The human body is a balanced mechanism controlled by the brain. Any pathological disorder destroys this harmony, and periventricular leukomalacia (PVL) is one of them. The disease manifests itself as a result of impaired nutrition of the brain during intrauterine development and occurs mainly during prematurity.
Leukomalacia is a fairly severe neurological condition. As it develops, foci of necrotic lesions worsen in the brain. If left untreated, the disease can lead to irreversible consequences, such as mental retardation and cerebral palsy.
Features of the pathology
Periventricular leukomalacia in premature infants is a lesion of the white matter localized near the lateral ventricles. It is characterized by necrotic damage to brain tissue due to insufficient oxygen supply and weakened blood flow. PVL occurs mainly in children whose body weight does not exceed 2 kg. Due to fetal hypoxia (lack of oxygen), a cyst gradually develops in the brain, but this process does not occur during intrauterine development. Such formations appear in the first 30 days from birth. Their diameter usually does not exceed 3 mm and the cavities are localized mainly in the parietal and frontal regions.
The focus of leukomalacia can be seen using a neurosonogram. Such an instrumental examination is mandatory for premature babies and is prescribed to all babies from this group.
The following stages are typical for PVL:
- First. In the first 7 days, an increase in echo density in the ventricular region is observed;
- Second. The echo density increases and small cyst-like formations form;
- Third. The echo density remains at a high level and at the same time the number of cystic formations becomes significantly larger;
- Fourth. A high level of echo density spreads to the white matter and cyst-like formations begin to appear in it.
Forecast
How long they live when diagnosed with cerebral leukoencephalopathy depends on the causes of development and the nature of the pathology. The life expectancy forecast is compiled individually by the attending physician, taking into account the age and physical condition of the patient. The prognosis of a disease of vascular origin is conditionally favorable. Timely correction of vascular disorders allows delaying large-scale damage to the white matter.
When diagnosed with HIV, leukoencephalopathy caused by the virus is the second leading cause of death, second only to non-Hodgkin's lymphoma. Numerous autopsy results showed the absence of a direct connection between mortality and the morphological features of the structure of lesions (size, localization, degree of tissue atrophy, hydrocephalus) in the viral form of the disease.
Description history
The first microscopic description of a PVL focus belongs to JM Parrot (1873). R. Virchow only macroscopically described yellowish foci in the periventricular zones of the lateral ventricles of the brain in deceased newborns born to mothers with syphilis and smallpox, classifying them as congenital encephalitis. There are no sufficient grounds to classify these lesions as PVL. The lesion has been described under various names (“encephalodystrophy”, “ischemic necrosis”, “periventricular infarction”, “coagulative necrosis”, “leukomalacia”, “cerebral softening”, “periventricular white matter infarction”, “white matter necrosis”, “diffuse symmetrical periventricular leukoencephalopathy"), more often by German scientists, but the term “periventricular leukomalacia”, introduced in 1962 by BA Banker and JC Larroche, became widespread worldwide. The term is not clear enough, since with PVL it is not softening that occurs, but foci of coagulation necrosis that are denser than the surrounding areas of the brain. The first article in the USSR and Russia dedicated to PVL was written by V.V. Vlasyuk et al. (1981), who proposed using the term “periventricular leukomalacia.”
The most complete studies of PVL in the world on the largest sectional material were carried out by V.V. Vlasyuk (1981) (frequency, etiopathogenesis, topography, degree of damage to various parts of the brain, stages of development of lesions, neurohistology, role of microglia, electron microscopy, etc.), who for the first time revealed a high frequency of damage to the optic radiance and proved that PVL is a persistent process, that old foci of necrosis can be joined by new ones, that PVL foci can be at different stages of development.
What is periventricular leukomalacia

Leukomalacia of the brain in newborns is a severe lesion and abnormality in the structure of the white matter of the brain, located on the sides of the ventricles filled with cerebrospinal fluid.
As a rule, leukomalacia occurs in premature infants due to underdevelopment of protective and restorative functions. In a full-term newborn, even with temporary ischemia and hypoxia of the brain, the work of the heart muscle and blood supply to the suffering brain tissues increase. According to statistical data, on sectional material without sampling, leukomalacia is diagnosed in 12.6% of cases, more often in boys.
- Ischemia – local deterioration of blood supply
- Hypoxia is a lack of oxygen in the tissues of the body.
At the site of the lesion, coagulation necrosis is formed - compaction of the tissue of the head sections. Subsequently, after 28–35 days, a periventricular cyst transforms and appears. A benign cystic cavity in children is filled with serous transparent contents and is easily determined by EEG.
Development of leukomalacia
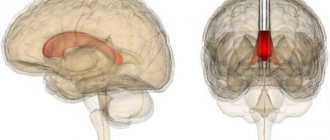
Periventricular leukomalacia in premature infants affects the so-called optic radiation and visual tuberosities, located near the initial part of the dorsal horns and the central zone, respectively.
In the pathogenesis of leukomalacia of the brain, there are three main stages:

Leukomalacia in newborns is necessarily accompanied by a diffuse component. Without it, the diagnosis can be considered doubtful, then an additional revision of diagnostic indicators takes place to verify the nosology.
The diffuse component includes a number of brain structures:
- Apoptosis of pro-oligodendrocytes;
- Division of microgliocytes, astrocytes;
- Hemorrhage;
- Swelling;
- Destruction of the capillary wall.
The diffuse component in the form of tissue necrosis distinguishes periventricular leukomalacia from similar pathologies: diffuse and subcortical leukomalacia, telencephalic gliosis, hemorrhagic infarction, pseudocyst.
Provoking factors
A periventricular cyst occurs against the background of a hypoxic and ischemic component; with the appearance of encephalopathy in a child, the death of nerve pathways and disruption of the transmission of nerve impulses to organs, tissues, and muscles are formed.
The main reasons for development include:
- Brain hypoxia due to fetoplacental insufficiency, unfavorable environmental conditions, work in hazardous industries and bad habits of women.
- Cyst against the background of ischemia of certain areas of the brain.
- Severe gestosis during pregnancy with a persistent increase in blood pressure, nausea, vomiting, swelling of the extremities, and loss of consciousness.
- Chronic infectious diseases, pathogens of which are able to penetrate amniotic fluid.
- Weak labor, premature rupture of water and the so-called dry period, premature birth.
- Fetal growth retardation and low birth weight newborns (1500–2000 grams).
- Violation due to severe asphyxia with delayed passage through the birth canal, the need for mechanical ventilation and resuscitation measures.
Main reasons for development
Lack of oxygen has a detrimental effect on the brain of premature babies. This is due to the insufficient development of compensatory mechanisms that cannot provide the organ cells with oxygen in a timely manner.
If a child is born on time, then his nervous system and blood flow are better formed, so with oxygen starvation, blood circulation will increase and damage will not occur.
The situation may be aggravated by the lack of a strong connection between the arteries of the brain in premature babies.
As a result of hypoxia, free radicals are formed, acidic metabolic products that damage neurons and disrupt blood circulation in small vessels, and also provoke congestion in arteries and veins. This is accompanied by tissue necrosis, the development of metabolic disorders and thrombosis.
Periventricular leukomalacia in premature infants is more common if the child was on mechanical ventilation. The device supplies oxygen, but when there is a large amount of it, small arteries spasm, which causes ischemic disorders to develop.
Interestingly, the pathology occurs more often in children born in the winter-spring period. Scientists suggest that this is due to insufficient amounts of vitamins and unfavorable weather conditions, which negatively affect a woman’s body in the last weeks of pregnancy.
The following factors increase the risk of developing leukomalacia:
- severe pregnancy;
- chronic infectious processes in the mother's body;
- impaired blood flow in the placenta or fetus, which leads to hypoxia;
- premature birth, weak labor;
- pathologies after birth that require artificial ventilation.
Causes and risk factors
The possibility of the occurrence of this pathology increases in premature infants: the lower the birth weight, the more likely the development of the pathological process. Other risk factors include the gender of the child: boys are diagnosed with this disease more often than girls.
In addition to brain hypoxia, the appearance of PVL foci can be influenced by an excess amount of carbon dioxide (hypercapnia) in the blood, as well as oxygen poisoning (hyperoxia), which sometimes occurs during artificial ventilation during resuscitation. A dangerous situation is the sudden change from hypoxia to hyperoxia, which can happen without monitoring the content and ratio of oxygen and carbon dioxide in the blood during mechanical ventilation. In addition, a developed infection can aggravate the situation.
It was also noted that the risk of developing PVL increases depending on the time of year: most often it is diagnosed in those children whose last two to three months occur in winter or early spring. Experts attribute this to the influence of meteorological changes that affect pregnancy. Hypovitaminosis may also play a role.
Preventive measures
To reduce the risk of developing leukomalacia you need to:
- extend the pregnancy period, since the shorter the period, the greater the likelihood of developing this disease;
- If possible, it is necessary to prevent premature birth in a woman in labor.
But not only the doctor can influence the development of pregnancy, but the pregnant woman herself can change the situation in a positive direction. What do we have to do:
- first of all, a pregnant woman is a future mother and she should lead a healthy lifestyle;
- Pregnancy cannot occur spontaneously; it must be carefully planned;
- nutrition should be harmonious and balanced;
- every pregnant woman must register and strictly follow doctors’ recommendations;
During pregnancy, you should try not to get sick from various diseases, especially viral and infectious ones. Due to the illness, the unborn baby may suffer.
Consequences of the disease
Before the disease begins to progress, the child is no different from a healthy one. However, after this, cerebral palsy develops and all the symptoms corresponding to this disease:

- Impaired consciousness.
- Swallowing and breathing problems.
- Increased blood pressure.
- Deterioration in mental development and lag behind peers.
- Pathological work of the central nervous system.
Depending on the area of white matter and meninges affected, the child may experience some or all of the effects listed above.
Modern medicine can cure a person from almost any disease. However, periventricular leukomalacia is not always treatable. In the case of a severe form of the disease, the child becomes disabled for the rest of his life, and the parents will have to maintain a stable state of health.
It is worth remembering that a prematurely born child is not disabled in 100% of cases. Many factors must come together for a newborn to receive such a diagnosis. The main thing is to undergo courses of drug treatment and physiotherapy in a timely manner.
Symptoms
Symptoms of leukomalacia brain can be very different.
There are 3 stages of periventricular leukomalacia of the brain:
- Mild - here the symptoms of damage to the nervous tissue last less than a week from the moment of birth;
- Average - no more than ten days, there are convulsions, hypoxia inside the skull, autonomic dysfunction;
- Severe – severe brain damage, very often the baby falls into a coma.
Cerebral leukomalacia has signs and symptoms such as:
- Excessive excitability on a neuro-reflex background or its suppression;
- Convulsions;
- Paralysis and paresis;
- Brain stem symptoms;
- Deterioration of vision (squint);
- Muscle hypotonicity;
- Late development of psychomotor skills, impaired mental performance, hyperactivity.
The connecting nerve pathways are located around the ventricles, which provide the function of movement, therefore the main factor in cerebral leukomalacia is cerebral palsy in children. But how much it has developed depends on the complication of necrosis.
Impaired motor skills are a characteristic symptom of leukomalacia. Seizures appear by the 6th month. If the size of the necrosis is large, then there are more cysts, and insufficient brain activity is more pronounced.
Symptoms of leukomalacia depend on the location of the source of damage (convulsions, visual and movement disturbances, untimely development of the psyche).
Severe damage to the parietal and frontal areas is accompanied by paralysis and abnormal development of the psyche. If only the connecting pathways that are responsible for the provision of limbs are involved, then the child’s intelligence and development may not be entirely affected.
Often after perinatal hypoxia, there is a lack of attention and excessive activity of the child. This option is favorable and can be corrected with special treatment methods.
As a result of these numerous symptoms, parents may not know what to do, what to expect when a child is born in the early stages and hypoxia. If the disorder is severe, then the baby will not learn to sit, roll over and, of course, walk in a timely manner. The speech apparatus is inhibited, the child does not know how to play, is indifferent to toys, and does not show interest in the things around him.
Hypertonicity plays an important role, because of which the child becomes capricious, sleeps poorly, and is restless. It is very difficult for mothers to breastfeed when the sucking reflex and excessive neuromuscular excitability are impaired.
The child slowly gains weight, grows beyond his age, and does not have the skills and abilities that a growing body needs to master.
By the first year of life, the baby develops cerebral palsy and inhibited psychomotor skills. Later, when the recovery period ends, signs such as untimely psycho-speech development, emotional instability, sleep disturbance, and attention deficit appear.
Gradually, the symptoms worsen and the disease manifests itself as follows:
- High or low neuro-reflex excitability, manifested due to various external stimuli (light, sound, palpation, movements, etc.);
- Convulsions;
- Decreased tone of certain muscle groups;
- Strabismus.
Gradually, the child reacts less and less to surrounding events, and over time may completely cease to understand their meaning. You can stop the development of pathology by promptly detecting its symptoms and starting treatment.
Leukomalacia in newborns: causes, consequences, symptoms, treatment
© A. Olesya Valerievna, candidate of medical sciences, practicing physician, teacher at a medical university, especially for SosudInfo.ru (about the authors)
Leukomalacia is classified as ischemic-hypoxic brain damage diagnosed in newborns. It represents a serious problem in neonatology and neurology, since the long-term consequences of the pathology are very difficult to treat, leading to disability.
With leukomalacia, foci of necrosis are found in the brain that arise after severe hypoxia and impaired blood flow . They are located mainly around the lateral ventricles, so periventricular lesions are the most common variant of the pathology, which will be discussed below.
periventricular (periventricular) leukomalacia
Periventricular leukomalacia (PL) occurs in approximately 12% of cases among newborns, usually in premature infants, and its frequency depends on the weight with which the baby was born. The largest number of babies suffer from leukomalacia if the birth weight was 1500-2500 g. In this case, the pathology is found in almost every third child.
About 60% of newborns who survive up to a week have signs of LP.
Caesarean section significantly increases its risk (up to 35%) compared to natural childbirth, but this applies to cases with pre-existing prenatal pathology.
If the baby grew and developed normally in utero, and the caesarean section is carried out on time, then the operation itself does not increase the risk of such brain damage.
Causes of leukomalacia
The brain of premature newborns is very sensitive to a lack of oxygen, since compensatory mechanisms have not yet developed, and the microvasculature cannot provide blood delivery in a timely manner. In full-term babies with a more or less mature nervous system and blood flow, hypoxia stimulates blood circulation, so the damage will not be as pronounced.
Option for the development of intrauterine hypoxia (oxygen starvation) due to insufficiency of placental blood flow
The problem is aggravated by the fact that premature babies do not have a good connecting network between the arteries of the brain, and the subcortical region around the ventricles, at a distance of up to 1 cm from their walls, is especially affected, more so in the parietal zones. This explains the periventricular (near the ventricles) location of the foci of necrosis.
Hypoxia causes the formation of free radicals, acidic metabolic products, which not only have a direct damaging effect on neurons, but also contribute to disruption of microcirculation in the form of thrombosis, stagnation of blood in small arteries and veins. Thus, hypoxia, which itself causes necrosis, provokes metabolic disorders and thrombosis, which further aggravate the situation.
It has been noted that periventricular encephalopathy develops more often in children who were on artificial pulmonary ventilation (ALV). It would seem that the device provides breathing and oxygen delivery, so the brain should not suffer. However, excess oxygen supplied through the device provokes spasm of the arterioles, which leads to ischemia.
The frequency of LP among newborns depends on the time of year. Typically, a greater number of such patients occur in the winter-spring period. A possible reason is considered to be a lack of vitamins and the influence of unfavorable weather conditions on the body of a pregnant woman in late gestation.
Risk factors for leukomalacia are:
- Severe gestosis;
- Chronic infections in pregnant women;
- Intrauterine hypoxia due to disturbances in the placenta or blood flow to the fetus;
- Anomalies of childbirth - premature birth, premature rupture of water, weakness of labor forces;
- Pathology of newborns – respiratory distress syndrome, pneumonia requiring mechanical ventilation.
What happens in the brain during leukomalacia?
With leukomalacia of the brain, foci of necrosis appear in the subcortical structures, usually coagulative, nerve cells die, and the defects are replaced by multiplying microglial cells, similar to how scars form in other organs. Neurons cannot reproduce, and the brain has nothing to fill the dead fields with, so the result is cysts (cavities) - cystic leukomalacia.
More than half of cases of LP are accompanied by secondary hemorrhages in the area of ischemia and necrosis; hemorrhages into the ventricles of the brain are possible. It is important that the cerebral cortex in such children is affected extremely rarely due to good blood supply.
Leukomalacia begins in the first days and lasts about a week from the moment of birth. Its later occurrence is also possible, usually associated with infection or breathing problems in a newborn child. In these cases, against the background of existing necrosis, new ones may appear, and the child’s condition will progressively worsen.
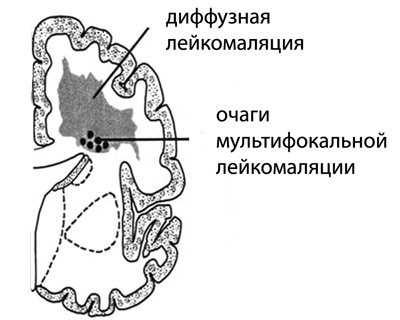
Foci of multifocal leukomalacia with a diameter of 2-3 mm are found in the parietal and frontal lobes, symmetrically, around the walls of the lateral ventricles. Less commonly, the temporal and occipital lobes of the brain are affected.
The outcome of necrosis is the formation of many cysts of different sizes, scattered throughout the subcortical layer of the brain (cystic degeneration), the number of which increases over time.
In severe PL they occupy the entire periventricular part of the hemispheres.
It takes about two weeks for necrosis and the formation of cysts, and over the next few months, the cavities in the baby’s brain collapse, the dead areas are replaced with scars from neuroglia, and irreversible atrophy of the nervous tissue occurs.
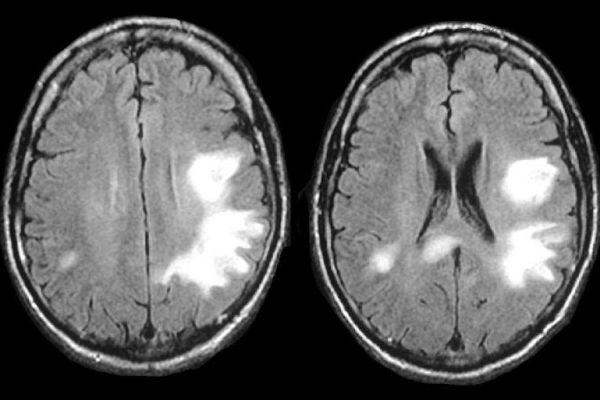
leukomalacia on MRI images
Manifestations of leukomalacia
Signs of leukomalacia are varied and often nonspecific, but severe hypoxic damage to brain tissue cannot be asymptomatic. There are several degrees of PL:
- Mild degree - signs of damage to the nervous system persist up to a week from the moment of birth;
- Moderate severity – from 7 to 10 days, convulsions, intracranial hypertension, autonomic disorders are possible;
- Severe PL – deep damage with brain depression, often coma.
Symptoms of cerebral leukomalacia include:
- Excessive neuro-reflex excitability or, conversely, its inhibition;
- Convulsive syndrome;
- Muscle hypotonia;
- Stem symptoms;
- Paresis and paralysis;
- Visual disturbances in the form of strabismus;
- Delayed psychomotor development, intellectual impairment, hyperactivity, attention deficit.
Experts especially note that neurological symptoms in the acute period and up to 3-5 months of life may not be expressed. In approximately 90% of children, after the acute period, imaginary well-being occurs, lasting up to 5 and even 8-9 months of life. And only after such a long time do signs of a deficit of nervous activity appear against the background of atrophy of brain tissue.
The nerve pathways responsible for the motor function of the limbs are concentrated around the ventricles of the brain, so the main symptom of cerebral leukomalacia in children is cerebral palsy, but its severity depends on the severity of necrosis.
Due to the involvement of the brain stem and cranial nerves, more than half of children suffer from strabismus, more often convergent, swallowing disorders and respiratory disorders are possible. By the age of six months, convulsive syndrome appears.
The larger the size of the necrosis fields and, accordingly, the cysts, the more pronounced the brain failure. The nature of the symptoms is determined by the localization of the lesions (motor, visual disturbances, convulsions, mental retardation).
Severe damage to the parietal and frontal lobes leads to cerebral palsy with simultaneous impairment of mental development. If only the pathways responsible for the innervation of the limbs are involved, then paralysis may not be accompanied by impairments in the child’s intelligence and development.
Often, in children who have suffered perinatal hypoxia, symptoms include attention deficit and hyperactivity with intact motor development. This is a relatively favorable variant of the pathology, which can be corrected with special therapeutic measures.
Due to such unpredictability and variety of symptoms, it can be difficult for a mother to figure out what to expect when the baby is born prematurely and under hypoxic conditions.
If the damage is moderate or severe, then the child will not develop according to his age - he will not learn to roll over, sit, and, especially, walk in time.
Speech development will slow down, the baby will not be able to walk, will not follow toys and will not show such curiosity as is typical for his age.
Particular attention is drawn to hypertension, which can be painful, so the child will be restless, whiny, and sleep will be disturbed. Breastfeeding can be problematic due to a poor sucking reflex, excessive neuromuscular excitability, or atonia.
Poor weight gain, slow growth that is not appropriate for age, and a lack of skills that a growing child needs to master are the main symptoms that parents of a baby with moderate or mild damage to the subcortical structures have to deal with.
By about a year, neurological deficits become noticeable, cerebral palsy develops, and psychomotor development is delayed.
After a year, when the recovery period comes to an end, the clinical picture is dominated by such consequences as delayed psycho-speech development, emotional lability, problems with sleep and attention, which can occur along with more severe motor disorders (cerebral palsy).
PL in adults can cause cerebral palsy, hypertonicity, intellectual impairment, and severe mental retardation . With a favorable course of the pathology, adults are not much different from others.
Frequency
The frequency of PVL, according to different authors, ranges from 4.8% to 88%, but often among a certain group of children or according to neurosonographic studies, which is not entirely objective. On non-selected sectional material, the frequency of PVL is 12.6%, more often in boys, and depending on birth weight: 1001-1500 g - 13.3%, 1501-2000 g - 21.5%, 2001-2500 g - 31.6%, 2501-3000 g - 14.8%, more than 3000 g - 3.5%. It occurs most often in premature infants of the 1st and 2nd degrees. In those who died on the first day after birth, PVL occurs with a frequency of 1.8%, and in those who died on the 6th-8th days - 59.2%. In the group of those born with cephalic presentation, the frequency of PVL is 19.6%, with breech presentation - 17.4%, and with caesarean section - 35.6%.
Development of leukomalacia

The disease comes in different types, but the most common is periventricular leukomalacia, since the foci of damage to the white matter of the brain are located in its periventricular region. The size of these lesions is about 2 millimeters. They are located in the pubic and parietal lobes of the brain on both sides and symmetrically to the walls of the lateral ventricles.
Basically, the disease develops in the first couple of hours after the birth of the child, but you should be under observation for 10 days. Lack of oxygen supply to the brain leads to blood stagnation, blood clots and death of diseased areas. In addition, hemorrhage may occur in dead areas of the brain or its ventricles.
Leukomalacia can develop, and new lesions will appear and grow over time. There are cases of no symptoms of the disease in the newborn period, as well as death caused by periventricular edema.
With the onset of one month of age, the newborn is sent for neurosonography. This ultrasound reveals the dynamics of the disease and the degree of pathological changes.
Why is leukomalacia dangerous for the brain?
During this pathological process in the brain, the following occurs:
- Tissue death.
- Death of nerve cells.
- Replacement of defective cells with microglial cells, that is, scar formation.
- The loss of the ability of neurons to reproduce, as a result of which the dead areas are not filled with anything, and cysts develop in them.
The development of leukomalacia occurs in the first days after birth and lasts for a week. The problem may appear later, but in this case it occurs due to infection or breathing problems. In such a situation, new necrosis joins the existing necrosis, and the child’s condition rapidly deteriorates.
Tissue death and cyst formation develop over several weeks. After this, the cavities in the brain disappear, the dead areas are replaced by scar tissue, and irreversible atrophic changes occur in the nervous tissue.
What happens in the brain during leukomalacia?

With leukomalacia of the brain, foci of necrosis appear in the subcortical structures, usually coagulative, nerve cells die, and the defects are replaced by multiplying microglial cells, similar to how scars form in other organs. Neurons cannot reproduce, and the brain has nothing to fill the dead fields with, so the result is cysts (cavities) - cystic leukomalacia.
More than half of cases of LP are accompanied by secondary hemorrhages in the area of ischemia and necrosis; hemorrhages into the ventricles of the brain are possible. It is important that the cerebral cortex in such children is affected extremely rarely due to good blood supply.
Leukomalacia begins in the first days and lasts about a week from the moment of birth. Its later occurrence is also possible, usually associated with infection or breathing problems in a newborn child. In these cases, against the background of existing necrosis, new ones may appear, and the child’s condition will progressively worsen.
Foci of multifocal leukomalacia with a diameter of 2-3 mm are found in the parietal and frontal lobes, symmetrically, around the walls of the lateral ventricles. Less commonly, the temporal and occipital lobes of the brain are affected. The outcome of necrosis is the formation of many cysts of different sizes, scattered throughout the subcortical layer of the brain (cystic degeneration), the number of which increases over time. In severe PL they occupy the entire periventricular part of the hemispheres.
It takes about two weeks for necrosis and the formation of cysts, and over the next few months, the cavities in the baby’s brain collapse, the dead areas are replaced with scars from neuroglia, and irreversible atrophy of the nervous tissue occurs.
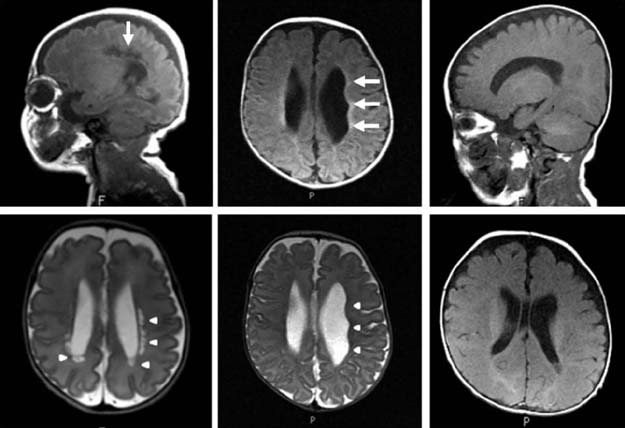
leukomalacia on MRI images
Morphology
According to the morphological essence of PVL
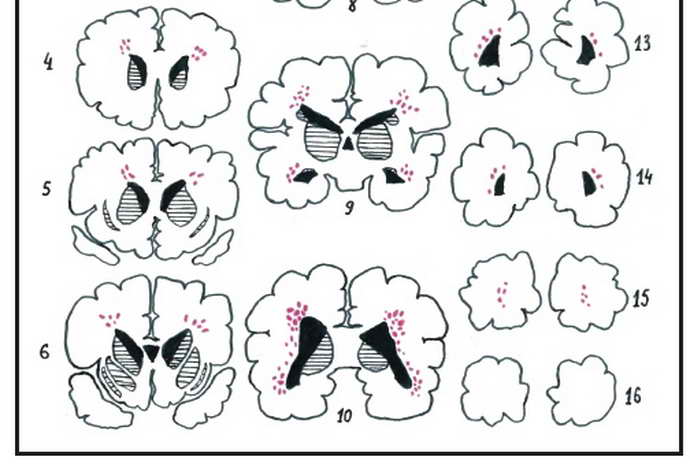
- These are small-focal, mainly coagulative periventricular infarctions of the white matter of the brain, often bilateral and relatively symmetrical. In PVL, foci of necrosis are located in the periventricular zone, but in the presence of many foci (severe lesions), some of them can spread to the central parts of the white matter of the brain. With the highest frequency, PVL foci occur in the periventricular white matter of the initial sections of the posterior horns of the lateral ventricles of the brain (the optic radiation is affected) and the central sections of the ventricles at the level of the visual thalamus (the corticospinal tract is affected). During the process of morphogenesis, lesions go through three stages: 1) development of necrosis, 2) resorption and 3) formation of a glial scar or cyst. Cysts occur with large and merging foci of PVL, with mixed necrosis (colliquation in the center and a coagulation rim along the periphery). Around the lesions, an area of other lesions of the white matter of the brain is usually determined - death of pro-oligodendrocytes, proliferation of microgliocytes and mast astrocytes, edema, hemorrhages, death of capillaries, etc. (the so-called “diffuse component” of PVL). However, diffuse lesions without necrosis are not PVL. If 15 frontal sections of the brain are made, then the detection of PVL foci in 1-4 sections indicates a mild degree of PVL, in 5-8 sections - a moderate degree of PVL, and in 9-13 sections - a severe degree of PVL (2).
Classification of the disease
There are different forms of pathology depending on the causes of occurrence. The vascular form of leukoencephalopathy, known as Binswanger's disease, is a brain disease that is progressive in nature and develops against the background of hypertension, which indicates a leading role in the pathogenesis of atherosclerosis and other vascular pathologies.
The clinical picture resembles manifestations of subcortical (subcortical) encephalopathy of arteriosclerotic etiology. The pathogenesis is associated with damage to the white matter against the background of atherosclerosis of small arteries and arterioles, as a result of which the vascular walls thicken and the lumen narrows, hyalinosis develops - protein degeneration with the replacement of normal tissue with a denser, low-elastic structure.
Typical complications: TIA (transient cerebrovascular accident), stroke. A third of all clinical cases of vascular dementia are caused by multifocal leukoencephalopathy. In 80% of cases, the age of patients is 50-70 years. Focal white matter lesions of infectious origin occur due to reactivation of the JC virus.
Periventricular leukoencephalopathy, known as periventricular leukomalacia, is characterized by white matter lesions occurring more frequently near the ventricular system. With large-scale lesions, the lesions spread to the central parts of the white matter.
The demyelinating process of an aggressive, long-term course leads to the formation of necrotic cavities in the brain structures. Leukoencephalopathy (leukomalacia) of the brain, found in children, is often the cause of the development of cerebral palsy (CP) in childhood.
How does pathology manifest itself?
Leukomalacia cerebri can have different symptoms. Damage to brain tissue cannot occur unnoticed. There are such degrees of development of the disease:
- Easy. At the same time, signs of brain damage are noticeable throughout the week.
- Average. Over the course of ten days, the child experiences convulsions, disturbances in autonomic functions, and increased intracranial pressure.
- Heavy. The deep layers of brain tissue are damaged, and children often fall into a coma.
Among the main manifestations of the disease are:
- Suppression or significant increase in neuro-reflex excitability.
- Cramps.
- Decreased muscle tone.
- Symptoms of brain stem damage.
- Paralysis.
- Visual impairment, which manifests itself as strabismus.
- Increased activity, impairment of intelligence and psychomotor development.
Neurological symptoms may not appear in the acute period. In most children, after the end of the exacerbation period for 5-9 months, their condition improves. This period is called imaginary well-being. After this, symptoms of nervous tissue atrophy appear.
The location of the nerve pathways around the ventricles leads to impaired motor function. Therefore, if a child has leukomalacia, its first manifestation will be cerebral palsy. Its severity depends on the degree of brain damage.
Due to damage to the brain stem and cranial nerves, strabismus and impaired swallowing and breathing develop. At the age of 6 months, seizures appear.
With severe damage to the parietal and frontal lobes of the brain, cerebral palsy with mental retardation develops. If the pathways are affected, paralysis occurs without a decrease in intelligence and developmental disorders.
Children who suffered oxygen deprivation during perinatal age suffer from attention deficit and hyperactivity. This variant of the course of the disease can be considered favorable, since the child’s condition can be normalized with the help of special medications.
With moderate or severe damage, speech development is inhibited, the baby untimely begins to walk, roll over and perform other actions typical of children of his age.
More attention should be paid to the development of hypertonicity, which causes pain to the child. Because of this, the baby sleeps poorly, often cries and is capricious.
The sucking reflex is impaired, so breastfeeding may remain in question.
The presence of a neurological deficit is most pronounced at one year of age and is expressed by cerebral palsy and delayed psychomotor development.
At the end of the recovery period, children experience:
- slowdown in psychological and speech development;
- mood instability;
- sleep and attention disorders;
- in severe cases, cerebral palsy develops.
In adults, the disease may progress more favorably and does not distinguish them from other people.
Prognosis and severity of PVL
If a woman fails to carry her baby to term, the children are born premature. Parents should prepare in advance to properly care for their newborn.
The prognosis will be relatively favorable for mild leukomalacia of the brain. In the periventricular clinic, attention deficit prevails, as well as hyperactivity - chaotic movements of the limbs. While motor development - the timeliness of crawling, walking, and turning over - is preserved.

Special corrective measures can achieve compensation for the disorder and improve physical and intellectual development.
With moderate and severe periventricular leukomalacia, the baby will not meet average age standards - parents should be prepared for this. He will later begin to roll over, sit down, and walk.
Speech development is also hampered - syllables will appear later, and sentences will be practically inaccessible. Other manifestations of periventricular pathology:

- lack of natural childhood curiosity;
- soreness and tension in the muscles of the limbs;
- restlessness, excessive tearfulness;
- sleep disturbance – intermittency, frequent confusion between day and night;
- breastfeeding is difficult - the sucking and swallowing reflex is poorly expressed;
- deviations in the dative system – the need to use an artificial respiration apparatus.
Diagnostics
A neurologist will tell you how terrible this diagnosis of leukoaraiosis is. The main methods of instrumental research include:
- Blood analysis.
- Angiography. Study of the condition of arteries, veins, vessels of the circulatory system.
- MRI, CT examination. Visualization of all departments, parts, elements of the brain.
In case of leukoaraiosis of the brain, MRI always shows the presence of vascular pathologies, which confirms the close connection of the disease with disruption of the blood flow system, which also determines treatment tactics.
Newborn brain
Prolonged oxygen deprivation can lead to the death of brain neurons. This is how necrosis develops in newborns. In the place where neurons were previously, cystic connections of different sizes begin to form. After two weeks of development of the disease, the nerve tissues of the brain atrophy.
Degree of brain damage

The degree of development of PVL depending on the degree of brain damage:
Mild degree. The disease develops within 7 days and is treatable. With proper care and a set of measures to stabilize the newborn’s condition, the difference in development between a sick and healthy child can be minimized.
Average degree. Pathological irreversible changes take up to 10 days. New disorders begin to be added to the main diagnosis: increased intracranial pressure, limb spasms, disorders of the autonomic nervous system.
Course of therapy
To date, a cure for PVL has not been invented. When drawing up a treatment regimen, the doctor focuses mainly on the results of the examination and the manifestations of the disease. The course of treatment for leukomalacia is mainly aimed at relieving the symptoms of the pathology.
The treatment is based on medications from the nootropic group. They improve metabolic processes and blood circulation in the brain. Stugeron or Piracetam is usually prescribed. It is equally important to correct motor and psychomotor impairments, since PVL is the main cause of cerebral palsy.
In this case, the chances of developing pathology will decrease.
The danger of periventricular leukomalacia and methods of its treatment

During labor, the unborn baby faces many dangerous moments. One of them is periventricular leukomalacia - a pathological focus in the brain of a newborn, caused by a lack of oxygen supply to its cells.
The predominant location of the periventricular lesion zone is along the outer-superior sections of the lateral ventricles of the organ. In the future, they can transform into cysts or cavities, leading to severe disorders of the baby’s central nervous system. Therefore, the prevention of this pathology is given great attention by doctors all over the world.
Prevention
To reduce the chance of developing PVL, it is advisable to avoid preterm birth. To do this, a pregnant girl must follow these rules:
- To refuse from bad habits;
- Get enough sleep;
- Avoid mental and physical overload;
- Eat properly;
- Do special therapeutic exercises;
- Be observed by a doctor throughout pregnancy;
- Try to avoid diseases, especially infectious ones;
- Strengthen the immune system, for example, with the help of vitamin complexes.
Preventive actions
To prevent pathology, patients with multiple sclerosis who are treated with Natalizumab are prescribed a preventive examination for the presence of the JC virus. Preventive measures include general recommendations to strengthen the immune system:
- Hardening procedures.
- Rejection of bad habits.
- Organization of healthy, nutritious meals.
- Active lifestyle, dosed physical activity.
Prevention of birth injuries during the perinatal period and injuries to the head in adulthood, systematic monitoring and correction of blood pressure values will help avoid complications and rapid progression of the disease.
Leukoencephalopathy is a progressive process of destruction of white matter. Early diagnosis and correct treatment of pathology of vascular origin contributes to a significant improvement in the patient’s condition.
Treatment methods
With leukomalacia, irreversible damage to brain tissue develops. It is not possible to completely restore necrotic lesions. But to eliminate the negative manifestations of the pathological process, symptomatic therapy is prescribed. The child’s well-being is improved with the help of special medications. Among them:
- Nootropic drugs. They are necessary to improve blood flow to brain tissue and improve metabolic processes. Piracetam and Nicergoline have these properties.
- Antihypertensive drugs. They are prescribed to reduce intracranial pressure and eliminate cerebral hydrocele.
- Anticonvulsants. Relieves cramps.
- Beta blockers. With their help, they normalize blood pressure and eliminate tachycardia.
- Hypotonic medications. Indicated if muscle tone is increased.
- With the help of Valerian, Melissa and other sedatives, the child’s sleep is normalized.
All physiological indicators of the child must be monitored.
In addition to drug treatment, to improve the child’s condition, they use therapeutic massages, physiotherapeutic procedures, classes with special teachers, during which attention and memory are normalized, and speech development is improved.
If it is not possible to normalize intracranial pressure with the help of drugs, then surgical intervention is necessary, during which shunts are installed to reduce the amount of cerebrospinal fluid and reduce the pressure inside the skull.
What the prognosis will be for such a pathological process depends on the volume of damaged nerve tissue and the degree of damage. If the disturbances in periventricular leukomalacia are minor, then the patient’s condition and organ functions can be corrected with special medications.
In severe cases of the disease, medications cannot stop the manifestations of leukomalacia. In this case, cerebral palsy, mental retardation, epilepsy and other complications develop.
To avoid the development of the disease, specialists can try to bring the pregnancy to a point where childbirth will not be dangerous for the baby.
Treatment options
Treatment of pathology of vascular origin involves eliminating the causes that provoked the development of the disease. More often, medications and other therapies are prescribed to stabilize high or low blood pressure. Drugs indicated:
- Improving blood microcirculation in brain structures.
- Stimulating metabolic processes in brain cells.
- Eliminating neurological symptoms.
In parallel, therapy is carried out for atherosclerosis and concomitant somatic diseases. There is no specific treatment for the viral form. Effective measures are considered:
- Stop taking immunosuppressants (corticosteroids, cytostatics). Or reducing their dosage.
- Discontinuation of Natalizumab, a drug based on monoclonal antibodies, if reactivation of the virus occurred as a result of its use. In parallel, it is recommended to carry out plasmapheresis up to 5 sessions daily to remove the drug.
- Prescription of Meflocin (an antimalarial drug). Some studies show the effectiveness of a drug that slows down the replication (multiplication) of the JC virus.
The antidepressant Mirtazapine inhibits the reuptake of serotonin and prevents the spread of the JC virus. The mechanism of action is based on blocking 5-HT2 receptors, which are the target of the polyomavirus.
Complications
Serious complications of PVL in newborns may manifest themselves at a later age. Such negative consequences include:
- seizures;
- hyperactivity syndrome;
- memory loss;
- fast fatiguability.
The most dangerous complications of this disease in newborns and premature babies are epilepsy and cerebral palsy. The prognosis of the course of the disease depends on the degree of damage to the cerebral cortex and the effectiveness of timely rehabilitation measures.
Periventricular leukomalacia (PVL) in newborns
1. Causes and risk factors 2. Pathogenesis 3. Clinical picture 4. Therapeutic measures
Complicated childbirth can cause injuries in newborns. One of the injuries is hypoxic-ischemic damage to the substance, which is located along the outer-superior sections of the lateral ventricles of the brain. The main damaging factor is oxygen starvation, although in some cases there are other causes. Thus, in the presence of small focal infarcts of the substance, a diagnosis of “periventricular leukomalacia” (PVL) is made.
Brain changes include cysts and cavities that form over a period of about one month. That is why neurosonography (NSG) should be performed at the end of the first month of life for all newborns.
The defeat is irreversible. This means that the treatment that is used after this diagnosis cannot help get rid of the pathology.
Premature newborns may often have other brain lesions that need to be differentiated from PVL. Some of them include cerebral leukomalacia, telencephalic gliosis, pseudocysts, multicystic encephalomalacia, subcortical leukomalacia, etc.
Consequences of pathology
The consequences of leukomalacia of the brain in children are necrosis, death of nerve cells and proliferation of microglial cells (similar to the formation of scars in other organs). The child’s brain cannot replenish the dead areas because the neurons are no longer multiplying. This phenomenon is called cystic leukomalacia.
In more than 50% of cases with periventricular leukomalacia, repeated hemorrhage occurs in the cerebral ventricles. In these newborns, the cerebral cortex is not often damaged because the blood circulates quite normally.
This disease can occur in the first days after birth and lasts for a week. It may occur later, depending on whether the child’s breathing is impaired or whether the child has a viral infection. The newborn's condition will gradually worsen as new necrosis appears.
Leukomalacia of a multifocal nature (damage 2-3 mm in size) is observed in the frontal and parietal areas more often than in the occipital and temporal areas.
This entire process develops over the course of 2 weeks; over the course of several months, the cavities recede, dead areas are replaced by scars from neuroglia, and nervous tissue atrophies.
When the child is already 1 year old, it is necessary to carefully ensure that the symptoms characteristic of PVL do not appear. If manifestations of the disease are detected, the doctor will prescribe Phenibut or Pantogam. They slow down the development of tissue atrophy in the brain.
To restore the rhythm of sleep, it is recommended to give the baby sedative medications (calming) such as tablets or tinctures based on Valerian or Melissa. In combination with them, you can use water procedures.
If the pressure increases, it must be stabilized immediately; for this it is advisable to drink Diacarb or Glycerin. The latter medication must be taken with vitamin complexes, which contain a high concentration of potassium.
Convulsive seizures are eliminated mainly with the help of Phenobarbital. If side effects appear, such as high blood pressure and rapid heart rate, then it is changed to beta-blockers. Among them you can choose Anaprilin or Obzidan.
Motor disturbances characteristic of PVL are usually relieved with the help of massage, physiotherapeutic procedures and therapeutic exercises. If there are problems with the speech apparatus, they usually turn to speech pathologists and special teachers to correct this complication.
In the most advanced cases, the baby may develop respiratory distress syndrome. This complication means acute respiratory failure and its development can be prevented by using medications based on surfactant.
Initially, it is virtually impossible to notice the differences between a child with periventricular leukomalacia and a simple baby. However, over time, this disease can lead to cerebral palsy. Its severity will directly depend on the degree and location of the lesion in the brain.
At this moment the baby has the following symptoms:
- Confusion;
- Respiratory and swallowing problems;
- High pressure;
- Mental retardation;
- Malfunctions of the central nervous system.
The prognosis for timely treatment and minimal damage to brain tissue is quite positive and only minimal neurological impairment remains. In the case of extensive lesions, cerebral palsy and mental retardation develop. It is impossible to completely eliminate such consequences.
The disease is a consequence of hypoxia and ischemia during fetal development. This problem mainly affects premature babies. After their birth, in the first weeks it is necessary to undergo neurosonography to identify pathology. In this case, undesirable consequences can be avoided, and the child will not be much different from other healthy babies.
Causes, symptoms and consequences of leukomalacia of the brain in newborns
Leukomalacia of the brain in newborns is a disease in which death and decomposition of the white matter of the brain occurs. Pathology leads to the development of cerebral palsy and convergent strabismus. The disease usually occurs in premature babies and is preceded by a hypoxic state during childbirth and early discharge of amniotic fluid.
Causes of leukomalacia of the brain
The disease is necrosis (death) of the brain's pathways, i.e., the nerve fibers that transmit nerve impulses between neurons. The causes of this pathological process are often:
- intrauterine hypoxia;
- ischemia;
- increased oxygen concentration during resuscitation of premature infants, causing depression of the respiratory center;
- intrauterine and vaginal infections;
- premature birth.
Lack of oxygen and impaired blood supply lead to the death of nerve tissue.
Leukomalacia in premature infants is caused by hypoxia due to imperfect development of pulmonary surfactant, a substance that ensures normal gas exchange in the lungs.
Respiratory hypoxia, caused by immature lungs, is aggravated in premature infants by the destruction of red blood cells containing fetal hemoglobin (i.e., hemoglobin characteristic of the developing fetus).
With respiratory and hemic hypoxia, the partial pressure of carbon dioxide in the blood increases (hypercapnia), and the oxygen content decreases. Hypercapnia leads to cerebral edema and worsening white matter necrosis.
Periventricular leukomalacia is a pathological condition when the nerve fibers adjacent to the ventricles of the brain undergo necrosis, which leads to cerebral palsy.
Multifocal leukomalacia is the presence of multiple foci of white matter destruction. After the death of nerve fibers, a cyst (with liquefaction necrosis) or a scar (with coagulation necrosis) is formed. A cyst is a cavity with fluid, and a scar is an accumulation of rough connective tissue. These formations are visualized during studies such as CT and MRI.
Why does multiple sclerosis develop in children under three years of age: causes, symptoms, prognosis.
What does asymmetry of the ventricles of the brain lead to and how to treat the pathology.
Periventricular leukomalacia in premature infants is also caused by a sharp increase in oxygen concentration during resuscitation measures. Oxygen saturation after birth asphyxia in a newborn is dangerous. This leads to depression of the respiratory center in the central nervous system and deterioration of independent respiratory function.
Infections in the genital tract in the uterine cavity lead to rupture of the amniotic sac. Such spontaneous release of amniotic fluid provokes premature labor and the birth of a premature baby with underdeveloped lungs and poor adaptation to breathing atmospheric air.
Important! Premature birth provokes blood clotting disorders and hormonal disorders in a woman (for example, lack of progesterone).
Symptoms
Cerebral leukomalacia of the newborn is a pathology that leads to damage to the pathways (myelin fibers), which leads to damage to the optic radiation (central visual pathway) running next to the lateral ventricles of the brain.
The ventricles are cavities filled with fluid. Various fibers pass next to them, including those from the optic nerves. Dry (coagulative) fiber necrosis occurs. Damage to these pathways can cause convergent strabismus.
The main symptoms of damage to the white matter of the central nervous system:
- impaired vision, hearing, coordination of movements;
- intellectual disorders;
- spastic paralysis of the limbs (cerebral palsy);
- strengthening or weakening of reflexes (tendon, joint);
- strabismus;
- convulsions in newborns.
With leukomalacia of the brain in newborns, in severe cases, consequences such as disability or death are observed. As the pathological process progresses, the destruction of myelin fibers worsens. But sometimes it is possible that leukomalacia does not manifest itself clinically: with minor injuries. With grade 1 leukomalacia, complete recovery is possible.
Diagnostics
To detect pathology in newborns, neurosonography is performed - ultrasound examination through the fontanel. In older children, ultrasound, CT or MRI are performed. If there is a threat of premature pregnancy, women are examined for sexually transmitted infections, antiphospholipid syndrome, and hormonal disorders (hypoprogesteronemia).
Treatment
Therapy includes massage, physiotherapy, correction of visual impairment, physical therapy, and acupuncture. In case of hypoxic damage, antihypoxants (Mexidol) are prescribed, which increase resistance to oxygen starvation and improve blood flow.
Actovegin, Cerebrolysin, and Neuromultivit vitamins are used as angioprotectors. The conductivity of nerve fibers is improved by the drugs Tropatsin, Dibazol. With spastic paralysis, operations to cut the tendons and obturator nerve are sometimes necessary.
Intellectual disabilities are corrected by special educational programs for children with disabilities. Nootropic drugs are used to improve impulse transmission and prevent the hypoxic process.
Read what hypoxia in newborns is and how to prevent the consequences of the pathology.
Find out what perinatal central nervous system damage is: what parents should know about.
How to recognize cerebral palsy in newborns: early signs and forms of pathology.
To improve the properties of surfactant in distress syndrome (severe respiratory distress), leading to cerebral hypoxia in infants, surfactant preparations are prescribed: Alveofakt, Surfaxin.
To prevent the situation of premature birth, it is necessary to treat sexually transmitted infections that a pregnant woman and her husband have. If there is a threat of premature birth of a child, it is necessary to use glucocorticoid hormones for the normal development of the surfactant system in the lungs. If there is a lack of progesterone, treatment with Duphaston and its analogues is required.
Forecast
Mild disease may be self-limiting, while severe disease may involve large areas of white matter. The disease should be monitored by a neurologist.
(2 5,00 of 5) Loading...
Source: https://golmozg.ru/deti/leykomalyaciya-golovnogo-mozga.html
Pathogenesis
As a result of these reasons, necrosis of the white matter of the brain occurs, after which the pathological process is supplemented by degeneration of astrocytes (stellate neuroglial cells with processes), proliferation of microglia (specific glial cells of the central nervous system) and accumulation of lipid-containing macrophages in necrotic tissues.
After this, phagocytosis of the damaged areas begins - after about 5-7 days, and after a week cysts form (this takes two weeks, and sometimes more).
In the final stages, glial scars or pseudocysts appear. Secondary hemorrhagic infarctions appear in necrotic areas. Tissue atrophy occurs within 2–4 months.
PVL develops in the first hours, but can also occur later – up to 10 days after birth. Leukomalacia can also affect in utero - if the course of pregnancy is pathological (preeclampsia, exacerbation of chronic pyelonephritis, hepatitis, fetoplacental insufficiency).
Clinical picture
Already in the maternity hospital, children experience depression of the central nervous system. It is expressed by a decrease:
- muscle tone;
- specific reflexes;
- motor activity;
About a quarter of newborn babies have seizures. Almost half of children suffer from hyperexcitability syndrome. Some infants may experience brainstem symptoms (cardiovascular and respiratory disorders).
In some cases, there may be no abnormalities in the neonatal period, and in some cases, PVL is fatal, regardless of treatment.
This pathological process is characterized by the presence of a stage of “imaginary well-being,” which can last 3–9 months, after which signs of cerebral insufficiency develop.
Periventricular leukomalacia becomes the cause of cerebral palsy (CP) in almost 90% of cases, and convergent strabismus in 60% of cases.
The severity of cerebral disorders depends on the number and area of leukomalacial cavities. However, in cases where the lesions are distributed thinly around the ventricles, the prognosis is more favorable.
The percentage of apparently healthy infants with PVL is approximately 4%. The consequences of defeat for them may be insignificant.
Changes in the brain are irreversible - for this reason, there is no radical treatment to get rid of the pathology. Therapy is aimed at eliminating negative symptoms and improving brain processes.
Since PVL in most cases occurs in premature newborns, the main measure to prevent pathology is to prolong the pregnancy period and prevent premature birth.
The incidence of complications after hemorrhage may be reduced if surfactant preparations, which reduce the manifestation of respiratory disorders, are adequately used in treatment.
In addition, equipping neonatal intensive care units with modern equipment for autonomous artificial ventilation reduces the possibility of serious consequences for children.
Supportive treatment of a child with this diagnosis should occur throughout childhood.
So, periventricular leukomalacia is a severe brain damage that occurs in newborns (mainly premature) children due to difficult labor and complicated pregnancy.
The disease should be distinguished from other pathologies (including pseudocysts, cerebral leukomalacia, telencephalic gliosis, etc.), for the reason that the treatment of these diseases may differ from each other.
The process of pathology formation
In order to understand what PVL is and how to deal with it, it is necessary to understand the mechanism of its formation. Against the background of provoking factors, a pathological focus appears in the nerve cells - due to oxygen starvation, the white matter of the organ dies. Full-fledged neurocytes are replaced by other elements that are not able to perform the same functions.
Later - after 7-14 days, periventricular cysts appear in this area - hollow or filled with a special liquid. At the final stage, scars may appear on the nervous tissue. Less commonly, secondary hemorrhagic infarctions can be observed in the lateral ventricles of the organ. Subsequently, the affected areas completely atrophy.
As a rule, periventricular leukomalacia develops in the first hours of the baby's birth. However, there are cases when the periventricular variant of the pathology occurs later - up to 5-7 days from the moment of birth.
Damage to the lateral ventricles of the brain can also occur in utero - during pregnancy, accompanied by exacerbation of pyelonephritis and hepatitis. In order to avoid this, a woman needs to contact a doctor monitoring the course of her pregnancy at the first signs of deterioration in her health.
Causes
Most often, the cause of the development of leukoencephalopathy may be a state of acute immunodeficiency or due to infection with human polyomavirus.
Risk factors for this disease include:
HIV infection and AIDS; malignant blood diseases (leukemia); hypertonic disease; immunodeficiency states during therapy with immunosuppressants (after transplantation); malignant neoplasms of the lymphatic system (lymphogranulomatosis); tuberculosis; malignant neoplasms of organs and tissues of the whole body; Sarcaidosis.
Definition of pathology
Leukoencephalopathy is always accompanied by damage to the white medulla, which occurs due to various reasons: vascular pathologies, infection with polyomavirus, gene mutations. The infectious form develops due to the reactivation of the polyomavirus JC, which lies latent in the body of many people.
The hereditary form of the disease of autosomal recessive genesis occurs against the background of a gene mutation (mainly the EIF2B5 gene). Small focal leukoencephalopathy of vascular origin is a disease that develops as a result of damage to small elements of the circulatory system of the brain, which provokes symptoms characteristic of hypoxic-ischemic tissue damage.
Main symptoms
The main symptoms of the disease will correspond to the clinical picture of damage to certain brain structures.
Among the most characteristic symptoms of this pathology are:
impaired coordination of movements; weakening of motor function (hemiparesis); speech dysfunction (aphasia); the appearance of difficulties in pronouncing words (dysarthria); decreased visual acuity; decreased sensitivity; a decrease in a person’s intellectual abilities with an increase in dementia (dementia); clouding of consciousness; personal changes in the form of changes in emotions; violation of the act of swallowing; gradual increase in general weakness; epileptic seizures are not excluded; constant headache.
The severity of symptoms may vary depending on the person's immune status. People with less weakened immunity may not have such a pronounced symptomatic picture of the disease.
One of the very first signs of the disease is the appearance of weakness in one or all limbs at the same time.
Symptoms
Small focal encephalopathy of infectious origin is characterized by the absence of signs of an inflammatory process in the medulla. Penetrating into the central nervous system, the virus causes lysis (dissolution) of oligodendrocytes, which leads to large-scale demyelination - damage to the myelin sheaths.
Infected oligodendrocytes are located at the edges of the demyelination lesion. Gradually, the pathological process covers large areas of the brain, which provokes the increasing development of neurological symptoms:
- Hemiparesis (paresis on one side of the body).
- Hemisomatosensory disorders (impaired sensitivity - numbness, tingling, change in temperature perception, change in reaction to painful stimuli, distortion of the spatial representation of the position of individual parts of the body relative to each other).
- Epileptic seizures. They are observed in 20% of patients, which indicates the proximity of the lesion to the cortex.

Depending on the location of the lesion, symptoms such as ataxia (impaired coordination during contraction of a muscle group), aphasia (speech dysfunction), visual disorders, apraxia (impaired purposeful movements), dysmetria (excess or insufficiency in performing voluntary movements) appear. Cognitive disorders are typical for the pathology, often developing into dementia.
Damage to the tissues of the hemispheres with corresponding symptoms in clinical practice occurs 10 times more often than stem structures. During an MRI study, large subcortical (subcortical) lesions are detected - hyperintense (T2 mode) and hypointense (T1 mode). As the diameter of the lesion increases, the neurological deficit increases. Vascular leukoencephalopathy is accompanied by symptoms:
- Cognitive disorders (deterioration of memory and mental activity) with a tendency to progress.
- Ataxia, motor dysfunction.
- Impaired motor coordination.
- Urinary incontinence, involuntary defecation.
Late stages of the disease are characterized by the development of dementia. Patients lose the ability to self-care and need medical care around the clock. Patients have no interest in speech, motor, cognitive, and mental activities. Periodically there is a feeling of euphoria. Some patients experience epileptic seizures.
Binswanger's disease tends to progress. Long periods of stable conditions are often observed. Dementia develops due to disruption of cortical-subcortical connections that arise as a result of damage to white matter. Dysfunction of the thalamus and basal ganglia plays an important role in pathogenesis.
Focal leukoencephalopathy is a disease characterized by changes in gait, which indicates damage to the vascular origin of the extrapyramidal system. The patient's gait becomes slow, mincing, steps are shortened, postural dysfunction is observed - difficulty moving when turning. It is difficult for the patient to initiate (start) movement. Sometimes movement disorders manifest themselves as parkinsonism (rigidity, muscle stiffness, tremor).
Symptoms are supplemented by hemiparesis (paresis in one half of the body) and pseudobulbar syndrome (dysarthria - impaired pronunciation, dysphonia - weakening of the voice, dysphagia - difficulty swallowing, involuntary crying or laughter). To make a diagnosis of multifocal leukoencephalopathy of vascular etiology, the following symptoms must be present:
- Dementia.
- Risk factors for the development of vascular diseases or signs of vascular pathology affecting the circulatory system of the brain.
- Neurological syndromes characteristic of damage to subcortical (subcortical) brain structures (changes in gait, urinary incontinence, paratonia - involuntary resistance to passive movements).
A CT scan shows bilateral leukoaraiosis - minor vascular ischemia, damage to elements of the white matter vascular system. With periventricular leukoencephalopathy, the MRI scan reveals diffuse focal lesions of the white matter, predominantly symmetrical.
For comparison, with a viral infection, the lesions are located predominantly asymmetrically. A single nonspecific focus of leukoencephalopathy may be mistakenly regarded as a manifestation of a stroke.
The forecast is disappointing
Unfortunately, it is impossible to cure leukoencephalopathy; in the absence of the above-mentioned treatment, patients live no more than six months from the moment the first signs of central nervous system damage appear.
Antiretroviral therapy can increase life expectancy from a year to a year and a half from the moment the first signs of damage to brain structures appear.
Cases of acute disease have been reported. With this course, death occurred within 1 month from the onset of the disease.
In 100% of cases, the course of the pathological process ends in death.
Symptoms and signs of the disease
It is difficult to suspect that leukomalacia of the brain has appeared in newborns - the signs of periventricular pathology are varied and extremely nonspecific. However, the lack of oxygen supply to nerve cells is not completely asymptomatic. The main clinical signs of periventricular leukomalacia:
- excessive excitability of the newborn - loudness, excessive randomness of movements;
- tendency to convulsive states;
- sluggish muscle reflexes.
In extremely premature babies, the symptoms are much more severe:
- fluctuations in body temperature;
- lethargy;
- increased drowsiness;
- decreased appetite;
- sleep disturbance;
- paresis/paralysis of limbs;
- respiratory disorders;
- visual disturbances – strabismus.

Experts emphasize that manifestations of the periventricular form of the disease may subside after the acute period. This period of imaginary well-being lasts up to 8-9 months. And only by the age of one year does leukomalacia of the brain make itself felt by a deficit of nervous activity. The course of the pathological process is indicated by:
- insufficient weight gain;
- slow growth;
- skills lag;
- discrepancy between intelligence and age;
- delayed psycho-speech development;
- pronounced emotional lability.
NSG norms and protocols – diagnostician
The article is under development.
Normally, the interhemispheric fissure has a strictly median position; the width in a newborn of 30-34 weeks of gestation is 2.8 ± 0.2 mm, in older infants it is 2.0 ± 0.1 mm. Separate assessment of the interhemispheric fissure and the falciform process is possible only in cases of fluid accumulation along the fissure and in cases of atrophy of the brain substance.
An arched deformity usually indicates a space-occupying process or fluid accumulation in the intrathecal space on one side. Displacement of the interhemispheric fissure and falciform process without deformation usually indicates hypoplasia of the cerebral hemisphere, which is often combined with changes in the facial skull.
Assessing the size of the various parts of the ventricular system is necessary to exclude ventricular enlargement (ventriculomegaly).
The most stable dimensions are the body (depth no more than 4 mm) and its anterior horn (depth 1-2 mm); the occipital horn is often asymmetrical, variable in depth and size; the dimensions of the 3rd ventricle are 2-4 mm.
Assessing the 4th ventricle is difficult, so attention is paid to its shape and structure, which can change significantly with abnormalities in brain development.
Using NSG, you can identify the level of occlusion (aqueduct - 60%, foramen of Monroe - 25%, foramina of Luschka and Magendie 10%, subarachnoid space - 5%).
There are:
- Initial signs of expansion of the ventricular system, manifested by an increase in the depth of the bodies of the lateral ventricles to 5-8 mm, the disappearance of lateral curvatures and the appearance of a rounded shape of the lateral ventricles; The 3rd and 4th ventricles are not dilated;
- Moderate ventriculomegaly - body depth up to 9 mm, slight uniform expansion of all parts of the lateral ventricles; The 3rd ventricle is enlarged to 4-6 mm, the 4th ventricle is usually normal;
- Severe ventriculomegaly - the depth of the bodies is more than 9 mm, the 3rd ventricle is dilated - interthalamic fusion in its cavity is visible, the 4th ventricle and the brain cisterns are dilated.
The average size of the cistern magna in a full-term newborn is 4-5 mm; In premature babies, the size of the cistern magna varies depending on the gestational age and can reach 10 mm or more.
The quadrigeminal cistern is usually represented by a hyperechoic line between the 3rd ventricle and the cerebellar vermis, its thickness is no more than 3 mm. It can increase with subarachnoid hemorrhages and with cysts of this cistern, which are difficult to differentiate from an arachnoid cyst in this area.
The dimensions of the cavity of the transparent septum can vary from 2 to 10 mm.
Neurosonography is normal - Protocol
The interhemispheric gap is 1 mm (the norm is up to 4 mm).
Subarachnoid spaces - 2 mm (normal is up to 3 mm).
The cavity of the transparent septum: not expanded.
Anterior horns of the lateral ventricles: on the right - 3 mm; on the left - 3 mm (norm up to 5 mm). Body of the lateral ventricle – on the right – 3 mm; on the left - 3 mm (norm up to 5 mm). Temporal horns are not detectable (normal). Atrium - filled with choroid plexuses (normal up to 12-16 mm). Occipital horns are not detected (normal).
The third ventricle is 2 mm (normal is up to 4 mm).
The fourth ventricle is triangular in shape in the sagittal plane, not dilated (normal is up to 8 mm).
Choroid plexus - 10 mm, with smooth and clear contours.
The brain parenchyma is of medium echogenicity. The pattern of convolutions and grooves is distinct. The echogenicity of the subcortical zones is not changed. Caudothalamic notches are not changed. Periventricular areas have normal echogenicity.
The structures of the posterior cranial fossa are differentiated. Large tank 5 mm (norm up to 12 mm).
Stem structures are of normal echogenicity.
In the CD mode, the arteries of the circle of Willis are determined up to branches of the 4th-5th order, zones of hypo- and hypervascularization are not identified, the course of the vessels is not changed. Indicators of velocities and peripheral resistance in the arteries of the brain are not changed: ACA IR - 0.72 (normal up to 0.72). Venous blood flow is not changed, the maximum speed in the vein of Galen is 7 cm/s (the norm is up to 10 cm/s).
CONCLUSION: The brain parenchyma is not changed. The intrathecal spaces and ventricles are not dilated. Cerebral blood flow parameters are normal.
NSG hypoxic changes - protocol
Structures are veiled and poorly differentiated. The furrows and convolutions are pronounced. Periventricular tissues and areas of the basal ganglia have increased echogenicity.
CONCLUSION: hypoxic changes.
NSG enlarged intrathecal spaces and ventricles - protocol
The structures are differentiated and symmetrical. The pattern of grooves and convolutions is “emphasized”. The interhemispheric fissure is widened: up to mm in the frontal lobes, up to mm in the parietal lobes and up to mm in the occipital lobes. Along the convexital surface in the intrathecal space, an anechoic strip is determined - up to mm.
CONCLUSION: Fluid accumulation in the intrathecal space. Dilatation of the lateral ventricles.
NSG immaturity of the brain - protocol
Structures are veiled and poorly differentiated. The furrows and convolutions are weakly expressed. S.magna is expanded to mm, the cavity of the transparent septum is up to mm, the occipital horns are deep. No expansion of other cavities is detected.
Periventricular tissues and areas of the basal ganglia have increased echogenicity.
CONCLUSION: echo signs of brain immaturity.
NSG cyst - protocol
The brain structures are formed correctly and asymmetrically. The furrows and convolutions are pronounced. In the projection of the lobe, an anechoic formation is visualized - mm, communicating with the cavity of the lateral ventricle.
The lateral ventricles are asymmetrically dilated. Anterior horns of the lateral ventricles: on the right - 3 mm; on the left - 3 mm (norm up to 5 mm). Body of the lateral ventricle – on the right – 3 mm; on the left - 3 mm (norm up to 5 mm). Temporal horns are not detectable (normal). Atrium - filled with choroid plexuses (normal up to 12-16 mm). Occipital horns are not detected (normal).
Periventricular tissues and areas of the basal ganglia have increased echogenicity.
CONCLUSION: cyst in projection
NSG subepindymal pseudocyst - protocol
Periventricular tissues of increased echogenicity. In the projection of the middle third of the choroid plexus, an anechoic inclusion with a diameter of mm is visualized.
CONCLUSION: pseudocyst of the choroid plexus.
NSG subepindymal cyst - protocol
Periventricular tissues of increased echogenicity. In the projection of the caudothalamic notch, an anechoic inclusion with a diameter of up to 5 mm is visualized.
CONCLUSION: subependymal pseudocyst.
NSG intraventricular hemorrhage 1st degree - protocol
The structures are differentiated and symmetrical.
The furrows and convolutions are well defined.
The cisterns of the subarachnoid space and the ventricular cavities are not dilated.
Periventricular tissues of increased echogenicity.
In the projection of the caudothalamic notch, an echogenic inclusion measuring mm is determined.
CONCLUSION: grade 1 intraventricular hemorrhage.
NSG intraventricular hemorrhage 2nd degree - protocol
The structures of the brain are formed correctly and symmetrically.
The furrows and convolutions are pronounced.
The cerebrospinal fluid cavities and cisterns of the subarachnoid space are not dilated.
Periventricular tissues of increased echogenicity. The choroid plexus on the right is dilated (asymmetry - mm), heterogeneous.
CONCLUSION: grade 2 intraventricular hemorrhage.
NSG intraventricular hemorrhage grade 3 - protocol
The structures are differentiated and symmetrical. The furrows and convolutions are pronounced. The interhemispheric fissure is not widened.
The lateral ventricles are dilated.
Periventricular tissues and areas of the basal ganglia have increased echogenicity.
CONCLUSION: grade 3 intraventricular hemorrhage.
NSG meningitis - protocol
The structures are poorly differentiated and veiled. The furrows and convolutions are thickened, “emphasized”. The interhemispheric fissure is widened to mm at the level of the frontal lobes, to mm at the level of the parietal lobes.
An anechoic strip up to mm thick is visualized along the convexital surface. The lateral ventricles are dilated:
Periventricular tissues and areas of the basal ganglia have increased echogenicity.
Organized pathological inclusions are not differentiated.
CONCLUSION: Meningitis cannot be excluded.
NSG agenesis of the corpus callosum - protocol
The structures are not formed correctly. The corpus callosum is absent. The interhemispheric fissure is not widened. The lateral ventricles are widened:
The grooves and convolutions extend fan-shaped from the bodies of the lateral ventricles.
The third ventricle is flask-shaped dilated (mm), pulled upward.
The fourth ventricle is elongated.
Periventricular tissues have normal echogenicity.
The choroid plexuses are deformed and not dilated.
CONCLUSION: agenesis of the corpus callosum. Dilatation of the lateral and 3rd ventricles.
Treatment of leukomalacia
Leukomalacia lesions are irreversible damage to brain tissue. There is no treatment that can restore the affected areas. However, there is symptomatic treatment that can remove the negative manifestations of the disease in a child. Among the drug therapy methods used:
Nootropics - drugs that improve blood flow to brain cells and metabolism in general (Piracetam, Nicergoline) Antihypertensive drugs for high intracranial pressure and hydrocephalus (Diacarb, Furosemide, Glycerin, potassium supplements) Anticonvulsants (Carbamazepine, Phenobarbital) Beta-blockers for high blood pressure pressure and tachycardia - increased heart rate (Anaprilin, Obzidan) Hypotonic drugs for increased muscle tone (Baclofen, Mydocalm, Relanium) Herbal sedatives for sleep disorders (Melissa, Valerian)
In addition to medications, treatment includes massage and physiotherapy, correctional classes with teachers aimed at stimulating attention and memory, as well as speech development. If drugs against intracranial hypertension are ineffective, surgical interventions are performed using shunts to eliminate excessive amounts of cerebrospinal fluid from the brain cavity. Severe LP requires treatment in an intensive care unit with a ventilator.
The prognosis of periventricular leukomalacia depends on the degree of detected disorders. The mild degree can be corrected, the violations are reversible. More severe degrees are difficult to treat with medications. Children may suffer from cerebral palsy, epilepsy, oligophrenia - mental retardation. Prevention of leukomalacia consists of trying to bring pregnancy to the required term so that childbirth is safe for the child.
Leukoencephalopathy is a disease characterized by damage to the white matter of the subcortical structures of the brain.
This pathology was described from the very beginning as vascular dementia.
Most often, elderly people suffer from this disease.
Among the varieties of the disease, we can distinguish:
Small focal leukoencephalopathy of vascular origin . Being by its nature a chronic pathological process of cerebral vessels, it leads to gradual damage to the white matter of the cerebral hemispheres. The reason for the development of this pathology is a persistent increase in blood pressure and hypertension. The risk group for morbidity includes men over 55 years of age, as well as people with a hereditary predisposition. Over time, such a pathology can lead to the development of senile dementia. Progressive multifocal encephalopathy. This pathology refers to a viral infection of the central nervous system, which results in persistent resolution of the white matter. The impetus for the development of the disease can be given by immunodeficiency of the body. This form of leukoencephalopathy is one of the most aggressive and can be fatal. Periventricular form . It is a lesion of the subcortical structures of the brain, against the background of chronic oxygen starvation and ischemia. The favorite localization of the pathological process in vascular dementia is the brain stem, cerebellum and parts of the hemispheres responsible for motor function. Pathological plaques are located in subcortical fibers and sometimes in deep layers of gray matter.
When does oxygen deprivation cause periventricular leukomalacia?
The birth of a baby is always a joyful event, but often this joy can be overshadowed by a diagnosis made by a doctor - periventricular leukomalacia.
This disease, which affects the child’s brain, directly depends on the course of pregnancy and labor.
In particular, the presence of a problem associated with oxygen starvation during intrauterine development, however... First things first
What is the baby's fault?
An unborn baby is not able to take care of its health, so its mother must do this. The main cause of leukomalacia of the brain is the lack of oxygen that the baby experiences as a result of hypoxia and oxygen starvation. And the less a mother monitors her health during pregnancy, the greater the likelihood of acquiring such an anomaly.
Arrows indicate tumors
Mostly premature infants are at risk; the ratio of sick premature infants to full-term infants is 70/30. This is due to the fact that in premature babies microcircular blood delivery is not developed, and during oxygen starvation it is the near-ventricular areas that suffer (periventricular - periventricular).
As for full-term babies, in the case of hypoxia, the brain increases blood circulation, and the consequences for them are not critical. In addition, the reasons contributing to the development of periventricular leukomalacia in premature infants include:
- infectious diseases of the mother during pregnancy;
- bad habits during pregnancy;
- the presence of severe gestosis;
- fetal hypoxia;
- unplanned caesarean section. How the infection gets to the fetus
As a rule, newborns weighing from 1500 to 2000 kg are susceptible to the disease. In addition, there is some seasonality of the disease. So, in the spring-autumn period the percentage of patients increases. Most likely, it is due to a lack of vitamins. By gender, the vast majority of patients are representatives of the stronger sex, but this does not exclude brain damage in girls.
Leukomalacia of the brain is a swelling of the brain matter into a kind of tumor. After some time, the tumor goes away, but as a result of the death of neurons, cysts form, which pose the main threat to the further harmonious development of the baby.
Leucomolation refers to one of the so-called hypoxic-ischemic encephalopathy
How does a newborn feel?
Small children, and especially infants, cannot tell their parents what is bothering them, so from the very first day it is necessary to carefully monitor the baby’s behavior, especially if there were various anomalies during childbirth or during pregnancy.
As a rule, every fourth patient has convulsive syndromes and may develop strabismus. Over time, the baby may stop responding to factors that irritate him.
The totality or each symptom individually should be carefully studied by a doctor who is able to recognize neuro-reflex abnormalities.
There are three degrees of severity of the disease:
- light;
- moderate severity;
- heavy.
Mild degree
As a rule, symptoms are noticeable within a week and after this time disappear on their own, however, observation by a neurologist if you are diagnosed with leukomalacia is necessary.
Average degree
Symptoms usually appear within 10 days. Among them are convulsive syndromes, hypertension, and changes in the human autonomic system.
Severe degree
In this case, there is long-term depression of the child’s nervous system, symptoms appear for a long time. It is possible that the baby may fall into a comatose state.
In severe cases, children are advised to go to the intensive care unit.
The main symptoms indicating the presence of periventricular leukomalacia in premature infants:
- neuro-reflex abnormalities;
- muscle hypertonicity;
- nervous excitability;
- depression of the nervous system;
- visual impairment;
- movement disorders;
- attention deficit.
Periventricular leukomalacia is the cause of cerebral palsy!
In the long term, periventricular leukomalacia leads to irreversible consequences. For example, a newborn is diagnosed with minor developmental disabilities. So, a sick baby develops differently from his peers.
For example, by the age of 4-5 months, an ordinary child calmly rolls over onto his stomach and back, while children with leukomolation are unable to do this.
In addition, due to hypertonicity, they have problems sleeping, the sucking reflex is absent or not developed, which leads to the inability to eat mother's milk, or, to be precise, not to get enough.
And hence the whims and similar manifestations.
How to treat a serious illness
It is possible to use ultrasound machines to diagnose the disease, but the difficulty lies in the fact that provincial cities with mediocre medical infrastructure are not able to afford expensive devices that support the ability to diagnose such diseases (Neurosonographs). Typically, only modern medical centers use such devices. But you need to treat!
In order to draw up a treatment plan, the doctor needs to make an accurate diagnosis, since the symptoms that indicate the presence of the disease are similar to some other ailments, such as:
- subcortical leukomalacia;
- cerebral leukomalacia;
- multicystic encephalomalacia;
- presence of pseudocysts.
Subcortical leukomalacia is an infarction of the subcortical white matter of the cerebral hemispheres (complete or incomplete). Leukomalacia, called periventricular, is much less common.
Due to the lack of an effective way to diagnose the disease at an early stage, the doctor first of all evaluates the general condition of the patient and the presence of symptoms characteristic of periventricular leukomalacia in premature infants.
As a rule, at the first stage, drugs are prescribed that improve blood circulation in the brain:
- stugeron;
- piracetam;
- nicergoline.
In addition, work is being done with motor and psychomotor disorders of the newborn.
After the child reaches the age of one year or more, treatment is carried out as needed, as a rule, it is aimed at eliminating the consequences of leukomalacia, which in adults can cause such disorders as cerebral palsy, severe mental retardation, intellectual impairment, etc.
Prevention
Prevention of disease for a newborn consists primarily of its mother observing the most banal safety measures during pregnancy:
- eliminating bad habits (alcohol and smoking contribute to oxygen starvation that the baby experiences);
- reducing to a minimum the possibility of contracting an infectious disease;
- taking vitamin complexes;
- supportive care to help you reach your due date and not give birth early.
If premature birth occurs, the first thing doctors should take care of is providing the baby with oxygen and regulating other gases entering his body.
Thus, periventricular leukomalacia is a serious disease of the central nervous system, which requires close attention, since the consequences are terrible, despite the low mortality rate, the level of disabled people who have suffered this disease is high.
Source: https://nervivporyadke.ru/detskaya-nevrologiya/periventrikulyarnaya-lejkomalyatsiya.html
Prevention of leukomalacia

To minimize the disease of the mother of the unborn child, a number of rules should be followed:
- Healthy lifestyle.
- Pregnancy planning, i.e. giving up bad habits at least six months before pregnancy.
- A balanced, vitamin-enriched diet for a pregnant woman.
- Protecting the expectant mother from stress.
- Close supervision by doctors, timely registration, adherence to all medical recommendations.
- Protect yourself from viral and infectious diseases; if they appear, consult a doctor in a timely manner.
The expectant mother should clearly understand the consequences of alcohol abuse or smoking. Doctors need to prevent the birth of a premature baby and check the pregnant woman for any diseases, abnormalities, or pathologies.