What is rabies in cats?
Cats become infected with rabies after catching a sick small animal or receiving a bite from a rabid animal. The virus lives in saliva, so the main method of transmission of the disease is through saliva during a bite.
The incubation period lasts 2–3 weeks. The rate of damage to the animal’s body is affected by the location and extent of the wound.
Symptoms vary among different forms. The violent form becomes immediately noticeable to the owners: the cat caresses, rubs against the owner, or, on the contrary, sleeps a lot and hides in a dark place.
Her drooling increases. The fur on the chest is wet, becomes dirty, and icicles appear. As the disease progresses, the mouth opens unnaturally.
The cat is afraid of light and water. The animal eats little or not at all, but tries to chew on inedible objects. Becomes aggressive and attacks the owner. At such moments, it is almost impossible to drag the cat away.
At the last stage, the animal develops convulsions and paralysis occurs. The violent form is the most common. But sometimes there are no attacks of aggression. The cat hides in the dark and after 3-5 days the stage of paralysis begins.
How to recognize a sick animal
The problem with this disease is that it is almost impossible to cure once clinical symptoms have already appeared. The progression of the disease can only be stopped through vaccination. The rabies vaccine must be given urgently, immediately after the bite.
It must be remembered that even a domestic cat can be a carrier of the virus if it has been in contact with a sick yard animal. The incubation period of the virus in animals takes 3-10 days, so it is impossible to know at an early stage of infection that the pet is already sick. He may behave calmly, but there will be a huge amount of virus in his blood. This animal is very contagious.
When the virus has captured the nerve cells, symptoms of rabies begin to appear: aggression (the animal attacks for no apparent reason, reacts painfully to any irritants), drooling (saliva can flow like a river or, like foam, collect in the corners of the mouth). It is easier for the owner to observe a pet, so if the pet suddenly becomes lethargic, hides in dark corners, or eats almost nothing, he needs to be taken to the vet immediately!
In the excited stage, the dog growls almost continuously and barks until he becomes hoarse. Everything irritates her: any shout, harsh light, etc. Due to spasms of the pharyngeal muscles, she cannot drink water. The animal is salivating profusely, its jaw is slack, and its tongue is hanging out of its mouth. Clouding of the cornea of the eyes often occurs. After the stage of excitement, a period of relative calm begins, when the animal becomes obsessively affectionate. This is the first sign of approaching paralysis and subsequent death.
How do you determine if a cat has rabies?
Tests to determine the virus are taken after the death of the cat to make an accurate diagnosis. The causative agent of rabies is detected in brain tissue.
This method allows you to reliably determine the presence of rabies. The virus can be diagnosed in saliva and cerebrospinal fluid, but a negative test does not guarantee the absence of disease.
Animals are rarely diagnosed. Diagnosis is made by symptoms. A sick cat is isolated for up to a month. If infected, the animal dies.
Prevention
Prevention (specific and nonspecific) in this case occupies a special place. A person who has been attacked must be vaccinated. In addition, everyone whose profession is related to animals (veterinarians, hunters) is vaccinated. Nonspecific prevention consists of thoroughly treating the wound surface with a 20% solution of medical soap.
During the consultation, the doctor will answer questions and tell you what can be done if you become infected with rabies. Appointments can be made online and at the above numbers.
Related services: Ambulance call 5288
Vaccinating cats against rabies: when to vaccinate
There is no cure for rabies. The only way to avoid the disease is timely vaccination. The vaccination is given to a kitten at the age of 3 months.
The animal must be healthy. 2 weeks before the injection, the kitten must be given anthelmintic drugs.
Vaccines that have proven positive:
They are easily tolerated by cats and do not cause discomfort. Before the first vaccination, contact of the animal with sick individuals should be avoided.
It is not advisable to let your cat outside. Vaccinations in Russia are provided free of charge in state veterinary clinics.
The most likely methods of infection
The rabies virus is contained in the saliva of a sick animal. Infection occurs when the virus enters the bloodstream, usually through a bite. It must be taken into account that the virus can appear in saliva 1-7 days before the first symptoms of the disease, so you can become infected even from an animal that looked healthy.
The most dangerous are bites from sick carnivores (especially wild ones, such as foxes). People rarely become infected from farm animals. Domestic birds get rabies, but they cannot infect humans due to the lack of salivary glands. Infection from birds of prey is possible, but unlikely due to their low prevalence.
But a bite is not the only way to transmit the virus, so when contacting wild or stray animals you need to be as careful as possible. Possible routes of transmission of rabies include:
- through contact with the saliva of a rabid animal on the mucous membranes of the nose, eyes, mouth and damaged skin;
- through scratches caused by claws, as animals lick their paws and particles of saliva with the virus may remain on them;
- while cutting up the carcass of a sick animal through scratches and wounds on the hands.

Also in medicine, cases of infection through atypical or unusual routes are described - for example, through airborne droplets, which is only possible with a very high concentration of the virus in the air that is practically not found in nature. Isolated cases of infection through the placenta during pregnancy and during tissue and organ transplantation have been recorded. There have also been cases of animals becoming infected through the digestive tract after eating raw meat; humans have not yet become infected. This is due to the fact that the virus can very rarely penetrate the blood and glandular organs, and when cooked it dies instantly.
How often do cats get a rabies injection and who is the vaccine contraindicated for?
Rabies vaccinations are given annually. The countdown starts from the first injection. The exception is the Dutch vaccine Novibak. When used, immunity is formed for 3 years.
If the cat is taken outside the Russian Federation, then the vaccination will have to be repeated in a year.
It is prohibited to vaccinate an animal that has an acute viral or chronic disease. Pregnant and weakened cats should not be vaccinated.
Can a vaccinated cat get rabies?
The rabies vaccine does not completely guarantee that the animal will not get sick. If during vaccination the cat was infected with worms, then there remains a risk that the vaccination will not give results.
Symptoms of the disease appear within 2 weeks. The presence of the rabies virus in the body during vaccination is the cause of the disease.
Factors that influence the formation of immunity to the virus:
- age of the cat;
- exhaustion;
- stress;
- chronic diseases;
- multiple births.
Is it possible to get rabies from a person through a kiss?
A letter will be sent to this address soon. Confirm your subscription if everything is valid. A good spray can is the most effective thing there is against both dogs and people.
Trauma is a completely useless thing for dogs, as long as you get it, while you take aim, you are already being bought and against people, hello, exceeding the necessary self-defense. By the way, about “Impact”. I have experience of real “combat” use against stray dogs and several times I had to shoot back from attacking dogs. I don’t know how it is with rabid dogs, but usually dogs are smart, and a simple noise cartridge that imitates the sound of a gunshot is enough for them.
They turn around and leave. But sometimes this is not enough, then “Tarantula” or “Teardrop” is used, the same “Tarantula”, but with the addition of something tear-inducing. It is enough for the dog's head to be at least slightly caught in a cloud of rubbish. The dog is guaranteed to become very uncomfortable with an attack for several hours, and this is understandable, the thing is very burning, even getting a drop on your finger is unpleasant, to put it mildly. Naturally, in case of a sudden attack, a bite from the gateway will not help. You just won't have time to apply it.
But if the time before the attack is still relatively far away, or the attack is in the “prelude” phase - they surround, growl, lunge towards the target, it works well. I also admit that there are dogs with anomalies that are capable of attacking despite being hit by an aerosol, but I haven’t met them yet. The disease does not occur immediately after infection. The vaccine helps during the period when you have already become infected, but have not yet gotten sick.
I support the concerns. Also a cat of unknown origin. Despite the fact that she bit my finger, I went to the emergency room that same day, where they gave me an injection for tetanus and rabies. And then there were no injections on the same days. There was no sick leave, they were only released from work for injections. Everything is compulsory medical insurance. A bite to the finger is a serious case due to the large concentration of nerve cells in the hands.
For the same reason, a severe one is a bite in the genitals. In the face and neck - a short distance to the brain. Finnish colleagues said that they have such a program along the border with Russia. Precisely because they don’t seem to have rabies at all. Finland is on the list of countries without rabies, but animals cross the border freely and, accordingly, there is a risk that they will be brought.
As far as I know, all successful cases were from bat bites. There was no successful cure for other routes of infection. Or do you have such data? Does probability theory tell you anything? The epidemiologist only states that the likelihood of such and such a stamp is greatest, so you need to be vaccinated against it. A motorcyclist wears a helmet because, according to statistics, in the vast majority of cases the impact occurs in the head. A motorcyclist will wear a helmet, but die due to a fat embolism as a result of a broken leg and will say “your helmets are garbage, they are big, heavy, expensive, they are hot, and they do not protect at all 1.
Firstly, viruses are not magical crap from movies that do not penetrate just any cells, but only strictly defined ones, to whose receptors they have adapted, and accordingly, a virus cannot simultaneously attack, say, both intestinal epithelial cells and “ kill bacteria in the intestines." And secondly, the vaccine does not contain the virus itself, but its “spare parts”, which by definition do not have “killing” elements.
And I have: coincidence. Well, there are coincidences in life, you know? Of course, there is a possibility that this is really a consequence of the vaccination, but in the same way it could also be due to age, like in millions of other children. There may be a low-quality or counterfeit vaccine, or there may be a genetic disease. Just judging by the above, there is no reason to be absolutely sure that the vaccine is to blame. Moreover, based on exactly how vaccinations work, the main version should be just the opposite.
Your argument causes such a reaction because followers of the cult “vaccines cause autism” argue their position in exactly the same way. After vaccination, they also discovered that the child had autism, there were no other effects on the body, some doctors confirmed that they have no other explanations.
Moreover, there are many such cases, which means vaccinations for sure. But we know that autism doesn’t work that way. And the explanation is simple - autism can be diagnosed no earlier than a certain age, which approximately coincides with the age of the first vaccinations. Among the doctors there are people of different qualifications, including those who believe in homeopathy or the harm of vaccinations. It is very easy to collect the opinions of those who confirm your point of view. By the way, a completely correct question: Ryav, have you done any genetic test like 23andme, don’t forget, do you need a Health level?
The problem is that by doing so he can put a pig on someone else. Exaggerating, a person has the right to bring tuberculosis to an open form, but, after sneezing on the bus, give a gift to a neighbor. Who is unlikely to be happy about this. Therefore, it is worth remembering that the freedom of one person ends where the freedom of another begins. If he lives in isolation, anything is welcome. If you want to live in society, be so kind as to adhere to social norms.
Vaccination is not only about your personal health. Refusiers are those who refused at this particular moment from this particular vaccination. Anti-vaxxers are those who oppose vaccinations.
Inappropriate refusers - those who refuse all vaccinations without reasonable justification, as I see it, are mainly intimidated by anti-vaxxers or are themselves anti-vaxxers. Adequate refusers are those who refuse, I will further clarify, just in case, for themselves or their children, they refuse all or part of vaccinations for reasonable reasons. I think so.
The nurse, while treating the bite site, told me that it was my own fault. I couldn’t expand on the statement, I just said that I should have guessed.
The most interesting thing on the list. After all, a dog considers a very large space to be its territory. And you will most likely always cross the territory of some dog, simply walking according to your needs. So from the dog’s point of view, the attack may turn out to be very justified. But this will not make it any easier for the person who was bitten. And the flock will have an even larger territory. One of the cases when I used “Strike” on dogs. I'm standing alone at a public transport stop. The time is very early, there are no people there.
Suddenly a growl is heard from behind. I slowly turn around and see that dogs are approaching me with bared muzzles and a clear desire to attack. How did you define the desire to attack?
Naturally, I take out the “Udar” and shoot with noise. The dogs stop growling and baring their teeth, turn around and leave. In most cases, by the way, a pack or a dog runs past without being interested, yes. Then, accordingly, the conflict does not arise. But in some cases, for some reason, they attack. Terms are not argued about, they are agreed upon.
It was probably assumed that the dogs I meant were “stray”, “not “wild”. So be it. It turns out that they are more dangerous than wild ones, because the average person will never see a wild dog in his life, but there are any number of stray ones. At the same time, the danger from the fact that they are not “wild” is no less. These are ordinary... after all, wild animals, that is, not raised by humans, and do not recognize the supremacy of man.
I can only add that dogs can move from category to category - for example, at one time I managed to tame several “strays”. This is all very clear. It’s just jarring: “puts to sleep”, which is used to disguise the more correct “kill”. It is suspected that the marine mammal will drown fairly quickly when the first symptoms appear. True, then someone else could eat it and still get infected. All Habr services. How to become an author of a remote marathon. Log in registration.
A little over a year ago I had to deal with such an unpleasant thing as suspected rabies infection. An article I read yesterday about vaccinations for travelers reminded me of that case - especially by the lack of mention of rabies in it, although this is an extremely widespread and very insidious virus, especially in Russia, Asia, Africa and America. Unfortunately, the risks associated with it are not always given due importance. So what is rabies?
How does a person become infected with rabies from a cat?
Rabies is transmitted from a cat to a person by a bite when an infected animal attacks a person. Infected saliva enters the human nervous system.

Rabies is transmitted from a cat to a person by a bite
The virus remains at the site of the bite for up to 10 days. After this, the infection spreads along the nerve fibers throughout the body. The propagation speed is 3 mm/h.
It is impossible to detect the virus in the blood. The infection reaches the spinal cord and travels through the nerve endings to the brain. The virus also settles in the salivary glands.
Brain damage leads to severe impairment. A person loses control over himself, hallucinations and aggressive behavior appear.
The patient has difficulty breathing and swallowing. Salivation increases, attacks occur: the patient throws his head back, stretches his arms forward.
You can become infected with rabies from a cat that has no symptoms of the disease. If the animal has become infected in the last two weeks, then signs of infection have not yet appeared.
What to do if bitten by a cat?
If a person is bitten by a cat, then it is necessary to provide first aid to the victim:
- Rinse the wound under running water for 10 minutes. Use soap.
- Treat the edges of the wound with a disinfectant.
- Apply a sterile bandage. Wrap loosely.
- Go to the hospital emergency room.

These actions will help avoid bacterial infection, but will not protect you from illness. If someone else's cat has bitten you, the doctor will suggest giving you a rabies injection.
The injection is placed in the forearm area or at the site of injury. Refusal of the injection in case of infection will lead to the death of the patient.
If you are bitten by a domestic cat that has not been exposed to other animals for the past two weeks, you can refuse the vaccine.
What not to do in case of a cat bite:
- stop minor bleeding;
- apply pressure to the affected area;
- engage in self-diagnosis and treatment if bitten by an unfamiliar cat.
You should seek medical help in the following cases:
- heavy bleeding;
- multiple bites;
- when feeling unwell;
- the appearance of inflammation;
- bite in the face or neck area.
If you are scratched by a cat
The rabies virus is not transmitted by cat scratches. The exception is a wound that has received saliva from a sick animal. If a domestic cat is vaccinated, there is no chance of contracting rabies.
Is rabies a fatal disease?
The rabies virus affects the central nervous system of animals and humans.
Rising along the nerve pathways, it reaches the brain and causes inflammation (specific encephalitis). Until 2005, rabies was considered a fatal infection for humans. There are only a few known cases of people being cured of this terrible infectious disease. However, a timely vaccination or certain measures, which will be discussed later, can save the patient’s life. The main carriers of the rabies virus are:
- Wild animals (wolves, foxes, wild cats, lynxes, bats, hedgehogs, rodents)
- Farm animals
- Pets
Statistics of rabies incidence in Russia by animal carrier species for 1997 - 2007
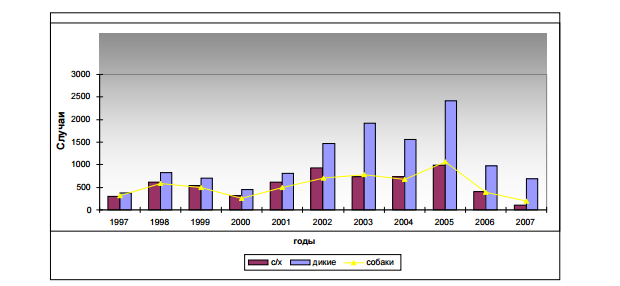
The diagrams show that the main sources of rabies are wild animals. Recently, due to the spread of rabies among wild animals, the virus penetrates simultaneously into several biological species. For example, it is transmitted from a wolf to a fox or marten. Therefore, you need to be especially careful and attentive in the forest. We have previously written about safety rules in the forest.
Approximately half of all cases of rabies infection occur in domestic and farm animals that come into contact with wild animals. The most dangerous wild animals in terms of rabies infection are foxes (first diagram). Moreover, you can meet mad foxes both in the forest and in the city. When infected with rabies, foxes can manifest themselves in two ways. Some may behave aggressively and attack people. Others, on the contrary, are drawn to people and show affection, like domestic cats. This behavior is not typical for a healthy fox.
If you encounter such a fox, you must immediately leave the forest or area in which it is located. Under no circumstances should you pick them up.

Signs of rabies in humans
The very first symptom of the disease is inflammation of the bite site. Swelling and redness appear, which increases in size.

The disease appears faster in children than in adults
The skin color becomes dark red. The itching increases, the person feels pain that was not there before. Fatigue, heaviness in the head, weakness indicate that the virus has entered the body.
Often the disease is accompanied by additional symptoms:
- body temperature 37.5 degrees or more;
- nervousness;
- nausea, vomiting;
- painful sensitivity to light;
- avoiding harsh sounds;
- worsening sleep;
- anxiety;
- apathy.
The primary signs of infection are nonspecific; similar symptoms accompany other viral diseases. If you have been bitten by an animal before, you should immediately consult a therapist.
Features of the lush form
In the violent form, a person becomes aggressive and tries to hurt himself or others. Auditory hallucinations occur.
During the examination, the doctor notes the following signs in the patient:
- increased breathing and heart rate;
- difficulty swallowing;
- fear of water;
- attacks of fear in bright light, open space;
- convulsive attacks.
Paralytic form
The paralytic form lasts 2-3 days and is identified by symptoms:
- drooling due to muscle paralysis;
- weakness in the arms: the person is unable to lift objects;
- slack jaw;
- increased body temperature;
- during an attack the person cannot breathe;
- anxiety gives way to apathy.
The entire period of the disease reaches 10 days without an incubation period. The paralytic form always ends in the death of the patient.
Excitation stage
The stage is characterized by increased sensitivity to external stimuli (light, smell, touch, sound) and fear of water. For example, the patient cannot even take a sip of water - convulsive contractions begin, even to the point of vomiting. As the disease progresses, convulsions occur even from the sound of pouring water. The patient's blood pressure rises, the heart rate increases, breathing becomes frequent and shallow, profuse sweating and drooling appear.
This stage is characterized by periods of excitement when the sick person cannot control himself. He becomes aggressive, tears his clothes, attacks people, and screams in a voice that is not his own. The attack is accompanied by aggressive hallucinations.
On our website Dobrobut.com you will find more information on this topic. By calling the above numbers, you can make an appointment with a doctor who will tell you when to do a blood test for rabies and what can alleviate the condition of an already sick person.
How can a person avoid infection?
Rabies is a disease that is easier to prevent than to treat.
To avoid infection, you must:
- vaccinate pets in a timely manner;
- keep an eye on your pet during a walk, do not allow contact with wild and stray animals;
- catch stray dogs;
- do not touch street cats;
- do not hand feed squirrels in the park;
- When traveling to other countries, check the level of rabies and, if necessary, get vaccinated.
If you are bitten (scratched) by a rabid cat, what should you do?
The bite of a rabid cat is a mortal danger that will certainly kill the victim, but not immediately, but over time. For the time being, the person bitten may feel completely normal, but then events will develop rapidly. Therefore, if a person has been bitten or scratched by a rabid cat or an ordinary cat in which rabies is theoretically possible, it is necessary to urgently take measures to prevent the development of the disease.

In this article we will consider such questions!
Herpes
Herpes simplex, which manifests itself in the form of blisters on the lips, is transmitted primarily through the oral route, that is, through kissing. Once the virus penetrates the nerve cells, it is impossible to remove it from the body; the person will be a carrier for the rest of his life. But this disease is far from being as harmless as it seems, and rashes on the lips are one of the most harmless symptoms. For example, herpes is a catalyst for the development of Alzheimer's disease. Therefore, during the period of exacerbation of the disease, when characteristic rashes appear on the lips, you should refrain from kissing, as well as contact through dishes or other household items.
Rabies from a cat bite or scratch - is it possible?
The rabies virus is found in the brain and saliva of an infected animal. And it can infect a person by getting into the blood. Therefore, the answer to the question of how you can become infected with rabies from a cat will be this:
- by a bite (including rabies is transmitted through a small scratch with a fang);
- through a scratch, if the rabies virus was on the cat’s claws (and it could get there with saliva);
- the rabies virus may be present on the cat’s paws if she has just licked them: infection will occur if the cat tramples on the owner’s hands or feet and there are scratches and wounds on them;
- when a cat licks skin where there are already scratches.
Let us dwell in more detail on the question of whether rabies is transmitted through a scratch, since everything is clear with a bite. A domestic cat infected with the virus can transmit it to its owner in the early stages of the disease without even biting. To do this, just lick your hand where there is a scratch, perhaps not even caused by a cat. Accordingly, the owner, having learned after some time that his cat is sick, may not even suspect that he is now also a carrier of the terrible virus and will soon die.
Initial stage of the disease
Symptoms do not appear immediately. A week, two or even a month may pass from the moment of the bite. If the bite was on the arm or upper body, symptoms will appear after 10-14 days. When bitten on the legs, the first signs of the disease may appear after one or two months. The incubation period for rabies in humans ranges from three days to three months.
The first symptoms are discomfort in the area of the bite (scratch). In some cases, suppuration and redness of the skin are observed. In addition, the patient may complain of:
- decreased appetite and weight loss;
- sleep disturbance and nightmares;
- development of apathy;
- low-grade fever.
If the bite was in the face, the patient is haunted by hallucinations. The pulse rate gradually increases, blood pressure rises, and anxiety appears.
Signs of rabies after a cat bite
After a person is bitten or scratched by a cat, they may develop rabies. Of course, only if the cat itself was sick. Symptoms will not appear immediately: the incubation period in exceptional cases can reach a year. But more often we are talking about a period from 1 week to 3 months after contact.
Rabies can manifest itself in different forms. Violent, with which everyone associates this disease, is only one of three scenarios. The most common symptoms of rabies in humans with this form are:
- itching and pain at the site of the bite, which can appear even on an almost healed wound;
- fever;
- headache;
- general malaise;
- disorders of appetite and digestion;
- depression and anxiety;
- increased sensitivity to noise and bright light;
- hydrophobia (a person cannot swallow or swallows with difficulty, and sometimes even at the mention of water his throat begins to spasm and he is overcome with horror);
- attacks of agitation and aggression;
- hallucinations;
- convulsions;
- excessive salivation.
Once even the very first symptoms of rabies appear, it is no longer possible to help a person. He is placed in a hospital, where he spends his last days. Ultimately, the rabies virus makes the human brain unable to perform its basic functions, causing the person to die. As a rule, death occurs as a result of stopping the respiratory center or heart.
The set of symptoms depends on the form of the disease. Rabies, as we have already said, has 3 forms: violent, paralytic and atypical. Violent is usually diagnosed without problems. Symptoms of the disease in its violent form look something like this. Attention! Do not watch for the impressionable.
But the paralytic form, which is observed in almost 30% of cases, often remains undiagnosed, not to mention atypical. The fact is that there are no tests to diagnose rabies in humans if symptoms have not yet appeared. Diagnosis is based on symptoms and subsequent testing, but when symptoms are mild or atypical, doctors will not suspect rabies and will not test. In this regard, the following case is indicative.
A woman went on holiday to Nepal where she was bitten by a cute little puppy. She did not immediately attach any importance to the situation, but when she returned home to Ireland, she consulted a doctor, because... The bite site became very inflamed. He prescribed an ointment that helped heal the wound. And after 1.5 years, when the woman was already living in Latvia, she was admitted to the hospital with a diagnosis of pinched sciatic nerve, because... the symptoms resembled this disease. The woman began having attacks of suffocation at the sight of water or trying to swallow saliva, that is, hydrophobia was evident. Then the patient herself suspected rabies, but the doctors believed that she was having attacks of hysteria. The patient was transferred to a psychoneurological hospital. And then she was given another diagnosis - acute psychosis. The woman soon died from pulmonary edema. Post-mortem diagnosis: rabies.
The reason for this situation is the lack of awareness among doctors about this disease and lack of alertness, because In Europe, this disease practically does not occur. In the CIS countries, where the rabies situation is unfavorable, things are better with diagnostics.
First aid
When a person has reason to believe that they may have contracted rabies, they should immediately consult a doctor
But it is equally important to provide yourself with first aid, as well as take care of safety. This is especially true in cases where the victim was bitten by a pet that became a carrier of a dangerous virus.

Immediately after the bite you need to do the following:
- Call an ambulance or choose the nearest medical facility (trauma center).
- Tie up your pet, isolating it from surrounding people and animals, or call the sanitary service through the rescue phone.
- Wash the wound with clean water and laundry soap, trying to cause heavy bleeding to remove the virus from the blood, and go to the hospital.
- Once the doctor has taken all the necessary measures, you should definitely show your pet to a veterinarian when returning home.
You can identify rabies in pets yourself. However, this can only be done after the active development of the disease begins, and the carrier becomes infectious about a week before. Therefore, in some cases, you can catch the virus even from an apparently healthy pet. Nevertheless, the symptoms will help identify a guaranteed sick animal. These include:
- Desire to chew or scratch where another animal has bitten you;
- Dilated pupils, eating inedible objects;
- Increased salivation, foam at the mouth and vomiting;
- Severe hydrophobia (not experienced by everyone);
- Aggressive behavior, attempts to run away from home.
What to do if bitten by a mad cat?
If a person is bitten or scratched by a rabid cat, it is necessary to urgently take preventive measures. This is first aid for treating the wound, and then you need to consult a doctor.
After a cat attack, you need to stop contact with the animal by hiding from it, for example, in the bathroom. Or lock him in some room from which he cannot escape. This way you will protect yourself and other people from being attacked again.
As soon as possible, the wound should be intensively washed with soap and running water for at least 15 minutes, and then the edges of the wound should be treated with either tincture of iodine 5% or a solution of brilliant green. Primary treatment minimizes the amount of virus entering the blood. After this, you need to call for help. For example, you can call the rescuers. They will catch the animal and put it in quarantine.
Prevention and vaccination against rabies in humans
After animal bites, you must immediately thoroughly wash the wound with laundry soap and running water, treat it with alcohol and iodine. It is strictly forbidden to cauterize or excise the wound, as this contributes to the spread of the virus.
After treatment in the hospital, the wound is sprinkled with powder containing anti-rabies gamma globulins.
They no longer give 40 rabies injections in the stomach. This method is outdated.
A person should be vaccinated against rabies no later than two weeks from the moment of the bite. After the specified period, it is practically ineffective.
Rabies vaccination schedule
At the moment, the following rabies vaccination schedule for humans is used: 1 milliliter of vaccine five times on the day of the bite. The drug is injected into the shoulder or thigh. Next, the rabies vaccine is administered on the third, seventh, fourteenth, twenty-eighth (or thirtieth) and ninetieth day after the bite.
The injection is given on the 28th or 30th day, depending on the vaccine manufacturer.
In case of severe bites or late treatment (10 days from the moment of the bite), anti-rabies gamma globulins are administered in addition to the vaccine.
Preventive vaccinations are recommended for people working with animals, hunters, researchers, veterinarians, etc. The rabies vaccine is valid for about a year. Therefore, for patients bitten by an animal within a year after a full course of vaccinations, vaccination is indicated only on the day of the bite + on the third and seventh days.
Preventive vaccinations are carried out upon application, as well as on the seventh and thirtieth day. A year later, the first revaccination is indicated (one administration), with further administration of the vaccine every three years (single administration of the vaccine).
Compatibility of rabies vaccination in humans and alcohol
Alcoholic beverages should not be drunk for six months after rabies vaccination and throughout the entire course of vaccination.
Drinking alcohol increases the risk of developing adverse reactions to the rabies vaccine.
The use of glucocorticosteroid drugs and immunosuppressants is also contraindicated.
Is it possible to wet the rabies vaccine?
The instructions for vaccines do not contain information about the prohibition of getting the vaccine wet. However, it is not recommended to actively rub the grafting site while swimming. Also, it is advisable to refrain from visiting the sauna (overheating is contraindicated).
During the course of preventive vaccination, overheating, hypothermia or excessive physical activity should be avoided.
Side effects of rabies vaccination in humans
Side effects of the vaccine can be manifested by the development of swelling at the injection site, pain, fever, gastrointestinal disorders of a dyspeptic nature, arthritis, and enlarged lymph nodes.
Read further: Vaccination measles, rubella, mumps - side effects, which vaccine is better, revaccination
- about the author
- Recent publications
Are you an infectious disease doctor?
Previous article What medications should be taken for arrhythmia
Next article How long do people live with chronic appendicitis?
Page visited today
93 times
TOP 5 authors
- Lashkina Ulyana
- Nabokina Zlata
- Young Juno
- Sukhomlin Gleb
- Balsunov Miron