, and in 30 years to 75%.
To accurately establish the secondary progressive type of MS, it may take up to 6 months or more after the start of observations.
Symptoms of SPMS
With the relapsing-remitting type of MS, there is a pattern of disease progression with alternating exacerbations and remissions. The symptoms of SPMS are not so obvious as to provide such a picture of the course of the disease. Exacerbations may occur less frequently or not at all. If an exacerbation occurs, then recovery is not performed. Obvious symptoms of SPMS include:
- great weakness
- serious problems with coordination
- hard and dense leg muscles
- increasing bowel and bladder problems
- obvious problems with clarity of thinking
- the occurrence of depression
- persistent fatigue
Your doctor can only diagnose SPMS by comparing your symptoms over time
Therefore, it is important to have a trusting relationship with your doctor so that you can provide him with as much information as possible about any changes in your symptoms
Secondary progressive type. Causes
It is not yet clear why multiple sclerosis begins to move towards the secondary progressive type.
Some scientists believe that this may occur as a result of nerve injury, which could occur in the early stages of the disease. More research is needed to more accurately substantiate these changes in the course of the disease.
Secondary progressive type. Treatment
Secondary progressive MS is often more difficult to treat than relapsing-remitting MS.
The main type of drugs for MS are called disease-modifying drugs (DMDs), which make relapses less frequent and symptoms less severe. For people with the secondary type who still have exacerbations, DMT may still serve its function of slowing the progression of the disease. But for those whose symptoms simply get worse, the drugs don't really work.
One of the basic drugs for the treatment of SPMS is called mitoxantrone, which is approved in the USA. The drug rather works to treat relapses. Plus has a number of serious side effects such as
- tachycardia
- hair loss
- back pain
- myocardial ischemia
- nausea, vomiting
- liver dysfunction
and etc.
Typically, this drug is used to treat an acute or rapid illness when other treatments are not suitable. Methoxantrone is an immune suppressant and is often used to treat rheumatoid arthritis, but it may still be used to improve symptoms in secondary progressive MS.
Symptom management
There are a large number of medications that help relieve pain and normalize bowel and bladder function, including those for multiple sclerosis. As with other forms of chronic illness, one should remember the lifestyle with MS. Physical exercise will help you monitor your energy levels, normalize and control your weight, and maintain your mood tone. In MS, moderate exercise is recommended to increase energy and maintain physical activity.
Symptoms
The clinical picture depends on the location and form of multiple sclerosis. In the early stages, there may be no manifestations, or they are so weak that they do not make themselves felt until a certain moment. The first signs are weakness, dizziness, which are attributed to fatigue and changes in weather. The duration of the initial period is from a couple of months to 3-4 years. In total, 7 groups of characteristics are distinguished.
Impairments of cognitive and mnestic functions
Accompanied by the following manifestations:
- Decrease in intelligence level. The decrease in cognitive functions is especially noticeable in the mental nature of professional activity. The patient is unable to perform duties. Formally, intelligence is preserved, but the ability to use it is no longer there.
- Memory loss. The patient distinguishes between relatives, remembers words, and speaks correctly. In this case, the lexical structure and vocabulary may be impoverished.
- General dementia. An extreme degree of impairment of mnestic functions is also possible. It is observed at the terminal stage of multiple sclerosis and cannot be corrected. Characterized by a total disruption of brain function. The patient is unable to take care of himself in everyday life, becomes helpless, and falls into childhood.
Disorders of the natural needs of the body, dysfunction of the pelvic organs
Complete urinary incontinence. It is observed with severe disruption of the spinal cord, generalized damage to the white matter. The patient is unable to control the urge to empty the bladder. In difficult cases, the process of defecation also suffers. Both symptoms are indications of damage to the lumbosacral spinal cord.
In milder cases, an imperative urge to urinate is likely. The patient is not able to contain them, but partial control is present.
The opposite phenomenon is the inability to relieve need naturally. Constant catheterization of the bladder and cleansing of the large intestine using artificial methods are required. The patient becomes deeply disabled.
Decrease in musculocutaneous sensitivity, loss of tactile sensations
Sensitivity falls below the level of demyelination. If the brain is damaged, sensation below the head is lost. Complete or partial - depends on the stage of the pathological process. All types of tactile sensations decrease. Up to the inability to feel pain impulses. Formally, this is not paralysis or paresis. Motor activity is fully preserved. The sheaths of nerve endings along the periphery die off, which makes it impossible to transmit signals, including pain impulses. The numbness does not go away, tactile sensitivity is not restored, the process is irreversible.
Multiple sclerosis is manifested by a neurological defect in the coordination of movements
The first thing the patient encounters is constant mild or moderate dizziness. It occurs in fits and starts. Indicates a disruption of the cerebellum for the reasons stated above. The second possibility is muscle stiffness. The patient is unable to perform simple movements due to muscle stiffness. There is a lack of coordination. The body literally does not obey commands. The upper and less often the lower limbs are affected. In severe cases, both.
Pyramid violations
Determined by paresis or paralysis (in more severe cases).
Deviations of nervous functions caused by damage to the cranial nerves
- Dysphagia. Loss of ability to swallow. Leads to difficulty or complete loss of the ability to eat naturally.
- Loss of speech.
- Nystagmus. Horizontal voluntary eye movements. Not controlled by the patient.
Visual impairment
Complete blindness occurs extremely rarely. More often there is a unilateral decrease in visual acuity. Up to monocular blindness (in one eye). An early, almost obligatory symptom is the formation of a scotoma in the field of view. This is a blind, black spot that reduces the field of view. In the focal, cerebral form, complete loss of vision is likely.
Main symptoms of multiple sclerosis
In addition to the described manifestations, regular headaches (for no apparent reason) are possible. Increased body temperature to mild subfebrile levels (up to 37.8 ° C).
The symptoms of multiple sclerosis are defined by a heterogeneous group of neurological manifestations. They are easy to detect, but determining the root cause is much more difficult.
Sexual dysfunction is also detected. It manifests itself as impotence, anorgasmia. Unsteadiness of gait, insomnia.
Indications for use of piracetam
is a popular drug that allows many patients to recover from serious illnesses (
). In many cases, it makes it possible for people in old age to maintain good intellectual and physical shape. It is successfully used in various fields of medicine, as it is well tolerated and has virtually no contraindications.
- in elderly patients, with memory loss, decreased concentration, decreased general activity, mood changes, behavioral disorders, gait disturbance;
- for Alzheimer's disease;
- with dementia - acquired dementia, with the collapse of mental functions caused by brain damage (dementia can be vascular, senile, atrophic, as in Alzheimer's disease);
- in the recovery period after an ischemic stroke (acute cerebrovascular accident) with disturbances in speech, emotional sphere, motor and mental activity;
- for chronic alcoholism (for the treatment of psychoorganic and withdrawal syndromes);
- in the recovery period after a coma;
- after brain injuries;
- after brain intoxication;
- for dizziness and balance disorders;
- with nystagmus (involuntary oscillatory eye movements);
- with cortical myoclonus (involuntary and unexpected muscle twitching);
- for sickle cell anemia as part of complex therapy (a hereditary blood disease that changes the shape of red blood cells);
- for dyslexia in children as part of complex therapy (difficulties in mastering reading and writing skills in children) and for other pathologies.
This drug is used as part of complex treatment for a large number of neurological diseases. Improving blood supply, microcirculation and metabolic processes in brain cells and the central nervous system (
), this medicine treats and restores impaired functions of the nervous system and brain associated with
, ischemia, toxic, traumatic and other effects on nerve cells.
A stroke is an acute disease in which the blood supply to any part of the brain is disrupted, resulting in nerve cells being damaged or dying. As a result, a person’s functions for which this part of the brain is responsible are disrupted. A person who has had a stroke may experience
) or
) in any part of the body, loss of speech, memory and other disorders. The larger the area of brain death, the more serious the consequences of a stroke.
Types of stroke are:
- Ischemic stroke. It occurs due to thrombosis of blood vessels (blood clots, cholesterol plaques) supplying blood to the brain, as a result of which the nerve cells in it are damaged or die. This is the most common form of stroke.
- Hemorrhagic stroke. Hemorrhagic stroke is bleeding in the brain. It occurs due to a rupture of a blood vessel in the brain. In this case, blood begins to leak and accumulate in the brain tissue, putting pressure on it and disrupting its normal functioning. It occurs much less frequently than ischemic stroke, but is more dangerous.
- Age over 40 years. Nowadays, stroke is no longer a disease of old people.
- Arterial hypertension (high blood pressure). With this pathology, the risk of cerebral vascular rupture increases.
- Heart disease: Arrhythmias can cause blood clots, increasing the risk of stroke.
- Increased cholesterol levels. Cholesterol plaques can clog blood vessels and cause stroke.
- Diabetes. This disease causes blood vessels to become brittle, which increases the risk of rupture.
- Aneurysms of cerebral vessels. These vascular formations can rupture and cause hemorrhagic stroke.
- Blood clotting disorder. Changes in blood composition can cause the formation of clots, which can clog blood vessels and cause a stroke.
- Obesity and poor nutrition. Obesity causes increased cholesterol levels in the blood.
- Smoking, alcohol abuse. These bad habits impair vascular health, increase blood pressure and increase the risk of stroke.
The chances of returning to a full life after a stroke depend on the extent of brain damage, the speed of delivery of the patient to the hospital, the quality of first aid provided, and the correctness of recovery procedures (
). Medical treatment of this disease includes the use of many drugs. These include neuroprotectors and neuroreparants that protect healthy nerve cells, restore the functioning of damaged cells and prevent the development of stroke. These drugs include piracetam and others
Various medications, including piracetam, can be taken to prevent stroke in healthy people. However, the most important preventive factor is a correct and healthy lifestyle, which involves giving up bad habits and junk food, exercising, and eliminating excessive emotional, mental, physical stress and stress.
Atherosclerosis is a common chronic disease that affects blood vessels. Atherosclerosis affects the arteries
, brain and other organs. With this pathology, cholesterol deposits form on the inner surface of blood vessels (
), with the subsequent growth of connective tissue in them (
) and impregnation with calcium salts (
). The consequences of this pathological process are increasing insufficiency of blood supply to the organ or part of the body supplied by this artery. It is also possible to completely block the lumen of the vessel with a plaque or thrombus, which leads to a heart attack (
) fabrics or
organ or body part.
People over 50–60 years of age are most susceptible to atherosclerosis. Its causes are stress, causing hypertension, which, in turn, negatively affects arterial tone, diabetes, obesity, inactive lifestyle, and bad habits. The first symptoms of cerebral atherosclerosis (ischemia - insufficient blood circulation and nutrition of brain cells) are periodic headaches, tinnitus, especially during periods of intense mental work, memory impairment for current events, sleep disturbances, suspiciousness, tearfulness, a tendency to depression, long-term experience of failures or insults.
It should be noted that atherosclerosis can be completely cured in the early stages of its development. However, in the advanced stage, it causes temporary (transient) strokes with transient paresthesias (impaired skin sensitivity), impaired tone of skeletal and facial muscles, unilateral distortion of the face due to loss of muscle tone, impaired coordination of movements, weakened movements and trembling of the limbs and head, especially when excitement.
Treatment for this disease is complex, it includes medication, physical therapy, a healthy and moderate diet, minimizing stress, quitting smoking and alcohol abuse, and other measures. In severe, threatening cases, surgical treatment of this pathology cannot be ruled out. Drug therapy for atherosclerosis includes the prescription of statins, fibrates, nicotinic acid preparations, drugs based on omega-3-triglycerides, bile acid sequestrants and other drugs.
Encephalopathy is damage to the brain and disruption of its functions that occurs in various diseases that are not associated with inflammatory processes.
The causes of encephalopathy may be:
- traumatic brain injury;
- impaired blood circulation in the brain (with hypertension, previous strokes, osteochondrosis of the cervical spine and others);
- poisoning (alcohol, drugs, poisoning with various poisons and toxic substances);
- addiction;
- liver disease (cirrhosis);
- renal failure;
- diabetes;
- irradiation;
- congenital encephalopathy in a newborn child can develop due to diseases of the woman during pregnancy, intrauterine hypoxia, birth injuries and other factors.
The manifestations of this disease may vary depending on the cause that causes it. However, its common symptoms are impaired attention and memory, headaches, dizziness, bad mood, and a tendency to depression. Treatment of this disease is complex, first of all, it is aimed at treating the disease - the cause of encephalopathy.
The therapy also uses drugs that improve blood circulation, metabolism and the function of the nervous tissue of the brain. These include piracetam and other nootropics. With proper and timely treatment of this disease, its complete cure is possible. However, more often it becomes chronic, and in especially severe cases it can even cause the death of the patient.
A panic attack is a complex of symptoms that occurs in patients with vegetative-vascular dystonia (
), in which inexplicable anxiety and panic suddenly develop, blood pressure may rise, the pulse may increase, a feeling of heat, trembling, and fainting may occur. Most often, this pathology occurs in women and people prone to depression,
. There are several forms of panic attacks - sympathoadrenal (
) or vagoinsular (
Symptoms of Multiple Sclerosis
The process of nerve impulse transmission is disrupted when the myelin sheath of the nerve is lost. Massive demyelination is detected with damage to the axial cylinders and the formation of pink-gray sclerotic plaques, foci of proliferation and necrosis. It is the defeat of the axial cylinders that ensures the irreversibility of the neurological defect. Demyelination can occur anywhere, the conduction of nerve impulses is disrupted and various neurological disorders occur.
In multiple sclerosis, exacerbations are followed by periods of remission. In the initial stages, during remyelination, neurological symptoms may disappear or decrease; with exacerbation, that is, new demyelination, they may worsen or a new one may arise, depending on the functional significance of the affected area of the nervous system. Foci of demyelination are “scattered” throughout the nervous system and are multiple in nature.
And the same many-sided symptoms of the disease. Depending on the area of localization of the lesion, a corresponding neurological defect occurs.
The range of symptoms of multiple sclerosis is quite wide: from mild numbness in the arm or staggering when walking to enuresis, paralysis, blindness and difficulty breathing. It happens that after the first exacerbation the disease does not manifest itself in any way for the next 10, or even 20 years, the person feels completely healthy. But the disease subsequently takes its toll, and an exacerbation occurs again.
More often, the symptoms are dominated by motor disorders - paresis, paralysis, increased muscle tone, hyperkinesis, visual disturbances. Violations may initially be transient, that is, appear and disappear.
During examination, a neurologist may detect nystagmus, double vision, increased tendon reflexes, anisoreflexia, loss of abdominal reflexes, pathological signs, coordination disorders - statics and dynamics, dysfunction of the pelvic organs - urinary retention and incontinence, disorders of the cranial nerves, symptoms of vegetative-vascular dystonia , mental disorders - neurosis-like symptoms, asthenia, euphoria, uncriticality, depression, sensory disorders, decreased vibration sensitivity. Moreover, all of the above can be in any combination and as a mono symptom.
According to the degree of severity, multiple sclerosis is divided into: mild - relapsing-remitting (with rare exacerbations and long-term remissions), moderate - remitting-progressive, severe - progressive (primary, secondary). Forms of multiple sclerosis, depending on the predominant symptoms - cerebral, spinal, cerebrospinal, ocular, hyperkinetic, atypical.
Any disease can provoke an exacerbation, even ARVI, hypothermia and overheating, insolation, neuro-emotional overload.