Neuritis is a pathology related to diseases of the nervous system.
The disease of the upper extremities occurs in four main peripheral nerves - median, ulnar, radial, brachial. With neuritis of the lower extremities, damage occurs to the femoral, tibial, peroneal, and sciatic nerves.
The disease is characterized by an inflammatory process of the nerve itself, its sheath, and the axial cylinder. In this article we will talk about neuritis of the upper and lower extremities (inflammation of the nerves in the arms and legs), symptoms and treatment of the problem.
Neuritis: main symptoms, causes, how to treat, complications
Inflammation of the nerve manifests itself in the form of sensory disturbances and motor disorders in the affected area.
If one nerve is inflamed, then this pathological process is called mononeuritis, if two or more - polyneuritis. This neuralgia may be associated with infectious diseases or hypothermia. Whatever the cause of the disease, in no case should you let it take its course or self-medicate.
If treatment is not started in a timely manner, the situation worsens; the disease becomes chronic, which is very difficult to treat.
This pathology can occur for various reasons. If mononeuritis or polyneuritis appears, the following signs appear:
- changes in skin sensitivity;
- pain at the location of the affected nerve;
- decreased muscle tone;
- malaise, weakness.
- If these signs occur, you should immediately contact a specialist.
- The most common polyneuritis and mononeuritis occur in the occipital, intercostal, and facial areas.
- The disease can be classified according to different criteria.
- The division occurs according to:
- location;
- pathomorphological changes;
- the conditions of its occurrence;
- the number of affected nerves.
By localization they are divided into:
- Optic neuritis. The cavity of the eyeball, the back of the orbit or the intracranial area is affected. If you do not go to the clinic in a timely manner, you can completely lose your vision.
- Vegetative. Any area of the human body is affected. Peripheral nerve fibers become inflamed, after which disturbances in blood circulation occur. A different shade of skin appears in the area of inflammation.
- Lesions of the cochlear nerve. Occurs after injuries to the skull, ear or infectious disease. If left untreated, deafness occurs, which later cannot be treated. A common symptom of this pathology is the appearance of noise and ringing in the ears.
According to pathomorphological changes, neuritis is as follows:
- Axial. Such inflammation disrupts the functioning of internal organs. Deviations manifest themselves in the inability to see anything with the eye. Failures can lead to the inability of the organ to function normally.
- Adventitial. During the destruction of the upper outer sheath of the nerve, this type of neuritis occurs.
- Interstitial. Manifest in the form of fiber transformations. During the examination, you can notice hemorrhage, due to which a red tint appears at the site of the pathology. Sometimes there is pus.
- Segmental. Individual small areas of nerve fibers are affected.
- Rising. This is a process in which damage occurs to the nerves located close to the initial inflammation. In this regard, even the spinal cord may be damaged.
- Parenchymatous. Damage to nervous tissue (parenchyma). Necrosis appears in neighboring areas.
- Gombo-segmental. Nerve destruction occurs partially. The center is not affected, so this pathology can be restored.
- Hypertrophic. All inflammations tend to recover over time. Hypertrophy of the vascular walls causes scars to appear, which in turn compresses certain nerve bundles and they are destroyed again.
If we take into account the conditions for the occurrence of neuritis, they are divided into:
- Infectious. Appear as a complication after infectious diseases (diphtheria, measles, scarlet fever, rubella). Toxic substances that spread throughout the body quickly give rise to new foci of the inflammatory process.
- Vibrating. If people's professions are associated with constant vibration, then they may suffer from such a disease. Oppression of the hand or foot occurs. In most cases, miners, drillers and construction workers suffer.
- Traumatic. Appear after accidents, bruises, falls, after which bone fractures occur. Another reason is prolonged compression of some part of the body.
- Toxic. The ulnar nerves suffer if heavy metal affects the body. Peroneal nerves, if affected by alcohol. Toxic poisoning can occur in the workplace when working with mercury or zinc.
- Endemic. Appears when there is a lack of nicotinic acid or B vitamins in the body. Frequent victims are patients with diabetes and pregnant women who have toxicosis.
If we take into account the number of affected nerves, neuritis is divided into two types:
- Multiple lesions - polyneuritis.
- Single - mononeuritis.
If any of the above processes are diagnosed early, the pathology can be cured.
The disease can occur due to external or internal reasons.
With internal causes, various diseases affect inflammation of the nerves. With external ones, the action comes from the environment.
These include:
- infectious diseases (influenza, scarlet fever, measles, herpes, polyarthritis, rubella, etc.);
- presence of diabetes mellitus;
- various stages of obesity;
- osteochondrosis and intervertebral hernia;
- circulatory disorders;
- thyrotoxic goiter;
- poisoning (alcohol, drugs, mercury, zinc, drugs, etc.);
- lack of B vitamins and nicotinic acid;
- various injuries (fractures, dislocations, wounds, unskilled injection, poorly performed surgery, etc.);
- last trimester of pregnancy (associated with excessive stress on the spine);
- hypothermia.
Regardless of what caused the inflammation of the nerve, only a highly qualified specialist should treat the disease.
Symptoms of the disease will vary depending on the nerve affected. Common signs include:
- numbness of the affected area;
- feeling of goosebumps and tingling;
- poor sensitivity;
- pain when working or staying in one position for a long time;
- weakness and lethargy in the muscles (if left untreated there will be complete atrophy);
- poor motor activity;
- poor functioning of the glands of the skin and organs.
Swelling and blue discoloration may occur in the area where inflammation is localized.
Most often it happens:
- Neuritis in the forearm (radial, ulnar and median). There is a violation of bone mobility. It is difficult to bend your arm and move the phalanges of your fingers. My hand goes numb.
- Femoral neuritis. The knee and hip joints bend poorly. There is poor sensitivity on the front surface of the thigh below and inside the side of the shin. Muscle mass decreases in size and weakens.
- Peroneal neuritis. There is lameness due to the pain of standing on the heels. There is also shuffling and stumbling. When walking, a person lifts his feet strongly upward when he brings them forward.
- Facial neuritis. The affected part of the face immobilizes and relaxes. There is asymmetry. The eye cannot close, the forehead does not wrinkle. Pain behind the ear may occur, and half of the lips lose mobility.
The disease can be noticed immediately, since the signs of neuritis are very specific.
With signs of an inflamed nerve, the patient is sent to see a neurologist. The doctor conducts an examination and functional tests. They determine movement disorders.
https://www.youtube.com/watch?v=tbi1K2_q3Rc
If a person has radial neuritis, then:
- when the hands are on the table surface with palms up, the thumb is not moved to the side;
- if the patient is in an upright position, with his arms down along his body, he is not able to turn the hand with the palm forward and move the thumb.
When a patient has median neuritis, then:
- a person cannot make scratching movements on the surface of the table if the palm is located on its surface;
- It is not possible to make a contrast between the little finger and the thumb.
For ulnar mononeuritis or polyneuritis:
- the patient is unable to spread the phalanges of the fingers when the palms are on the table surface;
- it is impossible to bend your hand into a fist;
- You cannot take a piece of paper between your index finger and thumb.
The patient may be referred by a doctor for a CT or MRI.
Electroneurography is used to measure the speed of transmission of a nerve impulse through peripheral nerve fibers. Using this technique, it is possible to identify pathology, discover where it is localized, and at what stage it is.
Electromyography is done to evaluate the bioelectrical activity of muscle tissue. This makes it possible to determine the functional state of the nerves and understand how far everything has gone.
Evoked potentials are a study of the bioelectrical activity of nerves. Neurologists use this method to study how the autonomic nervous system functions and evaluate the visual and auditory nerves.
After a complete examination of the patient has been carried out, the causes of the disease and its degree have been determined, it is necessary to eliminate all the factors that provoked this pathology. This is done so as not to aggravate the situation and cause complications.
The result and effectiveness of treatment depends on age, type of disease and therapy. All medications and physiotherapeutic procedures are used only after prescription by the attending physician:
- Bacterial mononeuritis and polyneuritis are treated with antibiotics and sulfonamides.
- Viral - “Gamma globulin” and “Interferon”.
- Traumatic - complete immobilization of the affected part of the body, anti-inflammatory and painkillers are used. At the same time, you should take B vitamins and biogenic stimulants for 3 to 6 weeks (according to indications).
- Vascular - treated with vasodilating drugs (Complamin, Papaverine, Eufillin). If necessary, Hydrocortisone with Novocaine is administered.
If the neurosurgeon decides that surgery is inevitable, then surgery is performed. During it, the compressed nerve is released. Plastic surgery or stitching is done, so the functionality of the damaged area is restored.
Medicines for neuritis are usually anti-inflammatory. Physiotherapy, normalization of water-salt balance, and intake of vitamin complexes are required.
Anticonvulsants and antidepressants are prescribed if inflammation occurs in the area of the glossopharyngeal or trigeminal nerve.
Physiotherapy refers to the use of:
- ultrasound;
- pulse current;
- exposure to high-frequency currents;
- electrophoresis.
All of the above procedures can restore functionality to the damaged nerve.
If there are no contraindications, then massage therapy and exercise therapy are advisable. If recovery does not occur for a long time, then inductophoresis procedures, chamber hydrogalvanic sessions, mud and radon baths may be prescribed.
If you do not seek medical help in a timely manner, complications may arise in the form of motor disorders, paralysis, and complete muscle atrophy.
Rational treatment will help to avoid serious consequences and quickly return to a full life. In most cases, after quality treatment by a specialist, complete recovery and recovery occurs.
Nerve inflammation is a serious disease that requires early treatment. To avoid its occurrence, you should eat well, monitor your health, treat all infectious diseases in a timely manner, harden yourself, and avoid hypothermia. It is impossible to treat neuritis on your own, since without examination the treatment will not be beneficial.
Symptoms of neuritis of the upper extremities
Shoulder (plexus brachialis)
The disease is preceded by a spasm of the muscular system of the inflamed area . This spasm may feel like an involuntary muscle contraction or twitching. Often the first symptoms of brachial neuritis go unnoticed by patients.
As inflammation increases, swelling appears. The swelling causes compression of the nerve plexus of the brachial region. When pinched, pain occurs.
Painful sensations can manifest themselves in the form of cutting, burning sharp pains . Sharp pain may occur periodically, layered with a dull, aching pain.

Discomfort and pain spread from the shoulder to the entire arm.
But this manifestation is not the rule, and the pain can be localized, directly in the shoulder area. The supraclavicular brachial plexuses are more often susceptible to neuritis than the subclavian plexuses .
With significant inflammation, pain can radiate to the chest, shoulder blade, or the side where the source of inflammation is located.
Patients also note such sensations as:
- tingling;
- goosebumps;
- numbness;
- limited movement.
Disease of the shoulder region often causes the inability to fully raise the arm, place it behind the back, move it to the side as much as possible, and sometimes even grasp an object tightly.
Elbow (n. ulnaris)
Clinical picture of inflammation n. ulnaris appears more intensely than in the shoulder area . The degree of manifestation of symptoms is influenced by the level of physical activity/stress, the area and involvement of innervated tissues in the inflammatory process.

Symptoms of ulnar nerve neuritis:
- numbness;
- paresthesia (pins and needles);
- hypersensitivity or lack of perception of tactility of the palm in part of the ring finger and the entire little finger;
- limitation or complete loss of motor activity, especially the fingers mentioned in the previous paragraph.
As the inflammatory process increases, numbness and loss of motor activity can spread to the muscles of the little finger and thumb.
Visually, the palm with atrophied muscles, as a result of damage to the ulnar region, looks flattened.
The hand resembles the paw of a bird of prey with claws when the fingers are bent above the middle phalanges and the rest are in a straight position.
Atrophy of the muscular skeleton develops in the area of inflammation and reflex contraction of the tendons decreases. Often, carpal tunnel syndrome occurs in the affected arm.
Median (n. medianus)
In order to clench your hand into a fist, you have to make the maximum possible effort, but even this does not lead to the expected result - this symptom is characteristic of median neuritis.
The surface of the palm is insensitive or slightly sensitive to any touch. A person does not distinguish between cold and hot, sharp and dull.
Angioneurosis is a disease of the vascular nerves
Violation of the function of narrowing or dilation of blood vessels can also occur due to the fault of nerves. The vasomotor nerves are responsible for this function. Thus, angioneurosis is a vascular disorder associated with a disorder of the peripheral nervous system. Angioneurosis is a disease that most often affects young women.
As angioneurosis progresses, attacks become more frequent, pain appears, and the lower extremities may turn blue and become blistered. At the critical stage of angioneurosis, the nail phalanges die. The causes of angioneurosis are the same factors as those of the previously discussed neurological diseases.
These are intoxication with harmful substances and alcohol, infections, physical and mental injuries, frostbite of the extremities, hormonal disorders, finger injuries and vibration in industrial activities. This neurogenic disease is incurable and becomes chronic.
Drug treatment and physiotherapy improve quality of life, relieve pain and slow down the development of angioneurosis. The patient himself can reduce the symptoms of angioneurosis. You need to give up bad habits, follow a diet rich in vitamins C and PP, avoid hypothermia and, if possible, avoid stress in your life.
Neuritis, polyneuritis and angioneurosis often develop as a secondary disease. Therefore, it is so important to monitor your health, not to neglect the underlying disease and promptly treat neurological disorders. Take care of your nervous system!
Diagnostics
With signs of an inflamed nerve, the patient is sent to see a neurologist. The doctor conducts an examination and functional tests. They determine movement disorders.
If a person has radial neuritis, then:
- when the hands are on the table surface with palms up, the thumb is not moved to the side;
- if the patient is in an upright position, with his arms down along his body, he is not able to turn the hand with the palm forward and move the thumb.
When a patient has median neuritis, then:
- impaired flexion of the hand and fingers in the interphalangeal joints,
- impaired sensitivity on the lateral surface of the palm and 1-4 fingers;
- It is not possible to make a contrast between the little finger and the thumb.
For ulnar neuritis:
- the patient is unable to spread the phalanges of the fingers when the palms are on the table surface;
- deformation of the hand like a “bird’s paw” as a result of paralysis and atrophy of the small muscles of the hand;
- pain and decreased sensitivity on the 5th and 4th fingers.
The patient may be referred by a doctor for a CT or MRI.
Electroneurography is used to measure the speed of transmission of a nerve impulse through peripheral nerve fibers. Using this technique, it is possible to identify pathology, discover where it is localized, and at what stage it is.
Electromyography is done to evaluate the bioelectrical activity of muscle tissue. This makes it possible to determine the functional state of the nerves and understand how far everything has gone.
Evoked potentials are a study of the bioelectrical activity of nerves. Neurologists use this method to study how the autonomic nervous system functions and evaluate the visual and auditory nerves.
Inflammation of the occipital nerve
Inflammation of the occipital nerve leads to frequent headaches. Pain occurs in the back of the head and radiates to the front and sides of the head. Often, patients describe pain similar to what they experience with migraine. The scalp can also become very sensitive to various types of touch. For example, even when trying to comb your hair, unpleasant painful sensations occur.
By the way, with occipital inflammation of the nerve endings, doctors often encounter some difficulties. They are due to the fact that it is often difficult at this stage to distinguish inflammation from other causes that cause headaches. Therefore, the patient is obliged to describe all the symptoms present in as much detail as possible and honestly answer the doctors’ questions.
If headaches bother you constantly, you should immediately consult a specialist. In this case, taking exclusively painkillers, which the patient chooses at his own discretion at the pharmacy, is not enough. Doctors often conduct complex diagnostics, including computed tomography and magnetic resonance imaging.
If the inflammation does not require surgical intervention, the doctor will prescribe treatment aimed at relieving pain. Drug treatment is combined with physiotherapy procedures and massage. In addition, doctors recommend getting more rest. Additionally, a course of anticonvulsants and steroidal anti-inflammatory drugs may be prescribed.
Cases where surgical intervention is required to treat a disease occur less frequently. For chronic pain and lack of positive results from conservative treatment methods, surgery is indicated.
Consequences and complications
If you do not seek medical help in a timely manner, complications may arise in the form of motor disorders, paralysis, and complete muscle atrophy.
Rational treatment will help to avoid serious consequences and quickly return to a full life. In most cases, after quality treatment by a specialist, complete recovery and recovery occurs.
Nerve inflammation is a serious disease that requires early treatment. To avoid its occurrence, you should eat well, monitor your health, treat all infectious diseases in a timely manner, harden yourself, and avoid hypothermia. It is impossible to treat neuritis on your own, since without examination the treatment will not be beneficial.
Diagnosis and treatment
Making a diagnosis involves a direct examination of the patient, collection of anamnesis, collection of biomaterial for analysis - blood and
urine. It is also necessary to refer the patient for electroneurography (assessment of nerve conductivity) and examination by a highly specialized specialist.
Correct and effective treatment begins with eliminating the root cause that provoked the inflammatory process that affects the nerve endings:
- If the cause is an infectious lesion of the nervous system, then the doctor prescribes a course of antibiotics, plus antiviral drugs such as Gamma globulin or Interferon.
- If ischemia develops, the doctor prescribes a course of drugs that stimulate the work and dilation of blood vessels, for example, Papaverine and Eufillin.
- In case of traumatic damage to the nerve ending, during the treatment process the doctor prescribes analgesics, as well as anti-inflammatory and painkillers such as Ibuprofen and Diclofenac. Doctors are required to prescribe medications that relieve swelling, vitamin complexes containing large quantities of B vitamins. Finally, the patient is prescribed a course of physiotherapeutic procedures - UHF heating, a course of therapeutic exercises and massage, which allows you to restore and normalize muscle function.
- If there is severe infringement of the nerve ending, surgical intervention may be prescribed, when neurosurgeons free the pinched ending or the entire nerve.
In the absence of timely diagnosis and treatment, the patient may develop the following negative consequences:
- failure in the motor functions of the limbs, the whole body, up to the development of complete or flaccid paralysis;
- impairment, complete or partial loss of sensitivity, as well as the development of muscle tissue atrophy.
Treatment with drugs for neuropathy of the lower extremities
Neuropathy of the lower extremities is a serious disease of the nervous system. Its treatment is carried out using various drugs, as well as physiotherapy, special procedures, and physical education.
What is lower extremity neuropathy?
Neuropathy is damage to peripheral nerves and the vessels that supply them. Initially, this disease is not inflammatory in nature, but later it can be layered with neuritis - inflammation of the nerve fibers. Neuropathy of the lower extremities is included in the group of polyneuropathies, the basis of which is metabolic disorders, tissue ischemia, mechanical damage, and allergic reactions.
Neuropathy is classified according to the type of course:
- spicy;
- chronic;
- I'll sharpen it up.
According to the type of pathological process in nerve fibers, neuropathy can be axonal (encompasses the processes of neurons - axons) and demyelinating (extends to the sheaths of nerve fibers). According to the symptoms, the pathology is:
- Touch
. Symptoms of sensory impairment and pain predominate. - Motor
. It manifests itself mainly as movement disorders. - Vegetative
. Signs of vegetative and trophic disorders are noted.
The causes of the pathology are varied. Thus, the diabetic form is characteristic of metabolic disorders in neurons in diabetes mellitus. Toxic, alcoholic is caused by poisoning, intoxication. Other possible causes are tumors, deficiency of vitamins B, hypothyroidism, HIV, trauma, family history.
Sensory disorders - the main group of symptoms
Manifestations of pathology in the leg area can be varied, often depending on the cause of neuropathy. If the disease is caused by injury, symptoms affect one limb. In diabetes mellitus and autoimmune diseases, symptoms spread to both legs.
Sensory disturbances can be so unpleasant that they cause depression in the patient.
Sensory disturbances occur in all cases of lower extremity neuropathy. Symptoms are usually observed constantly, do not depend on body position, daily routine, rest, and often cause insomnia.
- numbness of the legs;
- crawling sensation;
- sensation of the presence of foreign objects under the skin.
In addition to the described signs, there are often sensory disturbances - slow recognition of cold and hot, changes in the pain threshold, regular loss of balance due to decreased sensitivity of the feet. Pains also often appear - aching or cutting, weak or literally unbearable, they are localized in the area of the affected area of the nerve.
Other signs of the disease
As the pathology of the extremities develops, the motor nerve fibers are damaged, and therefore other disorders occur. These include muscle spasms, frequent cramps in the legs, especially in the calves.
If the patient visits a neurologist at this stage, the doctor notes a decrease in reflexes - knee and Achilles. The lower the reflex strength, the further the disease has progressed.
In the final stages, tendon reflexes may be completely absent.
Muscle weakness is an important sign of leg neuropathy, but it is characteristic of the later stages of the disease. At first, the feeling of muscle weakening is transient, then it becomes permanent. In advanced stages this leads to:
- decreased activity of the limbs;
- difficulty moving without support;
- muscle thinning and atrophy.
Vegetative-trophic disorders are another group of symptoms for neuropathy. When the autonomic part of the peripheral nerves is affected, the following symptoms occur:
- hair falls out on the legs;
- the skin becomes thin, pale, dry;
- areas of excessive pigmentation appear;
- the work of the sweat and sebaceous glands changes.
In patients with neuropathy, cuts and abrasions on the legs do not heal well; they almost always fester. Thus, with diabetic neuropathy, changes in trophism are so severe that ulcers appear, and sometimes the process is complicated by gangrene.
The procedure for diagnosing pathology
An experienced neurologist will easily make a presumptive diagnosis based on the symptoms described according to the patient and on the available objective signs - skin changes, impaired reflexes, etc.
Diagnostic methods are very diverse, here are some of them:
| Methodology | What does it show |
| Electroneuromyography | Determining the source of damage to the nervous system - roots, nerve processes, neuron bodies, membranes, etc. |
| General, biochemical blood test | Inflammatory, infectious process, presence of autoimmune changes |
| Blood sugar test | Development of diabetes mellitus |
| X-ray of the spine | Pathologies of the spinal column |
| Spinal tap | Presence of antibodies to own nerve fibers in the spinal cord |
The main method for diagnosing problems with nerve fibers remains the simple technique of electroneuromyography - it helps to clarify the diagnosis.
Neuropathy Treatment Basics
This disease must be treated comprehensively, always with correction of the underlying pathology. For autoimmune diseases, hormones and cytostatics are prescribed; for diabetes, glucose-lowering medications or insulin; for toxic types of disease, cleansing techniques (hemosorption, plasmapheresis).
The goals of treatment for lower extremity neuropathy are:
- restoration of nervous tissue;
- resumption of conductivity;
- correction of disorders in the circulatory system;
- improvement of well-being;
- reduction of pain and other disorders;
- optimization of motor function of the legs;
- increasing metabolic rate.
There are many treatment methods, the main one being medication.
Surgical treatment is practiced only in the presence of tumors, hernias, and after injuries. To prevent muscle atrophy, all patients are recommended to exercise from a special exercise therapy complex; at first, they are performed under the supervision of a rehabilitation physician.
If you have neuropathy, you should follow a diet with an increase in the content of vitamins B, and you should also exclude alcohol, foods with chemical additives, marinades, fried, and smoked foods.
The disease is successfully treated with physiotherapy. Massage, magnetic therapy, therapeutic mud, reflexology, and electrical muscle stimulation have proven themselves to be excellent.
To prevent the formation of ulcers, you should wear special shoes and use orthoses.
Basic drugs for the treatment of pathology
In the treatment of neuropathy, drugs play a leading role. Since the basis is degeneration of nerve tissue, the structure of the nerve roots should be replenished with medication. This is achieved by using the following medications:
- Neuroprotectors
, accelerators of metabolism in nerve cells - Piracetam, Mildronate. They improve the trophism of nervous tissue, helping to improve its structure. - Anticholinesterase drugs
– Ipidacrine, Prozerin. They optimize the sensory functioning of nerves and help in the transmission of nerve impulses. - Antioxidants
– Mexidol, Cytoflavin. They help to “quench” the action of free radicals, which aggravate the destruction of peripheral nerves. - Alpha lipoic acid preparations
. They enhance metabolism, enhance the restoration of neurocytes, especially indicated for diabetic neuropathy.
B vitamins are mandatory in the course of therapy, especially B12, B6, B1. Most often, combined drugs are prescribed - Neuromultivit, Milgamma in tablets, injections. After taking them, sensitivity disorders are eliminated, all symptoms are reduced in severity.
What else is used to treat neuropathy?
Vitamins that are powerful antioxidants - ascorbic acid, vitamins E, A are very useful for the body in any form of neuropathy of the lower extremities. They are necessarily used in complex therapy of the disease to reduce the destructive effects of free radicals.
In case of severe muscle spasms, the patient will be helped by muscle relaxants - Sirdalud, Baclofen, which are used only with a doctor's prescription - if abused, they can increase muscle weakness.
There are other medications against this pathology. They are selected individually. These are:
- hormonal agents to suppress pain, inflammation - Prednisolone, Dexamethasone
; - vascular medications to improve blood circulation in tissues - Pentoxifylline, Trental
; - antidepressants, sedatives, drugs against excessive anxiety - Amitriptyline, Duloxetine
; - analgesics, including narcotics for severe pain - Tramadol, Analgin, as well as NPVS - Ketoprofen, Ketonal Duo
.
Locally it is recommended to use ointments with novocaine, lidocaine, non-steroidal anti-inflammatory drugs, as well as warming ointments with red pepper and animal poisons. In case of bacterial infection of the skin of the feet and legs, bandages with antibiotics are applied (Tetracycline ointment, Oxacillin).
Traditional treatment of neuropathy
Treatment with folk remedies is used with caution, especially for diabetes. Recipes can be like this:
- Combine the yolk of a raw egg and 2 tablespoons of olive oil. Add 100 ml of carrot juice, a tablespoon of honey. Drink 50 ml three times a day after meals. Course – 14 days.
- Pour 2/3 cup of 9% vinegar into a bucket of warm water, add a glass of salt. Soak your feet in the water for 15 minutes. Course – once a day for a month.
- Mix 3 tablespoons of fenugreek seeds, a tablespoon of bay leaf, chop everything. Brew a liter of boiling water in a thermos for an hour, then drink in small portions throughout the day. Course – 10 days.
- Dilute blue clay with water to a paste and apply to feet. Let it dry, then rinse off. Repeat every day for 2 weeks.
With timely treatment, the disease has a good prognosis. Even if the cause of neuropathy is very severe, it can slow or stop its progression and improve a person's quality of life.
i
Please rate the article, we tried:
Source: https://netbolezni.net/nevrologiya/247-lechenie-preparatami-neyropatii-nizhnih-konechnostey.html
Diseases arising from inflammation of the nerves
Due to the fact that the inflammatory process is the infringement of the nerve ending, this can lead to the development of many neurological diseases. In particular, with inflammation of the nerve endings of one location or another, the patient may develop the following symptoms:
- Inflammation of the optic nerve roots and, as a result, the appearance of fog before the eyes, problems with visual acuity, pain when moving the eyeball.
- An inflammatory process affecting the hearing aid - in this case, the patient hears poorly and is bothered by tinnitus. If the inflammatory process spreads to the nerve surrounding the brain and the vestibular apparatus, the patient may experience fainting and dizziness, nausea and vomiting, and sensorineural hearing loss may develop.
- Inflammation of the nerve ending can also lead to damage to the facial nerve and, as a result, the lower lip will be displaced downward, the palpebral fissure will widen, and the patient will lose the ability to control facial wrinkles.
- Inflammation of the end of the radial nerve leads to the patient developing drop hand syndrome - the inability to straighten the forearm, wrist, and loss of sensitivity on the back of the hand.
- Inflammation of the nerve endings affecting the endings of the fibular nerve leads to the development of the syndrome of hanging lower limbs - the patient loses the ability to fully move and stand on his heels. His gait changes and muscle atrophy occurs at the site of the inflammatory process and pinching of the nerve ending.
- The inflammatory process and damage to the end of the brachial nerve leads to attacks of pain in the joint, inability to fully move the arm, muscle weakness is diagnosed, and sensitivity of the dermis at the site of inflammation.
- Solaritis - we are talking about inflammation of the end of the solar plexus nerve, acute pain is felt in the chest.
As you can see, inflammation of the nervous system can be localized anywhere - it can be the eyes and shoulders, arms and legs, the solar plexus area, the face and the hearing aid.
Most often, inflammation and, accordingly, infringement of the end of the nerve process affects the facial, optic and tibial nerves - the nervous system permeates the entire body of the patient, which determines that the location of the neuritis can be anywhere.
Symptoms depending on location
The symptoms of inflammation depend on which nerve or its ending is affected. However, doctors identify common symptoms that are generally characteristic of inflammation of the nerve ending:
- attacks of neuropathic pain , which intensify during physical exertion, during hypothermia, or after a long stay in an uncomfortable position;
- loss of sensitivity and numbness , a feeling of tingling and crawling “goosebumps” throughout the body;
- inability to fully move the limbs , muscles weaken, may gradually atrophy and decrease in size;
- there is a malfunction in the functioning of the vascular system, internal glands of organs and systems , as a result of which the patient sweats excessively, cyanosis and swelling appear on the skin.
Treatment of inflammatory diseases
Symptoms of infectious neuritis of the sciatic, tibial, femoral and knee nerves can be relieved by taking antibacterial drugs. Additionally, treatment with non-steroidal, anti-inflammatory, antiviral drugs, muscle relaxants, and vitamin therapy is prescribed.
If the symptoms of neuralgia are caused by dilation of blood vessels, ischemia, thrombophlebitis, treatment with vasodilators is prescribed. In case of injury, the limb is fixed and, if necessary, a plaster or tight bandage is applied. The patient is prescribed bed rest; he needs to sleep on a hard mattress.
If the pain is too severe, it must be stopped with novocaine or hormonal blockade.
After acute symptoms are relieved, patients are treated with physiotherapeutic procedures: massage, electrophoresis, exercise therapy, UHF, electromyostimulation, manual therapy. For carpal tunnel syndrome, medications are injected directly into the affected canal.
When medication and physiotherapeutic procedures do not help relieve pain, the patient’s condition worsens, and surgery is performed. In this way, decompression of the pinched femoral or tibial nerve is performed.
Inflammation of the sciatic, femoral, tibial and peroneal nerves in young people responds well to therapy, treatment has a positive prognosis. In elderly patients suffering from diabetes, the disease is progressive, and paralysis of muscle tissue and deformation of the joints of the foot may develop.
Pain is the main signal that an unnatural, inflammatory process is occurring in the body, affecting one or another organ or system.
So, inflammation of the nerve endings can cause a lot of pain and neurological problems - numbness and flaccid paralysis, loss of performance, and so on.
Inflammation of nerve endings is an inflammatory process that occurs in the body and affects nerve fibers, endings, and as a result, the development of neuritis occurs.
Doctors distinguish two types of neuritis - primary, which in turn is divided into colds, tunnel or ischemic, and secondary, developing against the background of other neurological pathologies, or as a consequence of their development.
A drug for restoring nerve fibers and damaged endings
The central nervous system (CNS) is a single mechanism that is responsible for the perception of the surrounding world and reflexes, as well as for controlling the system of internal organs and tissues.
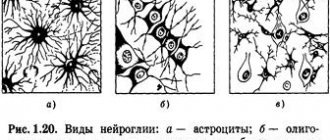
The last point is performed by the peripheral part of the central nervous system with the help of special cells called neurons. They make up the nervous tissue, which serves to transmit impulses. The processes coming from the body of the neuron are surrounded by a protective layer that nourishes the nerve fibers and accelerates impulse transmission, and this protection is called the myelin sheath. Any signal transmitted along nerve fibers resembles a current discharge, and it is their outer layer that prevents its strength from decreasing.
If the myelin sheath is damaged, then full perception in this part of the body is lost, but the cell can survive and the damage will heal over time. If the injuries are quite serious, you will need drugs designed to restore nerve fibers like Milgamma, Copaxone and others.
Otherwise, the nerve will die over time and perception will decrease. Diseases that are characterized by this problem include radiculopathy, polyneuropathy, etc., but doctors consider multiple sclerosis (MS) to be the most dangerous pathological process.
Despite the strange name, the disease has nothing to do with the direct definition of these words and, when translated, means “multiple scars.” They arise on the myelin sheath in the spinal cord and brain due to immune failure, which is why MS is classified as an autoimmune disease.
Instead of nerve fibers, a scar consisting of connective tissue appears at the site of the lesion, through which the impulse can no longer pass correctly.
Is it possible to somehow restore damaged nerve tissue or will it forever remain in a crippled state is a relevant question to this day.
Doctors still cannot answer this question accurately and have not yet come up with a full-fledged drug to restore sensitivity to nerve endings.
Instead, there are various medications that can reduce the process of demyelination, improve nutrition of damaged areas and activate the regeneration of the myelin sheath.
Milgamma
Milgamma is a neuroprotector for restoring metabolism inside cells, which allows you to slow down the process of myelin destruction and begin its regeneration. The drug is based on vitamins from group B, namely:
- Thiamine (B1). It is essential for the absorption of sugar in the body and the production of energy. With acute thiamine deficiency, a person's sleep is disturbed and memory deteriorates. He becomes nervous and sometimes depressed, as in depression. In some cases, symptoms of paresthesia are observed (goose bumps, decreased sensitivity and tingling in the fingertips);
- Pyridoxine (B6). This vitamin plays an important role in the production of amino acids, as well as some hormones (dopamine, serotonin, etc.). Despite rare cases of a lack of pyridoxine in the body, due to its deficiency, a decrease in mental abilities and a weakening of the immune defense are possible;
- Cyanocobalomin (B12). It serves to improve the conductivity of nerve fibers, resulting in improved sensitivity, as well as to improve blood synthesis. With a lack of cyanocobalamine, a person develops hallucinations, dementia (dementia), disturbances in heart rhythm and paresthesia are observed.
Thanks to this composition, Milgama is able to stop the oxidation of cells by free radicals (reactive substances), which will affect the restoration of sensitivity of tissues and nerve endings.
After a course of taking pills, there is a decrease in symptoms and an improvement in general condition, and the drug must be taken in 2 stages.
In the first, you will need to make at least 10 injections, and then switch to tablets (Milgamma compositum) and take them 3 times a day for 1.5 months.
Stephaglabrine sulfate
Staphaglabrine sulfate has been used for quite a long time to restore the sensitivity of tissues and the nerve fibers themselves. The plant from whose roots this drug is extracted grows only in subtropical and tropical climates, for example, in Japan, India and Burma, and it is called smooth stephania. There are known cases of obtaining Stafaglabrine sulfate in laboratory conditions.
Perhaps this is due to the fact that stephania smooth can be grown as a suspension culture, that is, suspended in glass flasks with liquid. The drug itself is a sulfate salt, which has a high melting point (more than 240 ° C).
It refers to the alkaloid (nitrogen-containing compound) stepharine, which is considered the basis for proaporphine.
Stephaglabrin sulfate serves to reduce the activity of enzymes from the class of hydrolases (cholinesterase) and to improve the tone of smooth muscles that are present in the walls of blood vessels, organs (hollow inside) and lymph nodes. It is also known that the drug is slightly toxic and can reduce blood pressure.
In the old days, the medicine was used as an anticholinesterase agent, but then scientists came to the conclusion that Stefaglabrin sulfate is an inhibitor of connective tissue growth activity. From this it turns out that it delays its development and scars do not form on the nerve fibers.
That is why the drug began to be actively used for injuries to the PNS.
During the research, specialists were able to see the growth of Schwann cells, which produce myelin in the peripheral nervous system.
This phenomenon means that under the influence of the medication the patient noticeably improves the conduction of impulses along the axon, since the myelin sheath begins to form around it again.
Since the results were obtained, the drug has become hope for many people diagnosed with incurable demyelinating pathologies.
It will not be possible to solve the problem of autoimmune pathology only by restoring nerve fibers. After all, no matter how many lesions have to be eliminated, the problem will return, since the immune system reacts to myelin as a foreign body and destroys it.
Today it is impossible to eliminate such a pathological process, but you no longer have to wonder whether the nerve fibers are being restored or not.
People are left to maintain their condition by suppressing the immune system and using drugs like Stefaglabrin sulfate to maintain their health.
The drug can only be used parenterally, that is, past the intestines, for example, by injection. The dosage should not exceed 7-8 ml of 0.25% solution per day for 2 injections.
Judging by time, usually the myelin sheath and nerve endings are restored to some extent after 20 days, and then a break is needed and you can understand how long it will last by asking your doctor about it.
The best result, according to doctors, can be achieved through low doses, since side effects develop much less frequently, and the effectiveness of treatment increases.
In laboratory conditions, during experiments on rats, it was found that with a concentration of the drug Stefaglabrin sulfate of 0.1-1 mg/kg, treatment proceeds faster than without it.
The course of therapy ended earlier when compared with animals that did not take this medicine. After 2-3 months, the rodents’ nerve fibers were almost completely restored and the impulse was transmitted along the nerve without delay.
In the experimental subjects who were treated without this medication, recovery lasted about six months and not all nerve endings returned to normal.
Copaxone
There is no cure for multiple sclerosis, but there are drugs that can reduce the effect of the immune system on the myelin sheath, and these include Copaxone. The essence of autoimmune diseases is that the immune system destroys the myelin located on nerve fibers.
Because of this, the conductivity of impulses deteriorates, and Copaxone is able to change the target of the body’s defense system to itself. The nerve fibers remain untouched, but if the body’s cells have already begun to corrode the myelin sheath, then the drug will be able to push them aside.
This phenomenon occurs because the drug is very similar in structure to myelin, so the immune system switches its attention to it.
The drug is capable of not only attacking the body’s defense system, but also producing special cells of the immune system to reduce the intensity of the disease, called Th2 lymphocytes. The mechanism of their influence and formation has not yet been thoroughly studied, but there are various theories. There is an opinion among experts that dendritic cells of the epidermis are involved in the synthesis of Th2 lymphocytes.
The produced suppressor (mutated) lymphocytes, entering the blood, quickly penetrate into the part of the nervous system where the source of inflammation is located. Here, Th2 lymphocytes, due to the influence of myelin, produce cytokines, that is, anti-inflammatory molecules. They begin to gradually relieve inflammation in this area of the brain, thereby improving the sensitivity of nerve endings.
The drug has benefits not only for the treatment of the disease itself, but also for the nerve cells themselves, since Copaxone is a neuroprotector. The protective effect is manifested in stimulating the growth of brain cells and improving lipid metabolism.
The myelin sheath mainly consists of lipids, and in many pathological processes associated with damage to nerve fibers, they are oxidized, so the myelin is damaged. The drug Copaxone can eliminate this problem, as it increases the body's natural antioxidant (uric acid).
It is not known why the level of uric acid increases, but this fact has been proven in numerous experiments.
The drug serves to protect nerve cells and reduce the severity and frequency of exacerbations. It can be combined with medications Stefaglabrin sulfate and Milgamma.
The myelin sheath will begin to recover due to the increased growth of Schwann cells, and Milgamma will improve intracellular metabolism and enhance the effect of both drugs. Using them yourself or changing the dosage yourself is strictly prohibited.
Whether it is possible to restore nerve cells and how long it will take only a specialist can answer, based on the results of the examination. It is prohibited to take any medications on your own to improve tissue sensitivity, since most of them are hormonal and therefore difficult to tolerate by the body.
Source: https://NashiNervy.ru/o-nervnoj-sisteme/meditsinskie-preparaty-dlya-vosstanovleniya-nervnyh-tkanej.html
Drug therapy
The patient is given a course of treatment with the following medications:
- vasoactive drugs to improve tissue nutrition (Trental, Emoxipin, Nicotinic acid and others);
- antioxidants (vitamin E, Actovegin, Mexidol, etc.);
- B vitamins to improve conductivity and restore nerve sheaths;
- anticholyesterase drugs that improve the conduction of nerve impulses (Amiridine, Epidacrine);
- Muscle relaxants are used with some caution to restore muscles (Mydocalm, Baclofen), but it should be remembered that they are not suitable for all patients (they can increase muscle weakness);
- non-steroidal anti-inflammatory drugs (Nimesulide, Ketoprofen, Meloxicam), as well as ointments and patches containing them (Lidocaine ointment, Voltaren patch and others) are used for pain relief;
- antidepressants (Duloxetine, Sertraline, Ketadolon);
- anticonvulsants (Pregabalin, Neurontin);
- in severe cases, narcotic painkillers (Tramadol, etc.) are prescribed to relieve pain.
In addition to the listed medications, the patient is prescribed drugs and procedures to combat the underlying disease. In the case of diabetes, these will be drugs that correct blood sugar levels. For toxic neuropathy, measures are taken to cleanse the body of toxins. For pathologies of the thyroid gland, autoimmune diseases, hormonal therapy is possible, and so on.
Vitamins for the conduction of nerve impulses
Polyneuropathy of the lower extremities is a common pathology of the peripheral nervous system.
The structural features of the terminal sections of nerves make them extremely vulnerable to the influence of a variety of pathological factors.
Regardless of the nosological form of polyneuropathy, it is based on demyelination of nerve fibers.
Therefore, the main goal when prescribing drugs for the treatment of polyneuropathy of the lower extremities is to restore impaired innervation and prevent the progression of the disease.
- muscle weakness;
- inhibition of tendon reflexes;
- pain syndrome;
- decreased sensitivity;
- muscle atrophy.
To eliminate the symptoms of polyneuritis in such cases, first of all, etiotropic treatment is indicated, that is, an impact on the main cause of the disease.
https://www.youtube.com/watch?v=Ffy6PRdtjzQ
In cases of alcoholic polyneuropathy, alcohol intake is excluded, in diabetic polyneuritis, blood sugar levels are normalized, and in case of infectious damage to peripheral nerves, the therapeutic effect is achieved by prescribing antibacterial and antiviral drugs. However, in almost 50% of cases the cause of polyneuritis remains unclear.
Alcoholic and diabetic polyneuropathy of the lower extremities - treatment, drugs of various groups will be discussed in the article.
Metabolic and blood flow influencing agents
These drugs play a major role in the treatment of PNC. In addition to the main metabolic effect, they usually have a number of other therapeutic effects: they improve the regeneration of nervous tissue, have antioxidant properties, and improve trophism and blood circulation of damaged tissues.
The drugs of choice in the treatment of PNC are:
- Cerebrolysin;
- alpha lipoic acid preparations;
- Mexidol;
- Actovegin;
- cytochrome C;
- instenon;
- pantothenate Ca.
The principle of monotherapy and long courses of treatment (over 1 month) make it possible to achieve maximum effect in the treatment of various types of neuropathy. Thus, the symptoms of diabetic PNK are better relieved by alpha-lipoic acid, and Actovegin is prescribed for obliterating atherosclerosis of the vessels of the legs.
Thioctic (alpha-lipoic) acid preparations have a powerful antioxidant effect, reducing the content of free radicals, normalizing metabolic processes and blood circulation in nervous tissue.
The result of its use is a significant regression of the neurological clinic in patients with polyneuritis. The effectiveness of the drug thiogamma in the treatment of PNC has been confirmed by large-scale international studies.
The course of treatment usually begins with intravenous administration of the drug, and after 2-3 weeks they switch to tablet dosage forms. Alcohol is contraindicated during treatment.
Actovegin (solcoseryl) is a hemoderivative from calf serum with a pronounced stimulating effect on regenerative processes and an antihypoxic effect. Its administration for PNC combines intravenous and oral administration. The complex action of Actovegin is simultaneously aimed at processes in the peripheral and central nervous systems.
Instenon is a multicomponent drug with vasodilating, metabolic and antispasmodic activity.
The complex effect during PNK provides improved neuromuscular conduction and improved blood supply to tissues depleted of oxygen.
By restoring trophism, it is possible to quickly restore impaired functions. The course of treatment consists of intramuscular injections and internal use.
Cerebrolysin is generally recognized as one of the best neurometabolites, capable of stopping degenerative processes in nervous tissue, accelerating its metabolism and protecting it from harmful factors. The drug minimizes the risk of neuronal death during hypoxia and ischemia and has a strong neurotrophic effect. It is used for PNC in courses both intramuscularly and intravenously.
Alcoholism has a detrimental effect on all organs. Alcoholic polyneuropathy is one of the dangerous complications of excessive drinking.
You can learn how to recognize the symptoms of intracranial pressure here.
And in this topic https://neuro-logia.ru/zabolevaniya/nervno-myshechnye-patologii/nervnyj-tik-kak-izbavitsya.html you will learn what a nervous tic is and how to get rid of it. All about home therapy methods.
Vitamins
In complex vitamin therapy for PNC, the main role is given to B vitamins. The use of these neurotropic drugs promotes myelination of peripheral nerves and accelerates the transmission of impulses to muscles.
In addition, vitamin B 1 has an indirect analgesic effect and significantly accelerates regeneration processes, and vitamin B 6 has antioxidant activity and helps improve neuromuscular conduction.
Vitamin B 12 (cyanocobalamin) in PNK is necessary for the restoration of damaged nerve fibers, as it participates in the normal synthesis of myelin.
In addition, it ensures normal blood composition and has an analgesic effect. Complex administration of vitamins for polyneuritis has a positive effect on metabolic and regenerative processes in tissues, restores innervation and strengthens blood vessels.
Painkillers
The choice of pain relief depends on the cause of polyneuritis, however, a 100% solution to the problem of pain in this condition has not yet been achieved. Drugs from the group of analgesics and non-steroidal anti-inflammatory drugs are not able to relieve pain in PNC.
For local anesthesia, normalization of sleep, treatment of depressive conditions and improvement of social adaptation, the following are prescribed:
- local anesthetics (lidocaine, versatis);
- anticonvulsants (tebantin, pregabalin);
- irritating drugs (capsaicin);
- antidepressants (amitriptyline, Cymbalta);
- narcotic opioid analgesics (tramadol, oxycodone).
Drugs that improve the conduction of nerve impulses
To improve neuromuscular conduction in the treatment of PNC, anticholinesterase drugs are successfully used, which provide a pronounced effect on impulse transmission in peripheral synapses.
Even with damaged myelin sheaths of the nerves of the lower extremities, these agents guarantee the conduction of motor signals along the surviving sections of the nerve fibers.
The use of anticholinesterase drugs helps restore lost muscle strength and increases the level of sensitivity.
In addition to standard anticholinesterase agents (proserin), modern methods of treating PNC use ipidacrine, which has a dual effect on peripheral nerves . It helps stimulate neuromuscular transmission and at the same time improves conduction along the peripheral nerve.
The drug is highly effective and has no side effects. It is well tolerated when administered long-term in combination with antioxidants and neurotropic medications.
The arsenal of modern means of treating PNC, which modern medicine is armed with, when used in a complex manner, can effectively influence the symptoms of PNC.
With individual selection of medications by the attending physician and sufficient patience on the part of the patient, the disease gradually but steadily recedes.
People who work in production and are constantly exposed to vibration can eventually develop an occupational disease - vibration disease. It is important to observe preventive measures at work and receive timely treatment in the presence of risk factors and at the first symptoms of this disease.
Read all about the dangers of a ruptured brain aneurysm on this page.
Causes
This pathology can be primary, that is, it occurs without special prerequisites, or secondary. In such a situation, the pain is explained by pathological changes in the neck area.
Secondary neuralgia develops under the influence of such factors:
- Osteochondrosis. This disorder, which can occur in the cervical spine, often provokes degenerative processes in the intervertebral discs. As a result, there is a disruption of the nerve roots located in the back of the head.
- Prolonged tension in muscle tissue of a static nature. It may be a consequence of a violation of the position of the body. This condition is provoked by prolonged use of the computer. It can also be the result of stress or heavy physical activity.
- Neck injuries. They can lead to compression of nerve endings.
- Hypothermia.
- Gout. This disease can lead to joint damage.
- Arthritis. This disease can affect joints located in the cervical region.
- Complex forms of viral pathologies.
- Oncological diseases. They can affect the brain or cervical spinal cord.
- Infectious pathologies. Diseases such as encephalitis and meningitis can lead to damage to nerve tissue.
- Endocrine disorders. Neuritis of the occipital nerve can be a consequence of diabetes mellitus.
- Autoimmune disorders. When such problems develop, the immune system negatively perceives nerve cells. Such diseases include lupus erythematosus, rheumatoid arthritis or.
- Inflammatory processes in blood vessels.
- Tuberculous spondylitis.
Causes and localization
The main “initiators” of neuritis are injuries, joint diseases, and leg tumors. In addition, some industries associated with vibration (mines, construction sites, drilling rigs) “give” their employees vegetative neuritis. Infections, especially viral ones, can also cause neuritis.
During illnesses, for example, measles, scarlet fever, rubella, the body becomes intoxicated, toxins reach the nerve and cause inflammation, i.e. neuritis. Abuse of alcoholic beverages, especially low-quality ones, affects the peroneal nerve of the leg and is called toxic neuritis. Any injury that results in a bone fracture or prolonged compression of a part of the leg can cause traumatic neuritis.
Doctors distinguish the following types of neuritis according to their location on the legs.
- Inflammation of the nerve plexus in the lumbosacral region is called plexitis. With this disease, one leg, lower back and hip joints hurt. The muscles of the thigh and lower leg lose sensitivity. The foot swells, trophic disorders of the nails appear.
- Neuritis of the sciatic nerve makes itself felt by dull pain on the back of the thigh and buttocks. Your legs may become numb from your hips to your feet. The lower leg muscles are in reduced tone or even atrophy. This type of neuritis is more common with flat feet. The disease is sometimes confused with sciatica. But with sciatica, the pain is shooting and intensifies when changing the position of the leg.
- Femoral nerve neuritis manifests itself as pain when flexing/extending the legs. The painful syndrome is especially pronounced on the front surface of the thigh and above the inguinal fold. It becomes difficult for a person to climb stairs. This form of neuritis is called neuralgia or neuropathy. The symptoms are very similar to arthritis and arthrosis of the hip joint. A neurological examination is performed to exclude diseases of the leg joints.
- Compression of the nerve on the anterior outer side of the thigh is called meralgia paresthetica, or Bernhardt-Roth disease. At the beginning of the disease, a person feels a “crawling sensation” when walking, tingling or burning of the skin of the thigh. Subsequently, coldness or numbness of the skin is replaced by pain, especially at night.
- Tibial neuritis is characterized by pain and decreased sensation in the back of the leg. It is difficult for the patient to bend his toes and move his foot.
- Pain in the front outer part of the leg and foot drop in such a way that a person has to raise his leg high when walking, which indicates neuritis of the peroneal nerve.
Muscle performance and blood circulation in the affected area of the legs are not immediately impaired.
Classification
The disease can be classified according to different criteria.
The division occurs according to:
- location ;
- pathomorphological changes;
- the conditions of its occurrence;
- the number of affected nerves.
By localization they are divided into:
- Optic neuritis The cavity of the eyeball, the back of the orbit or the intracranial area is affected. If you do not go to the clinic in a timely manner, you can completely lose your vision.
- Vegetative. Any area of the human body is affected. Autonomic nerve fibers become inflamed, after which disturbances in blood circulation occur. A different shade of skin appears in the area of inflammation.
- Lesions of the cochlear nerve. Occurs after injuries to the skull, ear or infectious disease. If left untreated, deafness occurs, which later cannot be treated. A common symptom of this pathology is the appearance of noise and ringing in the ears.
- Trigeminal neuralgia, etc.
On this topic
According to pathomorphological changes, neuritis is as follows:
- Axial. Characterized by predominant damage to the axial cylinders.
- Adventitial. During the destruction of the upper outer sheath of the nerve, this type of neuritis occurs.
- Interstitial. Inflammation of the connective tissue structure of the nerve is observed
- Segmental. Individual small sections of nerve fibers along its entire length are affected.
- Rising. This is a process in which the lesion occurs in the distal part of the limb and spreads proximally.
- Parenchymatous. Inflammation of the nervous tissue itself occurs, involving axons and Schwann cells.
- Hypertrophic Gombo neuritis is characterized by segmental disintegration of the myelin sheath in limited areas of the nerve fiber with relative preservation of the axial cylinder; manifests itself in reversible dysfunction of the nerve fiber.
On this topic
If we take into account the conditions for the occurrence of neuritis, they are divided into:
- Infectious. Appear as a complication after infectious diseases (diphtheria, measles, scarlet fever, rubella). Toxic substances that spread throughout the body quickly give rise to new foci of the inflammatory process.
- Vibrating . If people's professions are associated with constant vibration, then they may suffer from such a disease. Oppression of the hand or foot occurs. In most cases, miners, drillers and construction workers suffer.
- Traumatic. Appear after accidents, bruises, falls, after which bone fractures occur. Another reason is prolonged compression of some part of the body.
- Toxic. The ulnar nerves suffer if heavy metal affects the body. Peroneal nerves, if affected by alcohol. Toxic poisoning can occur in the workplace when working with mercury or zinc.
- Endemic. Appears when there is a lack of nicotinic acid or B vitamins in the body. Frequent victims are patients with diabetes and pregnant women who have toxicosis.
On this topic
If we take into account the number of affected nerves, neuritis is divided into two types:
- Multiple lesions - polyneuritis.
- Single - mononeuritis.