What causes a cyst in the head?
A benign spherical formation - a cyst in the brain - is filled with cerebrospinal fluid inside. The severity of symptoms depends on the size of the tumor, but it is detected during a random medical examination or when any other disease is diagnosed. Arachnoid cysts of the brain are asymptomatic in most cases. Vivid neurological symptoms are present in only 20% of patients. Factors influencing the appearance and growth of cysts:
- any brain injury;
- increase in fluid pressure inside the cystic formation;
- inflammatory process in the brain (infection, virus).
Treatment regimen for illness
The main condition for good health in the presence of an arachnoid cyst of the brain (operated or non-operated) is compliance with the treatment regimen. The patient must adhere to the daily routine and especially the work and rest schedule, abstain from alcohol, strong coffee, energy drinks and drugs that increase the tone of the nervous system.
Taking any medications that affect the nervous system and vascular tone should be agreed with a neurologist. Extreme and dangerous sports, driving, and activities related to working at heights or near moving machinery are not recommended.
There are several membranes in the brain, including the arachnoid membrane. The subarachnoid, which is located underneath and contains cerebrospinal fluid (CSF), in some situations can expand, and benign formations-cavities filled with cerebrospinal fluid appear. These are archanoid cysts, or arachnoid changes of a liquor cystic nature.
Types of arachnoid cyst
Leading experts in the field of medicine today identify two types of neoplasms, which differ from each other in the cause of their occurrence. The first is primary, which develops in the baby while still in the womb. Secondary manifests itself in the process of the above pathologies. Also, a cyst can be simple, formed from the cerebrospinal fluid, or complex, containing various types of tissue. Based on their location, tumors in the brain are divided into:
- left or right temporal lobe;
- parietal or frontal part of the head;
- cerebellum;
- spinal canal;
- posterior cranial fossa;
- spine (perineural);
- lumbar region.
Primary (congenital)
It can form as a result of inflammatory processes that developed during the prenatal period. The cause of the appearance of a neoplasm is sometimes birth trauma or meningitis in a newborn. There are often numerous developmental disorders of the fetus due to smoking, taking medications, and drinking alcohol by a pregnant woman. If the primary cyst progresses rapidly, then with severe symptoms it can be removed at any age of the child.
Secondary (acquired)
This type of arachnoid cyst of the brain develops after illnesses, injuries, and surgical interventions. The occurrence can be triggered by a strong blow to the head, concussion after an accident, subarachnoid hemorrhage or mechanical damage. When a secondary cyst begins to form as a result of some pathology, its walls consist of scar tissue. If a cyst in the brain of an adult has developed for another reason, then its walls contain tissue of the arachnoid membrane.
Reasons for development
Arachnoid changes of a liquorocystic nature are formed even during the period of bearing a child; they are called primary:
- drug abuse, use of several groups of drugs in one period of time;
- radiation exposure during pregnancy (CT, MRI, X-ray);
- intrauterine infections: herpes, toxoplasmosis, rubella;
- bad habits;
- constant overheating of the mother's body;
- genetic mutations (Marfan syndrome);
- poor environmental situation.
A secondary arachnoid cerebrospinal fluid cyst forms in response to inflammatory processes that affect the brain. Most often these include: encephalitis, meningitis, arachnoiditis. May occur in response to hemorrhages, surgical interventions, hematomas and strokes. A concussion often provokes the formation of a cyst.
Main signs and symptoms of formation
Signs of a cyst appear as it grows. Headaches begin, tinnitus and skin sensitivity are disrupted. If an arachnoid cyst of the brain is not treated, paralysis of the limbs may occur, epileptic seizures may appear, deafness may increase, and vision may be lost. Symptoms of the disease are characteristic of a specific affected area.
In adults
Small bubbles with liquid contents in the brain tissue do not pose a threat to humans, and he can easily live with them throughout his life. Large formations of a progressive type have clear signs of pathology. This:
- loss of orientation;
- regular migraine;
- loss of sleep;
- violation of muscle tone;
- lameness;
- nausea, vomiting;
- twitching of limbs (involuntary);
- dizziness.
- pulsating fontanel;
- lethargy of the limbs;
- disoriented look;
- spitting up like a fountain after feeding.
Symptoms
These pains can be very intense, and even provoke nausea and vomiting. However, in cases where a cyst occurs as a consequence of a long-term illness, symptoms of the disease may not appear.
Another sign of such changes, depending on their location, may sometimes be numbness of the limbs, “goosebumps” on the skin and uncertainty in gait; specific manifestations here are determined by the localization of pathological changes. There may also be a feeling of fullness, or a feeling of pulsation, noise in the ear in the absence of hearing impairment, epileptic seizures, double vision, partial paresis of the limbs and sporadic blackouts. Similar symptoms can occur with vascular malformations in the vessels of the brain, primary and metastatic brain tumors, and some other pathologies. To exclude these processes, which require urgent treatment, an X-ray examination of the skull in two projections, rheovasography of cerebral vessels, and nuclear MRI are performed.
Diagnostic methods
The optimal diagnostic method for pathology is MRI of the brain. If there is a cyst, the final description of the tomography results will indicate: “arachnoid changes of a liquor cystic nature.” The location of the formation is revealed by the use of contrast agents. The main property of a neoplasm, unlike a tumor, is the ability to accumulate contrast. If necessary, laboratory tests and studies are carried out:
- blood for cholesterol;
- to detect infections;
- Dopplerography of blood vessels;
- measuring blood pressure (detects its surges).
Treatment methods
Treatment methods for the disease will depend on the diagnostic results. If the arachnoid cyst of the brain is small, it does not pose a health hazard. The patient will be observed by a doctor and undergo periodic examinations. During this period, it is important to eliminate the cause of the pathology and minimize the influence of negative factors. If the tumor grows rapidly, drug therapy or surgery will be used.
Drug therapy
Medium-sized cysts can be eliminated with medications. The course of treatment is prescribed individually and is carried out under the supervision of a doctor until the patient’s condition improves. Names of medications that can stop the growth of tumors:
- absorbable adhesions: Longidaz, Karipatin;
- activating metabolic processes in tissues: Actovegin, Gliatilin;
- immunomodulators: Viferon, Timogen;
- antiviral: Pyrogenal, Amiksin.
Folk remedies and herbs
With an asymptomatic brain cyst, it is possible to support the body with folk recipes:
- Tincture of hemlock herb. Eliminates headaches. The duration of treatment is 79 days. If necessary, the course can be repeated. You can prepare the tincture as follows: 100 g of seeds or crushed stems are poured with olive oil (0.5 l). The solution should be left in a dark place for three weeks. Afterwards the oil is passed through cheesecloth several times. The infusion is taken through the nose 3 times a day, 2 drops.
- Infusion from the root of Caucasian dioscorea. It has a beneficial effect on brain function: it cleanses and dilates blood vessels. The course of treatment is 2-3 months. The root (200 g) is crushed, the jar is filled, and 700 ml of vodka is poured. The composition is infused in a cool place for 5 days. Afterwards, the infusion is drained and another 700 ml of vodka is poured. After 5 days, both compositions are mixed, filtered and consumed 2 tsp. three times/day before meals.
- Yeast elixir. Helps reduce inflammation and normalize intracranial pressure. The course of treatment is three weeks. Yeast (1 tablespoon) is mixed with dried elecampane grass (40 g) and three liters of boiled water. Leave for 2 days, then take half a glass 4 times a day.
Surgical intervention
If the brain cyst increases in size, then surgery will be prescribed to remove it. Modern medicine involves several types of surgical intervention:
- endoscopic method - the least traumatic, when the contents are removed through punctures;
- Bypass surgery is carried out by inserting a drainage tube into the cyst cavity (high risk of infection);
- fenestration is performed by excision of the formation using a laser;
- puncture, which involves removing the capsule using an ultra-thin instrument (high probability of neurological complications);
- Cranial trepanation is the most radical and effective operation, combined with increased morbidity.
Video: what is an arachnoid cerebrospinal fluid cyst
Attention!
The information presented in the article is for informational purposes only.
The materials in the article do not encourage self-treatment. Only a qualified doctor can make a diagnosis and give treatment recommendations based on the individual characteristics of a particular patient. Found an error in the text?
Select it, press Ctrl + Enter and we will fix everything! Hello! My daughter is 2 years old. At birth she underwent surgery on the sacral spine. She is currently diagnosed with poppy 2, static-coordinative disorders, pelvic disorders in the form of urinary and fecal incontinence. The child feels well and is developing normally. An MRI was done at three months. : on a series of MRI tomograms, images of sub- and supratentorial structures were obtained. Focal and diffuse changes in the signal from the cortex and white matter of the brain were not detected. In the basal ganglia, internal capsule and corpus callosum, no signal changes were detected. Focal changes in the signal in the cerebellum and in the brainstem brain not identified. the median structures of the brain are not displaced. the lateral ventricles are symmetrical, expanded in the region of the anterior, posterior horns and central sections (anterior horns 19 mm, cent. sections of the bodies 20 mm) third ventricle 5 mm. fourth ventricle not expanded. Sylvian aqueduct can be traced. subarachnoid the spaces of the cerebral hemispheres and cerebellum, the interhemispheric fissure are expanded to 7-9 mm. the convexital grooves of the cerebrum are without features. the cerebellar grooves are not changed. additional formations in the area of the cerebellopontine angles have not been identified. the internal auditory canals are not expanded, symmetrical. the pituitary gland is of normal shape and size. the structure of the adenohypophysis is homogeneous. the relationship between the neuro- and adenohypophysis is preserved. the infundibulum and chiasm are not displaced. The cerebellar tonsils are located at the entrance to the foramen magnum to the depth of the bone plate. pneumatization of the paranasal sinuses corresponds to age. when performing non-invasive myelography at the level of the craniovertebral junction in the area of the bzo There is a filling defect with fixation of the cerebellar tonsils. conclusion: at the time of the MRI study, the picture was MAC2. internal occlusive compensated hydrocephalus with cerebrospinal fluid blocks at the level of the bzo. At two years old, a new examination of the brain and back was done: MRI of the spinal cord and spine: lumbosacral region. Conclusion at the time of the study: MRI picture of postoperative changes in the sacrum (herniomyeloplasty condition): open spinal canal, meningomyelocele, “fixed spinal cord” syndrome, spinal cord hypotrophy. MRI of the brain (including the craniovertebral junction) on a series of MRI scans, images of sub- and supratentorial structures were obtained. No focal and diffuse changes in the signal from the cortex and white matter of the brain were detected. There were no signal changes in the basal ganglia, internal capsule and corpus callosum determined. no focal signal changes were detected in the cerebellum and in the brain stem. the midline structures of the brain are not displaced. the lateral ventricles are symmetrical, sharply expanded in the region of the anterior, posterior horns and central sections (anterior horns 17 mm, cent. sections of the bodies 35 mm) third ventricle 13 mm .the fourth ventricle is slit-shaped. the subarachnoid spaces of the cerebral hemispheres and cerebellum are narrowed. the convexital grooves of the cerebrum and cerebellum are shortened. additional formations in the area of the cerebellopontine angles are not identified. the internal auditory canals are not expanded, symmetrical. the pituitary gland is of normal shape and size. the structure of the adenohypophysis is homogeneous .the relationship between the neuro- and adenohypophysis is preserved. the infundibulum and chiasm are not displaced. pneumatization of the paranasal sinuses corresponds to age. The cerebellar tonsils are located at the entrance to the foramen magnum to the depth of the bone plate, reaching the level of C2. The C1 arch deforms the spinal canal up to 14 mm. The diameter of the spinal canal is up to 20 mm. When performing non-invasive myelography at the level of the craniovertebral junction (along the posterior contour), a “half-filling defect” can be traced with compression of the cerebellar tonsils. The subarachnoid spaces of the cerebellar and cervical spine are narrowed. The Sylvian aqueduct is not traced. Compared to the MRI study from 2008, negative dynamics are noted. Conclusion: at the time of the MRI study, the picture was MAC2. internal occlusive compensated hydrocephalus with liquor blocks at the levels of the Sylvian aqueduct and the CVJ. Our doctor said that we need to have an operation in the sacral region. Tell me, is it possible to have this operation done at your place, what is needed for this, how much will it cost? Thanks in advance. Irkutsk. Quite often, after undergoing an MRI of the brain, you receive a doctor’s conclusion: “MR picture of liquorocystic arachnoid changes.” Many people ask what it is and whether it is very scary.
Let's answer these questions.
Diagnostics
Neuroimaging methods are used to diagnose the disease:
- . Reveals the cyst, its size and relationship to neighboring tissues.
- X-ray of the skull in two projections.
- Cisternography. After introducing a contrast agent into the body, the cavities and cisterns of the subarachnoid space are studied. Usually combined with computed tomography.
Diagnosis should be sought if the cyst causes symptoms and reduces the standard of living. With normal sizes and “acceptable” arachnoid changes, the disease in most cases is asymptomatic and does not require treatment.
Time
Question
2010-07-13 18:33:47
PLEASE CONSULT ME. I AM 26 YEARS OLD. I HAVE FEELINGS OF CONSTANT FATIGUE AND WEAKNESS, VERY POOR MEMORY, HEAVY HEAD. I DO NOT DRINK ALCOHOL, BUT I DO SMOKE. I WAS EXAMINED WITH AN MRI: A SERIES OF T1 AND T2 WEIGHTED MR TOMOGRAMS VISUALIZED SUB- AND SUPRATENORIAL STRUCTURES IN THREE PROJECTIONS. THE LATERAL VENTRICLES OF THE BRAIN ARE USUAL SIZES AND CONFIGURATIONS. THE III AND IV VENTRICLES AND BASAL CISTERNS ARE NOT CHANGED. SYLVIUS WATER PIPELINE IS VISUALIZED CLEARLY. CORPUS CALLOSUM WITHOUT FEATURES. THE CHIASMAL AREA IS WITHOUT FEATURES, THE PITITUITARY TISSUE HAS A USUAL SIGNAL. THE SUBARACHNOIDAL CONVEXITAL SPACES ARE LOCALLY NOT UNIFORMLY SLIGHTLY ENHANCED, MAINLY IN THE AREA OF THE FRONTAL PARIETAL LOBE. THE MIDDLE STRUCTURES ARE NOT DISPLACED. THE CEREBELLAR TONSILS ARE LOCATED AT THE LEVEL OF THE FORAMA magnum. NO FOCAL AND DIFFUSE CHANGES IN THE BRAIN SUBSTANCE WERE DETECTED. THE PARAGRAPHY SINUSES ARE AIR. CONCLUSION: MR PICTURE OF ARACHNOIDAL CHANGES OF LIQUIROCYSTIC CHARACTER.
ALEXEI.
(RUBTSOVSK. ALTAI REGION.)
Answer: Mark answer as helpful Votes: 184
Alexey, you were looking in the wrong place for the cause of your malaise. Changes in the brain detected on MRI cannot cause such symptoms. Take an MRI of the cervical spine using a machine with a magnetic field strength of at least 1.5 Tesla. The reason is a violation of blood circulation in the vertebrobasilar system, which supplies blood to the brain stem, occipital region of the brain, etc. This disturbance of blood circulation in the vertebral arteries is caused by either protrusions or herniations of intervertebral discs in the cervical spine. Send a description of the examination results.
Stayer Healthy Spine Clinic
Arachnoid cysts of the brain, or, as they are also called, arachnoid changes of a liquorocystic nature, are benign formations of the arachnoid membrane of the brain. The word “benign” implies that such pathologies are not prone to uncontrollable growth and metastasis, but does not mean that they are harmless.
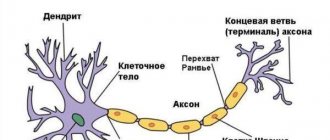
The human brain is successively covered with three membranes - hard, arachnoid and soft.
The arachnoid membrane (mater arachnoidea) is located between the hard and soft and performs the function of creating and conducting cerebrospinal fluid (CSF). Between it and the pia mater there is a space called subarachnoid, in which there are blood vessels that supply blood to the brain, and liquor cisterns (extensions of the subarachnoid space) above the most important parts of the brain.
A cyst is a bubble-shaped formation that is located under the arachnoid membrane and filled with cerebrospinal fluid. It may not manifest itself for a long time or cause serious neurological complications. It is formed when the arachnoid membrane is separated by an excess amount of cerebrospinal fluid. This creates a cavity filled with liquid. It may have a constant size, or it may slowly increase over time, causing an increase in intracranial pressure and mechanical compression of nearby parts of the brain.
Arachnoiditis - causes, signs, symptoms
First, let's deal with the concept of arachnoiditis. It is believed that various brain diseases suffered in childhood (traumatic brain injuries, microhemorrhages, latent meningitis) can cause chronic inflammation of the soft and arachnoid meninges - the so-called arachnoiditis.
...if you have been diagnosed with arachnoiditis, you should always keep in mind that it does not carry much meaning
The diagnosis of “cerebral arachnoiditis” is made clinically by neurologists, based on complaints of headaches, fatigue, attacks of nausea and vomiting, memory impairment, etc. But the difficulty is that all these symptoms are nonspecific and can have different causes, and therefore in modern medicine the diagnosis of chronic arachnoiditis is very controversial. If only because we cannot reliably prove whether there is chronic inflammation of the meninges or not. We simply do not have any methods that could reliably detect this inflammation. Therefore, if you have been diagnosed with arachnoiditis, you should always keep in mind that it does not carry much meaning.
Why is an accurate diagnosis difficult to make?
- Symptoms are not specific
- Chronic inflammation is difficult to detect
- The nature of the arachnoid cyst is difficult to determine
On MRI of the brain, arachnoiditis most often does not have reliable signs, but sometimes it can lead to the formation of cysts located in the subarachnoid space, that is, between the brain and the skull bone. These are so-called arachnoid cysts. Arachnoid cysts have clear signs on MRI. But, unfortunately, most often we cannot say whether these cysts arose as a result of arachnoiditis, or whether they are congenital. Therefore, in modern neurology, the concepts of “arachnoiditis” and “arachnoid cyst” are different, and they should not be confused.
Clinical manifestation of the disease
Arachnoid cerebrospinal fluid cysts manifest themselves in different ways, and often the symptoms do not make it possible to make a diagnosis. Here are just a few common signs:
- congenital pathologies begin to manifest themselves closer to 15-20 years, but not later;
- the nature of the symptoms is influenced by the size of the tumor formations;
- hemispheric location leads to problems with coordination, vomiting, nausea and constant headaches;
- arachnoid cyst of the posterior cranial fossa, as well as focal lesions lead to symptoms depending on the area on which the tumors press;
- general cerebral symptoms are accompanied by high blood pressure, vision problems, epilepsy and inhibited psychomotor development.
MR picture of arachnoid changes of a liquorocystic nature - what is it?
...cerebrospinal fluid cystic arachnoid changes are most often just an invention of radiologists...
Most often, the diagnosis of “arachnoid changes of a liquor cystic nature” is written when no cysts are reliably visible on MRI, but there is simply an uneven expansion of the subarachnoid space, that is, an increase in the amount of cerebrospinal fluid (CSF) between the brain and the skull bone. This expansion has nothing to do with arachnoid cysts, so liquorocystic arachnoid changes are most often just an invention of radiologists that do not have a reliable morphological basis. This term is absent in the scientific literature. You won’t find it on English-language sites, for example, on the world’s main radiology site Radiopaedia.
Treatment
If such manifestations are detected, even some of them, arachnoid changes of a liquorocystic nature can be suspected, and to make an accurate diagnosis, you should urgently contact a neurologist. This disease is more often observed in men, and mostly in children and young men. It should be taken into account that arachnoid changes of a liquorocystic nature are not a separate disease, but accompany various types of infections, circulatory disorders, as well as autoimmune phenomena.
The size of the cyst can be determined using MRI or computed tomography. Treatment is prescribed only if the cyst enlarges or there is a danger of developing new cystic formations. But in any case, the primary thing is to identify and treat the underlying disease. For this purpose, studies are carried out, based on the results of which the doctor can prescribe medication or surgical treatment, which is used only as a last resort. Surgical procedures include various endoscopic operations, or craniotomy and complete removal of the cyst.
Since cystic formations of small sizes almost do not manifest themselves and you can live to a ripe old age without suspecting the presence of a cyst, in this case no treatment is required, and arachnoid changes of a liquorocystic nature only reflect the relationship between the size of the brain and its membranes.
In the conservative treatment of the disease, drugs that affect the tone of cerebral vessels and nootropic drugs are prescribed, but all these actions should be carried out only under the supervision of a neurologist.
The human brain has several membranes. One of them is arachnoid. Below it is the subarachnoid space. It contains cerebrospinal fluid (CSF). In some cases, expansion of the space occurs and the formation of benign formations-cavities. These are arachnoid changes of a liquorocystic nature.