Causes of tetanus
Tetanus is an acute infectious disease from the group of saprozoonoses, caused by the anaerobic microorganism Clostridium tetani, characterized by damage to the nervous system and manifested by periodic generalized clonic convulsions against the background of constant tonic tension of skeletal muscles.
Tetanus has always been a problem of wound infection during wars. During World War I, the incidence of tetanus reached 23 per 1000 wounded, so the development of measures to prevent this disease became the most important task. Tetanus vaccine (toxoid or toxoid) was first developed by P. Descombies in 1924-1927, then improved by G. Ramon in 1937 and has since been widely used for the prevention of tetanus. After administering the toxoid to the animals, hyperimmune homologous sera were obtained, which were used to treat sick people. Subsequently, heterologous immunoglobulins were also obtained through immunization of human donors.
Tetanus still remains a serious medical and social problem, as it is characterized by widespread distribution, predominantly affecting the elderly and young children, and an extremely severe course with high mortality. Around the world, about 4 million people suffer from this disease every year (mainly in countries with weak economic and medical systems), and about 1 million die (50% of those killed are infants, 15% are women after childbirth).
The highest incidence was recorded in 2005 in Somalia - more than 750 people per 100 thousand population. Meanwhile, according to the WHO definition, the disease is one of the “preventable infections” that can be prevented through vaccination.
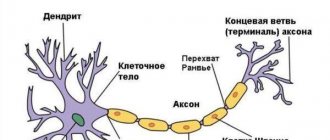
The causative agent of tetanus, Clostridium tetani, now belonging to the genus Clostridium family, is a large thin gram-positive rod, motile due to peritrichially placed flagella. They are obligate anaerobes; oxygen is very toxic to them. It has a group somatic O-antigen and a type-specific basal H-antigen, which distinguishes 10 serotypes. In the presence of oxygen and a temperature of at least 4 ° C, it forms spores. Spores can withstand heating up to 90 °C for 2 hours, when boiled they die only after 1-3 hours, in a dry state they can withstand heating up to 150 °C, autoclaving neutralizes spores at a temperature of 120 °C for 30 minutes, they live in salt sea water up to 6 months. They persist in animal feces, soil, and on various objects for more than 10 years. Conventional disinfectants neutralize them in 10-12 hours. An ambient temperature of at least 37 °C, sufficient humidity and the absence of oxygen allow spores to germinate into vegetative forms. An important feature of these forms is the ability to produce an exotoxin, which is a protein. It consists of the following fragments:
- Tetanospasmin is an aggressive fraction of the toxin, consists of two chains, the heavy one affects the motor axons of the central nervous system, the sympathetic nervous system, the reticular formation, and the light one enhances the secretion of acetylcholine in the neuromuscular junctions and can cause a certain hemolysis of red blood cells;
- tetanolysin - entails hemolysis of red blood cells, and also has cardiotoxic properties, although its main function has not yet been identified.
Tetanus exotoxin is unstable, quickly inactivated when heated, under the influence of sunlight, or an alkaline environment. It is one of the strongest bacterial poisons, which is second only to botulinum toxin in its potency. The lethal dose for humans is considered to be 150 ng.
The disease belongs to sapronoses. The causative agent of tetanus is a ubiquitous microorganism that is widely distributed in nature. The source of infection is herbivores and humans, in whose intestines the tetanus bacillus lives and multiplies. Together with feces, the pathogen enters the soil. A special environment for it is certain soils in which decay processes take place. These are black soils, greenhouses, vegetable gardens where natural fertilizers are applied, and land on livestock farms. Animals become infected by eating grass or contaminated soil that contains tetanus bacillus spores. In the intestines of animals and humans, vegetative forms are formed from spores. They can even secrete a toxin that does not penetrate into the blood and therefore does not exhibit pathogenic properties, in addition, it is quickly destroyed by digestive enzymes. When released into the soil with feces, vegetative forms again turn into spores. However, at the moment there are more and more reasons to include tetanus in the group of saprozoonoses, because the death of a sick animal under natural conditions leads to severe decay and a significant level of reproduction of vegetative forms, after which they turn into spores and persist in the soil.
The mechanism of human infection is contact, wound. More often, the disease develops when spores or vegetative forms enter a wound contaminated with soil. A factor favorable to infection is walking barefoot (“bare foot disease”). The disease can also occur due to injuries accompanied by damage to the skin, without contact with the ground (pricks from thorns, scratches, bites of wild and domestic animals, household injuries), because the spores fall on trees, bushes, clothes, and can be in the mouths of animals. Infection is also possible through contaminated burns, frostbite, electrical injuries, criminal abortions, childbirth under aseptic conditions, colon surgery, removal of foreign bodies, etc.
Tetanus is not transmitted directly from a sick person or animal. Spores can sometimes get into wounds without turning into vegetative forms due to reasons unfavorable for the spores, persist for a long time in scar tissue and become active under certain conditions favorable to them (surgery in this area, suppuration). Then we are talking about the so-called cryptogenic tetanus.
Susceptibility to tetanus is high. The risk group includes rural residents. The disease is recorded sporadically throughout the year. An increase in incidence in our country is observed during the period of increased agricultural activity - April-October. Tetanus is especially common among injecting drug addicts; This may be because homemade opiates and heroin often contain spores, and heroin is often mixed with quinine, which sharply reduces the recovery potential at the injection site and promotes the growth of tetanus. A special risk group in some geographical areas of Africa and Asia consists of women in labor and newborns, who are not provided with adequate hygienic conditions during childbirth and in the neonatal period. For example, according to prejudices existing in Central Africa, the umbilical cord is cut with stones, bones and other objects likely contaminated with spores of the tetanus microbe. Most mothers in these regions are not vaccinated, so babies are not protected from tetanus.
After an illness, immunity is not formed due to the weakness of antigenic irritation.
The entry gate for the causative agent of tetanus is damaged skin, less often mucous membranes. Wounds in which anaerobic conditions are created - puncture wounds, with deep pockets and necrotic areas are especially dangerous. Infected wounds are also dangerous, because in this case a symbiosis of clostrilia occurs with putrefactive bacteria that actively absorb oxygen. Under conditions of anaerobiosis, vegetative forms germinate from spores, multiply and release exotoxin. Tetanus bacillus does not spread beyond the wound, except in rare cases during criminal abortions. The toxin spreads in the body in three ways: through the circulatory, lymphatic system and along the nerve fibers, reaching the spinal and medulla oblongata, the reticular formation, where it causes a block of interneurons of polysynaptic reflex arcs, eliminating their inhibitory effect on motor neurons. Circumstances arise for the occurrence of generalized clonic convulsions in response to any nonspecific irritation of the central nervous system (sound, tactile, light, taste). The nuclei of the vagus nerve, respiratory and vascular-motor centers are affected. A significant increase in the reactivity of the sympathetic nervous system leads to arterial hypertension, tachycardia, and arrhythmia. Convulsive syndrome causes the development of metabolic acidosis, hyperthermia, and increases respiratory and circulatory dysfunction. As a rule, damage to the nervous system in this disease is of a descending nature.
Heart damage may be caused by the direct effect of the toxin on cardiomyocytes (development of toxic myocarditis) and the conduction system of the heart. Causes of death include asphyxia, cardiac or respiratory paralysis and the development of purulent-septic complications (pneumonia, sepsis due to bedsores).
Pathomorphological changes in the body occur mainly due to increased functional load during seizures. Coagulative necrosis is found in skeletal muscles, which often leads to muscle rupture with the formation of hematomas. Histological changes in the central nervous system are insignificant (edema, congestive plethora of the brain and its soft membrane, minor hemorrhages) and are reversible.
According to ICD-10 there are:
- neonatal tetanus,
- obstetric tetanus,
- other forms of tetanus.
The incubation period ranges from 3 to 31 days, with an average of 8-12 days. The severity and prognosis of the disease often depends on the duration of the incubation period: the shorter it is, the more severe the disease and the higher the mortality rate.
Most doctors consider it necessary to apply the clinical classification of tetanus, according to which they distinguish:
- generalized tetanus;
- local tetanus;
- cephalic tetanus;
- tetanus of newborns.
Based on the severity of the course, tetanus is divided into:
- easy;
- moderate severity;
- heavy;
- extremely heavy.
Generalized tetanus. The disease may be preceded by minor prodromal signs. Patients complain of:
- general weakness,
- headache,
- irritability,
- sweating,
- pain and muscle twitching in the wound area.
Examination can reveal increased tendon reflexes on the affected side. Such early symptoms are absent with a short incubation period.
Most often, the disease begins acutely. The first characteristic and very constant symptom of tetanus is bilateral trismus - tonic tension of the masticatory muscles, making it difficult to open the mouth. Almost simultaneously, tonic spasms of the facial muscles develop, as a result of which the face acquires a peculiar appearance of a smile along with crying - a “sardonic smile.” At the same time, the mouth is stretched, its corners are lowered, the forehead is wrinkled, the eye slits are narrowed. Next, difficulty swallowing occurs due to contraction of the throat muscles (dysphagia). The presence of these three symptoms results in the so-called early tetanus triad. It is considered a pathognomonic symptom for generalized tetanus; in this combination - trismus, sardonic smile and dysphagia - are not observed in any other disease.
Next, a process occurs with the development of rigidity of the muscles of the back of the head, muscle rigidity spreads to other muscle groups in descending order - neck, back, abdomen, limbs. Tonic tension of predominantly extensor muscles leads in severe cases to a bent body position with the head thrown back. The patient lies in bed on his back, touching its surface mainly with the back of his head, buttocks and heels (opisthotonus). Sometimes the patient can only rest on the back of his head and heels. From the 2-3rd day of illness, tension in the abdominal muscles is observed, which is accompanied by pain, especially upon palpation, which can be mistakenly regarded as an acute abdomen. Severe muscle pain due to constant tonic tension is one of the leading symptoms of the disease.
If the tension of the flexor muscles predominates, a forced position of the body occurs with the body tilted forward - emprostotonus, and if the muscles on one half of the body contract, the body bends to one side - pleurostotonus develops.
At the same time, tonic tension spreads to the intercostal muscles and diaphragm, which leads to difficult shallow and rapid breathing. Due to tonic tension of the perineal muscles, difficulty urinating and defecating is observed. Tonic contraction applies mainly to the large muscles of the limbs. The muscles of the feet, hands, and fingers are not tense. This period of the disease is characterized by severe sweating and hypersalivation. The tongue is dry, the patient is thirsty due to significant loss of water through sweat. The body temperature is febrile. Against the background of constant hypertonicity, general clonic (tetanic) convulsions occur, which last from several seconds to 1 minute and are repeated several times a day. Then they become frequent and prolonged, repeating several times an hour and even every minute (“status tetanicus”). During convulsions, the patient's face turns blue, swells, takes on a pained expression, opisthotonus becomes pronounced, and the body becomes covered with drops of sweat. The patients groan in pain.
Due to the high excitability of the nervous system, convulsions intensify under the influence of any irritant: touch, bright light, noise, air flow. In the future, they may even arise spontaneously. Severe attacks of spasms of the respiratory muscles, larynx, and diaphragm can cause asphyxia and death. Throat spasm significantly complicates the act of swallowing, which, together with trismus, leads to starvation and increases dehydration. Painful cramps are accompanied by insomnia, in which sleeping pills and narcotics are ineffective. Constant general hypertonicity and frequent attacks of convulsions sharply increase metabolism, accompanied by hyperthermia (up to 42 ° C) and profuse sweating.
Consciousness remains clear throughout the entire period of the disease, and can only become darkened before death. Changes in the circulatory system at the onset of the disease are characterized by tachycardia against the background of loud heart sounds, unstable blood pressure (mostly elevated, especially against the background of seizures). If disorders in the myocardium progress, the tones become dull, the boundaries of the heart expand, and cardiac paralysis is possible. The increase in convulsive symptoms occurs within 3-4 days, then in the next 5-7 days it remains at the same level and then gradually subsides. Improvement in the patient's condition is manifested by lengthening the periods between attacks, reducing trismus, and then a gradual decrease and disappearance of muscle tension in the lower extremities, back, back of the head, shoulder girdle and, ultimately, abdominal muscles.
The severity of generalized tetanus is determined not only by the duration of the incubation period, but also by the rate at which generalized clonic convulsions appear at the onset of the disease, their frequency, and the height of the fever. The presence and nature of complications are also taken into account.
A mild course is rare. The duration of the incubation period is more than 14 days. Symptoms of the disease appear and increase slowly over 5-6 days. Trismus, sardonic smile, opisthotonus are moderately expressed. Generalized convulsions are absent or observed rarely, there are no swallowing or breathing disorders. Body temperature is normal or subfebrile.
The course of moderate severity is characterized by a short incubation period (7-14 days). Symptoms increase over 3-4 days. The same symptoms are observed as in mild cases, but more pronounced. Muscle tone is moderately increased, generalized cramps occur several times a day and are short-lived. Body temperature can reach 38-38.5 °C. The duration of the disease is up to 1.5-2 weeks.
For severe tetanus, the incubation period usually lasts less than a week. The onset is acute, the clinical picture (before the onset of generalized convulsions) unfolds within 36-48 hours: severe tachycardia, frequent convulsions, often at short intervals, can be spontaneous, and respiratory distress occurs more than once. Body temperature reaches 39-40 °C, probably higher.
In extremely severe cases, the incubation period lasts several days. The disease develops at lightning speed, within 12-24 hours, sometimes from the first hours, accompanied by severe tachycardia, shortness of breath, frequent convulsions (every 3-5 minutes), cyanosis, and the threat of asphyxia. Obstetric tetanus develops very severely after illegal abortions or home births. The severity of the course is due to anaerobiosis in the uterine cavity and often the addition of a secondary staphylococcal infection, which leads to the development of sepsis and also contributes to the activation of tetanus bacillus. Occasionally, with this variant of generalized tetanus, Cl. tetani and in the patient’s blood.
Local tetanus is rare; clinical manifestations largely depend on the location of the wound. Its mild course is observed if the patient experiences pain and tonic muscle tension in the area of the entrance gate; tension increases with palpation and percussion in this area. Such symptoms may persist for weeks or months. Local tetanus usually does not progress; all its manifestations quickly disappear with timely treatment and treatment of the wound. Generalization of the process is rarely possible.
Head tetanus. A peculiar variant of it is facial paralytic tetanus Rose, which occurs when infected through a wound surface of the head, neck, or face. Paresis or paralysis of the facial nerve on the affected side develops in a peripheral manner. Trismus appears later, sometimes it can only be detected when chewing. A spasm of the sternocleidomastoid muscle, paralysis of the muscles of the eyeball and eyelids, and the soft palate on the affected side may occur. Speech disorders are observed, rarely - swallowing due to cramps of the throat muscles. In severe cases, paralysis of the vagus nerve occurs, which is accompanied by severe shortness of breath and tachycardia. Rose's tetanus can develop into a generalized form.
The most severe type of cephalic tetanus is Brunner's bulbar tetanus, which occurs when there is a wound to the head with damage to the brain matter. The incubation period is very short - less than 3 days. The disease occurs with primary damage and a sharp spasm of the muscles of the throat, glottis, diaphragm and intercostal muscles. In such cases, death is possible due to respiratory or cardiac paralysis. This form of tetanus should be considered a generalized process, developing in a descending manner.
Separately, tetanus of newborns is distinguished. The infection enters mainly through the umbilical cord, rarely through macerated skin or mucous membrane. The incubation period is from 1-3 to 7 days. The first sign is a change in the child's behavior. Due to trismus, he becomes restless, cries constantly, cannot suck, and squeezes the nipple with his gums during feeding. The skin of the face is wrinkled, the mouth is stretched, its corners are downturned. Muscle hypertonicity and tetanic spasms often manifest as blepharospasm, tremor of the lower lip, chin and tongue. Gradually, the tension spreads to the muscles of the neck, back, abdomen, and limbs. General convulsions occur very quickly (sometimes after 1-2 days), against the background of which there is an increase in body temperature, tachycardia, breathing disorders, up to asphyxia. The mortality rate for this form of tetanus is more than 90%.
How to treat tetanus?
Treatment of tetanus begins with mandatory hospitalization, regardless of the severity of its course. Hospitalization in the intensive care unit or specialized centers is advisable. The patient is transported by medical transport equipped with medications and special equipment for controlled breathing. Before transport, anticonvulsants are administered to prevent seizures.
Tetanus therapy is complex - a combination of etiotropic, pathogenetic, symptomatic. The following activities are planned:
- anticonvulsant treatment,
- surgical treatment of the wound,
- neutralization of toxin circulating in the blood,
- antibacterial therapy,
- maintaining vital body functions,
- elimination of hyperthermia, acidosis and dehydration,
- prevention and treatment of complications,
- proper regimen and care, good nutrition.
The first action of a doctor when prescribing treatment for a patient with tetanus is to resolve the urgent question: is muscle relaxant anesthesia with artificial ventilation necessary or will it be sufficient to use anticonvulsant drugs and their combinations.
The administration of anticonvulsants turns out to be an extremely important precursor to other treatment methods and manipulations, since the implementation of the latter without such preparation can intensify tetanic convulsions with corresponding negative consequences. To eliminate seizures, the patient is initially created with appropriate conditions - complete rest is provided with the exclusion of all external stimuli. For mild to moderate tetanus, diazepam is prescribed intramuscularly or in enemas every 3-4 hours (or other benzodiazepines that can be administered parenterally and in enemas, for example, gidazepam, phenazepam). It is recommended to use a lytic (neuroplegic) mixture, which includes 2 ml of a 2% solution of chlorpromazine, 1 ml of a 2% solution of trimeperidine (Promedol), 2 ml of a 1% solution of diphenhydramine and 1 ml of 0.05% butylscopolamine. The administration of diazepam or other benzodiazepines and the lytic mixture can be alternated throughout the day. For local tetanus without the threat of generalization, benzodiazepines are prescribed in tablets. In severe cases, the maximum increase in the dose of these drugs does not always achieve the desired result. In such cases, to relieve and prevent seizures, antidepolarizing muscle relaxants are used, which, being acetylcholine antagonists, block neuromuscular transmission. Their action is usually supplemented by the administration of benzodiazepines and antihistamines. Depolarizing muscle relaxants can also be used, but long-term use of these is possible only after the patient has been transferred to mechanical ventilation with intubation or tracheotomy and only in intensive care units.
A thorough surgical treatment of the wound is performed, its revision with previous local anesthesia and injection with antitetanus serum (TPS) in a dose of 1000-3000 IU. This also applies to small wounds that have healed at the time of illness and need to be opened.
In order to neutralize the circulating toxin, the patient is administered heterogeneous equine PPS (100,000-200,000 IU) intramuscularly or intravenously with previous desensitization or homologous human tetanus immunoglobulin as early as possible. Human immunoglobulin is considered the best antitoxic agent; its therapeutic dose is 900 IU.
With high-quality wound treatment, which eliminates the entry of new portions of the toxin into the blood, there is no need for repeated administration of serum or immunoglobulin. To create active antitoxic immunity, tetanus toxoid is subsequently used intramuscularly in a dose of 0.5 ml three times with an interval of 3-5 days.
Today, WHO recommends antibacterial therapy for tetanus, primarily with metronidazole intravenously. This drug has been proven to reduce the number of tetanus bacilli. Swedish penicillin, which was widely prescribed in the past, is practically not used due to the possibility of increased muscle spasms and the need for very frequent administration. It is also possible to prescribe doxycycline intravenously.
To prevent secondary microbial complications (pneumonia, sepsis), 3-4th generation cephalosporins and respiratory fluoroquinolones are used. To lower blood pressure, 20% magnesium sulfate is indicated intravenously several times a day. For severe tachycardia, beta blockers and cardiac glycosides are prescribed.
Correction of homeostasis is carried out according to the general principles of intensive care. Pronounced metabolic changes (acidosis), electrolyte imbalance are indications for the prescription of appropriate solutions, taking into account the nature and extent of these changes (alkaline, polyionic solutions).
With hyperthermia, there is a need to reduce body temperature - physical cooling methods and antipyretics are used.
In addition, the patient must be prescribed a diet of 3500-4000 calories and at least 150 g of protein per day through a tube and intravenously using special food mixtures. Oral nutrition in severe cases of tetanus due to severe trismus and tension of the diaphragm is possible only with liquid food, in small portions and with caution so as not to cause an attack of convulsions and asphyxia. A patient with tetanus should remain in bed for at least 2 weeks after the seizures have stopped. They carry out the prevention of bedsores and oral care.
Prognosis and prevention
Today, the incidence of tetanus remains consistently low, which creates the impression of its low prevalence and irrelevance.
However, this is not at all the case; the disease remains a problem.
Modern approaches, techniques, treatment methods, innovative medicines do not reduce the mortality statistics from tetanus.
The disease is very insidious and terrible because a conscious person experiences titanic torment. That is why it is necessary to pay special attention to the prevention of tetanus.
In medical practice, there are the following preventive approaches:
- nonspecific prevention of the disease, which consists of preventing household and work-related injuries, observing antiseptic rules in operating rooms and maternity wards, when treating wounds;
- specific prevention of the disease is carried out on a planned or emergency basis and consists of vaccination against tetanus starting from the age of three months, repeated three times every 45 days, then every 10 years;
- Emergency prevention of tetanus can be carried out in case of injury, both immediately and up to 20 days from the moment of injury, and consists of administering vaccination drugs and thoroughly treating the injury site.
Tetanus is an extremely dangerous disease that in most cases ends in death, which is frightening for many people. However, timely and complete tetanus vaccination can minimize the occurrence of tetanus and save people's lives.
Damage to the integrity of the skin due to poor asepsis and improper treatment can lead to infection. Bacteria affect a person through minor injuries: bruise, splinter, cut, bite. The symptoms of tetanus with a wound on the leg, which vary at each stage of the disease, deserve attention.
What diseases can it be associated with?
Complications of tetanus are divided into early and late:
- early ones occur during the height of the disease: bronchitis,
- pneumonia,
- sepsis - often due to gynecological tetanus,
- muscle and tendon ruptures,
- fractures of bones, spine,
- asphyxia, pulmonary atelectasis, hypoxia develop and intensify due to convulsions, aspiration of saliva and mucus,
- coronary spasm and myocardial infarction, mainly in elderly people due to prolonged spasms of the respiratory muscles,
- myocarditis due to the direct effect of tetanus toxin on the myocardium,
- fat embolism of the pulmonary artery due to fracture of bones rich in bone marrow,
- hemorrhages in the medulla, edema-swelling of the brain, intracranial hemorrhages with subsequent development of a coma,
- thrombosis of cerebral vessels against the background of seizures and severe metabolic disorders;
- prolonged tachycardia and hypotension,
Depending on the severity of the disease, mortality varies widely - from 10% to 70% or more. With mild tetanus, almost everyone recovers.
The insidiousness of a cat bite
Cats in most cases attack the hands and face of a person. Direct damage to the skin and tissues after an attack by a domestic or wild animal does not pose a great threat. Cats' jaws are not as powerful as those of dogs. In the rarest cases, when large arteries are damaged, there are risks to human life.
But the accumulation of pathogenic microorganisms in saliva and on cat fangs ensures infection at the time of a human bite.
A wound is formed, usually narrow, deep, and bacterially contaminated. The oral cavity of murks, especially street ones, is simply teeming with toxins. Even a small scratch can cause a lot of suppuration, a serious complication in the form of a soft tissue abscess, purulent inflammation.
The list of diseases that can be contracted from a cat bite includes the following diseases:
- wound botulism;
- chlamydia;
- pasteurellosis;
- rabies;
- tetanus;
- salmonellosis;
- streptococcosis.
The entry of the tetanus virus into the wound and then into the bloodstream does not manifest itself in any way at an early stage.
If the victim does not treat the bite of a domestic cat, the consequences, if infected, manifest themselves as symptoms of the disease after about 2 weeks, when the incubation period ends.
Treatment of tetanus at home
Treatment of tetanus must be carried out in a hospital setting, regardless of the severity of the clinical picture. Discharged from the hospital after clinical recovery. It is noteworthy that the patient remains in bed for another 2 weeks after the seizures have stopped.
During the recovery period, as well as for a long time after it, it is important to monitor your diet, which should be high in calories and contain a protein component.
Stages
Based on the existing clinical picture, tetanus is usually divided into a number of stages.
| Stage | Description |
| Lightweight | Duration up to 3 weeks. There is a moderate spasm on the face, sharp arching of the limbs may not appear at all, and the temperature is slightly elevated. |
| Average | In moderate cases, spasmodic signs are more pronounced, tachycardia is recorded, and the temperature increases to 38-39 degrees. Convulsive phenomena occur approximately once every half hour and last no more than a minute. |
| Heavy | The convulsions are intensified and intense, the grimace on the face changes. |
| Critical | In particularly severe cases, Bruner's tetanus is diagnosed, which damages the spinal cord function responsible for the functioning of the heart and lungs. Newborn children are more often susceptible to this form of the disease. |
Complications
The severity and presence of consequences for tetanus depends on the depth of its symptoms, which is determined by the extent and location of the pathogen population in the human body. The worst prognosis for complications will be in the fulminant form , when the death of adults or children is often recorded. Mild cases can be successfully treated and do not cause irreparable consequences.
Let's list what complications tetanus threatens if you do not get vaccinated against it, do not carry out prevention and do not engage in timely treatment:
- Foci of sepsis in the body,
- Muscle rupture
- Broken bones that could not withstand chronic stress. The complication is typical for young children.
- Inflammatory process in the lungs and bronchi,
What drugs are used to treat tetanus?
- Heterogeneous equine PPS - 100,000-200,000 IU intramuscularly or intravenously;
- Homologous human tetanus immunoglobulin - 900 IU intramuscularly or intravenously;
- Diazepam - intramuscularly or in enemas 0.005-0.01 mg every 3-4 hours;
- Doxycycline - intravenously 0.1 g 1 time per day for 7-10 days;
- Metronidazole - 1 g intravenously every 12 hours or 0.5 g every 6 hours for 7-10 days;
- Phenazepam - intravenously or intramuscularly 0.005-0.01 mg every 3-4 hours;
- 20% magnesium sulfate - 5-20 ml intravenously several times a day.
Treatment of tetanus with traditional methods
Treatment of tetanus with folk remedies is a very controversial process that raises a lot of doubts. You definitely shouldn’t resort to this at the stage of developing symptoms of the disease; in this case, it’s time to seek professional help. Folk remedies can be used to treat wounds received under questionable circumstances. At the same time, it is necessary to understand that an injury that causes serious concern should be a reason to contact a specialist and for professional prophylaxis of tetanus.
You can adopt the following recipes for treating wounds and medicinal baths:
- Pour 500 grams of chamomile inflorescences with cold water, place on low heat and boil for 10 minutes from the moment of boiling, dilute the concentrated decoction in the bathroom or use to treat a wound;
- Pour water over pine needles, cones and twigs, boil for half an hour, then cover the container with a lid or cloth and leave for up to half an hour; To take a bath, 1.5 liters of this hood will be enough for the total amount of water.
Symptoms of complications
An increase in signs of damage indicates the development of an inflammatory process.
Antibacterial therapy is required in the following cases:
- increased swelling in the bite area;
- the appearance of redness of the skin around the wound;
- suppuration at the site of inflammation.
After treating the injury from pus, regular dressings using a 10% hypertonic solution are required; ointment "Baneocin" with an antibacterial effect to accelerate healing.
In some cases, swelling of allergic origin appears. It is accompanied by the appearance of a rash on the skin and a feeling of itching. Why is a cat bite dangerous for people with immune hypersensitivity?
Anaphylactic shock may develop, which can be prevented by taking an antihistamine.
Mandatory consultation with a doctor is required in the following cases:
- prolonged bleeding from the wound;
- sensory disturbances at the site of the lesion;
- development of fever;
- presence of immunodeficiency;
- bite by an animal with obvious signs of disease;
- absence of vaccinations against tetanus and rabies in the affected person over the past 3-5 years.
In any medical institution, specialists know what to do in case of a cat bite.
Treatment of tetanus during pregnancy
The course of pregnancy against the background of tetanus is extremely difficult, therefore it is recommended to use all possible methods of prevention in order to avoid infection.
General prevention consists of disseminating medical knowledge about the ways of infection with tetanus and preventing injuries.
Specific prevention, its main measure to prevent the disease, involves active immunization, which is carried out as planned according to the vaccination calendar, as well as urgently. Active routine immunization is carried out with associated drugs: associated capityuk-diphtheria-tetanus (DTP) or associated diphtheria-tetanus (ATD) vaccine containing tetanus toxoid.
Children over 8 years of age and adults are vaccinated with ADS-M toxoid, a drug with a reduced antigen content. The vaccination calendar was developed by WHO, but in each country it may have its own characteristics and also change depending on the epidemic situation.
In Ukraine, routine immunization with DTP vaccine is given to children from 6 months of age, 0.5 ml three times with an interval of 30 days. Revaccination is indicated at 18 months, then at 6, 14 and 18 years. Further planned revaccinations for adults are carried out with ADS-M at intervals of 10 years from the previous vaccination.
Adolescents and adults who have not previously been vaccinated or do not have data regarding immunization are vaccinated with ADS-M three times (the interval between the first and second vaccination is 30-45 days, and between the second and third - 6-12 months).
Today, one of the priority global WHO programs is the elimination of maternal and neonatal tetanus by immunizing expectant mothers in areas at risk for this disease, combating prejudices and false traditions that lead to infection of newborns and infants. Emergency specific prevention is carried out when there is a threat of tetanus development (contaminated injuries of various types with damage to the skin or mucous membranes, frostbite, burns of II, III and IV degrees, out-of-hospital abortions and births, gangrene or tissue necrosis, animal bites, damage to the integrity of the intestines) at hospital emergency rooms . The wounds are subjected to careful surgical treatment. Further tactics depend on the vaccination status of the victim or patient and the availability of documented evidence of immunization against tetanus in the past.
Non-immunized and adults who do not have such documentary evidence carry out active-passive immunization: 0.5-1.0 ml of toxoid is administered, after 30 minutes in another part of the body - 3000 IU of PPS or tetanus immunoglobulin at a dose of 250 IU. Providing active immunization continues as usual with toxoid. Persons who have been vaccinated routinely, but have not had the latest age-related revaccination, are administered only 0.5 ml of toxoid.
First aid
The set of emergency measures is accessible; simple actions greatly reduce the risk of the tetanus virus entering the circulatory system and body tissues. What to do if you are bitten by an outdoor cat?
The algorithm of actions is as follows:
- Lightly press on the tissue adjacent to the wound to release harmful bacteria and microorganisms that did not have time to penetrate deeper with the blood.
- Wash the wound with plenty of running water and laundry soap, which enhances the antibacterial effect. If this is not possible, use temporarily wet wipes.
- Treat the damaged area with 3% hydrogen peroxide and a pharmaceutical antiseptic solution (Furacilin, Miramistin, Chlorhexidine).
- If there is swelling, lubricate the damaged area with the antimicrobial agent “Levomikol”; “Heparin” ointment is suitable for treating around the wound.
- Cover the wound with a sterile cloth and bandage the bite area.
- Check your tetanus (tetanus) vaccination history. If there is no vaccination for 3-5 years or more, you should contact the clinic. An injection of tetanus toxoid in a volume of 0.5 ml is administered under the shoulder blade.
For persons prone to allergic reactions, vaccination is carried out along with the administration of an antihistamine and observed for 30 minutes.
Post-traumatic swelling and pain subside with favorable developments after 1-2 days. The skin lesion dries out and decreases in size.
If the infection has penetrated into deep-lying tissues, then superficial treatment may not be effective enough.
Then the wound is widened, washed, drainage is placed if necessary and antibiotics are prescribed.
Which doctors should you contact if you have tetanus?
- Immunologist
- Infectious disease specialist
- Family doctor
The generalized form of tetanus is diagnosed based on the following data:
- a history of injury or trauma, burns, frostbite, surgery, childbirth, out-of-hospital abortion;
- information about previous tetanus vaccination.
The leading symptoms of clinical diagnosis are:
- presence of the classic early triad of symptoms (trismus, sardonic smile, dysphagia);
- constant tonic muscle tension, which does not disappear even during anesthesia;
- tetanic convulsions that occur periodically against the background of tonic tension;
- maintaining consciousness during seizures;
- fever, profuse sweating.
Local tetanus should be suspected if the patient experiences involuntary painful muscle twitching in the wound area.
As a rule, the diagnosis of tetanus is exclusively clinical and epidemiological. Specific diagnostics are usually not performed.
In some unexplained cases, bacteriological methods are used - the pathogen can be detected in the wound using bacterioscopy and isolated when inoculated on appropriate nutrient media under anaerobic conditions (blood agar, yolk agar, Kitt-Garonnet medium, Wilson-Blair medium), but no more than 1/3 of patients. To determine the toxin in the test material, a biological test on white mice is sometimes used according to the type of toxin neutralization reaction.
The determination of antitoxic antibodies has no diagnostic value; it only indicates a history of vaccinations, and an increase in their titer does not occur due to the lack of an immune response to the action of the exotoxin.
Diagnostics
The clinical manifestation of tetanus in a child and an adult patient is so specific that identifying it is not difficult; early diagnosis is quite possible. For research to detect the pathogen, suture or dressing material, swabs from surgical instruments, air, soil, and dust can be exposed. Often a scraping from the wound is taken for analysis, possibly a smear from the nasal mucosa, pharynx, or vagina. Mice are used to test tetanus exotoxin secretions.
You were recently bitten by a dog, did you treat the wound, but did not seek medical help? Did you know that you have a good chance of getting tetanus? In this article we will talk about what symptoms of tetanus appear in a person after a bite and how soon to expect the first signs of the disease.
Treatment of other diseases starting with the letter - s
| Treatment of salmonellosis |
| Treatment of cutaneous sarcoidosis |
| Treatment of pulmonary sarcoidosis |
| Treatment of Kaposi's sarcoma |
| Treatment of uterine sarcoma |
| Treatment of Ewing's sarcoma |
| Treatment of type 2 diabetes mellitus |
| Treatment of type 1 diabetes mellitus |
| Treatment of seborrhea |
| Treatment of sepsis |
| Treatment of heart failure |
| Treatment of anthrax |
| Treatment of Budd-Chiari syndrome |
| Treatment of Guillain-Barré syndrome |
| Treatment of Gilbert's syndrome |
| Treatment of Parhon's syndrome |
| Treatment of polycystic ovary syndrome |
| Treatment of empty sella syndrome |
| Treatment of irritable bowel syndrome |
| Treatment of Sjögren's syndrome |
| Treatment of sinusitis |
| Treatment of systemic lupus erythematosus |
| Treatment of systemic scleroderma |
| Treatment of systemic sclerosis |
| Treatment of syphilis |
| Treatment of scoliosis |
| Treatment of somatoform disorders |
| Treatment of spinal stroke |
| Treatment of spondylosis and spondyloarthrosis |
| Treatment of laryngeal stenosis |
| Treatment of tracheal stenosis |
| Treatment of stenosing ligamentitis |
| Treatment of stomatitis |
| Treatment of ringworm |
| Treatment of subarachnoid hemorrhage |
| Treatment of subdural hematoma |
The information is for educational purposes only. Do not self-medicate; For all questions regarding the definition of the disease and methods of its treatment, consult your doctor. EUROLAB is not responsible for the consequences caused by the use of information posted on the portal.