Senile dementia is a psychoneurological pathology caused by organic disorders in the functioning of the brain and blood vessels. Cognitive impairment in this disease always comes to the fore.
First of all, a person ceases to be aware of his actions, is poorly oriented in familiar terrain, is unable to use complex equipment and poses a danger to himself.
The first signs and symptoms: loss of memory for current events, while maintaining general knowledge and skills, inability to competently use household appliances and complex devices.
Causes
It is impossible to say unequivocally what was the cause of the development of the disease: there are many factors that have a negative impact on the nervous and vascular systems, which lead to senile dementia.
Most doctors are of this opinion: the disease affects those people who experience general aging of the circulatory and neuropsychological systems.
It is impossible to talk about a hereditary background one hundred percent, but it may turn out to be the decisive link that tips the scales on the side of pathology.
The following factors can cause senile dementia:
- Vascular changes in the brain, that is, atherosclerosis - the formation of so-called cholesterol plaques on the walls of blood vessels, leading to increased permeability, deterioration of nutritional functions and blood supply to the organ.
- Necrosis of brain tissue due to a stroke is hemorrhage in a certain area, which subsequently undergoes destructive changes.
- Infectious diseases that damage areas of the brain.
- Receiving head injuries, which causes a rupture between neural connections, which are subsequently replaced by connective tissue.
- A growing tumor causes compression of certain areas in which malfunctions occur or their complete exclusion from activity.
The causes of senile dementia can be various concomitant diseases that cause gradual depression or destruction of vital body systems.
Diabetes mellitus, chronic alcoholism, immunodeficiency virus - have a detrimental effect on all organs, primarily on blood vessels and nerves.
The underlying causes of the development of senile dementia is inhibition of brain functions.
This can happen due to one factor or several: in the latter case they speak of a mixed type.
ICD code senile dementia
Senile dementia is a psychoneurological pathology caused by organic disorders in the functioning of the brain and blood vessels. Cognitive impairment in this disease always comes to the fore.
First of all, a person ceases to be aware of his actions, is poorly oriented in familiar terrain, is unable to use complex equipment and poses a danger to himself.
The first signs and symptoms: loss of memory for current events, while maintaining general knowledge and skills, inability to competently use household appliances and complex devices.
ORGANIC, INCLUDING SYMPTOMATIC, MENTAL DISORDERS (F00-F09)
This block includes a number of mental disorders grouped together due to the presence of clear etiological factors, namely the cause of these disorders is brain disease, brain injury or stroke leading to cerebral dysfunction. Dysfunction can be primary (as in diseases, brain injuries and strokes that directly or selectively affect the brain) and secondary (as in systemic diseases or disorders when the brain is involved in the pathological process along with other organs and systems)
Dementia (F00-F03) is a syndrome caused by brain damage (usually chronic or progressive) in which many higher cortical functions are impaired, including memory, thinking, orientation, comprehension, numeracy, learning, language and judgment. Consciousness is not darkened. Decline in cognitive function is usually accompanied, and sometimes preceded, by deterioration in emotional control, social behavior, or motivation. This syndrome is observed in Alzheimer's disease, cerebrovascular diseases and other conditions that primarily or secondarily affect the brain.
If necessary, an additional code is used to identify the original disease.
Alzheimer's disease is a primary degenerative brain disease of unknown etiology with characteristic neuropathological and neurochemical manifestations. The disease usually begins insidiously and slowly, but progresses steadily over several years.
Vascular dementia is the result of cerebral infarction due to cerebral vascular disease, including cerebrovascular disease due to hypertension. Heart attacks are usually small, but their cumulative effect is manifested. The disease usually begins at a late age.
Includes: atherosclerotic dementia
Cases of dementia associated (or suspected to be associated) with causes other than Alzheimer's disease or cerebrovascular disease. The disease can begin at any age, but is less common in old age.
Presenile:
- dementia NOS
- psychosis NOS
Primary degenerative dementia NOS
Senile:
- dementia: NOS
- depressive or paranoid type
If necessary to indicate senile dementia with delirium or acute confusion, use an additional code.
Excludes: old age NOS (R54)
A syndrome characterized by a marked deterioration of memory for recent and ancient events, with preservation of the ability to immediate memories, a decrease in the ability to learn new material, and a disturbance in time orientation. Confabulation may be a feature, but perception and other cognitive functions, including intelligence, are usually preserved. The prognosis depends on the course of the underlying disease.
Korsakov psychosis, or syndrome, non-alcoholic
Excluded:
- amnesia: NOS (R41.3)
- anterograde (R41.1)
- dissociative (F44.0)
- retrograde (R41.2)
- alcoholic or unspecified (F10.6)
An environmentally nonspecific organic cerebral syndrome, characterized by simultaneous disturbances of consciousness and attention, perception, thinking, memory, psychomotor behavior, emotions, sleep-wake cycles. The duration of the condition varies and the severity ranges from moderate to very severe.
Included: acute or subacute:
- brain syndrome
- state of confusion (non-alcohol etiology)
- infectious psychosis
- organic reaction
- psychoorganic syndrome
Excludes: delirium tremens, alcoholic or unspecified (F10.4)
This category includes mixed conditions that are causally related to brain disorders due to a primary brain disease, a systemic disease secondary to the brain, exposure to exogenous toxic substances or hormones, endocrine disorders, or other physical diseases.
Excluded:
- associated with: delirium (F05.-)
- dementia classified under F00-F03
Changes in personality and behavior may be residual effects or comorbidities of brain disease, damage, and dysfunction.
Psychosis:
- organic NOS
- symptomatic NOS
Symptoms
Acute-onset dementia is characterized by the onset of cognitive impairment during the first month (but not more than three months) after the first or repeated strokes. Multi-infarct vascular dementia is predominantly cortical and develops gradually (over 3-6 months) after a series of minor ischemic episodes. With multi-infarct dementia, there is an “accumulation” of infarcts in the brain parenchyma. The subcortical form of vascular dementia is characterized by the presence of arterial hypertension and signs (clinical, instrumental) of damage to the deep parts of the white matter of the cerebral hemispheres. Subcortical dementia often resembles dementia in Alzheimer's disease. In itself, the distinction between dementia into cortical and subcortical seems extremely conditional, since pathological changes in dementia affect, to one degree or another, both subcortical sections and cortical structures. Recently, attention has been focused on variants of vascular dementia that are not directly related to cerebral infarctions. The concept of “non-infarct” vascular dementia has important clinical implications, since a large proportion of these patients are misdiagnosed with Alzheimer's disease. Thus, these patients do not receive timely and adequate treatment, and vascular damage to the brain progresses. The basis for including patients in the group of “non-infarction” vascular dementia is the presence of a long (more than 5 years) vascular history and the absence of clinical and computed tomographic signs of cerebral infarction. One form of vascular dementia is Binswanger's disease (subcortical arteriosclerotic encephalopathy). First described by Binswanger in 1894, it is characterized by progressive dementia and episodes of acute development of focal symptoms or progressive neurological disorders associated with damage to the white matter of the cerebral hemispheres. Previously, this disease was considered rare and was diagnosed almost exclusively posthumously. But with the introduction of neuroimaging methods into clinical practice, it turned out that Binswanger encephalopathy is quite common. It accounts for about a third of all cases of vascular dementia. Most neurologists suggest that this disease should be considered one of the variants of the development of hypertensive angioencephalopathy, in which the development of diffuse and small-focal changes is observed, mainly in the white matter of the hemispheres, which is clinically manifested by the syndrome of progressive dementia. Based on round-the-clock blood pressure monitoring, features of the course of arterial hypertension in such patients were identified. It has been established that patients with vascular dementia of the Binswanger type have higher average and maximum systolic blood pressure and pronounced fluctuations throughout the day. In addition, in such patients there is no physiological decrease in blood pressure at night and there are significant increases in blood pressure in the morning. A feature of vascular dementia is the clinical diversity of disorders and the frequent combination of several neurological and neuropsychological syndromes in the patient. Patients with vascular dementia are characterized by slowing down, rigidity of all mental processes and their lability, and a narrowing of the range of interests. Patients experience a decrease in cognitive functions (memory, attention, thinking, orientation, etc.) and difficulties in performing functions in everyday life and everyday life (caring for oneself, preparing food, shopping, filling out financial documents, orienting oneself in a new environment, etc.), loss of social skills, adequate assessment of your disease. Among cognitive impairments, first of all, memory and attention disorders should be noted, which are noted already at the stage of initial vascular dementia and steadily progress. Decreased memory for past and current events is a characteristic symptom of vascular dementia, however, mnestic disorders are more mildly expressed in comparison with dementia in AD. Memory impairments manifest themselves mainly during learning: it is difficult to remember words, visual information, and acquire new motor skills. Basically, active reproduction of material suffers, while simpler recognition is relatively intact. In later stages, impairments in abstract thinking and judgment may develop. A pronounced narrowing of the volume of voluntary attention and significant impairments of its functions - concentration, distribution, switching - are determined. In vascular dementia, attention deficit syndromes are modally nonspecific and increase as cerebrovascular insufficiency progresses. In patients with vascular dementia, there are disorders of counting functions, which, as the disease progresses, reach the degree of acalculia. Various speech, reading and writing disorders are identified. Most often there are signs of semantic and amnestic forms of aphasia. At the stage of initial dementia, these signs are determined only by conducting special neuropsychological tests. More than half of patients with vascular dementia experience so-called emotional incontinence (weakness, violent crying), and some patients experience depression. The development of affective disorders and psychotic symptoms is possible. Vascular dementia is characterized by a fluctuating type of disease course. Vascular dementia is characterized by long periods of stabilization and even a certain reverse development of mnestic-intellectual disorders, and therefore the degree of its severity fluctuates in one direction or another, which often correlates with the state of cerebral blood flow. In addition to cognitive impairment, patients with vascular dementia also have neurological manifestations: pyramidal, subcortical, pseudobulbar, cerebellar syndromes, paresis of the muscles of the limbs, often not rough, gait disturbances of the apraxic-atactic or parkinsonian type. Most patients, especially the elderly, have impaired control of pelvic functions (most often urinary incontinence). Paroxysmal conditions are often observed - falls, epileptic seizures, syncope. It is the combination of cognitive and neurological impairment that distinguishes vascular dementia from Alzheimer's disease. Aggressiveness. Apathy. Hallucinations. Closedness. Lethargy. Perseveration. Absent-mindedness. Auditory hallucinations. Weight gain.
Development mechanism
The disease has a rather complex development mechanism. The first changes in the structure of the brain occur long before the onset of dementia. As a rule, the hypothalamus is the first to be affected. Due to the naturally occurring involution, it decreases in size, and the hypothalamus is also involved in the process. Being an organ that regulates endocrine organs and metabolic processes, hormonal disruptions occur in the body. Signs of damage to the hypothalamus are short temper and sudden changes in mood.
The reduced size of the pituitary gland is not able to fully perform its functions, which is why other parts of the nervous system, especially the cortex and subcortical structures, become vulnerable.
Neurons gradually atrophy and die. Depending on which department they are located in, the symptoms change. The convolutions become pointed, the furrows expand. Due to the loss of a large number of neurons, the cavity of the ventricles expands and their walls become thinner. At this stage, many skills are lost, and complete or partial memory loss is possible.
The loss of neurons leads to a pronounced shrinkage of the brain. Senile dementia is characterized by a symmetrical decrease in its volume.
Nerve processes and neurons are prone to sclerosis after death. This is expressed in the appearance of coarse connective tissue in the lesion. Merging with each other, they form rounded foci of necrosis - senile drusen. Strands - threads - extend from them, and in the middle the lesions are filled with a brown homogeneous mass.
Symptoms
The pathology is characterized by the absence of focal neurological symptoms. The most persistent neuropsychiatric symptom at all stages of Alzheimer's type dementia is apathy. The patient is indifferent, indifferent to events and people. He does not strive for physical and mental activity, is detached from reality, and does not show emotions.
There is absent-mindedness and lack of interest in the outside world. 90% of patients with Alzheimer's disease and dementia exhibit behavioral and neuropsychiatric disorders. Characteristic marker symptoms require special attention:
- Depression, suicidal thoughts.
- Delusions, hallucinations (auditory, visual).
- Loss of self-control.
- Inappropriate sexual behavior.
- State of nervous overexcitation, agitation.
- Anxiety, astheno-neurotic syndrome.
- Lack of appetite.
- Sleep disorder.
Patients' cognitive functions deteriorate - memory, speech, logical thinking, spatial orientation. Deterioration in mood and cognitive abilities, changes in behavior can occur due to delirium (mental disorder with confusion, disturbance of perception and attention, thinking and emotions), latent medical condition (dehydration,), pain, physical and emotional discomfort.
Sleep disturbance is detected in 25-30% of patients. The causes of dyssomnia are associated with physiological processes - aging, increased activity of the suprachiasmatic nucleus, the consequences of somatic chronic diseases, side effects of drug therapy (for example, taking cholinesterase inhibitors), pain.
Prevention of senile dementia
Considering the fact that the disease cannot be cured, you need to think about preventing it in advance. It all starts from a young age, depends on how a person lived his life. In fact, you can avoid insanity, the main thing is to follow banal but very useful recommendations.
Healthy eating. Eliminate fatty, spicy fried and smoked foods from your diet. Lean more on fresh vegetables, fruits, steamed dishes, baked in the oven.
Important: you are strictly prohibited from drinking alcohol, smoking, or consuming drugs.
- Drink plenty of fluids. Water is the main supplier of oxygen to cells. If there is a lack of fluid, the functioning of the entire body is disrupted, interruptions occur in the heart, blood vessels, kidneys, liver, etc.
- Activity. Physical inactivity is a human enemy; it creates a condition in which all processes slow down, metabolism slows down, and the brain does not receive enough oxygen, which causes cell death.
None of us are immune from diseases associated with old age. The behavior of a person with dementia causes irritation and distress. In any case, you need to be patient and perceive the problem as a fact. No matter how difficult it is, you need to honorably fulfill your duty to your parents and try to alleviate their condition.
psycholekar.ru
General clinical picture
Alzheimer's disease symptoms, illness, and life expectancy are similar to those of other types of dementia and have early, intermediate, and late manifestations. BA gradually progresses, but there are also periods of plateau - a stable course. All disorders can be divided into cognitive, neurological syndromes and behavioral disorders.
Cognitive symptoms
Cognitive disorders include disorders of memory, speech, praxis, and gnosis. The most severe type is dementia. This diagnosis is made in the presence of amnesia and one of the cognitive disorders. The symptoms and onset of Alzheimer's disease are associated with diffuse damage to the white and gray matter, so the clinical picture of AD is characterized by impairment of all functions. The main symptom is considered to be progressive amnesia, which is later joined by aphasia, apraxia and agnosia; therefore, a diagnosis of dementia is appropriate for AD. The detection of focal neurological symptoms, usually absent in asthma, indicates the presence of a concomitant pathology.
Mental and behavioral disorders
The early stage and symptoms of Alzheimer's disease are already characterized by behavioral disturbances. It all starts with personality changes: the patient becomes capricious, irritable, gloomy. In the future, increased anxiety and concern appears. The patient refuses treatment, resists caregivers, and becomes tearful. During the period of severe dementia, loudness, pugnacity, insomnia, and vagrancy are common. For most asthma sufferers, symptoms worsen in the evening and at night. Patients are unable to control themselves, can undress in a public place, refuse to take medications, perceiving them as poison, feel lonely, and are often scared.
Neurological syndromes
The following syndromes are identified in patients with Alzheimer's dementia:
- parkinsonism;
- tremor;
- pyramidal syndrome;
- hypokinesia syndrome;
- pseudobulbar syndrome;
- vegetative syndrome;
- epileptomorphic seizures;
- stereotypies;
- disbasia.
The incidence of neurological syndromes does not depend on the type of disease, with the exception of epileptic seizures, which are more common in the senile form of asthma.
Frequency of neurological syndromes in different forms of asthma*
| Syndrome/frequency, % | Type I | Type II |
| Epilepsy | 2,9 | 19,0 |
| Tremor | 8,7 | 9,5 |
| Parkinsonism | 20,3 | 14,3 |
| Pyramid syndrome | 13,0 | 9,5 |
| Pseudobulbar syndrome | 78,6 | 71,4 |
| Dysbasia | 13,0 | 9,5 |
| Stereotypes | 42,0 | 57,0 |
| Hypokinesia without rigidity | 27,5 | 28,6 |
*Data presented by the Russian Academy of Medical Sciences, the Center for Extrapyramidal Diseases and the Russian Medical Academy of Postgraduate Education.
Moreover, the first symptoms of Alzheimer's disease in women and men occur with the same frequency and do not depend on the duration of the disease, age, or use of antipsychotic drugs. The severity of neurological symptoms correlates with the degree of cognitive impairment and the stage of dementia.
Classification of dementia according to ICD 10
Specialists diagnosing dementia select the main ones for a particular case from a variety of causes of impairment. Vascular dementia with ICD code 10 can be diagnosed to a patient in old age with certain manifestations or at a young age with injuries and pathology of the brain. Key numbers marked in the classification with the sign “*” cannot be used as independent numbers. Codification of dementia according to ICD 10:
- Alzheimer's disease has dementia code according to ICD 10: F00*. Alzheimer's disease is a brain disease of unknown origin, which manifests itself at the level of chemical regulatory mechanisms of the nervous system. The development of the disease occurs slowly and unnoticed by the patient and others, but progresses over several years;
- Vascular dementia ICD 10 code: F01 is interpreted as a result of cerebral infarction due to cerebral vascular disease. The development of the disease occurs at a late age;
- Dementia due to other diseases associated with causes not related to Alzheimer's disease or pathological conditions of the brain is coded: F02*. The development of the disease can begin at any age, but in old age the likelihood of its development is lower;
- dementia, unspecified. This category includes senile or senile dementia ICD: F03. Senile dementia is quite common: by the age of 80, the disease affects 25% of people.
Neurologists at the Yusupov Hospital use this classification when making a diagnosis, therefore, if a patient is diagnosed with ICD vascular dementia, then this fact is confirmed by certain clinical manifestations.
Diagnosis and treatment of dementia at the Yusupov Hospital
The neurology clinic at the Yusupov Hospital employs the country's leading specialists who specialize in the treatment of diseases associated with pathological conditions of the brain. Doctors help patients with dementia of any severity every day, around the clock.
When contacting the clinic with any complaints, the doctor sends the patient for appropriate tests. Diagnostic data allows you to make a diagnosis, for example, “vascular dementia,” and the ICD 10 code is determined for this disease. After this, a therapeutic complex is developed for the patient, which includes non-drug measures and medications. Medicines are prescribed to the patient exclusively by the attending physician, depending on the form of the disease. Vascular dementia (ICD code 10) requires taking medications that improve blood circulation and metabolic processes. The Yusupov Hospital provides a complete list of necessary medications.
Treatment in the neurology clinic for patients with dementia is aimed at socializing patients and teaching simple skills. The clinic’s neurologists pay special attention to working with the patient’s relatives, who need psychological support and training in the basics of interacting with a patient with dementia. You can ask neurologists at the Yusupov Hospital for help by phone at any time convenient for you.
Author
Polina Yurievna Vakhromeeva
Neurologist
Treatment tactics and prognosis, how long they live with this diagnosis
Unfortunately, it is not possible to radically change the course of the pathology or cure it altogether, but there are ways to influence the clinical manifestations.
More details about treatment methods can be found here. It is possible to improve the quality of life and thereby prolong it with the help of decent patient care, which should be carried out efficiently and in compliance with the recommendations of specialists.
Drug therapy for this pathology includes the following drugs:
- Nootropics help preserve memory and thinking, and improve conative functions.
- Neuroleptics or tranquilizers help stabilize the patient’s emotional background, because Often people suffer from sudden mood swings.
- Anticoagulants and antihypertensive drugs prescribed for pathologies of the vascular system. This choice is aimed at preventing strokes and heart attacks.
At the initial stage, the efforts of loved ones should be aimed primarily at maintaining the independence of the relative.
He must maintain daily responsibilities, the fulfillment of which will maintain a sense of completeness and will not allow important functions to fade away.
To maintain skills and to organize the day, relatives should create a daily routine that helps the patient feel protected and confident.
Especially for males, the issue of self-esteem is important: it is necessary to talk to a man, give him more opportunities and behave with him as a full-fledged healthy person.
The video will tell you how the relatives of a patient should behave in order to help him as much as possible and make his life easier:
The likelihood of death in senile dementia of the brain disease with proper and complete care is reduced several times.
People with this pathology live a long time, but only if all the doctor’s orders are followed.
Life expectancy will depend on the timely detection of symptoms and prescribed treatment, as well as the presence or absence of concomitant diseases, which also need to be eliminated.
It can take ten years from mild dementia to the development of senile dementia.
Senile dementia is a disease that is becoming increasingly widespread throughout the world. Elderly people living alone run the risk of not noticing the onset of the disease, which leads to disastrous consequences.
The development of dementia does not happen overnight; it is always preceded by pathological processes and chronic diseases of the body that provoke disorders in the brain.
Dementia: code in ICD-10
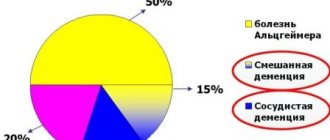
Dementia is any acquired dementia. It may be based on many organic causes, depending on the age and under what conditions it appeared. There are many forms, but the most common include:
- Vascular - with it, problems with mental activity arise due to circulatory disorders.
- Senile – also called senile, as it appears due to age-related changes in the brain.
- Mixed – which is based on both vascular and age-related disorders.
- Unspecified genesis - this form is spoken of if the objective reasons for the development of the disease could not be determined.
- Dementia associated with Alzheimer's disease.
Each of these forms is presented separately in the structure of ICD 10 and at the same time they are all combined under a common heading, since they have similar symptoms, origin, and often treatment. The general ICD 10 code for dementia in adults is presented in block F00-F03. It means that the syndrome of any of the presented forms is among the organic mental disorders (class F).
The main reason for combining diseases into this block is the fact that at the heart of all of them there is a clearly visible etiological factor. This means that the root cause of dementia is always brain disease, injury or stroke.
Signs of the syndrome develop gradually; any form of the disorder is considered progressive. But his signs are always the same and clearly defined in the classification, be it dementia of mixed genesis according to ICD 10 or typical senile insanity. Here are the main ones:
Higher cognitive functions always suffer, namely memory, thinking, attention, orientation, speech. Control over the emotional sphere, motivation, and one’s own behavior deteriorates. Motor functions gradually deteriorate.
To determine which form is typical for each specific patient, additional codes are used.
ICD-10 forms and code
Alzheimer's disease according to the ICD-10 classification includes the presenile form coded G30.0, and the senile form coded G30.1.
Diagnostic differences between the two types:
| Criteria | Types according to ICD-10 | |
| Presenile (early) | Senile (late) | |
| Debut | Development begins at young (up to 44 years) and middle (up to 65 years) age. | The first signs are established in the elderly (65-75 years) and senile period (75-90 years) of life. |
| Progression | Behavioral changes with irritability and emotional lability are noticeable. Difficulties appear in coordinating movements. | Slow progression of Alzheimer's disease. Subtle disorders, often mistaken for senile dementia. |
| Cognitive function | At an early stage, focal disorders are noticeable: fluency of speech, impoverished vocabulary, reduced executive functions, but implicit memory is preserved (the ability to hold cutlery, etc.). | Speech disorder, selection of incorrect words to replace forgotten ones (paraphasia). Difficulty coping with most daily tasks. Neuropsychiatric phenomena (wandering, crying, spontaneous screaming). |
| Neurological status | Obvious multiple severe damage to higher cortical functions. | Focal disorders are blurred, general deterioration of cortical functions. |
| Self-perception | The patient’s reaction to the existing pathology is preserved, and personal characteristics are not lost for a long time. | Violations of the personality as a social unit, reduced sensitivity to dementia of the Alzheimer's type at the initial stage. |
| Features of the clinical picture | Typical symptoms:
| Mixed symptoms, including various known types of dementia. |
Stages of development
There are three stages of disease development:
- Mild Difficulties in perceiving new information and reproducing old information, speech becomes monotonous and boring.
- Moderate At this stage, all knowledge and skills that have been acquired are erased. Fragments of old information are lost in the flow of new information, and the patient does not notice his forgetfulness. To prevent the process of degradation from accelerating, a person must be involved in all socially useful actions.
- Severe (implies complete insanity of the patient) The person cannot cook dinner, brush his teeth, or wash himself. Any elementary action turns into a disaster.
It is impossible to say exactly how long the severe stage of senile dementia lasts: the patient’s lifespan depends on the individual condition of the patient and the characteristics of his body.
It is often accompanied by neurological changes that reflect the essence of the disease:
- tremor of the limbs,
- motor impairment,
- akathisia.
It is worth noting that the last phase of dementia is the most rapid, usually after its onset a person lives no more than a year.
The video will tell you more about this stage of the patient’s life and how to help him:
At all stages of the disease, the patient needs care; hysterical forms of dementia, or pseudodementia, are precisely the reason for the lack of attention from loved ones.
Sooner or later, you have to resort to the help of professional nurses and emergency doctors; attacks of diseases that lead to dementia become more frequent at a later stage.
Find out more: what to do for loved ones of a person suffering from senile dementia, what is the treatment of the disease, what drugs are used to treat the disease.
The risk of stroke and sugar levels are monitored; if both diabetes and stroke have occurred, the patient is admitted to a hospital; unfortunately, doctors are increasingly prescribing bed rest for such patients at home.
The speed of transition from stage to stage depends on lifestyle and care.
It is impossible to avoid senile dementia, even if close relatives have not been diagnosed with it, and there are no people in the family who have been exposed to this disease.
There is a risk of developing side symptoms and signs that do not go beyond the norm and are considered standard character and behavioral disorders.
Quarrelsomeness, pickiness and greed, worsened in older age, are just such signs.
More complex types of presenile and senile forms of the disease also often go unnoticed by the neurologist, since the person does not notice forgetfulness, distracted attention and increased fatigue.
As a result, he comes to the doctor while in the middle stage of degradation.
Preventing dementia means being active, socially interacting with others, and paying attention to your health from an early age.
Stages of the disease
How many stages does the disease have and what are their symptoms?
With mild dementia, the patient may perfectly remember events that happened a long time ago, but forget current and recent episodes . We can say that a person’s “working memory” is impaired. Deviations in everyday behavior are noted, negligence appears, and orientation deteriorates.
Symptoms are complemented by absent-mindedness and difficulty solving ordinary tasks. Priorities change, a person can forget about his previous hobbies, replacing them with more primitive habits.
The moderate stage is characterized by significant memory impairment ; a person forgets large periods of time from his life. The names of acquaintances are erased from memory; the patient often does not even recognize relatives. Although the ability to take care of himself remains, the use of some household appliances poses a danger to him. At this stage, a person needs care and outside control.
In severe dementia, there is a complete loss of memory , orientation and practical skills. The patient is not even able to eat on his own. Spends almost all his time in bed. The patient needs constant care because he becomes absolutely helpless.
Vascular dementia is most often caused by stroke.
The course of the syndrome depends on the location of the affected area of the brain. In the later stages, the patient is not capable of independent living . Early diagnosis gives a better chance of successful treatment.
nerv.guru
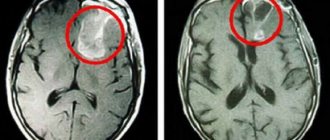
Changes in the brain
Detection of developing dementia occurs through personal conversation, special tests and instrumental studies. In this case, you can notice the appearance of lesions, depending on the type of dementia.
Changes in the brain in different types of dementia
| Type of dementia | Changes in the brain |
| Alzheimer's type | Gradual death of neurons and accumulation of beta-amyloid. Microcirculation is disrupted. At the second and third stages of the disease, one can notice enlarged grooves and ventricles of the brain, its substance is damaged, the development of dementia is aggravated by diffuse atrophy of the cortex. The amount of cerebrospinal fluid increases, hydrocephalus occurs |
| Vascular | The development of sclerosis or infarction of cerebral vessels, hemorrhages, causing extensive lesions. Gradually their number increases, in parallel with this there is a loss of those functions for which the affected area of the brain is responsible |
| Pick's disease | Development of atrophy of certain areas of the brain due to gliosis or amyloid deposition, while Pick bodies are formed at the site of the lesion |
| Alcoholic | Damage and death of neurons, vascular damage. Complicated by hemorrhages, microstrokes |
| Huntington's disease | An increase in dopamine in the ganglia, their degeneration, subsequent damage to the frontal lobes. Development of atrophy of the subcortex and cerebral cortex. |
All changes lead to the development of atrophy, reduction of brain tissue and their replacement with cerebrospinal fluid. The process is irreversible, improvement in dementia is possible, but does not last long.
Types of disease
Each type of senile dementia has its own code in ICD-10.
For Alzheimer's disease . The disease has neuropathological features and progresses over the years. The onset of the disease is 50–65 years .
Neurotic character traits become aggravated, anxiety and fear for oneself and loved ones come to the fore, poor memory aggravates the anxious state.
It is difficult for a person to express his thoughts. Over time, the help of a social worker is required. The pathological condition is dealt with by a neurologist and a psychiatrist.
Basic drugs with cholinesterase inhibitors that correct the patient’s well-being:
Treatment with folk remedies:
Vascular dementia . The consequence of hypertension is damage to the blood vessels of the brain. Makes itself felt in old age.
Brain neurons die from insufficient blood supply, the cause is atherosclerosis and coronary heart disease. The attending physician is a neurologist.
Drugs prescribed :
As additional treatment methods, you can resort to traditional medicine :
Concomitant diseases : arterial hypertension, concussions, stroke.
Pick's disease . A type of senile dementia with lesions in areas of the brain located in the frontal lobes.
It manifests itself in the same way: antisocial behavior, disinhibition of instincts, loss of cognitive abilities.
Treatment: neuroleptics and anticholinesterase agents.
For Creutzfeldt-Jakob disease . Genetic and viral pathology causes mutation of a healthy protein.
The pathogenic prion protein accumulates in the body, destroying healthy brain cells (there are no cells suitable for the development of the virus in other tissues).
Cases of infection have been reported from eating beef.
Signs of pathology remain unnoticed until old age . It is after 55 years that the degenerative properties of tissues allow the protein to develop in the human body.
For Huntington's disease . A hereditary disease caused by degeneration of gamma-aminobutyric acid.
A hallmark of this type of dementia is the presence of hallucinations and antisocial behavior. The disease is transmitted by a dominant type.
This type of dementia is difficult to distinguish from other types; the only symptom, a marker of the disease, is hyperkinesia.
For Parkinson's disease . Parkinson's disease is a debilitating neurological condition that causes dementia.
A lack of dopamine in the brain and insufficient transmission of dopamine to nerve endings make it difficult to move smoothly and make speech poor.
Protein deposits in the brain replace healthy tissue, blocking dopamine receptors, resulting in akathisia and tremors.
For an illness caused by the human immunodeficiency virus [HIV] (B22.0+) . HIV dementia is a complex of symptoms caused by microorganisms that do not develop if a strong immune system is present.
The severity of this type of dementia in older people is practically not observed - this is a special form of HIV infection.
Unspecified (NOS “not otherwise specified”) . Senile dementia with no symptoms.
The illness is on the verge of psychology/psychiatry and is often hysterical in nature. Common name: senile sclerosis.
Senile and presenile dementia
Presenile dementia occurs at early retirement age. Alzheimer's disease is an indicative type of presenile dementia.
A person ceases to understand the speech of others, and difficulty reading newspapers arises. The patient lets himself go.
Habits from a past life are forgotten, hygiene and comfort fade into the background.
Life activity decreases, by the age of 60–65 a person stops moving and slowly dies.
Alzheimer's type
Classic dementia of the Alzheimer's type is quite severe. It is diagnosed after 65 years , most likely, this is the middle - late stage of the disease.
The patient cannot distinguish complex phrases spoken to him at moderate volume. The sounds of speech perceived from the outside turn into cacophony. Rigidity of character is due to the restructuring of the brain to a simplified mode.
There is no place for hobbies and friends in a person’s life; all the time he is focused on himself and his experiences. Amnestic dementia syndrome, as a marker of the disease, occurs at a late stage of the disease.
Characterized by the inability to remember any dates or numbers.
At this stage the person becomes incapacitated . Mnestic-intellectual functions disintegrate, a person completely loses the concept of time and space. The rhythm of wakefulness is disturbed, night sleep is superficial.
The prognosis of the disease is disappointing, leading to complete maladaptation and disability . The drugs relieve only neurological symptoms, such as high blood pressure and tremors.
What is it in simple words
ICD-10 disease code: F03 – unspecified dementia.
Senile dementia is a common pathology, most often occurring in people over 65 years of age. Due to age-related changes in the structure of the brain and its involution, the patient loses many of his abilities and skills, he is not able to perceive and analyze new information, and the ability to learn and remember new information is completely lost.
After some time, dementia completely changes a person’s character and behavior, leading to a complete collapse of his personality. He stops feeling many emotions, his attitude towards family and friends changes. He loses basic skills and, as a result, becomes unable to take care of himself, take care of personal hygiene, or perform his usual work. Quite often the process is accompanied by memory loss.
A feature of senile dementia is that the patient is not aware of his condition, which is why dementia is a problem primarily for the relatives of the elderly person. Being completely socially unadapted, patients with dementia require additional assistance from social services and medical professionals.
According to statistics, senile dementia is diagnosed in 10% of people aged 65-79 years. In people over 80 years of age, the incidence rate exceeds 25%.