If the reader is looking for information about exacerbation of a herniated cervical spine, then two important conclusions can be drawn from this. First: most likely, the reader was diagnosed with a “cervical hernia” not now, but in the past. For example, the symptoms of a newly diagnosed hernia were treated conservatively, but now an exacerbation has occurred again, as with any other chronic disease. The second conclusion is the fact that for some reason the reader either refused surgical treatment, or there were no indications for surgery to remove a hernia of the cervical spine.
Cervical hernia on MRI.
Both facts indicate that in the neck there is a chronic source of inflammation and a source of pain impulses associated with a defect in the cartilage disc between the vertebrae. Let's consider how dangerous periodic exacerbation of hernias or protrusions is, how they manifest themselves, how they should be treated, and what the risk is from their periodic exacerbation. We should start with the causes of hernias of the cervical spine and their exacerbations in order to avoid these exacerbations in the future. But at the very beginning, let's look at the stages of cervical disc pathology.
Causes of brain herniation
A brain herniation is usually the result of a swelling in the brain. The swelling puts pressure on the brain tissue (called increased intracranial pressure), causing the tissue to be pulled away from its normal position.
The most common causes of brain herniation are:
- head injury resulting in a subdural hematoma (when blood collects on the surface of the brain under the skull) or swelling (cerebral edema)
- cerebral hemorrhage
- (bleeding in the brain)
- a brain tumor
Other causes of increased pressure in the skull include:
- an abscess (collection of pus) from a bacterial or fungal infection
- accumulation of fluid in the brain (hydrocephalus)
- brain surgery
- a defect in the structure of the brain called a Chiari malformation
People with brain tumors or blood vessel problems, such as an aneurysm, are at higher risk of developing a brain herniation. Additionally, any activity or lifestyle choice that puts you at risk for a head injury can also increase your risk of a brain herniation.
Risk factors for exacerbation
The most important factors for the formation of exacerbations of protrusions and hernias of the cervical spine are the following factors:
- Poor posture, stooping, flat feet or wearing the wrong shoes.
Despite the fact that the spine has powerful mechanisms for compensating for concussions during walking and running, all uncompensated concussions are transmitted upward, amplifying according to the “whiplash” principle, when the greatest amplitude and traumatic potential occurs at a far distance from the source of vibration.
Therefore, with poor posture and dehydration of the intervertebral discs, the risk of destruction occurs primarily in the cervical region;
- An important factor in the formation of chronic pain is the constant tonic tension of the deep muscles of the neck and back, the occurrence of muscle spasm and protective posture.
A large load on the head and neck muscles, associated with high women's hairstyles, heavy winter fur hats, leads to stagnation of blood in the neck muscles, deterioration of nutrition of the intervertebral discs and their dehydration;
- with age, with the onset and progression of symptoms of osteochondrosis, with the appearance of osteophytes on the vertebrae, blood circulation worsens, and, as a result, muscle spasm and limitation of neck movement again.
Therefore, with a rapid increase in pressure on the edge of the vertebral body, it is transferred to the disc. Uneven, eccentric and undistributed pressure causes the disc to collapse. Either a protrusion or a hernia occurs immediately. What symptoms will manifest protrusion and hernia in the cervical spine when it occurs or worsens?
Treatment of brain herniation
Treatment is aimed at relieving swelling and pressure inside the brain, which causes the brain to be chewed from one compartment to another. Treatment will be necessary to save the person's life.
To reduce swelling and pressure, treatment may include:
- surgery to remove a tumor, hematoma (blood clot), or abscess
- to remove a drain, called a ventriculostomy, through an opening in the skull to get rid of fluids
- osmotic therapy or diuretics (medicines that remove fluid from the body) to draw fluid out of brain tissue, such as mannitol or hypertonic saline
- to reduce swelling
- surgery to remove part of the skull to make more room (craniectomy)
While the cause of the brain herniation is being addressed, the person being treated may also get:
- oxygen
- a tube placed in their airway to support breathing
- sedation
- medications to combat seizures
- antibiotics to treat an abscess or to prevent infection
In addition, a person with a brain herniation will need close monitoring with tests such as:
- X-ray of the skull and neck
- CT scan
- MRI scan
- blood tests
AdvertisingAdvertise
Which doctors can help?
The choice of doctor's specialization depends on the clinical picture formed during the disease. So, these are mainly therapeutic doctors: neurologist, phlebologist, cardiologist. These are also surgeons, for example, an angiologist. These doctors study the clinical signs of vascular diseases, diagnose them, and treat them.
However, in order for the attending physician to cure, the cause of the pathology must first be identified. Which doctor checks blood vessels? Diagnostics can be prescribed by any clinical specialist who needs data on the functioning of cerebral vessels. The vessels are directly checked by a radiation or functional diagnostics doctor who examines the arteries and veins using ultrasound or magnetic resonance imaging using angiography.
Neurologist
A neurologist is a specialist in the field of neurology. He studies diseases associated with the pathology of the entire nervous system (central and peripheral).
You should contact a neurologist if there are signs of neurological diseases, the cause of which lies in the blood vessels. These are the following signs:
- Often headaches occur with high blood pressure.
- Mental activity decreased, attention became distracted, and it became more difficult to remember. It is difficult to control emotions, my sleep is upset.
- Asthenic syndrome: painful fatigue, rapid exhaustion from simple work, impatience, restlessness, intolerance to sound, light and smell, irritability, emotional lability. What is the clinical picture, for example, of multiple sclerosis.
- Increased intracranial pressure: headaches, dizziness, nausea, vomiting, painful urination and coughing, decreased visual acuity.
- Signs of ischemic and hemorrhagic strokes: impaired consciousness, headache like a blow to the back of the head, frustrated speech, blurred vision, loss of sensitivity, partial or complete lack of muscle strength in the arms or legs.
The clinical picture of neurological diseases of vascular origin may be accompanied by mental disorders. In this case, a head doctor – a psychiatrist – gets involved. Occurs in cerebral atherosclerosis. Signs: memory loss, amnesia, disorientation, muscle rigidity, loss of motivation for any activity.
Phlebologist
A phlebologist deals with vein diseases. Brain pathology associated with disruption of these vessels is called “venous encephalopathy.” The basis of the disease is the difficulty of the outflow of venous blood from the vessels of the brain due to cardiovascular diseases, diseases of the lungs and respiratory tract, blockage of the lumen by a tumor or hydrocephalus.
You can contact a phlebologist if you often have a headache. Periodic cephalgia with venous encephalopathy has the following characteristics:
- in terms of severity and subjective sensations, light or medium;
- the pain is aching, bursting and monotonous;
- usually symmetrical, less often localized in the occiput and parietal region;
- it hurts more in the morning than in the evening;
- the pain intensifies when tilting the head down, drinking alcohol, smoking, drinking coffee and strong tea.
With venous encephalopathy, the face usually acquires a bluish tint, lips, nose, and ears are cyanotic. In the morning there is swelling of soft tissues, mainly in the area under the eyes. You can also externally see an enlargement of the saphenous veins of the neck.
Cardiologist
A cardiologist studies the signs and treats diseases of the cardiovascular system. This specialist does not directly treat cerebral vessels, however, due to the close connection of the cardiovascular system with the performance of the central nervous system, a cardiologist can influence the dynamics of pathologies of arteries and veins, and prevent complications, because the brain is the target organ for hypertension .
The functionality of the brain is determined by blood pressure, a disease that is dealt with by a cardiologist. You should contact him if cardiac signs appear at a pressure above 140/90: cardiac pain, rhythm disturbances, heaviness in the chest.
A cardiologist can prevent or treat a hypertensive crisis. This is a condition in which high blood pressure increases the risk of vascular pathologies of the brain, for example, ischemic stroke or transient ischemic attack.
Arterial hypertension is often asymptomatic, but with the cerebral version of a hypertensive crisis the following symptoms appear:
- constant headache;
- spots before the eyes;
- vomit;
- chills, trembling in the limbs, sweating, palpitations;
- pale face;
- muscle weakness;
- mental agitation or vice versa, apathy and indifference.
Hypertensive encephalopathy against a background of constantly elevated blood pressure leads to neurological and mental disorders, for example, unsteadiness of walking, uncontrollable laughter and crying, decreased intelligence and memory, emotional disturbances or trembling of the fingers.
Which doctor should you contact if you have arterial hypertension and heart symptoms? A cardiologist. If arterial hypertension is accompanied by brain disorders, you should consult a neurologist.
Angiologist
An angiologist is a specialist who studies and treats diseases of the vascular and lymphatic systems. Angiologist is a conventional term, since formally this kind of specialist does not exist in developed countries of the world.
When talking about angiologists, we usually mean vascular surgeons. A doctor who treats surgical pathologies of cerebral vessels through surgery is called an endovascular neurosurgeon.
This doctor treats the head if vascular pathologies have arisen that can only be eliminated surgically:
- Cerebral aneurysm. You should consult a doctor if you have the following symptoms: headache in the frontal region, decreased intelligence, emotional lability, impaired sensitivity, decreased muscle strength.
- Arteriovenous malformation. It manifests itself as seizures, cluster headaches and focal deficit neurological symptoms, for example, loss of visual fields or speech disorders.
- Arteriovenous fistula. It manifests itself as headache, pulsating tinnitus, decreased vision, difficulty moving the eyes, dizziness, nausea and vomiting.
- Thrombosis of cerebral vessels. The symptoms are the same as the clinical picture of ischemic stroke.
Prospects for brain herniation
The outlook depends on the type and severity of the injury caused by the herniation and where in the brain the herniation occurs. A brain herniation can cut off the blood supply to the brain. For this reason, it is likely to be fatal if not treated promptly. Even with treatment, a brain herniation can lead to serious, permanent brain problems or death.
A brain herniation is considered a medical emergency. You should call 911 or go to the emergency room immediately if a person with a head injury or brain tumor becomes less anxious or disoriented, has a seizure, or becomes unconscious.
Spina bifida is a pathological condition in which the patient experiences a protrusion of the contents of the spinal canal through a defect in the arches or vertebral bodies.
This is a congenital pathology, a rather rare developmental defect. According to research, the anomaly is detected in approximately 0.1% of newborns (a latent form is observed in 15% of the population), in some of whom the disease becomes a cause of disability. May be combined with other developmental anomalies.
What it is?
Concussion is damage to the bones of the skull or soft tissues, such as brain tissue, blood vessels, nerves, and meninges. An accident can happen to a person in which he can hit his head on a hard surface, this is precisely what entails such a thing as a concussion. In this case, some disturbances in brain function occur that do not lead to irreversible consequences.
As already mentioned, a concussion can be caused by a fall, a blow to the head or neck, or a sudden slowdown in head movement in the following situations:
- at home;
- in production;
- in a children's group;
- when practicing in sports sections;
- in case of traffic accidents;
- in domestic conflicts with assault;
- in military conflicts;
- with barotrauma;
- for injuries with rotation (turning) of the head.
As a result of a head injury, the brain changes its location for a short time and returns to it almost immediately. In this case, the mechanism of inertia and the peculiarities of fixation of brain structures in the cranium come into force - not keeping up with the sudden movement, some of the nerve processes can stretch and lose connection with other cells.
The pressure in different parts of the skull changes, and the blood supply, and therefore the nutrition of nerve cells, may be temporarily disrupted. An important fact about concussion is that all changes are reversible. There are no ruptures, hemorrhages, or swelling.
Causes
The reasons for the development of pathology are not fully understood. The main factors contributing to the occurrence of spina bifida include:
- lack of vitamins (especially folic acid) in a woman’s body before and during pregnancy;
- genetic predisposition;
- pregnancy at an early age;
- abuse of alcohol and/or drugs by a woman during pregnancy;
- intoxication of the body;
- infectious diseases in the expectant mother.
In adult patients, existing pathology may manifest itself under the influence of the following provoking factors:
- lack of timely treatment of osteochondrosis;
- spinal injury;
- lifting weights;
- staying in an uncomfortable position for a long time (for example, while working);
- strength sports;
- metabolic disorders (overweight);
- incorrect posture;
- infectious diseases.
Depending on the location, hernias of the following parts of the spine are distinguished:
- cervical;
- chest;
- lumbosacral (the most common option).
Based on the contents of the hernial sac, pathology is divided into several groups, which are presented in the table.
The spinal cord is correctly formed and functions normally; only the spinal membrane penetrates into the intervertebral defect
There is protrusion of the meninges and substance of the spinal cord, neurological symptoms develop
There is protrusion of the meninges and spinal roots
The most dangerous form; the hernial sac consists of cerebrospinal fluid accumulated in the expanded central canal of the spinal cord, which is surrounded by the thinned substance of the spinal cord, its membranes and the dorsal roots of the spinal nerves
Forms
- Depending on the location of the hernia, the following forms are distinguished. Occipital : The hernia is located at the back of the head.
- Hernia of the calvarium : interfrontal - the hernia is located on the forehead;
- interparietal - the hernia is located on the crown;
- temporal - the hernia is located in the temple area.
- meningocele - in the hernial sac (protrusion, the walls of which are formed by the skin and membranes of the brain) only the membranes of the brain are located;
Symptoms
The course of the disease depends on the degree of damage to the spinal column and the volume of tissue that forms the hernial sac.
The mildest type of pathology is spina bifida. This reveals a slight deformation of one of the vertebrae, which, as a rule, does not cause much discomfort in a person. This form of pathology is often asymptomatic, but such patients may also show signs of prolapse; in some cases, neurological symptoms occur with this form of the disease. In some patients, clinical signs of pathology may appear in adulthood due to intense physical activity or other reasons.
A more serious defect occurs with spina bifida, in which a protrusion consisting of fluid and meninges is visually noticeable. In the most severe cases, the nerve roots and spinal cord are involved in the pathological process.
The photo shows that spina bifida is visualized as a round protrusion in the spine. On palpation it has a soft consistency. The skin over the formation is usually shiny and thinned, with a reddish or cyanotic tint.
The patient may complain about:
- weakness in the upper and lower extremities;
- violation of all types of sensitivity (temperature, tactile, pain);
- dry skin;
- non-healing ulcerations;
- coldness of the extremities.
- decreased limb reflexes (knee, plantar, grasping);
- atrophy of the muscles of the arms and legs;
- various forms of deformation of the lower extremities (clubfoot is often detected).
Symptoms also depend on the area in which the hernia developed.
The pathology affects the upper part of the spinal cord, which leads to a decrease in motor activity of the upper and lower extremities. The patient may also experience problems with the heart and lungs.
Disorders of the respiratory system, heart, stomach, liver, spleen.
Disturbances in the functioning of the organs of the genitourinary system, gastrointestinal tract, and lower extremities. Patients may experience problems with urination and defecation (including urinary and fecal incontinence).
Definition of pathology
Dislocation syndrome is the process of moving a fragment of brain tissue relative to other structural elements of the skull and brain. The skull is the hard part of the head. As the volume of the contents of the cranium increases, nerve tissue may bulge through the natural openings at its base. Supporting partitions that divide the contents of the skull into sections limit the possibilities of compensation for pathological displacement of brain fragments.
The brain inside the cranium does not occupy the entire volume. Between the medulla and the arachnoid membrane is the subarachnoid space. In areas of expansion of the subarachnoid space, subarachnoid cisterns are formed. As a result of various pathological processes, areas of distension (pressure) may appear in certain parts of the brain, which provokes a displacement of brain structures.
Pathological processes differ in etiology, but they cause the same shift in brain regions. Dislocation syndrome of brain structures manifests itself with the same type of clinical picture. Symptoms when there is a shift in parts of the brain do not depend on the nature of the pathological process, but depend on the localization of the lesion, the rate of development of the disorders and the volume of the structures involved. Dislocation syndromes are protrusions of the brain matter into the natural openings of the skull and open spaces of the dura mater.
Possible complications
- Pyelonephritis, renal failure due to urinary disorders.
- Increased intracranial pressure due to fluid retention in the brain, which can lead to atrophy of areas of nervous tissue, the development of meningitis, and encephalitis.
- Flexion contractures, paresis, paralysis.
- Infertility, erectile dysfunction in men.
- Pinched nerves, which leads to severe pain, decreased sensitivity, and decreased motor activity.
- Hydrocephalus.
- Decreased cognitive abilities.
- Vision disorders.
- Congestive pneumonia and pulmonary failure as a consequence of prolonged bed rest.
- Diseases of internal organs.
- Disability. In severe cases, the patient needs constant care at home, supportive treatment, and regular medical monitoring.
Postoperative therapy
To undergo such an operation, any baby will require a long rehabilitation period. A newborn needs careful care, maintaining impeccable hygiene, therapeutic massages, physiotherapy, gymnastics and prevention of constipation. The list of conservative measures also includes the prevention of bedsores, training of the sphincters of the bladder and anus, treatment of spinal deformities and correction with support corsets.
Typically, recovery from spina bifida occurs in one of two ways:
- After removal of the meningocele and all required rehabilitation procedures, the child’s development continues normally. In most cases, such children grow up capable of leading an active lifestyle.
- Repairing hernia meningomyelocele, meningoradiculocele and meningocystocele can cause certain difficulties, both during and after surgery. Proper compliance with the requirements of the rehabilitation period helps to avoid disturbances in the motor activity of the limbs, but one cannot expect the same from the functions of the pelvic organs. Urinary and fecal incontinence may persist much longer than in normal children. In adulthood, even with the preservation of external signs of health, infertility is found in women, and erectile dysfunction in men.
Read more: Erectile dysfunction in men
Diagnostics
Modern diagnostic methods make it possible to detect fetal pathology even during intrauterine development. This usually occurs during a screening ultrasound examination. In order to clarify the diagnosis, laboratory determination of alpha-fetoprotein levels and a number of other tests may be required.
In a latent form, the defect can be determined during diagnosis for another reason, as well as when determining the causes of back pain.
- collection of complaints and medical history, objective examination;
- neurological examination – allows you to assess motor activity, muscle tone of the upper and lower extremities;
- transillumination - a method that allows you to determine the nature of the contents of the hernial sac;
- computed tomography and magnetic resonance imaging - allow you to identify concomitant lesions of the tissues of the brain and spinal cord, as well as get a detailed picture of the hernia;
- laboratory tests: general and biochemical blood tests, general urine tests, etc.
How to recognize signs of a possible hernia
At the initial stages of the disease, the symptoms of a vertebral hernia may not be obvious: increased fatigue, weakness, an unreasonable slight increase in temperature, characteristic of sluggish inflammatory processes. Pain at an early stage of development may not be of a pronounced acute nature, especially with a sedentary lifestyle.
The symptoms of a vertebral hernia largely coincide with the symptoms of osteochondrosis and atherosclerosis. For an accurate diagnosis, it is necessary to conduct studies using technical means - X-rays, X-rays with a contrast agent, computed tomography and MRI of the spine. The technical diagnosis of intervertebral hernia is 100% accurate. In case of deviation, pinched nerve, ruptured intervertebral disc and other damage - all this will be displayed on the pictures.
The manual method for determining a vertebral hernia is not absolutely accurate and can be painful and even traumatic. The manual method is used mainly when it is impossible to carry out diagnostics using the appropriate equipment.
Signs of the development of the disease are quite obvious to the doctor. You cannot ignore severe pain in the back, a constant feeling of squeezing, numbness. Initial signs may be similar to heart problems, various nervous diseases and vascular problems. Without qualified diagnostics, you can confuse the signs of the disease and miss the moment for the most convenient start of treatment.
Call your doctor immediately for any severe pain in your spine. The first symptoms pass quickly, and people tend not to pay serious attention to them. The sooner you start treatment, the higher the likelihood of maintaining health.
Treatment
Typically, treatment of spina bifida involves its surgical removal, since conservative therapy, as a rule, is ineffective and is used only as an auxiliary one.
During the operation, the defect in the spine is reconstructed and the unclosed hole is closed. Non-viable structures are removed from the hernial sac, and healthy spinal cord tissue is returned to the spinal canal.
An operation to remove the hernial sac and eliminate a spinal defect can be carried out already in the first weeks of a child’s life. Surgical treatment is postponed if a mild form of pathology is detected (no need for surgery).
For hydrocephalus, a shunt may be placed to drain excess cerebrospinal fluid into the thoracic lymphatic duct.
After surgery, the patient requires rehabilitation, which allows:
- eliminate pain syndrome faster;
- prevent the development of possible complications (secondary infection, thrombosis, etc.);
- restore normal muscle tone;
- correct posture and gait disorders;
- improve general condition;
- minimize the risk of relapse.
In order to prevent the progression of the pathology, as well as to improve the general condition of the patient, he may be prescribed neurometabolic stimulants and vitamin therapy (vitamins A, E, C, group B). Physiotherapeutic techniques (magnetic therapy, laser therapy), therapeutic exercises can be used.
Patients with disorders of the digestive system require a diet. It is recommended to include more fiber-rich foods in your diet to normalize intestinal motility.
Cranial hernia (encephalocele, cephalocele)
Symptoms of cranial hernia:
- Visible soft protrusion on the head, face, nose.
- Difficulty in nasal breathing: the child breathes mainly through the mouth.
- Asymmetry of the eye sockets.
- Wide bridge of nose.
- Leakage of clear fluid (cerebrospinal fluid) from the nose.
- Child's anxiety: the child refuses to eat, sleeps poorly.
In less than 25% of cases, the hernia protrudes through the facial skeleton, usually in the forehead or between the eyes (both of these forms are called frontal hernias). If the encephalocele is located in the forehead, it can displace the eye sockets, causing patients to have wide-set eyes.
If the anomaly is located between the eyes, then an enlargement of the nasal bridge is observed, although sometimes such a hernia can only be noticed when examining the nasal passages, that is, the defect is completely invisible from the outside.
Often a hernia is mistaken for a nasal polyp, resulting in an incorrect diagnosis and a brain hernia remaining unrecognized. As a rule, an anterior cranial hernia entails external deformities, represented by a disgusting growth of a dense structure in the area of the nasolabial fold.
In addition, there is obvious facial asymmetry, that is, the distance between the patient’s eyeballs is noticeably distorted. There is also an equally eloquent symptom of fluctuation in the area of characteristic protrusion.
In the absence of timely therapy, the anterior cranial hernia continues to grow, and neurosurgeons in such clinical situations dare to perform surgery at any age of the patient. If this is not done, then symptoms such as abnormal reflexes, twitching of limbs, epileptic seizures and paresis will only worsen in their characteristic intensity.
Encephalocele often occurs in isolation, but this anomaly can be combined with many other defects, such as microsomia of the half of the face. A frontal hernia of the brain, located between the eyes, can be combined with a cleft palate or obstruction of the nasal passages.
The skin over such a tumor has a slightly altered structure and is rough, rough and tough. However, it is still dominated, albeit insignificantly, by hair. On palpation, the lump on the back of the head does not cause acute painful sensations, but is frightening due to its foreignness.
It is dense and immobile, and creates a certain visual defect and discomfort for the patient. So you should get rid of it at all costs. However, there are other signs of a posterior cranial hernia.
An abnormal increase in the distance between the patient's eyeballs is clearly observed, and there is also a symptom of fluctuation in the area of direct protrusion.
A distinctive feature is the fact that as the patient grows, the pathogenic formation of the head increases in size, and at the same time acquires more pronounced symptoms. For example, there is the presence of pathological reflexes, damage to individual pairs of nerves of the cranium, abnormal twitching of the limbs, as well as attacks of epilepsy and paresis. At this stage, the patient already knows about his diagnosis, and the worsening of the clinical picture only reminds of the lack of timely treatment.
Each congenital anomaly has its own specific complications. Some deformities are accompanied by the occurrence of functional disorders: disorders of swallowing, hearing, speech, breathing and vision. There are cases of developmental delay and decreased learning ability.
The child's self-image and relationships with family and other people—these emotional aspects of a child's life are always disrupted with facial deformities. Resolving these problems is as important a part of treatment as eliminating defects through surgery.
After the diagnosis is made, surgery is prescribed. Depending on the type of fetal encephalocele, different types of surgical intervention are used.
The general principle is excision of the hernial sac and plastic surgery of the hernial orifice - closing the skull defect to avoid recurrence of the hernia.
In the case of small intranasal hernias, endoscopic surgery is possible.
In case of a significant defect of the base of the skull, excision of the hernial sac, plastic surgery of the defect of the base of the skull, correction of hypertelorism in some cases in combination with the endoscopic endonasal stage of hernia removal and plastic surgery of the hernial orifice are carried out simultaneously.
Unfortunately, this disease of the fetus is considered extremely severe; no more than 5% of children born with this pathology are able to completely get rid of the consequences.
Occipital meningocele has the best prognosis; with basal encephalocele, a huge number of complications are possible, such as, for example, hydrocephalus or rachischisis.
Most children are stillborn, and only a small percentage survive and, in the best cases, live to 17 years of age.
In cases where there is no pronounced visible hernia, you should pay attention to such symptoms in the child as frequent meningitis, clear fluid coming out of the nose, difficulty in nasal breathing, a visually enlarged bridge of the nose with asymmetry of the orbits. If a child exhibits the above symptoms, you should contact a specialist:
- Neurosurgeon - determines indications for surgical intervention and its timing.
- ENT - determines the volumetric formation of the nasal cavity in the case of basal hernias, signs of liquorrhea.
- Neuropathologist - assesses the presence of neurological symptoms and delayed development of the child.
- An ophthalmologist evaluates the impact of the hernia on the visual pathways, signs of intracranial hypertension based on the results of a fundus examination (in advanced cases, decreased visual acuity).
- Pediatrician - assesses the presence of other anomalies in the development of organs and systems, somatic pathology
- Genetics - reveals the presence of the genetic nature of the disease, the likelihood of anomalies in other organs and systems, and the prognosis of the recurrence of a similar pathology in the next child.
It is necessary to carry out instrumental examination methods:
- An X-ray image that provides the features of the pathology, the size of the hernia, as well as the potential threat to life and health. In addition, computed tomography, which is also considered one of the main diagnostic techniques, allows us to determine the essence of the disease.
- Spiral Computed Tomography (Sp-CT) - allows you to identify a defect in the skull bones, its size, and plan a surgical operation. In some cases, in the presence of liquorrhea, it is necessary to perform a CTCG - the introduction of a contrast agent through a lumbar puncture and subsequent SP-CT in a certain position. This study allows you to identify the source of liquorrhea.
- Magnetic resonance imaging - allows you to identify the contents of the hernial sac and plan the operation.
- Endoscopic examination of the nasal cavity allows you to determine the volume of the encephalocele, visualize the hernial orifice, and evaluate the anatomical relationships for planning surgery.
- Ultrasound of brain structures determines the essence of the anomaly, in particular its geometric shape, size and area of predominance in the cranium.
The diagnosis can also be made during pregnancy. In the case of a large tumor, it is possible to detect pathology on ultrasound already at the beginning of pregnancy; it is also possible to draw the necessary conclusions from changes in blood tests (in the case of encephalocele, the concentration of the AFP protein - alpha-fetoprotein increases), as well as from the analysis of amniotic fluid.
Calculate the cost of treatment (0, average: 5 out of 5)
Cranial hernias, often called encephaloceles, are a fairly rare disease that is congenital in nature.
Cranial hernias occur due to abnormalities in the development of the brain in the fetus in the mother’s womb. As a result, the brain begins to protrude beyond the anatomical boundaries of the skull.
Previously, such a disease was considered incurable, but modern medicine will make it possible to cope with it.
Cranial hernia
general information
If a cranial hernia is suspected, a comprehensive examination is prescribed, which confirms or refutes the initial diagnosis.
A number of factors can lead to the appearance of a cranial hernia, as a result of which the neural tube in the fetus is positioned incorrectly. The main causes of cranial hernias include infectious diseases of the mother and pathological abnormalities in the development of the embryo.
The main causes of cranial hernias
A hernia that appears in the fetus is located among modified tissues, which themselves become a source of inflammatory processes and attract various infections.
Main types
According to their types, all hernias are divided into two main groups: Meningocele and Encephalomeningocele.

Hernias from the Meningocele group are relatively small formations that are filled with cerebrospinal fluid.
Main types
According to the area of localization, four out of five cranial hernias form on the back of the head. Frontal-ethmoidal hernias are less common, and the most severe type is the basal hernia, which does not give external signs, but impinges on the nasal cavity.
Prevention
Prevention should be carried out in the prenatal period. To this end, a woman planning a pregnancy, as well as during it, should:
- to refuse from bad habits;
- stop the uncontrolled use of medications;
- limit contact with aggressive chemicals (including household chemicals);
- not be exposed to ionizing radiation;
- reduce the risk of contracting a viral infection (avoid being in crowded places during periods of seasonal increases in the incidence of ARVI).
Symptoms
A hernia in an adult can be caused by severe trauma, a fall, heavy physical work, or heavy lifting. Children can also be easily injured at a young age, but spina bifida in children who have not yet been born can only be caused by an intrauterine developmental disorder. Adults can talk about the location of pain, its nature and other accompanying symptoms; a newborn child cannot do this.
The main signs of the disease:
- inability to fully control your muscles and limbs, involuntary movements, lack of coordination;
- pain in the affected area with any movement or change of body position;
- excessive sweating;
- feeling of numbness, tingling, goosebumps;
- frequent numbness of the limbs.
After prolonged physical exposure or an uncomfortable position of the body, pain may intensify and radiate pain to other parts of the body.
Video
We offer you to watch a video on the topic of the article.
I. Origin of encephalocele. Closure of the neuroectoderm to form the neural tube begins on day 22 of gestation at several locations along the neural plate and then proceeds bidirectionally to the anterior and posterior neuropores on days 25–26 and 27–28, respectively. The skull is formed from the paraaxial mesoderm covering the forebrain.
Cells derived from the neural crest form this mesenchymal tissue, which will develop into the cartilaginous neurocranium (chondrocranium) at the base of the skull. The mesenchymal vesicles surrounding the telencephalon form the membranes of the neurocranium, from which the cartilaginous skull will be formed. The natural development of the neurocranium and brain requires a normal sequence in the process of neurulation. The facial skull arises from the gill arches between 4–8 weeks of gestation. Violation of the convergence of the branchial arches and the cartilaginous and membranous skull leads to the formation of a basal encephalocele.
Encephaloceles have been regarded as neural tube defects and their origin is thought to depend on a primary cranial neurulation defect. If this were the case, then severe cutaneous and neural structural abnormalities would occur in all encephaloceles. Current hypotheses view encephalocele as a defect in neural tube closure, based on studies of distorted but relatively well-preserved cerebral cytoarchitecture. Most authors believe that the primary abnormality in most encephaloceles consists of defective movement of mesoderm between the neuroectoderm and the cutaneous ectoderm.
The cause of most encephaloceles is unknown. They can be single, family, environmental or genetic in origin. Encephaloceles have been produced experimentally by exposure to radiation, excess vitamin A, folate antagonists, and malnutrition. In humans, encephaloceles have been reported after exposure to antiepileptic drugs (phenytoin, primidone, valproate, and carbamazepine), warfarin, hyperthermia, viral infections, and maternal diabetes mellitus.
Meckel-Gruber, Knobloch, Walker-Warburg, Joubert, Voss syndromes, dissegmental dwarfism, cryptophthalmos and amniotic syndromes may be associated with cephalocele.
II. Epidemology and morbidity. The incidence of encephalocele ranges from 0.8 to 4 per 10,000 births, and there is no gender predominance. The ratio of spina bifida to cranium bifidum is 10:1. There is significant geographic variation in encephaloceles. Occipital encephalocele accounts for 85% of cases in Europe and the USA, while syncipital and basal encephaloceles are more common in Africa, Asia and Australia. The incidence of anencephaly and encephalocele is reduced by a) prenatal diagnosis and termination of pregnancy and b) supplementation with folic acid.
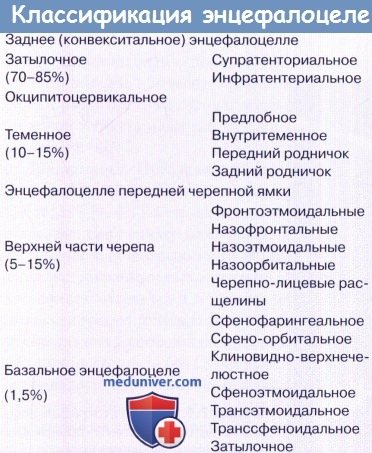
Classification and clinical forms of cerebral hernias. Cephaloceles are classified according to the bone in which the bony defect is located. From a practical point of view, we prefer the classification of Rutka et al., which groups lesions according to their two main sites of occurrence: posterior and anterior encephaloceles.
1. Posterior encephalocele. They occur anywhere from the nasion to the foramen magnum.
a) Occipital encephalocele is by far the most common variant. The size of the lesion does not always reflect the volume of brain tissue. The skin may be thinned but intact or ulcerated with leakage of cerebrospinal fluid. Lesions located above the sinus drainage include one or both occipital lobes and sometimes parts of the ventricle. When localized subtentorially, they are more complex and contain parts of the cerebellum, venous sinuses and even the brain stem.
b) Occipitocervical encephalocele extends from the posterior cranial fossa to the upper segment of the cervical spine.
c) The parietal cephalocele is usually located in the midline and contains one of the cerebral hemispheres.
d) Temporal cephaloceles arise from the greater and lesser fontanels, usually with meningocele, and contain cerebrospinal fluid and remnants of neuroglia.
2. Encephalocele of the anterior cranial fossa. These malformations are present at birth but may not become apparent until adulthood. They may differ in composition and contain dysplastic brain tissue or only cerebrospinal fluid. Possible combination with other facial anomalies, such as cleft lip or palate, microphthalmia, coloboma, cataracts and defects of the corpus callosum. Encephaloceles of the anterior cranial fossa can be divided into two main groups:
a) Syncipital encephalocele emerges from a skull defect in the foramen cecum of the cribriform plate of the ethmoid bone.
b) Basal encephaloceles are located more posteriorly and protrude through the ethmoid plate or from the sphenoid bone. They may contain parts of the brain, pituitary gland or hypothalamus, optic nerve, chiasma, and anterior cerebral artery. They are grouped into several subtypes: - Transethmoidal - Transsphenoidal - Sphenoethmoidal - Spheno-orbital - Sphenoid-maxillary - Occipital
Clinically, basal encephaloceles may present as nasal congestion, causing feeding difficulties, spontaneous rhinorrhea, meningitis, and even endocrine disturbances. They are often associated with palatal fissures. Basal encephalocele is one of the causes of recurrent meningitis. Differential diagnosis is made with nasal polyps, but they are almost never found in children. Nasal polyps do not increase tension during the Valsalva maneuver, while tension increases with intranasal encephalocele (Furstenberg's sign).
Associated anomalies. Approximately 50% of patients with encephaloceles are born with hydrocephalus, especially those with posterior encephaloceles. Reported intracranial abnormalities include corpus callosum agenesis or hypoplasia, arachnoid and porencephalic cysts, absence of septum pellucidum, cerebellar dysplasia or atrophy, neuronal migration disorders (neuronal heterotopia, lissencephaly, polymicrogyria and pachygyria), brain or brainstem atrophy, Chiari malformations and Dandy-Walker, white matter abnormalities, etc.
They may also be associated with anomalies of the venous sinuses and abnormalities of sinus drainage. Parietal cephaloceles may contain dorsal interhemispheric cysts and sagittal sinus duplication. Associated extracranial malformations are present in approximately 50% of cases and include malformations of the eye, heart, kidney, gastrointestinal tract, bone, lung, and muscle tissue.
III. Diagnostics. Prenatal diagnosis is performed through maternal screening and antenatal ultrasound and MPT. Assessment of the clinical condition of infants by a pediatrician is mandatory to assess the viability of children and to identify extracranial anomalies. Most convexital and parietal encephaloceles are diagnosed upon examination. The presence of a skull defect is a necessary condition to confirm the diagnosis. The main diagnostic tool in the evaluation of cephaloceles is MRI. Currently, MR angiography and MR venography are considered necessary for surgical planning.
Cranial X-ray and spiral CT with 3D reconstruction provide very valuable information, especially in cases of basal cerebral herniation.
IV. Treatment of encephalocele. Surgical treatment requires (a) a general pediatric evaluation and (b) complete neuroimaging, including MRI, MR angiography, and bone-based CT. Surgery is not indicated in cases with a prognosis incompatible with life. In children with hydrocephalus who have a poor prognosis, shunt placement may be indicated as a palliative measure. Urgent surgery is needed in cases of: a) lack of skin covering the brain, b) bleeding, c) leakage of cerebrospinal fluid, (d) airway obstruction and e) visual impairment.
Elective surgery is indicated to: a) protect the brain, b) prevent infection, c) improve function (airway, vision, etc.), and d) restore the contour of the skull (cosmetic surgery).
Treatment methods for cerebral hernia. The following methods can be used for different types of encephaloceles:
1. Convexital and simple syncipital encephaloceles. For convexital encephaloceles and some forms of syncipital cephaloceles, a direct surgical approach is performed. The child is intubated and placed in the optimal position for surgery. The bag and surrounding skin area are thoroughly cleaned and treated with betadine. A skin incision is made, the skin and membranes are freely dissected. An attempt should be made to place the majority of the cerebral tissues into the cranial cavity, which in most cases is an impossible task.
However, necrotic or nonviable tissue can be sacrificed. The dura mater is usually sufficient to perform primary repair. If this is not possible, duroplasty is performed with an autologous or heterologous graft. Usually, there is enough skin so there is no need to transpose it. If necessary, the operation is performed jointly with a plastic surgeon.
2. Combination of syncipital and basal encephalocele. When syncipital and basal lesions are combined, treatment is best carried out with the participation of maxillofacial and plastic surgeons. Therefore, the associated facial anomalies and fissures must be addressed. Such anomalies often require an intra- and extracranial approach. The intracranial approach is preferable, allowing the placement of vital structures into the cranial cavity and duraplasty.
Current approaches include bifrontal craniotomy (for most lesions) or pterional or infratemporal approaches for encephaloceles extending into the orbit or infratemporal fossa. Endosurgery is currently being evaluated for the treatment of small basal cephaloceles, but these techniques are limited to encephaloceles with a small skull defect and not all centers have this experience.
3. Advances in the treatment of cerebral hernias. In addition to the use of neuroendoscopic procedures and craniofacial reconstruction, there is growing interest in brain tissue preservation and techniques aimed at increasing the volume of the skull to accommodate herniated tissue.
V. Complications of treatment of cerebral hernias. Modern methods of anesthesia and neurosurgery have significantly reduced surgical mortality. Intraoperative complications reported include hemorrhage and cerebral infarction. Complications after surgery include wound dehiscence or necrosis, liquorrhea, meningitis, superficial or deep infections, the development of hydrocephalus and epilepsy.
VI. Encephalocele prognosis. Neurological and intellectual outcomes are better with anterior and basal cephaloceles than with convexital lesions. The prospects for children with encephalocele depend on the volume of the brain herniation, the presence of microcephaly, and hydrocephalus. Only 20-30% of patients with posterior encephalocele will achieve normal intellectual development. In the absence of hydrocephalus, this percentage increases to 40%, but many will be disabled. Atretic cephaloceles and meningoceles are associated with a much better prognosis than true encephaloceles.
Atretic cephaloceles and cranial meningoceles, due to the presence of less functional neural tissue, are associated with a much better prognosis than true encephaloceles.
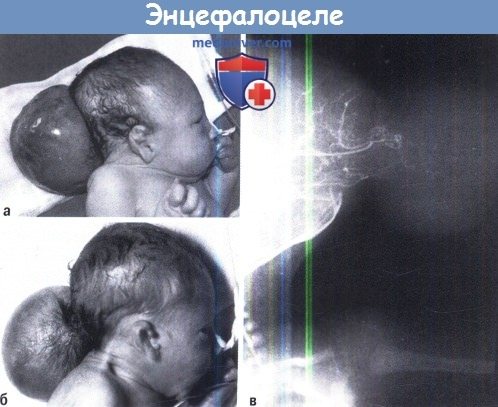
A-B Photograph of two typical cases of occipital encephalocellus. Angiography shows the volume of brain tissue penetrating the hernial sac.
A, B. Photograph of a newborn with a parietal encephalocele. MRI of the same patient.

A, B. Encephalocele base.
A Visualization of pathological changes (arrow) with MRI and B 3D reconstruction of the skull showing its defect (arrow). According to statistics, today for every 100 thousand people there are 100 cases of intervertebral disc herniation. However, not everyone knows what the symptoms of this disease are and how to treat intervertebral hernia without surgery.
A sedentary lifestyle over time can cause many diseases, including intervertebral disc herniation. The risk group includes men and women from 25 to 50 years of age who perform work that involves heavy lifting (for example, loaders) or prolonged sitting (for example, in an office in front of a computer). But what to do if you have already had to deal with this disease?
Symptoms depending on the level of damage
Naturally, if the hernia compresses the corresponding nerve roots in the neck, then compression syndromes for each level will be special:
- if the root of C2, the second cervical vertebra, is involved, then there is no cartilaginous disc at this level, and the posterior arch of the atlas acts as a source of compression;
- in case of damage to the C3 roots, there may be sharp pain in the neck and tongue, pain when mixing food with the tongue. If the nerve roots are irritated without pain by a hernia at this level, then the tone of the diaphragm increases, and this leads to a displacement of the liver slightly lower than necessary. There may even be chest pain reminiscent of angina pectoris. It should not be surprising that cervical osteochondrosis can lead to a downward displacement of the liver; this is not clinical casuistry at all, but reality;
- if a hernia affects a pair of roots in the C5 segment, the pain will radiate from the neck to the shoulder girdle, and if the motor portion is affected, there will be weakness and a decrease in the tone of the deltoid muscle. The patient will have difficulty raising his straight arm to a horizontal position;
- a lesion of C6 will manifest itself as pain along the outer surface of the shoulder from the neck, from the area of the shoulder blades up to the thumb, and sensory disorders in the area of innervation of this root. All these symptoms increase if the patient moves his head.
Accordingly, specific symptoms arise in other segments - C7 and C8, which is located between the last, seventh cervical and first thoracic vertebrae. In general, the symptoms of lesions in the cervical spine are very rich and varied; the doctor should always keep this in mind. Such a patient should be worked carefully. How to treat an intervertebral hernia, how to provide first aid, and what treatment methods are the best?