Radicular syndrome is caused by compression (compression) of the spinal nerve as it exits the bony canal of the spine.
Along the entire length of the spinal cord, branches of nerves depart from it, which innervate various organs. The base of these nerves is called the root or in Latin – radix. Therefore, other names for radicular syndrome are radiculopathy, radiculitis.
How are spinal nerves formed?
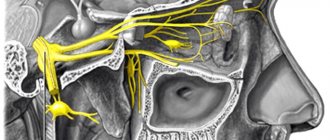
The spinal nerve is formed by two roots that arise from the spinal cord. The roots consist of neurons (nerve cells) of different types. One root is formed by sensory neurons (sensory or afferent), the second - by motor neurons (motor, efferent). Therefore, the spinal nerve is of a mixed type.
Spinal nerves leave the spinal cord through the bony canal of the corresponding vertebra. Located between adjacent vertebrae. When leaving the spine, they are divided into two branches: anterior and posterior. The posterior branches innervate the back muscles and spine. The anterior ones, intertwining with each other, form nerve plexuses and then go to the corresponding organs and tissues of the body.
There are a total of 31 pairs of spinal nerves. These include:
- Eight neck ones. Innervates the corresponding segments of the cervical spine - C1, C2...C8.
- Twelve chest (T1…T12).
- Five lumbar (L1…L5).
- Five sacral (S1…S5).
- One coccygeal nerve (Co1).
Each spinal nerve is accompanied by vessels (artery and vein), providing it with nutrition and oxygen enrichment.
How does radicular syndrome occur?
In various pathological processes of the spine, compression (squeezing) and/or inflammation of the spinal nerve roots may occur, which leads to the development of the disease. Such pathological processes can be:
- Osteochondrosis.
- Spinal cord herniation.
- Deforming spondyloarthrosis.
- Bruise and other vertebral injuries.
- Osteoporosis and its complications (fractures).
- Spinal cord tumors (neurinomas).
- Infectious process in the vertebrae (osteomyelitis, tuberculosis, syphilis) and other causes.
Whatever the causes of radicular syndrome, the essence of the syndrome is the same - trauma to the spinal nerve.
Diagnostic measures
In order to make an accurate diagnosis and assess the degree of tissue destruction, it is necessary to properly carry out diagnostic measures. The following methods and studies are relevant:
- X-ray of the spinal column in frontal and lateral projection. Allows you to identify possible curvatures, relief defects, and damage to bone structures. An X-ray image can indirectly determine whether there is destruction in the tissues of the intervertebral discs;
- Tomography of the spine (CT and MRI). A high-precision diagnostic technique allows you to examine soft and hard tissues in great detail for inflammation, growths, protrusions, destruction and degenerative phenomena;
- Myelography. This is a type of radiography. The spinal cord and nerve roots are subject to examination. A contrast agent is injected into the subarachnoid space. It allows you to determine the degree of tissue integrity.
What happens with osteochondrosis?
Osteochondrosis is the most common cause of radicular syndrome. With this disease, there is a narrowing of the bone canals in which the spinal nerves pass. It is also possible that the nerve can be injured by other complications of osteochondrosis: intervertebral hernia, osteophytes (bone growths), etc.
Radicular syndrome in osteochondrosis develops over several years as the pathological process in the spine progresses.
Most often, radiculopathy occurs with lumbar osteochondrosis. In second place is the thoracic region. The cervical and coccygeal regions are least commonly affected. This feature is directly related to the difference in the structure of the vertebrae.
Features of the structure of the vertebrae and the connection with radiculopathy
The frequency of development and intensity of manifestations of radicular syndrome directly depends on the structure of the vertebrae in different parts of the spine:
- The cervical vertebrae, compared to other vertebrae, have the strongest intervertebral ligaments. The intervertebral foramina in the cervical vertebrae are small. This feature significantly reduces the risk of hernial protrusions passing through them. Radicular syndrome in the cervical vertebrae appears mainly due to the involvement (ischemia) of the vessels accompanying the nerve. As a result, there is a disruption in the nutrition and oxygen supply of this nerve.
- Thoracic and lumbar vertebrae. The thoracic, and even more so the lumbar spine bears the main load. The intervertebral ligaments here are relatively weaker than the cervical ligaments. And the openings for the exit of blood vessels and nerves are larger. Therefore, hernias and other pathological formations are more likely to form in these sections, causing compression of the neurovascular bundles.
Causes of pathology
The main causes of the disorder are degenerative changes in the vertebrae and herniated disc. Usually, people with this pathology immediately consult a doctor, because the pain affects the organs near the lesion, develops sharply, and intensifies significantly with any movement.
Pathology in the thoracic spine occurs much more often than in the neck. This can be explained by the peculiarities of the anatomical structure of the spine.
Radiculitis can be triggered by the following factors and diseases:
- osteochondrosis;
- stress and nervous tension;
- degenerative changes in joints;
- syphilis;
- herpes zoster;
- tuberculosis;
- herniation of intervertebral discs of the sacral, cervical, thoracic, lumbar region.
Manifestations of radicular syndrome
The main symptoms of radiculopathy are pain, loss of sensation and movement. Let's look at these manifestations in more detail.
- Pain is the main symptom of radiculopathy in spinal osteochondrosis. Occurs along the affected spinal nerve. It can be constant or in the form of attacks - “lumbago”. The nature of the pain is very different. The pain is characterized as dull or aching, sharp or burning. The pain usually worsens with movement. The time of day also affects the occurrence of pain; it usually worsens at night.
- Impaired sensitivity. Painful sensations are usually always accompanied by a loss of sensitivity in the affected area. This may manifest itself as a feeling of numbness, "crawling." A decrease in the pain threshold often develops: when tingling with a needle, perception is reduced compared to a healthy area of the body.
- Motor disorders. A common symptom of radiculopathy is weakness in the muscles of the affected area. This symptom is especially pronounced on the upper or lower extremities.
- With a long-term pathological process, muscle atrophy develops - the muscles “shrink” and gradually lose their functions.
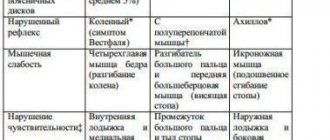
Symptoms of radiculopathy and their relationship with the localization of osteochondrosis
Manifestations of radicular syndrome directly depend on the location of the pathological focus of osteochondrosis in the spinal column. Now we will briefly look at the main symptoms.
Neck department
When the first two cervical roots (C1-C2) are affected, a headache occurs in the area of the crown and back of the head. Numbness of these areas is often observed, and the tone of the mental muscles decreases.
If there is a violation in C3, pain and a feeling of numbness in the neck appear. Numbness of part of the tongue may occur, which is accompanied by speech impairment.
A C4 lesion is characterized by pain and numbness in the shoulder girdle and scapula area. Muscle weakness develops in the scapular and cervical region.
Starting from C5, when the cervical spine is affected, symptoms of damage to the upper limb appear.
In addition to pain and numbness in the cervical and scapular areas when, for example, C5 is affected, the same symptoms appear in the projection of the shoulder joint. When C6-C7-C8 is affected, pain and numbness spread along the surface of the shoulder and forearm, reaching the fingers. In all cases, weakness of the muscles of the upper limb is observed.
Thoracic region
Pain when this section is affected often increases with breathing, sneezing, hiccups, and coughing.
When the first root of this section (T1) is affected, pain and numbness are directed from the scapula area to the armpit and further along the entire inner surface of the upper limb. Pain and discomfort may be felt in the pharyngeal area.
In localization T2 - T6, pain and numbness appear along the spine, as well as behind and in front in the projection of the ribs to the lowest edge of the sternum. That is, the pain has a character that encircles the chest. Muscle weakness appears in the scapular region. Often there is pain and an unpleasant sensation of a foreign body in the pharynx, esophagus or stomach.
With damage to T7 - T8, pain and numbness are also characterized by a shingles character. Such symptoms appear from the projection of the shoulder blades and to the lower edge of the ribs in the back, and in front to the epigastric region (epigastric region). Pain and discomfort in the heart area and behind the sternum are common.
Such patients quite often turn to a cardiologist with these complaints, without suspecting that they have a spinal disease.
Lesion T9 - T12 manifests itself with pain and numbness in the lower part of the body: from the lower edge of the ribs to the navel, and sometimes lower to the groin area (T12). Abdominal tone decreases. Abdominal pain often appears. This forces patients to seek initial help from a gastroenterologist.
Lumbar department
When the roots of the lumbar nerves are damaged, pain and sensory disturbances appear in the pelvis and lower extremities.
When the lesion is localized in the first three lumbar roots (L1-L3), pain and numbness appear in the lower back and abdomen and on the hips. Also, these sensations often occur in the groin area and external genitalia.
When L4 is affected, pain and a feeling of numbness are directed from the lower back and lower abdomen along the thigh to the knee, and sometimes to the lower leg. Muscle weakness appears when moving the limb in the knee joint. Sometimes some thigh muscles, such as the quadriceps, atrophy. At the same time, the thigh visually decreases in size and volume.
If the L5 root is involved in the pathological process, then pain and sensory disturbances spread to the entire lower limb and reach the foot. Weakness of the foot muscles occurs. Often the patient cannot stand on the affected lower limb.
Diagnostics
In the diagnosis of radicular syndrome in osteochondrosis, an important role is played by collecting anamnesis and examination. Usually, based on these data, a disease can be suspected.
Additional research methods are used:
- radiography of the spine;
- magnetic resonance imaging (MRI).
These methods make it possible to more accurately determine the degree and location of spinal damage in osteochondrosis.
Treatment
The patient is indicated for immobilization of the spine - lying in a lying position on a hard bed. In the absence of inflammation, you can get rid of pinching using dry heat: a heating pad, a bag of hot salt, warming ointments (Capsicam, Viprosal, Finalgon), pepper plaster, mustard plasters.
Treatment regimens include physiotherapeutic procedures - phonophoresis, electrophoresis, shock wave therapy, magnetic therapy. As prescribed by a vertebrologist or neurologist, “dry” or underwater traction of the spine can be performed.
In case of acute pain that cannot be eliminated by drugs, which lasts 3-4 months, the patient is prepared for surgery - removal of the intervertebral hernia.
| Drugs for the treatment of osteochondrosis with radicular syndrome | Therapeutic effect |
| Non-steroidal anti-inflammatory drugs - Diclofenac, Nimesulide, Meloxicam, Ketoprofen, Ibuprofen | Reducing the severity of pain and swelling, relieving inflammation |
| Muscle relaxants - Sirdalud, Mydocalm, Baklosan, Tolperisone | Relaxation of spasmodic skeletal muscles, elimination of pinching |
| Products with B vitamins - Milgamma, Kombilipen, Neuromultivit | Improvement of trophism of damaged tissues, normalization of innervation |
If you consult a doctor in a timely manner, the prognosis is favorable. A comprehensive treatment will be carried out using all healing techniques. This approach eliminates the development of irreversible complications and the occurrence of painful relapses.
How is radiculopathy treated?
Treatment of manifestations of radicular syndrome is complex and is aimed mainly at eliminating the symptoms of the main disease – spinal osteochondrosis.
For this purpose the following are used:
- medications;
- physical therapy;
- massage and manual therapy;
- exercise therapy;
- reflexology and other treatment methods.
Sometimes surgical treatment is also performed. It is indicated, for example, in the presence of a hernia in the vertebral area.
In the acute phase of radicular syndrome, it is important to adhere to bed rest.