The inflammatory process in the meninges (purulent meningitis) occupies a leading place among diseases of the central nervous system in newborns. The disease is a severe infectious process that can lead to disability and death of the newborn. Often purulent meningitis was not recognized immediately; the child was admitted to the hospital with a diagnosis of acute respiratory viral infection or enterocolitis; some children had local infectious processes upon admission to the hospital.
The Yusupov Hospital provides treatment and diagnosis of diseases and subsequent complications. The hospital's best neurologists treat hydrocephalus and other central nervous system diseases. CSF and blood tests, and other tests can be done at the hospital’s diagnostic center. The clinic accepts patients aged 18+.
Symptoms of meningitis in infants
Signs of meningitis in newborns are usually not specific. Babies develop lethargy, periodically alternating with anxiety, appetite decreases, they refuse to breastfeed and regurgitate. Doctors identify the following signs of meningitis in an infant:
- pale skin;
- acrocyanosis (bluish tint of the tip of the nose, earlobes);
- bloating;
- signs of increased intracranial pressure (bulging or tense fontanelle, “brainy” cry, increased head circumference, vomiting).
Doctors identify symptoms of meningitis in newborns as shuddering, hyperesthesia, floating movements of the eyeballs, and convulsions. In the first stages of the disease, you can notice Graefe's sign, or the “setting sun symptom” - when the eyeball is lowered down, the baby's eyelid remains raised, as a result of which the eye does not close completely.
Neck stiffness (pain or inability to bring the head toward the chest) usually appears in the later stages of the disease. At the same time, neurologists find the following meningeal symptoms in infants with meningitis:
- Babinski reflex - with line irritation of the sole along the outer edge of the foot from the heel to the base of the big toe, involuntary dorsal flexion of the big toe and plantar flexion of the other fingers occur (the reflex is physiological up to 2 years of life);
- Kernig's symptom - the doctor is unable to straighten the leg of a baby who is lying on his back, bent at the knee and hip joints at a right angle (until 4-6 months of age, the reflex is considered physiological);
- Lasegue reflex - the inability to bend the baby’s leg straightened at the hip joint by more than 60-70 degrees.
In newborns, to diagnose meningitis, doctors use Flatau syndrome (dilation of the pupils when the head is quickly tilted forward) and Lessage syndrome (the baby pulls the legs towards the stomach in a suspended state) in combination with the clinical picture. Brudzinski's reflexes up to 3-4 months of a child's life are also physiological. The top symptom is passive flexion of the child's head while rapidly bending the legs at the hip and knee joints. The average reflex is considered positive if, when pressing with the edge of the palm on the area of the pubic joint, the child's lower limbs. The lower Brudzinski symptom is positive when, with passive flexion of one leg at the knee and hip joints, the other leg of the baby also bends. Negative meningeal reflexes in infants are not a reason to exclude the diagnosis of meningitis in the presence of other symptoms of the disease.
Diagnostics
To establish a diagnosis, the doctor performs special tests. Typically, the doctor presses the baby's legs against the stomach or torso and assesses the reaction. Increased pain is a positive meningeal sign and requires additional diagnostics.
One of the most accessible tests is a general blood test. Its result provides information to doctors about the specific cause of the disease. Most often, a viral or bacterial etiology of the disease can be established. The leukocyte formula in a general blood test shows how severe the inflammatory process is.
Cerebrospinal fluid examination for meningitis in newborns
At the slightest suspicion of meningitis, a lumbar puncture is performed in newborns. The diagnosis can be confirmed or excluded only on the basis of cerebrospinal fluid examination. With purulent meningitis, cloudy or opalescent cerebrospinal fluid flows out under increased pressure, in a stream or in frequent drops. Laboratory technicians find a large number of neutrophils in it. In addition to high neutrophilic cytosis, purulent meningitis is characterized by increased protein levels and low glucose concentrations. To determine the type of pathogen, bacterioscopic and bacteriological examination of the cerebrospinal fluid sediment is carried out. The cerebrospinal fluid analysis is repeated every 4-5 days until the newborn is completely recovered.
Tuberculous meningitis in newborns is extremely rare. Bacterioscopic examination of cerebrospinal fluid in tuberculous meningitis may give a negative result. For the tuberculous form of meningitis, precipitation within 12-24 hours is typical in the taken sample of cerebrospinal fluid when it is standing. The sediment is a delicate fibrin cobweb-like mesh in the form of an overturned Christmas tree, sometimes coarse flakes. In 80% of cases, Mycobacterium tuberculosis is found in the sediment.
Bacteroscopic examination of cerebrospinal fluid in cases of suspected meningococcal or pneumococcal meningitis is a simple and accurate express diagnostic method. It gives a positive result at the first lumbar puncture 1.5 times more often than culture growth. Simultaneous bacterioscopic examination of cerebrospinal fluid and blood under a microscope gives 90% positive results for meningococcal meningitis, if the examination of the newborn was carried out during the first day of hospitalization. By the third day of illness in infants, the percentage of positive results drops to 60.
With meningococcal meningitis, the disease occurs in several stages:
- first, the liquor pressure increases;
- then a small number of neutrophils are found in the cerebrospinal fluid;
- later changes are noted that are characteristic of purulent meningitis.
Therefore, in approximately every fourth case, the cerebrospinal fluid, which is examined during the first hours of the disease, does not differ from the norm. In case of inadequate therapy, the cerebrospinal fluid becomes purulent, the concentration of neutrophils in it increases, and the protein level rises to 1-16 g/l. Its concentration in the cerebrospinal fluid reflects the severity of the disease. With adequate therapy, the number of neutrophils decreases and they are replaced by lymphocytes.
In serous meningitis of viral etiology, the cerebrospinal fluid is transparent and contains a small number of lymphocytes. In some cases, the initial stage of the disease is accompanied by an increase in the concentration of neutrophils, which indicates a severe course of the disease and has a less favorable prognosis. The protein content in serous meningitis does not go beyond the normal range or is moderately increased, up to 0.6-1.6 g/l. In some infants, protein concentration is reduced due to increased production of cerebrospinal fluid.
Causes
Among the various forms of meningitis, most are infectious forms. They are often caused by various viruses or bacteria. Meningococcal infection is the undoubted leader among the causative agents of the inflammatory process of the meninges. It occurs in 70-80% of cases in patients with meningitis.
Bacterial meningitis, which is quite severe and turns into purulent forms, is caused by various types of bacteria. The most common forms of meningitis in newborns and infants are meningococcal and streptococcal. Such diseases are characterized by a severe course and frequent development of complications.
Serous meningitis is caused in 80-85% by viruses. Often the culprits of the disease are rubella, chickenpox, measles, herpes viruses and Epstein-Bar viruses. In weakened children, meningitis can also be caused by a common influenza infection. In such cases, the child usually has disturbances in the functioning of the immune system or even immunodeficiency.
For children with diabetes or taking glucocorticosteroids from birth, infection with candidal meningitis is possible. In this case, a conditionally pathogenic fungus, Candida, quickly spreads in a weakened child’s body. Getting into the meninges with the bloodstream, the microorganism quickly multiplies there and causes severe inflammation. Treatment for these forms of the disease usually takes longer than for bacterial forms.
Treatment of meningitis in newborns
Pediatricians, neurologists and infectious disease specialists draw up individual treatment regimens for meningitis in newborns. The nature of treatment depends on the type of meningitis (serous or purulent), the type of pathogen and the severity of symptoms. Doctors individually select doses of medications depending on the age and body weight of the newborn.
For viral meningitis, dehydration therapy with diuretics is performed to reduce intracranial pressure. Anticonvulsants and antiallergic drugs are prescribed, which reduce the body's sensitivity to toxins and allergens. Antipyretic and painkillers are used. Antiviral drugs and immunoglobulin are prescribed. In most cases, newborns recover within 1-2 weeks.
Bacterial meningitis is treated with antibiotics, to which various types of bacteria are sensitive. Since the analysis of cerebrospinal fluid taken during puncture takes 3-4 days, empirical therapy with antibacterial drugs begins immediately after taking blood and cerebrospinal fluid for testing. Express analysis results can be obtained within 2-3 hours. When identifying the causative agent of infection, antibiotics are prescribed to which the identified microorganisms are most sensitive. If the baby's condition does not improve 48 hours after the start of antimicrobial therapy, a repeat puncture is performed to clarify the diagnosis.
Meningitis in newborns caused by Haemophilus influenzae can be prevented by vaccination. The ACT-HIB vaccine, which is registered and approved for use in Russia, can be administered to babies from 2-3 months. Starting from the age of one and a half years, children are vaccinated against meningococcal infection with the domestic vaccine meningococcal A and A+C. The imported MENINGO A+C vaccine, registered in the Russian Federation, is administered to newborns if someone in the family is sick with meningococcal infection. Vaccination against pneumococcus with the PNEUMO 23 vaccine is given only at 2 years of age.
Meningitis in newborns is especially dangerous. Its consequences for infants can be unpredictable. Children who have suffered purulent meningitis in infancy may lag behind in mental development. Children develop deafness, visual impairment and dysfunctional mental disorders.
At the first suspicion that your baby may be developing meningitis, consult a doctor. Only the help of a qualified specialist will help save the life and health of a newborn.
Author
At-risk groups
Children of any age are not immune from meningitis. The peculiarities of the structure and functioning of the nervous and immune systems of babies in the first months after birth make them quite vulnerable to various inflammatory diseases.
Not all babies are at the same risk of meningitis. To control and monitor children who are at high risk of the disease, doctors identify risk groups for the development of meningitis. These include:
Newborn babies with very low birth weight, as well as premature babies. These babies have not yet fully developed their nervous and immune systems. The blood-brain barrier in newborns functions very differently from that in adults. Microorganisms that are small in size easily penetrate this barrier and can cause inflammation.
Children with congenital or acquired immunodeficiency. The imperfection of the cells of the immune system does not allow them to respond in a timely manner to an external pathogenic factor. The leukocyte component of immunity is not yet capable of effectively eliminating any infectious agents from the body. In such children, the risk of a severe course of any, even the most harmless infection, increases many times over.
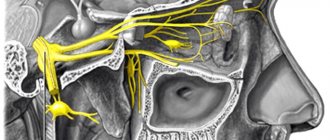
Birth injuries. Have adverse effects on the nervous system. Damage to the nerve trunks and membranes of the brain during traumatic external influences also contributes to the development of meningitis in children.
Chronic congenital diseases. Weakened children with many concomitant pathologies are not able to fight infection to the proper extent. The presence of congenital heart diseases, diabetes mellitus, and cerebral palsy affect the possible prognosis for meningitis.
How to treat?
All children with suspected meningitis must be hospitalized in a hospital. Newborn babies are delivered to hospitals equipped with all the necessary resuscitation equipment. The child must be monitored 24 hours a day by medical staff.
Treatment of the disease is carried out comprehensively. The leading role in therapy is played by eliminating the main cause that caused the disease. For infectious meningitis, large doses of antibiotics are prescribed. All antibacterial agents are administered parenterally. Intravenous administration of drugs allows you to quickly achieve the desired clinical effect and speed up recovery.
To relieve symptoms of headache and nausea, diuretics are used. Diuretics reduce high intracranial pressure resulting from inflammation and help improve the baby’s well-being.
To restore the nervous system, administration of B vitamins is used. Such injectable forms of drugs can reduce the toxic effect of bacterial agents on nerve trunks. Vitamins are usually prescribed for a long time, in courses of 10 days.
To eliminate the symptoms of intoxication, various detoxification drugs are used. Children are often given large doses of 5% glucose solution or isotonic sodium chloride solution. If seizures or movement disorders occur, electrolyte solutions are added to the treatment. With this administration of medications, the baby’s well-being returns to normal quite quickly.
After the condition has stabilized, children are prescribed immunostimulating drugs. They activate the immune system and help the immune system fight infection. Such medications are quite effective for newborns and babies in the first year of life. They are generally well tolerated and do not cause adverse side effects.