Rabies (rabies) is an acute zoonotic disease of viral etiology that develops after a person is bitten by an infected animal. The disease is caused by RNA viruses (rhabdoviruses).
The disease manifests itself as severe damage to the central nervous system and death. There is no cure for rabies. The rabies vaccine is the only chance for a person bitten by a sick animal to survive. Therefore, vaccination should be carried out immediately.
Most cases of rabies development in patients are caused by late seeking specialized help, as well as by violation of the recommended regimen during the period of preventive vaccination or by failure to complete the course of specific immunization.
What is rabies
Rabies, also known as hydrophobia, is a viral disease that causes acute encephalitis (inflammation of the brain). Found only in mammals.
Characteristics of Rabies Virus: As a member of the genus Lyssavirus in the family Rhabdoviridae, rabies virus is an enveloped, bullet-shaped virus approximately 75 nm in diameter and 180 nm in length, having a single-stranded, negative-sense RNA genome. The genus Lyssavirus consists of 7 members, of which only serotype 1 commonly infects humans, and the remaining 6 are rare causes of human disease.
The rabies virus enters the brain through peripheral nerves. From the moment of entry, the virus quickly spreads along the nerve pathways into the central nervous system and then further into the organs.
Incubation period for rabies
Scheme of damage to the central nervous system by the rabies virus.
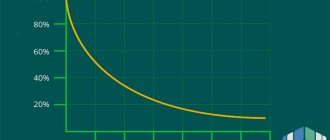
The incubation period of the disease depends on the distance the virus travels to the central nervous system (central nervous system), usually it takes several months. The incubation period of rabies can be short (9 days), long (99 days), but on average it is 30-40 days. This period may be shortened if the bite was on the head, and lengthened if the bite was on the limbs. All this time the person feels satisfactory. Well, except that he feels a pulling and aching pain at the site of the bite and along the nerves and itching appears. The scar sometimes becomes inflamed. These symptoms are especially characteristic within 1-14 days before the onset of the disease. Once the infection reaches the central nervous system and symptoms begin to appear. Rabies has the highest mortality rate—99.9%—of any disease on Earth. Any mammal can become infected with the rabies virus, including humans, and develop symptoms.
What to do if you are bitten
” After suspicious contact, it is necessary to urgently rinse and disinfect the wound (abrasion, scratch) into which the animal’s saliva has entered.
Disinfecting a wound is considered a way to reduce the risk of infection, slow down the penetration of the virus into nerve endings, the standard recommendation is to wash the bite site with soap and water for 15 minutes, and then apply any disinfectant solution.
After disinfecting the wound, you should immediately contact a medical facility for post-exposure vaccination.
” The post-exposure rabies prophylaxis regimen includes six administrations of the vaccine (on the day of treatment, on the third, seventh, fourteenth, thirtieth and ninetieth day).
Standard recommendations in Russia are the exclusion of alcohol and physical activity, however, in the instructions for vaccines and WHO recommendations there is no indication of the need to limit the intake of any food and drinks (including alcohol), as well as physical activity, visiting the sauna and solarium. There is even an opinion that Russian doctors introduced restrictions on alcohol consumption in order to discipline patients, whom festive libations could make them forget about the need for another procedure.
However, the effectiveness of rabies vaccination may be reduced while taking other medications (for example, corticosteroids, immunosuppressants).
” In addition to administering the rabies vaccine, you may also need rabies immunoglobulin - the decision about the need for its use is made by the attending physician.
According to WHO recommendations, the scope of post-exposure rabies prophylaxis is determined by the nature of the interaction with a potentially sick animal, the type of animal, the location of the bite and the area of the affected area.
” If contact with the animal occurred without biting or licking damaged areas of the skin, preventive measures are not required.
If contact with the animal involved biting bare skin, scratches and minor abrasions remain, urgent disinfection of the damaged areas and administration of an anti-rabies vaccine are necessary.
How is rabies transmitted?
Rabies is most often transmitted to humans through the bite of an animal infected with rabies. Bites to the head, neck and arms are most likely to transmit the infection. The amount of virus entering the body that reaches the lesion is also a transmission factor. For example, when a bite must penetrate clothing, saliva may remain in the fabric and prevent it from entering the bloodstream. Potential routes of transmission without bites include contamination of a pre-existing wound, mucosal or respiratory tract contact with saliva of an infected animal, or exposure to aerosolized rabies virus in the laboratory (or from bats). Direct person-to-person transmission is theoretically possible, but is rare and has only been documented in cases of transplantation (cornea, kidney, liver, blood vessels)
Vaccinations
Rules for rabies vaccination of dogs in Russia
There is a vaccination schedule for dogs, which indicates the recommended age of the animal.
Sometimes the vaccination date is postponed on the recommendation of a veterinarian for some reasons, for example, cropping of ears, weakened immunity, or change of teeth in a puppy.
Complex vaccine
There are mono-vaccines that protect against one disease, and poly-vaccines - complex preparations that form immunity against several diseases at once.
Polyvaccines are most often used for adult dogs to support already developed immunity.
Where to do it?
Vaccination of animals is carried out in any veterinary clinic.
If there are no contraindications at the moment, vaccination is carried out on the same day according to the instructions for the drug.
Free vaccination
On the territory of Russia, vaccination is free and mandatory for all dogs in regions affected by the epizootic situation of rabies.
Vaccination is carried out in state veterinary clinics and vaccination centers.
How to prepare your dog for vaccination?
Only healthy animals are vaccinated. A week or two before the expected date of vaccination, deworming is carried out - treatment for possible helminthic infestations.
Animals infected with worms are not allowed to receive vaccination.
When to do it?
According to the vaccination schedule for dogs, the first vaccination is carried out in puppies at the age of three months - preferably before the first change of teeth.
Sometimes, for health reasons or on the recommendation of a veterinarian, vaccination is postponed for up to six months.
If vaccination is carried out before three months of age, re-vaccination is carried out after two to three weeks for a more stable formation of immunity
. For older puppies, one vaccine is enough.
How long does it last?
On average, a dog's immunity lasts for a year.
Expensive drugs can provide longer-lasting immunity. It weakens over time, so annual booster vaccination is recommended.
How often to repeat?
Revaccination is carried out every year, at approximately the same time, coinciding with the first vaccination by month.
Sometimes, depending on the drug used, revaccination is carried out every two to three years.
Contraindications
On the day of vaccination, the veterinarian must examine the animal for contraindications. If the dog has an elevated body temperature, helminthic infestations, or the dog looks sick or exhausted, vaccination is postponed.
Contraindications include recent injuries and weakened immunity.
How to do it yourself?
You can vaccinate a dog yourself, but in this case you will not be able to enter information about the procedure into the veterinary passport.
It is recommended to carry out this procedure in a veterinary clinic. The doctor can choose the right drug and the required dose.
Where is the injection given?
Most anti-rabies injections are given intramuscularly in the thigh area.
It is possible for some drugs to be administered subcutaneously into the withers area. Information on the rules for administering the drug is in the instructions for use.
Vaccination for an adult dog
If the dog was not vaccinated as a puppy, vaccinating it is not only acceptable, but also desirable.
Adult animals tolerate the first vaccination a little more difficult. However, it is easier to endure minor side effects from vaccination than to euthanize a sick animal.
Puppy
Puppies tolerate vaccination quite easily, side effects depend on the type of vaccine
and individual characteristics of the animal. The first vaccination is recommended for puppies.
Old dog
The vaccine is administered to healthy animals of any age. For some reasons, the veterinarian may refuse to vaccinate, citing the dog’s age and the state of the immune system.
In some cases, older dogs should not be injured by the introduction of an anti-rabies vaccine.
Can a vaccinated dog get sick?
Cases of disease in properly vaccinated dogs are extremely rare.
Vaccinated dogs develop powerful immunity against the rabies virus. The percentage of sick vaccinated dogs averages 4–5%.
What if a vaccinated dog bites?
If a person or animal is bitten by a dog that is known to be vaccinated against rabies, administration of rabies immunoglobulin is not necessary.
It is enough to treat the wound with disinfectants to prevent the addition of a secondary infection.
Signs of rabies
The rabies virus can cause an acute infection accompanied by progressive encephalomyelitis and is usually fatal. The initial symptoms of rabies resemble those of other systemic viral infections, including
- fever,
- headache,
- malaise,
- diseases of the upper respiratory tract and gastrointestinal tract.
This prodromal phase (the period of illness that occurs between the incubation period and the disease) is 4 to 10 days before the appearance of specific symptoms. Almost all clinical cases of rabies are fatal. Human rabies usually occurs in two forms: rabid and paralytic (silent).
Furious rabies: accounts for 80% of rabies cases, encephalitis predominates and is manifested by hydrophobia, delirium (delirium) and agitation. Hydrophobia is the symptom most often identified with rabies; patients have severe difficulty swallowing and may become frightened at the sight of water, despite being very thirsty. Other manifestations of violent rabies include hyperactivity, seizures, and aerophobia. Hyperventilation is often present, presumably reflecting infection of the brainstem. Patients then fall into a coma and usually die within 1-2 weeks, despite maximum intensive care.
Paralytic (silent) rabies: Unlike frenzied rabies, patients with paralytic rabies do not show signs of cortical irritation, but instead have ascending paralysis or symmetrical tetraparalysis. As the condition progresses, the patient loses consciousness and death may occur, followed by coma.
Violent form - main symptoms
Symptoms of rabies in cats appear gradually in accordance with the stages of the disease. After a bite, the virus penetrates through the nerve trunks to the brain. The incubation period can last from 2 to 6 weeks in cats, most often the clinical picture is observed on days 10-18.
When Rabies virus reaches the cerebral cortex, it will also be present in the saliva of the kitten or cat. It is at this moment that the individual is already capable of infecting other pets, as well as humans.
How does rabies manifest in cats? The disease occurs in three different forms, and animals behave differently.
There are three stages of the impact of infection on the body: prodromal, manic, depressive.
At the first stage, characteristic signs can help identify rabies in a cat:
- significant change in mood;
- constant need for the owner’s attention, the need for the animal to be stroked;
- the pet rubs its head against the human body;
- frequent licking of the skin.
Other first signs of rabies in cats also appear:
- increased drowsiness;
- fear of light and desire to hide in a dark and deserted place;
- refusal to eat, loss of appetite;
- food interest in inedible objects;
- digestive disorders (vomiting, diarrhea, salivation);
- itching at the site of the bite.
How long do cats with rabies remain in this state? The stage lasts 2-4 days.
The next stage is manic. Rabid adult cats do not yet become lethargic, but symptoms should already appear in a more pronounced form. You can recognize them after observing the pet’s condition:
- change in the appearance of the fur on the lower jaw (wetness, dishevelment);
- severe fear of water and light;
- complete refusal to eat;
- aggression towards people and the owner, the desire to scratch or bite;
- drooping of the lower jaw;
- the pupils change position, strabismus develops;
- Paralysis of the paws and larynx occurs.
Rabies in an adult cat causes fear and anxiety in the owner, as the animal becomes inadequate and does not respond to the human voice, calls or punishment. It is not possible to lure or calm with the help of “sweets”.
With rabies, the individual remains in the manic stage for 2-5 days.
The final stage is depressive. The animal can no longer lead an active lifestyle, severe apathy is observed, the pet begins to tremble convulsively, the tremor does not stop until death. Hoarseness is heard when inhaling and exhaling, it seems that a lump has formed in the throat.
Rabies in any cat ultimately ends in death, caused by general exhaustion of the body due to refusal of food and respiratory arrest. Death occurs within 1-3 days.
It is also called silent and is also known as the paralytic form. It differs in that the symptoms described above are not noticeable, since they do not appear clearly. In some cases, the owner manages to find out about the disease by closely monitoring the pet. He may become more affectionate if he previously did not show much interest in people and did not caress, tries to be constantly nearby, tries to sleep on the person’s body.
In this case, rabies in cats and the symptoms are hidden. The disease manifests itself unexpectedly and sharply, the signs become:
- pharynx paralysis;
- increased salivation;
- the cat is trying to cough something up;
- the animal appears to be choking.
At this point, it is already useless to look for how to determine rabies in a cat and methods of treatment, since after 2-4 days the individual will die.
The most difficult to diagnose and dangerous for humans, since the incubation period of rabies in cats is hidden. First, the animal shows signs of digestive upset, which forces you to contact a veterinarian and undergo an examination. Symptoms:
- diarrhea and loose stools;
- vomit;
- indifference to the environment;
- feces may come out with blood;
- exhaustion of the body.
Can a cat infect its owner? If a pet develops rabies in this form, the owner runs a very high risk of contracting rabies because he is unaware of the danger. The duration of existence of the pathology in this form is up to 3 months.
There are three main forms of this infection:
- violent;
- paralytic;
- atypical.
The violent form is most often recorded; the first signs of rabies in cats in this case are as follows:
- Change in the animal's behavior - sometimes the cat looks lethargic, avoids contact with people, and has no appetite. And sometimes, on the contrary, the animal behaves too intrusively and affectionately, constantly resting its head on its owner’s legs.
- Increasing feeling of anxiety, increased fearfulness. The cat constantly scratches and chews the bite site.
- Perversion of appetite - the cat does not eat regular food well, but greedily swallows inedible objects (pebbles, straw, wood chips...).
As the pathology progresses, the main signs of rabies in cats appear:
- Difficulty swallowing caused by spasms of the smooth muscles of the pharynx, accompanied by copious amounts of saliva. Sometimes owners think that the animal has choked on something.
- Increased aggressiveness, even to the point of rage - the cat rushes at people and animals. At the same time, such attacks are replaced by a state of depression and exhaustion. Moreover, at the slightest shout, noise, bright light, the attack of violence resumes.
- Exhaustion and loss of voice.
- Dropping of the lower jaw, protrusion of the tongue from the mouth, accompanied by copious amounts of saliva.
- Strabismus, dilated pupils, and sometimes clouding of the cornea.
We suggest you familiarize yourself with: Do-it-yourself aquarium lid with lighting
In the final stages of the disease, paralysis of the limbs and torso occurs. On average, the active phase of violent rabies can last from 3 to 11 days. The death of the animal occurs from paralysis of the respiratory and cardiac muscles.
The paralytic (silent) form of rabies does not last long; rabies in a cat in this form can be recognized by the following signs:
- refusal of food and water;
- the animal hides in dark places;
Paralysis of the lower jaw, paws, and torso develops already 2-3 days after the onset of symptoms. With the paralytic form of rabies, the cat does not behave aggressively and does not react to the owner in any way.
The atypical form of the pathology is rarely observed and is characterized by a long course (up to several months). The disease is accompanied by lethargy, drowsiness, and depression. The cat does not eat well, and gastrointestinal disturbances may occur (diarrhea, constipation, vomiting). Atypical rabies is accompanied by exhaustion, convulsive trembling, and muscle atrophy.
Diagnosis of rabies in cats If rabies is suspected, the cat should be isolated from people and other domestic animals and reported to the nearest state veterinary institution, whose specialists will tell you how to proceed. If she scratches and bites the owner and family members, you should immediately wash the wound with hot water and ordinary laundry soap and be sure to go to the hospital.
A test for rabies in cats is carried out after death, examining brain tissue for the presence of the virus. If this deadly disease is suspected, it is prohibited to treat the animal so as not to put the lives of veterinarians at risk.
The danger that infected animals pose to humans is obvious. The virus can be transmitted by a cat bite during an aggressive period or by contact with saliva on the mucous membrane or skin. The unusual nature and low prevalence of the disease do not always suggest rabies in a pet.
Difficulty breathing and wheezing of a sick animal make the owner believe that the pet simply choked on a bone. When trying to remove a foreign body or calm a cat, the animal owner or veterinarian is at enormous risk of becoming infected. As the disease develops, cats lose the ability to adequately perceive their surroundings and, in a fit of aggression, are capable of attacking not only the owner, but also any other person.
Initial symptoms of rabies in humans:
- weakness, lethargy;
- headache;
- dry mouth, constant desire to drink;
- elevated temperature;
- vomit;
- irritability, aggressiveness;
- hallucinations;
- depression;
- insomnia.
The incubation period in humans is 10-90 days, depending on the distance of the bite site from the head. Subsequently, the infected person begins to feel strong spasms of the muscles of the larynx, suffocation, and convulsions. In the final stages of the disease, the person becomes aggressive, easily excitable, there is profuse salivation, fear of light and water.
Before death, painful symptoms disappear, apathy, lethargy, paralysis and death from respiratory or cardiac arrest occur. The disease develops within a week and without treatment is fatal. When infected with the rabies virus, a person is prescribed a course of anti-rabies treatment - 7 vaccinations over 6 months.
It should be noted that there are no effective treatment methods for the appearance of clinical signs of the disease; assistance can only be provided immediately after infection. In 2005, for the first time, a patient in the late stages of the disease was cured without vaccination. The treatment used the method of putting a person into an artificial coma.
In this episode of the TV show “Live Healthy!” with Elena Malysheva you will learn: Rabies can appear in people...
The very first symptoms you need to pay attention to are: 1. The cat has lost her appetite2. The pet is vomiting3. Constipation4. Diarrhea5. Drooling profusely6. The cat is constantly in an overexcited state7. Aggression unusual for a pet
8. The cat rushes at the owner or shows aggression towards another animal9. They try to be alone10. Seek shelter in dark and shadowy places (photophobia)11. They react aggressively to attempts to get them out of hiding12. Coordination of movements is impaired13. The cat exhibits paresis (conditions similar to paralysis, only not so pronounced)14. The cat experiences paralysis
In these violent cases, the pet dies in a coma within two to four days. When diagnosing a disease, a veterinarian must rule out similarities with pseudorabies. Revealing the real reason.
If you have even the slightest suspicion that your pet has rabies, you must immediately isolate it without touching it. The best and easiest way is to place the cat in a separate room, free from people. After this, immediately call the city trauma center and report your suspicions.
Where is rabies found in the world?
Rabies occurs throughout the world, with the exception of Antarctica and some island nations. The vast majority of cases occur in areas of uncontrolled domestic dog rabies. For epidemiological purposes, rabies is divided into two types: urban and forest.
Urban rabies: Found primarily in developing countries in Asia and Africa.
Sylvan rabies: Most common in developed countries in the northern hemisphere.
Rabies is estimated to cause 55,000 human deaths per year worldwide, the vast majority of which occur in Africa and Asia. Several countries, most of which are islands, are rabies-free, including the British Isles, New Zealand, Japan, Taiwan, many Caribbean islands, Sweden, Norway and Spain. These countries remain rabies-free due to the strictness of their quarantine laws on imported animals. Australia was once thought to be rabies-free, but bat-borne rabies is now endemic here.
How long does a sick dog live?
A dog suffering from a violent form of rabies dies within 5–7 days, but can live up to 14 days. These days pass in terrible torment for the animal, accompanied by convulsive seizures and gradual failure of internal organs.
With an atypical form, the animal can live up to two months,
while remaining a source of infection. The recurrent form allows the animal to live for up to 6 months, but death is inevitable in any case.
Reference.
The shortest form is depressive - the animal dies within a week.
Symptoms of rabies in humans
After a typical human infection through a bite, the virus enters the peripheral nervous system. It then travels along the nerves to the central nervous system. At this stage, the virus cannot be detected. The period between infection and the appearance of the first flu-like symptoms is usually two to twelve weeks, but can last up to two years.
At the initial stage:
- malaise,
- headache,
- heat.
Once the virus reaches the brain, it quickly causes encephalitis. This second phase is called the "prodromal" phase. At this time, treatment is useless. Symptoms will now begin to appear. Rabies can also cause myelitis; inflammation of the spinal cord.
At an advanced stage:
- mild or partial paralysis,
- cerebral dysfunction, anxiety,
- insomnia,
- confusion,
- extreme excitement
- abnormal behavior
- paranoia,
- terror,
- hallucinations (transitioning to delirium),
- acute pain,
- violent movements,
- uncontrollable excitability,
- depression,
- excessive salivation
- inability to speak or swallow water (hence the name hydrophobia)
At the final stage:
- periods of mania,
- lethargy,
- coma.
Death (which usually occurs due to respiratory failure) almost always occurs two to ten days after the first symptoms appear. The few people known to survive the disease are left with severe brain damage.
What animals have rabies?
Humans and many mammals, most commonly wild and domestic canids (e.g. dogs, foxes, coyotes), mustelids (e.g. skunks, badgers, martens), viverids (e.g. mongooses, civets, geneticists), procyonids (e.g. raccoons), and insectivorous and hematopoietic bats.
Urban rabies: stray dogs.
Forest rabies: dogs, foxes, coyotes, wolves, jackals, skunks, raccoons, mongooses and other biting mammals such as bats.
Infectious dose: unknown.
Symptoms of rabies in animals
The first stage is a one to three day period characterized by behavioral changes and is known as the prodromal stage.
The second stage is the arousal stage, lasting from three to four days. It is this stage that is often known as rabid rabies due to the tendency of the affected animal to become hyper-responsive to external stimuli and bite anything nearby.
The third stage is the paralytic stage, caused by damage to motor neurons. Loss of coordination is observed due to paralysis of the hind limbs and drooling, and difficulty swallowing is caused by paralysis of the facial and pharyngeal muscles. As in humans, death is usually caused by respiratory failure.
First aid for suspected rabies
Monitoring for symptoms is inadequate because by the time symptoms become apparent, rabies is invariably fatal. There are no diagnostic methods during the incubation period. After the incubation period, detection methods include virus isolation, RT-PCR and direct immunofluorescence of clinical samples (a set of immunological methods for the qualitative and quantitative determination of surface and intracellular antigens in samples of cell suspensions).
First aid for rabies begins with disinfecting the wound, this can reduce the risk of rabies by up to 90%. Wash the wound with soap and water, then with 70% ethanol or iodine-containing solution. After wound care, the physician must decide whether to perform passive and/or active immunization.
Treatment of rabies
There is no established treatment for rabies once symptoms appear; almost all patients die from the disease or its complications within a few weeks of its onset. Supportive care includes intubation, sedation, mechanical ventilation, fluid and electrolyte administration, nutrition, and treatment of intercurrent illnesses and complications.
Almost every case of rabies resulted in death until Louis Pasteur and Emile Roux developed a vaccine in 1885. Their original vaccine was obtained from infected rabbits whose nerve tissue was weakened by allowing them to dry out for five to ten days. Vaccines based on similar nerve tissue are still used in some countries today because they are less expensive than modern cell culture vaccines. The human diploid cell rabies vaccine (HDCV) was initiated in 1967; however, a new and less expensive purified chick embryo cell vaccine and a purified Vero cell rabies vaccine are now available.
Treatment after exposure, known as post-exposure prophylaxis or “PEP,” is very effective in preventing disease when administered promptly, usually within ten days of exposure. As soon as possible, thoroughly wash the wound with soap and water for about five minutes to reduce the number of viral particles. If possible, a virucidal antiseptic such as povidone-iodine, tincture of iodine, aqueous iodine, or alcohol (ethanol) should be applied after washing. Exposed mucous membranes such as the eyes, nose or mouth should be rinsed well with water.
One dose of immunoglobulin and five doses of rabies vaccine are administered over twenty-eight days. If possible, half the dose of immunoglobulin is injected into the bite area. the rest is injected intramuscularly away from the bite. This is less painful than injecting immune globulin through the abdominal wall with a large needle, as was done in the past.
The first dose of rabies vaccine is given as soon as possible after exposure, with additional doses given on the third, seventh, fourteenth and twenty-eighth days after the first. Patients who have previously received pre-exposure vaccination do not receive immunoglobulin, only post-exposure vaccinations on days 0 and 3.
Due to widespread vaccination of domestic dogs and cats and the development of effective human vaccines and immunoglobulin treatments, the number of vaccinations reported has decreased.
In cases where post-exposure prophylaxis is given as a precaution (for example, a person wakes up to find a bat in the room they were sleeping in), it is now primarily administered to the gluteal region and deltoid (shoulder) muscles.
The number of injections given in the gluteal area on the first day is determined by weight, and three such injections are often required. Subsequent injections of immunoglobulin (to create longer-term immunity to rabies) are given in the arm. These shots are no more painful than regular shots (such as tetanus vaccines).
Although the virus is only treatable during the incubation period, it is important to note that it is not completely treatable. It is completely treatable as long as the virus is present in tissues made up of cells other than neurons, such as skin and muscle. However, once the infection spreads to a neuron, the virus becomes isolated from the immune system and eventually travels to the spinal cord and then to the brain. Treatment at this stage may not be effective, even though symptoms may appear weeks or even months later.
Therefore, it is highly recommended to carry out PEP as soon as possible. When started immediately or with very little delay, PEP is very effective against rabies. If there is a significant delay in prescribing PEP
About rabies prevention (video)
If signs of disease are detected in a cat, you must strictly adhere to the following rules:
- isolate the animal in a separate room or a special box for carrying animals;
- exclude the possibility of any contact with humans and other animals;
- contact a state or municipal veterinary clinic and follow the instructions received;
- If a cat attacks a person or saliva gets on the skin, wash the wound or place of contact with saliva with plenty of hot water and laundry soap, and go to the clinic.
There is no cure for rabies in cats. Animals are isolated and, if symptoms are pronounced, are euthanized. The corpses of sick cats are cremated. The symptoms of the disease are quite pronounced, so at the slightest suspicion it is necessary to involve veterinarians. If aggressive behavior occurs, do not try to calm the animal, pick it up or stroke it. In this state, cats are not guided by logic; their behavior is determined by their painful condition and is beyond their control.
All pets must be vaccinated against rabies. Some clinics refuse to serve unvaccinated animals. The cost of vaccination is 500-1000 rubles, depending on the region. Two weeks before vaccination, the animal must be given anti-helminth medication, get rid of fleas, and monitor its general condition and body temperature. Domestic or imported products are used as vaccines:
- Rabikan;
- Rabisin;
- Nobivac Rabies (valid for 3 years);
- Nobivac Forcat;
- Nobivac Tricat;
- Defensor-3;
- Purevax RCP;
- Purevax RCPCH;
- Quadricate;
- Leucoriphenin;
- Felovax.
We suggest you read: Symptoms and signs of rabies in animals
Vaccination is carried out when the kitten reaches the age of 3-4 months and is repeated annually. Vaccination is mandatory in the following cases:
- animal participation in exhibitions;
- export abroad;
- use for breeding;
- living in an area unfavorable for the spread of rabies.
Vaccination takes place without complications; quarantine after vaccination is not required. Information about the procedure performed is entered into the animal’s passport and confirmed by the seal and signature of the doctor. Immunity is developed within 2-3 weeks, so if the need for vaccination is caused by any event, the procedure must be carried out in advance.
How soon can you drink after rabies?
Alcohol abuse is known to impair the functioning of the immune system, increasing the risk of infectious diseases and complications. Considering that rabies is a deadly infection, and vaccination is often carried out for the purpose of emergency prevention (that is, it means that the rabies virus has entered the body), the last thing you need to do is interfere with the immune system in the fight against a potential threat. We strongly recommend that you refrain from drinking alcohol throughout the entire vaccination course and for at least 14 days after completion.
Useful tips
- The sooner after a bite a person seeks help, the more effective the vaccine is.
- If possible, it is necessary to track the animal that bit the victim. If the animal dies within 10 days, it means that it actually transmitted the rabies virus to the patient. If the animal remains alive, then most likely the vaccines will be canceled.
- In the first six months after the bite, you should avoid hypothermia or overheating so as not to reduce the protective function of the immune system.