Benign paroxysmal positional vertigo (BPPV) is a fairly common pathological condition that occurs in the majority of patients who seek medical help. This dizziness is caused by most lesions of the vestibular system.
What is BPPV?
This disease is detected in approximately 80% of people who seek medical help. Recently the number of requests has increased significantly. Most patients are diagnosed with benign dizziness (vertigo).
What is the essence of the problem of BPPV, what is it? A brief description of the disease can be presented as follows:
- Benign – has no consequences, there is the possibility of self-cure.
- Paroxysmal - has a paroxysmal character.
- Positional – the disease manifests itself due to a change in the position of the body or head.
- Dizziness is the main symptom of the disease.
A person may feel dizzy due to many diseases. There are more than a hundred of them. But vestibular positional vertigo has distinctive clinical signs, thanks to which the doctor can make a diagnosis at the first examination.
Features of the manifestation of BPPV
The pathological condition occurs most often during movement or change of position. Benign dizziness lasts relatively short time. Even mild exercise can cause symptoms.
For more information about the disease, watch the video:
More often, signs of this type of dizziness appear in older people who are over 50 years old. In addition, it is diagnosed several times more often in women than in men. BPPV differs from other types of dizziness in that you can cope with it on your own. Moreover, treatment of benign paroxysmal positional attack is almost always effective.
BPPV has some distinctive symptoms that allow a correct diagnosis to be made during the first examination by a doctor.
How does the vestibular apparatus work?
Before talking about the causes of paroxysmal positional vertigo, it is necessary to consider how it occurs.
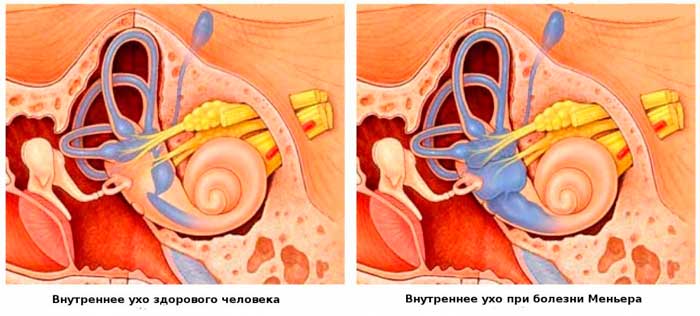
The organ in the inner ear, the vestibule, is based on three semicircular canals. Their function is to record human movements. The channels contain an ampoule and a certain amount of liquid. The ampoule is an extension that houses a gelatin-like substrate, the cupula. Her movements, interacting with receptors, help create a sense of balance in her body.
The liquid in the ampoule contains calcareous formations called otoliths. When a person performs any actions with his head, the liquid also begins to move. As a result, the otoliths are displaced, which irritate the nerve endings (ciliated cells).
All information about a change in position is transmitted by ciliated cells to the nerve endings of the brain. Due to failures and problems at this stage, a person develops benign paroxysmal vertigo. The part of the brain responsible for balance gives a signal to the muscles, thanks to which they relax or, conversely, become toned. These processes are aimed at maintaining balance in space. When the otoliths settle, the dizziness stops.
What's happening?
To understand the mechanism of development of dizziness, mention should be made of the structure of the vestibular apparatus.
The organ of balance is located in the cavity of the inner ear and is represented by a system of semicircular canals, round and oval sacs and the vestibular nerve .
The semicircular canals are three canals located in mutually perpendicular planes at right angles. The canals, like the oval and round sacs, are filled with a fluid called endolymph , and their inner surface is lined with hair cells , which are receptors of the vestibular apparatus. The hair cells of the semicircular canals perceive rotational movements, and the cells of the saccules respond to changes in the speed of rectilinear movement.
otoliths , float freely in the cavity of the sacs . With the pathological movement of otoliths into the cavity of the semicircular canals, the crystals impact the hair cells and a feeling of dizziness occurs.
Causes of BPPV

The cause of this disease is still not clear. In some other cases, benign paroxysmal dizziness is caused by the following factors:
- Head injuries.
- Surgical operations on the ear.
- Prolonged lying down (due to other diseases, recovery after surgery, etc.).
- Inflammatory ear processes.
- Spasm of the labyrinthine artery (with migraine).
- Meniere's disease.
- Alcohol intoxication.
- Consequences of improper treatment.
Classification of BPPV
The classification of positional vertigo is based on the mechanism of its development. Lime crystals (otoliths) can move freely in the fluid of the semicircular canal, irritating the receptors during head turns. This is canalolithiasis. When otoliths are localized on the canal wall (cupula) and constantly interact with receptors - cupulolithiasis.
When making a diagnosis, both the side of the lesion (left-sided, right-sided) and the semicircular canal (external, posterior, anterior) in which pathological changes occurred are taken into account.
Definition and classification of dizziness
Dizziness (vertigo) is a feeling of imaginary rotation of a person in different planes , as well as illusory rotation of a non-dynamic surrounding space in any of the planes.
Traditionally, systemic and non-systemic dizziness are distinguished.

Systemic (vestibular) - caused by direct damage to the vestibular apparatus. It is divided into peripheral and central, which depends on the location of the disorder. Peripheral systemic vertigo is caused by damage to the semicircular canals and vestibular nodes, and central is caused by damage to the nuclei located in the brain stem and associated with the cerebellum and cerebral hemispheres.- Non-systemic - occurs due to a mismatch in the functioning of the vestibular, visual and proprioceptive analyzers. Balance imbalance is described as a feeling of instability and difficulty maintaining a posture. Accompanied by a feeling of lightheadedness, nausea, vomiting, vegetative reactions (sweating, increased heart rate, pallor).
Distinctive signs of BPPV
The following signs characterizing paroxysmal positional vertigo are distinguished:
- Vertigo attacks begin and end unexpectedly.
- After 24 hours, they no longer occur.
- The patient’s well-being immediately improves after the attack.
- Associated symptoms may occur: fever, sweating, nausea and pale skin.
- The recovery period after illness is quite fast.
The above features of BPPV will help to recognize it among other diseases, the symptom of which is dizziness.
BPPV Clinic
The appearance of benign paroxysmal dizziness is associated with head movements. Usually the disease affects only part of the head, since one hemisphere of the brain (or ear) is left unaffected.
The clinical features of BPPV are as follows:
- Dizziness occurs mainly when turning (tilting) the head, not the body. It usually occurs during the day or in the morning, for example, after waking up when getting out of bed.
- A person may feel that he is falling somewhere or rising, he is swaying, objects around him are rotating.
- Associated symptoms may include nausea, sweating, vomiting, and palpitations.
- Patients do not have any additional complaints (head pain, tinnitus, hearing loss).
- One attack lasts no more than one or two minutes.
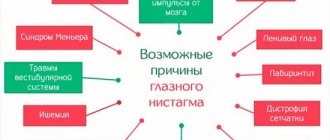
- An attack of dizziness may be accompanied by nystagmus. These are involuntary movements of the eyeball. After the attack subsides, the nystagmus disappears.
The disease is highly treatable and does not pose a serious threat to the patient’s life. But if a person has been diagnosed with benign positional vertigo, he should avoid diving and climbing to heights. After proper treatment, the disease may subside for a long time, but after 4-5 years the attacks usually return.
What to do if dizziness occurs?
BPPV is just one of many conditions that can cause balance problems. There are many reasons for dizziness, and many of them require immediate treatment. Therefore, such attacks should not be ignored. If you feel a sharp imbalance, a sense of rotation of surrounding objects or your own body in space, if this is accompanied by nausea, vomiting or blurred vision, this is a good reason to contact a therapist, pediatrician or ENT clinic as soon as possible.
Doctors' opinions on treatment
In 1969, a theory was put forward about the origin of benign paroxysmal vertigo - the “dome lithiasis theory.” Its author (scientist Schuknecht) said that with age, calcium deposits appear on the otoliths of a person, which contribute to the weight of lime crystals, and they change their neutral position. In this regard, the position of a person’s body and the force of gravity that acts on it affect the appearance of BPPV.
Ten years later, scientists McClure, Hall and Ruby put forward the theory of “canalolithiasis.” According to this theory, particles of statoconia, which move along the canal and excite receptors, provoke the appearance of positional vertigo, but the otoliths are not involved. When the particles reach the lowest point of the channel, the attack disappears.
Scientists of modern medicine criticize the above theories. They say that statoconium particles can come off even when the human body is stationary. They name the following reasons for their rejection, which results in benign dizziness:
- Head injuries.
- Meniere's disease.
- Certain antibacterial drugs (Gentamicin).
- Frequent migraines.
- Incorrect surgical treatment.
Diagnostics
In case of constantly recurring attacks, you should contact the clinic for consultation with a specialist. The doctor will prescribe the necessary examinations to make an accurate diagnosis.
Physical examination

The most common method that helps identify positional vertigo is the Dix-Hallpike test. The methodology for carrying it out is as follows:
- The patient needs to sit on an ottoman and turn his head at a certain angle to the side.
- The doctor, holding the person’s head with his hands, sharply places him back on the couch (on his back) so that the head is slightly further than the edge of the surface on which the patient is lying.
The patient will need to be informed of the onset of dizziness. It may not bother you right away, but after some time.
During positional vertigo, the eyeballs rotate involuntarily. This phenomenon is called nystagmus. The doctor determines in which part of the semicircular canal the pathology is present by the nature of the nystagmus and the time of its appearance.
Instrumental studies
For better visual observation of nystagmus, there is the practice of using Blessing or Frenzel glasses, electrooculography and videooculography.
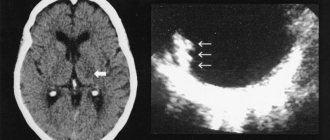
Along with the above diagnostic methods, the patient may be referred for an MRI or computed tomography of the brain, or an X-ray of the cervical spine.
Based on the results of the examination, the doctor will prescribe the necessary treatment. Some patients diagnosed with positional vertigo do not require treatment as it resolves on its own.
Diagnosis and treatment of benign paroxysmal positional vertigo
The most common cause of systemic vertigo is benign paroxysmal positional vertigo.
(BPPV). The disease can develop after middle ear infections, traumatic brain injury, prolonged bed rest, or otological surgery. In old age, BPPV often occurs after a labyrinthine infarction. In 50% of cases, the cause of BPPV cannot be determined. In women, the disease occurs 2 times more often than in men.
In pathogenesis
BPPV plays a leading role
cupulolithiasis
, which is a clot of calcium crystals.
Under the influence of its weight, the ampullary receptor, which normally perceives angular accelerations, comes into a state of irritation. BPPV occurs at a certain position of the head and torso in relation to gravity due to the movement of otolith fragments into the semicircular canals of the inner ear or their settling on the cupula of the ampullary receptor. Thus, cupulolithiasis
(
otolith particles on the cupula of the semicircular canal
) and
canalolithiasis
(
otolith conglomerate moves freely in the lumen of the semicircular canal
) are distinguished.
is most often involved
because it is in the plane of gravity.
An attack of BPPV begins after a certain latent period
(10 s). Initially, dizziness can be intense, accompanied by autonomic disorders and lasting about 1 minute. If you don't change your head position, it goes away quickly. If you change the position several times, BPPV disappears and does not recur, and after a long rest it appears again. There are no cochlear or other symptoms.
Currently, therapeutic manipulations
, aimed at moving otoliths from the semicircular canal back to the vestibule.
These manipulations allow the patient to completely relieve the symptoms of BPPV, but do not protect against the development of a possible relapse. In cases where it is not possible to remove the otolith from the semicircular canal, repeated provocation of dizziness leads to its gradual regression due to central compensation
.
Diagnosis of BPPV in lesions of the posterior semicircular canal
To confirm
For canalolithiasis of the posterior semicircular canal
of the right
labyrinth, the following maneuver is performed. The seated patient's head is turned 45° to the left. The examiner quickly positions the patient on the right side. After a latent period of several seconds, dizziness and nystagmus appear, gradually increasing, and then, when reaching a maximum, weakening and disappearing. Horizontal rotatory nystagmus is directed towards the underlying right ear. After the nystagmus and dizziness stop, the patient quickly moves back to the previous upright position in the “sitting” position. In most cases, dizziness and nystagmus reappear, much less intense, and the nystagmus is directed in the opposite direction - to the left.
To confirm canalolithiasis of the left
labyrinth, the head of the patient sitting in a straight vertical position is turned 45° to the right, and the patient is laid on his left side, by analogy with the previous turn.
Observation of positional nystagmus allows identifying diagnostic criteria
, typical for BPPV of the posterior semicircular canals (z-BPPV):
- latency
: dizziness and nystagmus begin one or several seconds after tilting the head towards the affected labyrinth and increase in intensity to a maximum; - reaction duration less than 40 s
: nystagmus gradually disappears after 10-40 s and ultimately weakens even with very rapid changes in head position; - linear-rotatory nystagmus is better visible in Frenzel glasses
(+16 diopters), which prevent suppression of nystagmus by the gaze reflex; horizontal nystagmus with a rotatory component is directed towards the underlying ear or upward if the gaze is directed towards the overlying ear; - reverse nystagmus
(changing direction): when the patient returns to the “sitting” position, dizziness and nystagmus of low intensity may occur, the nystagmus is directed in the opposite direction to the previously existing nystagmus; - tolerability
: constant repetitions of the maneuver can lead to the virtual disappearance of symptoms.
BPPV of the horizontal semicircular canal
The etiology of g-BPPV is the same as s-BPPV. Most cases are "idiopathic". BPPV of the horizontal semicircular canal (h-BPPV) is less frequently detected
- in approximately 10-20% of all patients with BPPV. It can be combined with s-BPPV of the opposite ear. Transitions between g-BPPV and s-BPPV are more often possible as a result of therapeutic positional maneuvers. While typical g-BPPV is caused by canalolithiasis, atypical g-BPPV may be caused by cupulolithiasis with unusual positional nystagmus.
The patient describes occasional dizziness when turning his head from side to side while lying on his back in bed. Therefore, the study of patients should begin with a s-BPPV test (sitting with the head turned 45°, etc.), and then a test with head turns to the right and left in a supine position (the actual s-BPPV test). It is better to take it energetically, after resting in bed.
The clinical characteristics of the g-BPPV variant are easily distinguished from s-BPPV (McClure (1985), BaLoh et al. (1993)). The diagnosis of g-BPPV is based on the following signs
(Strupp (1995)).
- Patients complain of short episodes of rotational vertigo, which are usually provoked by turning the head from side to side while lying on the back.
- Positional tests detect horizontal nystagmus striking toward the underlying ear (geotropic nystagmus) when the patient's head is rotated to the right and left around the longitudinal axis while the patient is lying on his back.
- Horizontal positional nystagmus when turning the head to one side or the other is stronger towards the affected ear. While maintaining this position, the nystagmus often changes direction.
- Positional nystagmus in g-BPPV has a short latency period (less than 5 s) and lasts longer (20-60 s) than s-BPPV.
- g-BPPV is rarely altered by repeated positional maneuvers.
- About 1/3 of patients show moderate horizontal semicircular canal paresis with caloric stimulation of the affected ear.
- Attacks of positional systemic vertigo are often more severe than with s-BPPV and are more often accompanied by vomiting. Unlike s-BPPV, attacks do not occur when lying down or getting out of bed, or when throwing back the head. Some patients describe brief episodes of dizziness when turning their head in an upright position (BaLoh et al. (1993)).
Anterior semicircular canal BPPV (a-BPPV)
p-BPPV is a rare form
BPPV, most often formed from s-BPPV and g-BPPV during maneuvers for their treatment (Hedman, Tusa (1996)). There is little information in the literature regarding p-BPPV. According to the effects of ampulofugal stimulation of the posterior semicircular canal, rotational vertigo in p-BPPV is associated with:
- downward positional nystagmus with a torsion component towards the affected superior ear;
- latent period, duration and change in direction of nystagmus (upward and torsional towards the unaffected ear) when the patient is seated in an upright sitting position (an effect similar to that of typical s-BPPV).
To confirm the diagnosis
p-BPPV is effective with the Dix-Halpike positional maneuver. In this case, the head of the patient sitting on the couch hangs down 145° and turns towards the unaffected ear, which leads to ampulofugal stimulation. The patient is then quickly returned to the upright sitting position from the previous position, which leads to ampulopetal stimulation.
For medicinal purposes
therapeutic maneuvers are performed, consisting of successive rapid lateral tilts of the head and torso, in order to move the conglomerate of particles towards the utriculus cavity. Currently, there are several varieties of techniques proposed by Semont, Epley, Brandt, Daroff, which are based on laying and turning the patient on a couch or other horizontal surface.
We used the following therapeutic procedures
. The patient was placed on the couch on the “sick” side, that is, on the side of the affected posterior semicircular canal. The patient should remain in this position until the dizziness stops (1-3 minutes). The doctor positions the patient's legs so as to be at the center of the rotation that he will perform next. The doctor's hand is located under the patient's head, clasping it in the neck and back of the head. Then the patient is abruptly shifted to the opposite side and held in this position for 5 minutes. If after a period of time from 1 s to 5 min. systemic dizziness appears, this means the release of otolith fragments from the posterior semicircular canal, which is confirmed by the occurrence of ageotropic nystagmus (beating towards the overlying ear). This sign is an indicator of a successful manipulation. After therapeutic manipulation, imbalance and dizziness lasting several hours may occur, indicating the return of otoliths to the elliptical sac. Complete elimination of BPPV symptoms in one session does not always occur; in this case, repeated sessions are required.
20 people under our supervision
, including 13 women and 7 men.
All had BPPV of the posterior semicircular canal. The patients' age ranged from 46 to 71 years
. To assess the severity of subjective symptoms arising during treatment, a visual analogue scale (VAS) was used. The following subjective symptoms were assessed on a 10-point scale: dizziness, vegetative manifestations, psycho-emotional reactions.
results
When performing the first stage of therapeutic manipulations—laying the patient on his side—all of them developed symptoms of BPPV, the duration and severity of which are indicated in Table. 1.
Table 1. Characteristic symptoms of BPPV
| Symptoms of BPPV | Duration, sec. | VAS scale score, point |
| Nystagmus | 46,5 ± 4,9 | |
| Dizziness | 125,3 ± 9,3 | 8,0 ± 0,92 |
| Autonomic symptoms | 138,9 ± 18,4 | 7,6 ± 0,85 |
| Psycho-emotional reactions | 178 ± 20,5 | 8,1 ± 0,94 |
When performing the second stage of the technique - turning the patient over to the opposite side - powerful systemic dizziness and ageotropic nystagmus lasting more than 1.5 minutes appeared after 20-150 s, which indicated a successful manipulation. Moreover, the severity of subjective symptoms was higher than during stage I:
- dizziness - 9.5 ± 0.97 points;
- vegetative symptoms - 9.0 ± 0.93;
- psycho-emotional reactions - 9.4 ± 1.1 points.
The therapeutic manipulations turned out to be effective in 17 patients, and in 8 of them the symptoms of BPPV were eliminated in one session
.
The rest are 9 people. repeated sessions were required the next day (from 2 to 7). It should be noted that most patients, after successful maneuvers, experienced dizziness and instability when walking for several days
. This is otolithic dizziness, apparently associated with the entry of a conglomerate into the receptor field of the utriculus - the macula.
Because vestibular dysfunction usually persists for some time
after the therapeutic manipulations, it is advisable to prescribe drug therapy aimed at reducing vestibular excitability (vestibulolytic drugs). For this purpose, drugs are used that act on vestibular receptors or on central vestibular structures.
Recently, betahistine dihydrochloride
(betaserk).
Summarizing the results of a number of studies, it should be emphasized that the analysis of the action of betaserc indicates a versatile effect on various pathogenetic mechanisms of dizziness, therefore, the pathogenetic validity of the use of the drug. Betaserc acts on histamine H1 and H3 receptors in the inner ear and vestibular nuclei of the central nervous system. Through a direct agonistic effect on the H1 receptors of the vessels of the inner ear, as well as indirectly through the effect on the H3 receptors, the drug improves microcirculation and capillary permeability, normalizes endolymph pressure in the labyrinth and cochlea, and increases blood flow in the basilar arteries. Betaserc also has a pronounced central effect, being an inhibitor of H3 receptors in the nuclei of the vestibular nerve, and normalizes neuronal transmission in polysynaptic neurons at the level of the brain stem. In recent years, it has been revealed that betaserc indirectly, through its effect on H3 receptors, in the brain stem increases the level of a neurotransmitter such as serotonin, which reduces the activity of the vestibular nuclei. It has been proven that the optimal regimen for taking betaserc is 24 mg orally 2 times a day
.
For drugs that act on vestibular receptors
, relate:
- anticholinergic drugs (scopolamine 0.25 mg 2 times a day), etc.;
- antihistamines (promethazine 25-50 mg orally 4-6 times a day), etc.
Central vestibulolytic drugs include benzodiazepines
:
- diazepam - 5-10 mg orally 3-4 times a day;
- alprazolam - 0.25-1 mg 3 times a day.
It is also advisable to prescribe antidepressants
, especially in the presence of a depressive component:
- imipramine 0.025 - 1 tablet 3 times a day for 2-3 weeks;
- amitriptyline 0.025 - 1 tablet 2-3 times a day for up to 3 weeks;
- fevarin 0.05 - 1 tablet at night.
Vasodilators and antiplatelet agents
:
- xanthinol nicotinate 0.15 - 1 tablet 3 times a day for up to 2 months;
- Cavinton 0.005 - 1 tablet 3 times a day for 2 months;
- tanakan 0.04 - 1 tablet 3 times a day for up to 3 months;
- pentoxifylline 0.1 - 1 tablet 3 times a day for 3 weeks.
For elderly people, calcium channel blockers
:
- cinnarizine 0.025 - 1 tablet 3 times a day from 3 weeks to 2-3 months;
- flunarizine 0.005 - 1 tablet 2 times a day for 3 weeks;
- nimodipine 0.03 - 1 tablet 3-4 times a day for 3 weeks.
a special complex of vestibular gymnastics are of decisive importance in restoring the functions of the vestibular system.
. For any type of dizziness, rational psychotherapy is of great importance.
Thus, adequate pharmacotherapy in combination with a complex of vestibular gymnastics and psychotherapy are necessary measures in the treatment of patients with benign paroxysmal positional vertigo.
Likhachev S. A., Alenikova O. A.
Republican Scientific and Practical Center of Neurology and Neurosurgery. Published: “Medical Panorama” No. 5, April 2008.
Non-drug treatment
This therapy gives a very good effect. It involves the patient performing positional maneuvers (changing the position of the body and head). When performing exercises, an attack of benign paroxysmal positional vertigo is possible. It is also worth remembering that some sets of exercises should be performed under the strict supervision of a specialist. The patient performs all maneuvers while sitting on an ottoman with his legs down.
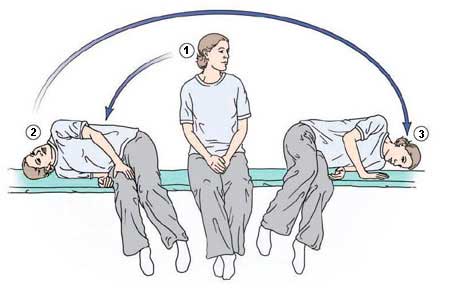
Brandt-Daroff maneuver
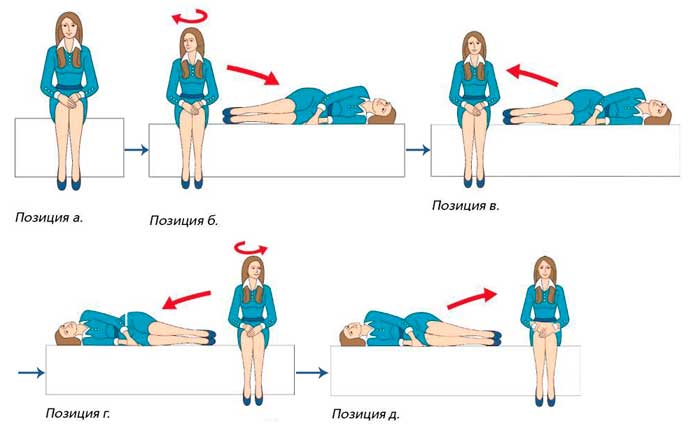
These exercises can be performed independently, the number of repetitions is five times in each direction. Progress:
- Take the starting position.
- Lie on your side (legs slightly bent) and turn your head to the side 45 degrees. Lie like this for 30 seconds.
- Sit down.
- Lie on the opposite side.
- Sit down.
If performing exercises is accompanied by the appearance of benign positional vertigo, then you should wait until the attack passes and continue further.
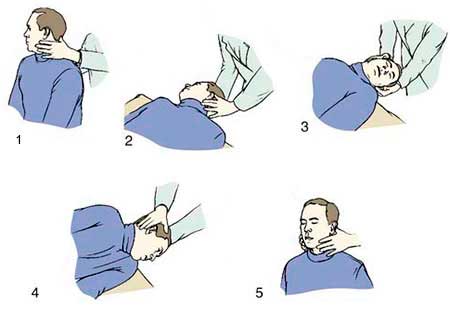
Semont maneuver
This set of exercises should be done under the guidance of a doctor, as nausea and other severe reactions may occur during the process.
To perform the exercises, a person needs to take a certain position. The next step is for the doctor to fix the patient’s head with his own hands; it should be turned to the side by 45 degrees. Next, the patient falls onto his side and remains in this position for a couple of minutes. Then he sits down again and immediately lies down in the same way on the other side for two minutes, after which he needs to sit down. All this time the head remains in the same position.
This set of exercises causes conflicting attitudes among doctors. Some recommend more gentle exercises, while others, on the contrary, consider this complex to be the most effective, even if benign paroxysmal positional vertigo is severe.
Epley and Lempert maneuver
This maneuver also requires the presence of a medic. The doctor, holding the patient's head, abruptly places him on his back (his head goes over the edge of the couch). The patient lies like this for about a minute, and then he needs to turn his head in the other direction, gradually turning his torso. So you need to lie down for 30-60 minutes, and then return to the starting position.
A similar exercise is the Lempert maneuver. When performing it, the patient turns over completely during the exercise: first to one side, then on his stomach, then on the sore ear and sits down. It turns out that during the exercise the person rotates around his axis.
How is the disease diagnosed?
Benign paroxysmal positional vertigo is diagnosed quickly and easily. The doctor just needs to listen carefully to the patient’s complaints and ask a few questions. However, in order for the diagnosis to be made as accurately as possible, the doctor can perform a special Dix-Hallpike test.
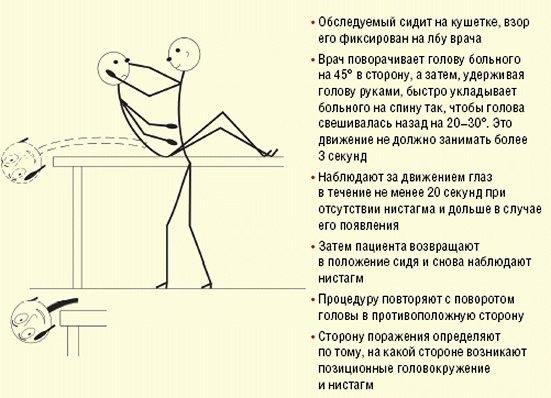
Dix-Hallpike maneuver technique
It's not difficult to do. To do this, the patient is asked to sit on the couch, and the doctor turns his head to the left or right 45 degrees. This way the head is fixed, and the patient quickly lies on his back. The rotation angle must not be violated. And your head should be tilted back a little, that is, slightly hanging off the couch. Next, the doctor should observe eye movements and ask the patient about his sensations.
If the test is positive, the doctor can make a diagnosis. In order to notice nystagmus (eye movement), a specialist will need special glasses. Infrared motion detection is also used.
For a detailed story about the diagnosis, watch the video from Candidate of Medical Sciences, Associate Professor of the Department of Otolaryngology, Russian National Research Medical University named after. N. I. Pirogova Alexandra Leonidovna Guseva:
Diagnosis must be differential to exclude the presence of brain tumors. In this case, additional instrumental research methods are used: MRI or CT. Characteristic of serious brain damage is the presence of neurological signs, which are completely absent in paroxysmal vertigo.
The patient should also exclude stroke, symptoms of multiple sclerosis, and vertebrobasilar circulatory failure.
They are characterized by additional symptoms that do not appear with paroxysmal positional vertigo.
Drug treatment
In order to alleviate the condition of a patient suffering from benign paroxysmal vertigo, medication treatment can be used. It will help get rid of nausea and other unpleasant symptoms. If attacks recur frequently, the patient must remain in bed.
The goal of treating such dizziness with medications is to improve the general condition of the patient. At the same time, medications may be prescribed that will help normalize blood circulation in the vessels of the brain.
In severe cases, surgery may be performed. It is used to fill the semicircular canal with bone chips. The surgical intervention method is used only in severe cases, as there is a risk of serious complications. There is no specific drug treatment for BPH.
Benign positional vertigo has a favorable prognosis for recovery. BPPV is a safe disease and does not pose a threat to human life.
Treatment of positional vertigo
DDPH is one of the few pathologies that does not require complex conservative or surgical treatment methods for complete cure. The basis of BPPV therapy is repositioning maneuvers , which are carried out to eliminate otolithiasis in the semicircular canals.
- Brandt-Daroff exercise - performed at home, in the morning, after waking up. The initial position is sitting in bed with your legs down. Then the head turns to the right to an angle of 45° and the person lies on his left side. You need to stay in this position for 30 seconds. Then you immediately need to lie on your right side, first turning your head to the left, and take this position for 30 seconds. After this, you need to take the starting position.
- The Epley maneuver is performed when otoliths are localized in the posterior semicircular canal and the Dix-Hallpike test is positive. The maneuver is carried out in several stages, each stage lasting 30 seconds. Initially, the patient is seated on the couch with his legs hanging down and his head is turned 45° towards the damaged canal. Then he is laid on the couch so that his head hangs freely below the edge of the couch. After this, the head is turned 90°, then turned to the side, and then face down. At the end of the maneuver, the patient again takes a sitting position, the head must be bent and pressed to the chest.
- The Lempert maneuver is used for damage to the horizontal semicircular canal. Procedure: the patient takes a horizontal position, then the head is turned to one side in the direction of the injury and held for 90 seconds. Then the patient sequentially turns to the healthy side 360° around the longitudinal axis in 90° increments. Each position is fixed for 90 seconds.
Among medications, vitamin D preparations and betahistine are used, but they are inferior in effectiveness to repositioning maneuvers. The previously used neurectomy is not used today. Treatment with folk remedies using Malysheva’s method also does not bring the desired results.
The problem of diagnosis and treatment of various types of dizziness is relevant and plays a leading role in the development of modern neurology. The application of modern theoretical developments in real practice will allow patients with this disease to be treated faster and more effectively.