| Hydrocephalus | |
| skull of a patient with hydrocephalus | |
| ICD-10 | 91., 03. |
| ICD-9 | 331.3331.3, 331.4331.4, 741.0741.0, 742.3742.3 |
| OMIM | 123155, 236600, 236635, 307000, 615219, 236600, 615219, 123155, 236635 and 307000 |
| DiseasesDB | 6123 |
| MedlinePlus | 001571 |
| eMedicine | neuro/161 |
| MeSH | D006849 and D006849 |
Hydrocephalus
(from ancient Greek ὕδωρ “water” + κεφαλή “head”),
hydrocephalus
is a disease characterized by excessive accumulation of cerebrospinal fluid in the ventricular system of the brain [1] as a result of difficulty in its movement from the place of secretion (ventricles of the brain ) to the site of absorption into the circulatory system (subarachnoid space) -
occlusive hydrocephalus
, or as a result of impaired absorption -
aresorptive hydrocephalus
.
Hydrocephalus
- a person suffering from hydrocephalus.
What's happened
Congenital hydrocephalus is caused by an abnormal accumulation of cerebrospinal fluid inside the brain. CSF is produced by the choroid plexus of the brain. Moreover, the level of productivity depends on the time of day. Normally, a person contains about 150 cerebral fluid. It covers the spinal cord and brain, fills the ventricular system, consisting of four ventricles. CSF flows through the ventricles of the brain and exits into the subarachnoid cavity, where it is reabsorbed into the bloodstream.
Absorption and production of cerebrospinal fluid are balanced processes. The liquid itself has special purposes. It acts as a shock absorber for the brain, providing protection against concussions and impacts. CSF also delivers nutrients the brain needs to function properly.
Liquor provides oncotic and osmotic balance. Antibodies accumulate in the CSF, protecting the brain from the penetration of bacteria and viruses. The fluid takes part in the regulation of blood circulation in the confined space of the cranial cavity and spinal canal.
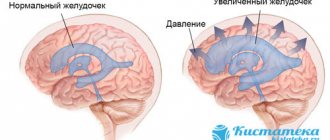
When an imbalance occurs between the production and removal of fluid, the ventricles of the brain expand. Due to their increase, pressure on the brain increases, which can lead to serious neurological damage to the organ.
What is mixed type hydrocephalus?
A complex neurological disease has a simple non-medical definition. Hydrocephalus is called dropsy. The disease is provoked by a violation of the circulation of cerebrospinal fluid (CSF). It is produced daily and distributed in the ventricles, subarachnoid fissures and cisterns of the brain. Circulating in tissues, cerebrospinal fluid nourishes brain cells and removes metabolic products. In addition, cerebrospinal fluid ensures a stable location of the brain in the skull and performs a shock-absorbing function. This is a kind of anatomical protective barrier that protects soft, vulnerable brain tissue from internal and external influences.
Normally, the volume of fluid is 120-150 ml, but for constant renewal the body produces more, approximately 500-600 ml per day. If the cerebrospinal fluid levels are normal, there are no abnormalities in brain function. But for various reasons its volume may increase. The intensively produced cerebrospinal fluid does not have time to be absorbed, accumulates in large quantities and blocks the work of vital centers in the brain area. Violation of the dynamic balance leads to the development of foci of the disease and the inevitable deterioration in such cases of the physical and psycho-emotional state of the patient.
International Classification of Diseases
Congenital hydrocephalus in ICD-10 refers to the group of congenital anomalies, deformations and chromosomal disorders (Q00-Q99). This class includes a wide variety of congenital abnormalities of the nervous system, eyes, ears, neck, circulation, breathing, palate, and lips.
In ICD 10, congenital hydrocephalus is included in the group of congenital anomalies of the development of the nervous system - Q00-Q07. This group includes a variety of cephalias and developmental defects, including congenital anomalies of the brain, spinal canal, and spinal cord. In ICD-10 CNS congenital hydrocephalus is described in section Q03.
Types of pathology
Currently, there is no unified classification of hydrocephalus. The reasons for diversity are polyetiology and diversity of morphological manifestations.
According to etiological properties, congenital hydrocephalus (ICD code 10 Q03) is divided into the following types:
- Hydrocephalus, in which normal cranial pressure is maintained. Usually the pathology is observed in people over 50 years of age. In most cases, the cause of the pathological condition is not determined.
- Congenital hydrocephalus. It can occur due to congenital infectious pathologies suffered by the mother during pregnancy, congenital anomalies and a number of other reasons.
- Acquired hydrocephalus. Most often it develops as a complication of stroke, brain tumors, after a head injury.
According to morphological characteristics, hydrocephalus can be occlusive and communicating. The latter is characterized by impaired absorption of cerebral fluid due to damage to certain structures.
According to the nature of the course, the pathology is divided into acute, subacute and chronic. The first type occurs before the development of severe decompensation. The acute form lasts up to three days. Then comes the subacute stage, which develops for about a month. In a chronic course, pathological changes develop slowly, up to six months or longer.
Clinic
Normal pressure hydrocephalus gradually causes dysfunction of movement, mainly walking. This is the first symptom. A short time later, signs of dementia and other mental disorders appear, and later disorders in some pelvic organs are observed.
Walking disorder
Deviations when walking are expressed by a “magnetic” gait - movement in short shuffling steps - difficulties in maintaining balance when turning and moving. There are no disturbances in hand movements while walking. Patients can also perform leg movements while lying down, as when walking.
Abnormalities in other brain functions
Patients with this pathology are usually in a state of complacency, disoriented in time, and cannot talk about their illness. Some patients suffer from hallucinations, various manias, attacks of depression, drowsiness and other abnormalities.
Functional disorders of cognitive type
Noticed in most patients in the initial stage of the disease. These are memory disorders and slow reaction speed, accompanied by an inability to use knowledge and complete apathy. However, all these symptoms are non-dominant.
Pelvic disorders
Already at the very beginning of the disease, patients may complain of a frequent urge to urinate, and later of urinary incontinence (when patients do not realize or notice these urges). But disturbance of sensations during stool occurs only in those patients who have a late stage of hydrocephalus.
Forms of the disease in children
Congenital hydrocephalus (ICD-10 code is indicated above) has several degrees of severity. It can be moderate, in which the lateral ventricles dilate up to three centimeters, and the minimum thickness of the brain cloak is more than two centimeters. When the ventricles expand to four centimeters, and the cloak narrows to one, they speak of severe dropsy. The critical form is characterized by dilation of the ventricles to five or more centimeters and a narrowing of the brain cloak to five millimeters or less.
Causes of congenital type of disease
The most common cause of congenital hydrocephalus is stenosis of the Sylvian Falls, which connects the fourth ventricle to the third. It is not uncommon for the disease to occur due to intracranial hemorrhage under the epindyma of the cerebral aqueduct caused by a cerebral vein aneurysm. Most often, congenital hydrocephalus of the brain is of a closed type, i.e. occlusive.
In half of the cases of the disease, a history of infectious pathologies of the mother is detected. This is another cause of congenital hydrocephalus in a child. Examples of pathologies that cause dropsy are:
- Cytomegalovirus. This is one of the most common types of viruses transmitted transplacetally - transmitted through the placenta from mother to fetus. It puts the fetus at risk of abnormal development.
- Rubella. The pathology is not dangerous, but if infected during pregnancy, especially in the early stages, there is a high probability of serious disturbances in the formation of the fetus.
- Piggy. The disease refers to acute infectious pathologies that affect the glands, in particular the parotid glands.
- Syphilis. The disease is classified as venereal. If a pregnant woman is infected in the early stages of pregnancy, the pathology can lead to miscarriage, delayed fetal development, and premature birth.
- Toxoplasmosis. The pathology is parasitic, caused by Toxoplasma. With the congenital type of the disease, an anomaly in the development of the child’s nervous system occurs.
There are a number of other pathologies that lead to the development of congenital hydrocephalus of the brain.
Hydrocephalus: A Brief Description
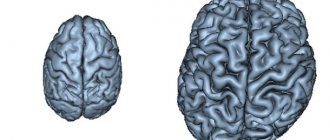
Hydrocephalus (dropsy of the brain) - excessive accumulation of cerebrospinal fluid in the ventricles of the brain and intrathecal spaces; manifested by symptoms of increased ICP • Occurs due to an imbalance between the formation and absorption of cerebrospinal fluid: less is absorbed than is formed. The cause may be an obstructive process in the ventricles or in the subarachnoid space, less often - true hyperproduction of cerebrospinal fluid (with villous plexus papilloma) • Characterized by excessive accumulation of cerebrospinal fluid in the ventricles of the brain or subarachnoid space with their expansion • In newborns it leads to an increase in the size of the skull and brain atrophy ( decreased metabolism in adjacent areas of the brain).
Code according to the international classification of diseases ICD-10:
- G91 - Hydrocephalus
- G91. 2 - Normal pressure hydrocephalus
- G94* - Other brain lesions in diseases classified elsewhere
- O33. 6 - Fetal hydrocephalus leading to disproportion requiring maternal medical care
- Q03 - Congenital hydrocephalus
- Q05 Spina bifida [incomplete closure of the spinal canal]
Classification
By the presence of communication between the cavities of the ventricles of the brain and the subarachnoid space.
• Non-communicating (obstructive) hydrocephalus is caused by a process that causes blockage of the ventricular system • Acquired hydrocephalus • Tumors of the IV ventricle (medulloblastoma, ependymoma - with them all ventricles are dilated) and the aqueduct of Sylvius (glioma of the midbrain tegmentum - the lateral and III ventricles are dilated, and the size of the IV ventricle not changed) • Fibrosis of the arachnoid membrane due to meningitis or intraventricular hemorrhage • Congenital hydrocephalus • Stenosis of the Sylvian aqueduct in the presence of a septum and true narrowing (#307000, Xq28, L1 cell adhesion molecule gene L1CAM, 308840, À ). Congenital stenosis is characterized by a small size of the posterior cranial fossa • Dandy–Walker syndrome - congenital atresia of the foramina of Magendie and Luschka. Characterized by cystic dilatation of the IV ventricle and cerebellar hypoplasia • Vein of Galen aneurysms (v. cerebri magna - Galeni) and other vascular malformations • Benign intracranial cysts (arachnoid and ependymal) • hydrocephalus is a rare form of congenital hydrocephalus in men.
• Communicating (non-obstructive) hydrocephalus occurs when there is an obstruction in the cerebrospinal fluid circulation pathways distal to the exit from the IV ventricle and at the level of pachion granulations • Acquired • Inflammation of the arachnoid membrane during meningitis and as a result of intraventricular hemorrhage (most often with birth trauma and in premature infants) • Venous thrombosis, stenosis of the dural sinuses • Trauma accompanied by subarachnoid hemorrhage, followed by inflammation of the arachnoid membrane • hydrocephalus • Congenital • Inflammation of the arachnoid membrane - intrauterine infection • Encephalocele • Agyria - developmental anomaly: absence of convolutions of the cerebral cortex; the cranial cavity is filled with cerebrospinal fluid.
Separately, functional hydrocephalus is distinguished, which develops as a result of excessive formation of cerebrospinal fluid with villous plexus papilloma. This tumor may also itself obstruct the ventricular system, causing obstructive hydrocephalus. Small hemorrhages from it cause obstruction of the subarachnoid space (after removal of the tumor, hydrocephalus may persist).
According to the predominant accumulation of cerebrospinal fluid • Internal (ventricular) hydrocephalus - hydrocephalus , characterized by the accumulation of cerebrospinal fluid mainly in the ventricles of the brain • External hydrocephalus - hydrocephalus with accumulation of cerebrospinal fluid mainly in the subarachnoid space or (less often) in the subdural space in the presence of communication between the subarachnoid and subdural spaces • General hydrocephalus - hydrocephalus with accumulation of cerebrospinal fluid both in the ventricles and in the subarachnoid space.
Signs of illness
The main sign suggesting dropsy in a child is an increase in the size of the head. The following symptoms may also occur:
- breathing problems;
- frozen, prone to contraction muscles of the arms and legs;
- delay in the development of certain stages, for example, a child cannot learn to sit or crawl;
- bulging fontanelles, changing their shape;
- loss of appetite;
- refusal to move the head;
- The scalp is thin, veins are visible.
Congenital hydrocephalus in children can be manifested by a violation of the location of the pupil; it is located close to the lower part of the eyelid. This symptom is called the “setting sun symptom.” Convulsions and vomiting may also occur.
Symptoms
If congenital internal hydrocephalus does not progress, then it does not have pronounced symptoms. Most often, in such children, the head circumference remains normal, and other clinical symptoms are practically absent.
As dropsy progresses, there is a dynamic increase in head size. In premature babies, in the first month of life, the circumference should not increase by more than one centimeter per week. With faster growth, doctors suspect dropsy.
Signs of progression of the disease are the following symptoms:
- swollen fontanelles;
- the head is deformed, the proportions of the skull are not respected, there is a pronounced predominance of the cerebral region;
- muscle tone is impaired;
- convulsions;
- chin tremor;
- tendon reflexes.
When intracranial pressure increases, the child vomits, the pulse quickens, and breathing becomes impaired. There is a lag in psychomotor development, the functions of the autonomic nervous system are disrupted, and the function of the cranial nerves changes.
Causes
One of the characteristic features of a neurological disease is the likelihood of its manifestation during a woman’s pregnancy. The cause of the development of congenital pathology is intrauterine infections and abnormalities in fetal development. The acquired form develops in children after birth. This type of disease can be caused by the following deviations:
- Birth injuries.
- Genetic predisposition.
- Intrauterine infections.
- Head injuries.
- Inflammatory processes (meningococcal infections, encephalitis, otitis).
- Brain neoplasms (hemotomas, tumors, parasitic cysts, abscesses).
For a long time, mixed hydrocephalus was considered exclusively a childhood disease. Many consequences of head injuries and strokes in adults were treated in special neurological hospitals and psychiatric hospitals. Today, patients are seen by neurosurgeons and neurologists. According to statistics, in 25% of patients, hydrocephalic syndrome is detected after the age of 18, and the disease is much more complicated than in children. This is due to the fact that in adults the cranial bones in the fontanel area are motionless. The fluid accumulates more intensely, compresses the brain tissue, which contributes to an increase in intracranial pressure.
Among the most common causes of the development of pathology in an adult patient are traumatic brain injuries, infectious and inflammatory diseases of the nervous system, strokes, vascular disorders, and intracerebral tumors.
Very often, mixed type hydrocephalus is diagnosed in old age, when atrophy of brain cells is observed under the influence of pathologies and external influences. A decrease in brain volume in the cranium leads to an increase in cerebrospinal fluid. Such changes are typical for the age of 60-70 years. Most often, pathological abnormalities develop in those suffering from atherosclerosis and arterial hypertension. At risk are people with diagnosed osteochondrosis in the cervical spine, frequent concussions and head injuries, and alcohol abusers.
Mixed hydrocephalus in older people can worsen suddenly. Often patients are not aware of the presence of pathology, and those around them treat progressive physical and mental abnormalities as normal aging symptoms. Meanwhile, it is in old age that people need timely treatment. At any moment, the disease can remind itself and lead to circulatory problems, dementia, disability, and death.
Diagnostic methods
To establish a diagnosis, different diagnostic methods are used. They include: collection of complaints, anamnesis, assessment of clinical data. Children experience head enlargement, nausea, vomiting, and headaches. Newborns cry constantly due to pain. Instrumental diagnostic methods in the form of MRI, CT, and fundus examination are required. A consultation with a neurosurgeon is often necessary.
There are methods that make it possible to detect congenital hydrocephalus of the brain in utero. For this purpose, determination of alpha-fetoprotein in blood serum, amniotic fluid, and karyotype is prescribed. An ultrasound examination is performed. These methods make it possible to determine an abnormality in the development of the nervous system, and the pregnant woman decides whether the pregnancy will be terminated. This approach helps reduce the birth rate of children with abnormal development of the nervous system in many countries around the world.
This diagnostic technique is carried out among women at risk. These are all those whose work involves heavy physical labor, who suffered infectious diseases during pregnancy, who have poor environmental conditions, or work in hazardous industries.
After birth, the baby's head circumference is constantly measured. If there is a deviation from the norm, various tests begin to be carried out. The simplest and most accessible method is diaphanoscopy - shining a light through the head. An ultrasound is required, and a tomography may be prescribed. It makes it possible to see the cavity with fluid, evaluate its size, and the severity of cerebral edema.
Diagnostics
Research methods • X-ray of the skull: dehiscence of the sutures of the skull, deepening of finger-like impressions, thinning of bones (with prolonged hypertension), intracranial calcifications (as a result of congenital infections). Small sizes of the posterior cranial fossa suggest stenosis of the Sylvian aqueduct, large ones - Dandy-Walker syndrome • Ultrasound (neurosonography) indicates the degree of ventricular dilatation, intraventricular hemorrhage • CT helps determine the size of the ventricles, the location of obstruction of the cerebrospinal fluid pathways, and allows to identify associated anomalies • MRI is the most informative , indicated for the combination of hydrocephalus with tumors, vascular malformations, and multi-chamber ventricles • Angiography helps to identify vascular anomalies • If a congenital infection is suspected, serological tests are performed for rubella, herpes, CMV, Toxoplasma gondii and Treponema pallidum viruses.
Differential diagnosis • Congenital macrocrania (normal head growth rate and family history of macrocrania) • Enlarged head with rickets (overgrowth of bone tissue of the skull and skeletal changes typical for rickets) • Volumetric intracranial formations (subdural hematomas, tumors).
Tests
When diagnosing, infusion and drainage tests are required. They make it possible to determine quantitative parameters, elastic properties of tissues, and liquor dynamics.
The test technique involves draining the lumbar cistern and reducing the pressure in the sinuses. When infused with saline, there is a short-term increase in pressure in the sinuses, then it decreases. Calculations are carried out using special formulas to determine fluid speed, resistance and other parameters.
Testing helps determine the need for surgery.
Treatment
The causes and treatment of congenital hydrocephalus are closely related. The doctor may prescribe surgery or select a conservative method of therapy.
Conservative methods include drugs that reduce intracranial pressure, diuretics are selected.
Therapy also includes drugs that eliminate the inflammatory process that led to the development of dropsy. These could be antibiotics and other medications. As the disease progresses, occlusions occur and surgical intervention is indicated.
In most cases, drug treatment does not give the desired results, which is the basis for surgical intervention. They are conditionally divided into several groups:
- Interventions to temporarily reduce ICP and neutralize craniocerebral disproportion.
- A surgical intervention that allows fluid to be removed to other body systems.
- Operations performed to restore fluid circulation.
- Interventions carried out to suppress the production of cerebrospinal fluid.
- A surgical intervention to activate the sorption of cerebrospinal fluid.
Surgical treatment involves eliminating the cause that led to the accumulation of fluid in the brain and performing shunt surgery. It involves implanting a silicone tube through which fluid is drained from the skull into another cavity.
Consequences of hydrocephalus
Lack of timely treatment for cerebral hydrocele is fraught with serious consequences. A long course of the disease leads to degeneration of brain tissue, which entails disruption of the activity of visceral organs and ultimately leads to the death of the patient.
The open form of the disease is characterized by a change in the shape of the head. High intracranial pressure provokes problems with vision and hearing. Among the frequent consequences of the disease, the following should be noted:
- slowdown in physical and intellectual development;
- hearing loss, visual impairment;
- speech dysfunction;
- headaches, migraines, dizziness;
- autism;
- learning difficulties, cognitive dysfunction.
Modern diagnostic and treatment methods make it possible to eliminate disorders at an early stage. After adequate treatment, children with hydrocephalus develop on par with their peers.
Methods of surgical treatment
At various periods of development, neurosurgery gave preference to cerebrospinal fluid shunt operations. They allow occlusion of the cerebrospinal fluid passages using the bypass method with implantation of the valve system. During surgery, a catheter is placed in the brain to drain excess cerebrospinal fluid to other parts of the body. This may be combined with the abdominal cavity and heart chambers. The doctor inserts one end of the catheter into a ventricle of the brain, then creates a subcutaneous tunnel. Typically, this procedure gives positive results, and there is no need for repeated operations after it. However, complications such as infection or clogging of the shunt may occur.
Patients with dropsy walk with a shunt all their lives. If it is installed in childhood, then as it grows, several more operations are performed in which the tube is replaced with a longer one.
In some cases, plastic surgery of the cerebral aqueduct is indicated. It is performed in patients with occlusion by endoscopic aqueductoplasty.
In patients, the rostral mouth of the cerebral aqueduct is covered with thin and elastic connective tissue, which was formed as a result of hemorrhages and infections. It is easy to eliminate, but before this procedure, a thorough examination of the patient is carried out using tomography.
For the treatment of newborns in cases where massive subarachnoid and intraventricular hemorrhages occur, diuretics are combined with unloading punctures of the lumbar and ventricular region. If an intrathecal hematoma appears, a procedure is performed to remove it.
The drainage system allows you to normalize ICP, as well as control the dynamics of the cerebrospinal fluid. This allows you to avoid hypertensive liquor crises and postpone bypass surgery.
For children with low body weight, an additional subcutaneous reservoir can be installed, which allows repeated pumping of cerebral fluid and monitoring of ICP.
Shunt surgery is performed to treat progressive hydrocephalus. In 50% of cases, immediately after installation of the shunt, children’s general condition returns to normal, which almost completely eliminates postoperative complications.
Acquired hydrocephalus of the brain in an adult: treatment with drugs
Modern medicine offers patients a lot of treatment options. If a couple of decades ago more than half of the patients died, today the mortality rate is about 5%.
Therapy in this case directly depends on the causes of the disease, the stage and reasons for its development. If hydrocephalus is the result of an inflammatory or infectious disease, then the patient is first prescribed a course of antibiotics or antiviral agents. Sometimes the amount of cerebrospinal fluid in the brain is not too large - in such a situation, excess fluid is eliminated with the help of diuretic drugs (Furosemide, Acetazolamide).
But, according to statistics, surgery for hydrocephalus is necessary in the vast majority of cases.
After operation
To treat hydrocephalus, a shunt is installed. Most often it remains for life. However, periodic monitoring of valve pressure by a physician may be required. The surgeon is watching him.
In addition, after bypass surgery it is necessary to monitor your health by constantly visiting a doctor. This is due to the fact that each operation can be complicated. To avoid this, it is recommended to undergo regular preventive examinations by a surgeon or neurologist. These specialists will monitor the development of hydrocephalus and also determine whether the shunt can be removed.
Prognosis and prevention
Timely diagnosis, an adequate course of treatment with medications or a professionally performed surgical operation can achieve a successful cure. The patient’s well-being improves, unpleasant symptoms disappear, and the patient returns to a full, healthy life.
Preventive measures help prevent the development of mixed hydrocephalus and protect yourself from pathological abnormalities of the brain. Avoid head injuries and stressful situations, do not ignore inflammatory and infectious diseases of the brain, strengthen your immune system with a healthy lifestyle and a balanced diet. Doctors recommend that expectant mothers undergo medical and genetic counseling, protect themselves from infections, and visit a doctor on prescribed days.
Complications of dropsy
Complications of dropsy can be:
- hearing loss, visual impairment up to blindness;
- muscle weakness;
- carbohydrate and fat metabolism is disrupted;
- There are disturbances in the respiratory and cardiovascular systems;
- regulation of body temperature is impaired.
If complications occur, there is a high risk of death. To avoid complications, it is necessary to begin treatment of the pathology as early as possible. It allows you to achieve either complete recovery or stable remission.
People live with implanted shunts their entire lives. If after several years the dropsy does not return, the shunt is removed. This outcome is considered a complete recovery.
Complications after surgery
Postoperative complications are observed in approximately 20% of cases, late complications - in 15%. Early complications are characterized by inflammatory changes and the formation of fibrinous clots.
Sometimes infectious complications occur in the form of bacterial meningitis and ventriculitis. Less common are glomerulonephritis and endocarditis. With prolonged ventriculitis, periventricular encephalitis occurs.
The causes of complications may be:
- infectious processes in postoperative wounds;
- contamination of the shunt with the growth of a pathogen on it;
- necrotic complications.
Most often, after ventriculostomy, non-infectious ventriculitis occurs, provoked by antiseptics.
Hyperthermia and a feverish state may be caused by the reaction of the hypothalamus to heating by the light flux of the endoscope.
The rarest complications are bleeding, leading to bulimia and diabetes insipidus.
Prevention
To prevent congenital hydrocephalus, pregnant women are carefully examined, especially if they are at risk. Women are advised to follow their daily routine, avoid stressful situations and overwork. Measures are also being taken to prevent infectious pathologies such as meningitis, encephalitis, syphilis and other diseases that lead to infection of the fetus and its abnormal development.
Newborns must undergo transcranial ultrasonography. This diagnostic procedure is done on the first day of life to exclude hemorrhages and congenital malformations of the central nervous system. When verifying intraventricular hemorrhages, neurosonographic monitoring is carried out every day.
When ventriculomegaly increases, children should be in intensive care under constant supervision. In some cases, it is advisable to immediately perform ventriculosubgaleal drainage in order to evacuate the cerebrospinal fluid.
In pediatric surgery, the most minimally traumatic method in the treatment of hydrocephalus is endoscopic ventriculostomy, which is performed for children over one year of age.
Disability
In some cases, the child is assigned a disability group due to congenital hydrocephalus. It is determined by the degree of health loss. The status of “disabled child” is given for 1 or 2 years, or until the child reaches 18 years of age.
Hydrocephalus is included in the list of pathologies in which a child is given a disability until he or she reaches 16 years of age. However, in order to clarify which group will be given, it is necessary to undergo a medical examination, at which doctors will make an opinion on the state of health, existing disorders, and developmental anomalies.
Timely treatment will allow the child to live and develop normally, without deviations from the norm. Even if he gets a shunt installed, there is a chance that he will live a full life or make a full recovery.
Modern medicine has learned to help people with a variety of diseases, and dropsy is no exception.