Description
Peroneal nerve neuropathy.
One of the mononeuropathies of the lower extremities, accompanied by foot drop syndrome - the inability to dorsiflex the foot and extend the toes, as well as sensory disorders of the skin of the anterolateral region of the leg and dorsum of the foot. The diagnosis is made on the basis of anamnesis, neurological examination, electromyography or electroneurography. Additionally, an ultrasound scan of the nerve and examination of the osteoarticular apparatus of the lower leg and foot are performed. Conservative treatment is carried out using a combination of medications, physiotherapy and orthopedic methods. If it fails, surgery is indicated (decompression, nerve suture, tendon transposition, etc.).
Symptoms and manifestations
The radial nerve is peripheral and is part of the brachial plexus. It has motor and sensory fibers, which is why it is called mixed.
Motor fibers innervate the extensor muscles of the shoulder (triceps muscle), wrist, fingers, as well as the supinator of the forearm and the muscle responsible for abductor of the thumb.
Sensitive fibers branch in the skin of the shoulder, forearm on the back side, back side and the first three fingers of the hand.
The presence of certain symptoms depends on how damaged the nerve is:
- motor;
- sensitive;
- trophic and vegetative.
Additional facts
Neuropathy of the peroneal nerve, or peroneal neuropathy, occupies a special position among peripheral mononeuropathies, which also include: neuropathy of the tibial nerve, neuropathy of the femoral nerve, neuropathy of the sciatic nerve, etc. Since the peroneal nerve consists of thick nerve fibers that have a larger layer of myelin sheath, it more susceptible to damage due to metabolic disorders and anoxia. This point is probably responsible for the fairly wide prevalence of peroneal neuropathy. According to some data, neuropathy of the peroneal nerve is observed in 60% of patients in traumatology departments who have undergone surgery and are treated with splints or plaster casts. Only in 30% of cases, neuropathy in such patients is associated with primary nerve damage. It should also be noted that often specialists in the field of neurology have to deal with patients who have a certain history of peroneal neuropathy, including the postoperative period or time of immobilization. This complicates treatment, increases its duration and worsens the result, since the earlier therapy is started, the more effective it is. The superficial peroneal nerve runs along the anterolateral surface of the leg, where it gives off a motor branch to the peroneal muscles, which are responsible for pronation of the foot with its simultaneous plantar flexion. In the area of the medial 1/3 of the leg, the superficial branch of the n peroneus passes under the skin and is divided into 2 dorsal cutaneous nerves - the intermediate and medial. The first innervates the skin of the lower 1/3 of the leg, the dorsum of the foot and the III-IV, IV-V interdigital spaces. The second is responsible for the sensitivity of the medial edge of the foot, the back of the first toe and the II-III interdigital space. Anatomically determined areas of greatest vulnerability of the peroneal nerve are: the place where it passes in the area of the head of the fibula and the place where the nerve exits the foot.
Neuropathy (neuropathy) of the femoral nerve
The cart is empty. Standard drugs Diagnoses and diseases Instructions for medicines Active ingredients Pharm. Active ingredients Instructions for medicines Pharm. By continuing to use the site, you consent to the use of cookies and agree to the privacy policy. To use Cyberis you need to enable javascript in your browser! How to do it?
Add to selection. ICD code G Associated diseases and their treatment Descriptions of diseases Neuropathy of the peroneal nerve. Mononeuropathies in adults. Standard of sanatorium-resort care for patients with damage to individual nerves, nerve roots and plexuses, polyneuropathies and other lesions of the peripheral nervous system.
Femoral nerve neuropathy. Damage to the n femoralis of various etiologies, leading to disruption of the conduction of nerve impulses through it. Clinical manifestations depend on the topic of the lesion and can be pain and sensory disturbances on the anteromedial surface of the thigh and lower leg, difficulty walking due to impaired extensor movements in the knee, etc. In the diagnosis of n femoralis neuropathy, they rely on ultrasound data of the nerve and EMG.
Therapeutic tactics include the elimination of nerve compression, metabolic, vascular, anti-inflammatory, analgesic and decongestant therapy, physical therapy and electrical myostimulation. Today it is one of the most common variants among mononeuropathies of the lower extremities.
Despite the almost year-long history of studying femoral neuropathy and its sufficient prevalence, it remains in some sense a little-known disease. Insufficient awareness of both general practitioners and some specialists in the field of neurology leads to the fact that neuropathy of the femoral nerve is often regarded as a vertebrogenic pathology, radicular syndrome, myelopathy, or as a manifestation of polyneuropathy. This is facilitated by the wide variability of symptoms, from purely sensory disturbances to the predominance of motor dysfunction, depending on the topic of the lesion.
The femoral nerve n femoralis originates from 3 lumbar spinal roots L2, L3 and L4, which, merging, form a single nerve trunk. The latter runs between the iliacus and psoas major muscles, descends to the inguinal ligament, passing under which it exits onto the anterior surface of the thigh, where it divides into cutaneous sensory and muscular motor branches and the saphenous nerve.
In the iliopsoas segment, the femoral nerve innervates the muscles between which it passes. Their function is to flex and supinate the hip, and with a fixed hip, flex the lumbar spine, allowing the torso to tilt forward.
The muscular branches that arise from the femoral nerve after it passes under the inguinal ligament innervate the muscles responsible for hip flexion and knee extension. The cutaneous branches provide sensory susceptibility to the anterior and slightly inner surface of the thigh. The saphenous nerve separates from the n femoralis in the area of the inguinal ligament, runs in front of the thigh, then takes a medial direction and enters the intermuscular canal of Gunter, the adductor canal, at the exit of which it passes along the medial edge of the knee joint, where it gives off the infrapatellar branch, innervating the anterior surface of the patella.
Next, the saphenous nerve runs along the medial edge of the leg and foot, reaching the base of the big toe. It provides sensitivity to the skin of the lower leg in front and on the medial surface, as well as the skin of the medial edge of the foot. Pathology of the femoral nerve at the iliopsoas level is often caused by its compression as a result of muscle spasm or hemorrhages in the psoas muscle that occur when it is overloaded or injured. Less commonly, neuropathy of the femoral nerve is caused by retroperitoneal hematomas or tumors of sarcoma, lymphoma.
Hematomas can form in hemophilia, thrombocytopathy and thrombocytopenia; as a complication of anticoagulant therapy used for thromboembolism and thrombosis, especially in patients with abdominal aortic aneurysm. Cases of femoral neuropathy caused by nerve damage during appendectomy, operations on the ureters and kidneys, as well as bursitis and abscesses of the iliopsoas muscles have been described.
The causes of compression of the femoral nerve in the area of the inguinal ligament can be: inguinal lymphogranulomatosis, femoral hernia, compression of the nerve by the inguinal ligament during a long forced position of the hip during surgical interventions. Nerve damage is possible during operations on the hip joint, surgical treatment of inguinal hernias, etc.
The occurrence of femoral neuropathy at the level of Gunter's canal is observed with professional or sports overstrain of the adductor muscles of the thigh that form this canal. Less commonly, muscle tension is caused by instability or abnormalities of the knee joint. Iatrogenic neuropathy can develop as a complication of knee surgery.
Isolated neuropathy of the infrapatellar branch of the n femoralis is often idiopathic in nature, but may be associated with thrombophlebitis, varicose veins, and repetitive minor trauma to the knee. The clinical symptom complex of femoral neuropathy depends on the topic of the process. When pathology occurs at the iliopsoas level, a full range of symptoms develops, including sensory, motor and autonomic-trophic disorders throughout the area innervated by the femoral nerve.
In rare cases, with a high division of the nerve, only sensory or only motor disturbances can be observed, sometimes a mosaic picture of motor and sensory disturbances. Complete neuropathy of the femoral nerve is accompanied by only partial disruption of the iliopsoas muscles, due to the existence of their alternative innervation. Therefore, flexion and supination of the hip are practically not impaired.
Paresis of the quadriceps muscle, which is responsible for straightening the leg at the knee joint, is more pronounced. Due to difficulty in extension, patients try not to bend their leg at the knee. Running and walking are difficult, especially when it is necessary to climb stairs. The gait changes. The leg is fixed in a hyperextension position.
There is a lack of knee reflex. Sensory disorders include disorders of tactile and pain perception on the anterior inner surface of the thigh and lower leg, and the medial edge of the foot.
In the same zone, trophic and vegetative changes are observed, and irritating pain is possible. When lying on the stomach, symptoms of tension are revealed - pain along the front surface of the thigh when trying to maximally raise a straight leg, Wasserman's symptom, or bend the leg at the knee joint, Mickiewicz's symptom. Neuropathy of the femoral nerve when it is affected in the area of the inguinal ligament is in general similar to the clinical picture described above. With a high origin of the saphenous nerve, predominantly movement disorders can be observed.
Along with the symptoms of tension, pain is detected when pressing in the middle of the inguinal ligament. Compression of the femoral nerve trunk in Gunter's canal is characterized by painful and tactile hypoesthesia of the skin of the medial edge of the knee joint, the anterior inner surface of the leg and the inner edge of the foot. In the same area, paresthesia and pain are observed, which increase in intensity when the lower leg is extended.
The latter forces the patient to walk and stand with the leg slightly bent at the knee. The knee reflex is not impaired. Pain is detected at the point of exit of the saphenous nerve from the adductor canal, Tinel's symptom is the appearance of paresthesia along the nerve when it is tapped with a neurological hammer.
Making a diagnosis of femoral neuropathy requires a careful and thorough examination of the lesion by a neurologist. X-rays of the spine are not very informative, since often neuropathy of the femoral nerve occurs in patients who already have changes in the spinal column, spondyloarthrosis, osteochondrosis, and radiographically detected spinal pathology does not in any way exclude the presence of neuropathy. In such cases, neuropathy is supported by the neural, rather than segmental, nature of the disorders identified during a neurological examination.
EMG helps resolve controversial diagnostic situations. With neuropathy, it reveals a slowdown in the conduction of impulses along the femoral nerve, a decrease in the amplitude of the M-response, signs of denervation in the muscles innervated by the femoral nerve and the absence of such signs in the paravertebral muscles of the L2-L4 segments.
A relatively new but promising method for studying peripheral nerve trunks is ultrasound, which can be used to assess the integrity of the nerve, identify its tumor changes, swelling, scar-adhesive deformation and degenerative processes. Ultrasound diagnostics of the femoral nerve Ultrasound of the nerve with dynamic tests allows you to determine the degree of its mobility in the adductor canal.
Damage to the femoral nerve needs to be differentiated from vertebrogenic radiculopathies L2-L4, lumbosacral plexopathy especially arising against the background of diabetes mellitus, knee injury or gonarthrosis. Treatment tactics are largely determined by the etiology of femoral neuropathy. If the femoral nerve is compressed by a retroperitoneal hematoma, urgent surgery is performed. Surgical treatment is also required in cases of traumatic nerve damage with its almost complete interruption.
Otherwise, conservative treatment is sufficient. It is based on decongestant therapy, pain relief, improvement of blood supply and metabolism of the femoral nerve.
Anti-edematous and anti-inflammatory therapy with glucocorticoids is carried out in cases of compression of the femoral nerve in the intermuscular canals or under the inguinal ligament. In this case, solutions of glucocorticoids hydrocortisone, diprospan in combination with local anesthetics lidocaine, novocaine are injected directly into the area of compression in the form of blockades.
If the pain is intense, the use of NSAIDs and analgesics is combined with the prescription of the antidepressants amitriptyline or the anticonvulsants topiramate, pregabalin, and gabapentin. For the functional restoration of the femoral nerve, vasoactive pentoxifylline, nicotinic acid and metabolic vitamins B6, B1 and their combinations are of great importance. In case of paresis of the quadriceps muscle and the lumboiliac muscles, exercise therapy, electromyostimulation and drugs that improve neuromuscular transmission, ipidacrine and neostigmine, are needed to prevent muscle atrophy and contractures.
Consultations with doctors Consultation with a neurologist any doctor - clinic doctor k. Tests General blood test without formula 3. Diagnostics Electrocardiography ECG. Surgery Oxygen therapy any 1 hour - 15 clinics 24 hours - 4 clinics 12 hours - 3 clinics. Content moderator: Vasin A. Login Registration. Menu Standard hp. Medication instructions. Diseases and syndromes. Cyberis understands what has been entered. Other sections. Selection of treatment Treatment according to the standards of the Ministry of Health. Femoral nerve neuropathy Add to selection.
Basic medical services according to treatment standards Select treatment using artificial intelligence Consultations with doctors. Consultation with a neurologist at any doctor - clinic doctor k. General blood test without the troika formula. Electrocardiography ECG. Oxygen therapy any 1 hour - 15 clinics 24 hours - 4 clinics 12 hours - 3 clinics. European MC on Shchepkina Recording. European MC in Orlovsky Lane Recording.
The femoral nerve Nervus femoralis is the largest of all the nerves of the lumbar plexus; its main function is to innervate the lower extremities.
Causes
There are several groups of triggers that can initiate the development of peroneal neuropathy: nerve injury; compression of the nerve by the surrounding musculoskeletal structures; vascular disorders leading to nerve ischemia; infectious and toxic lesions. Neuropathy of the peroneal nerve of traumatic origin is possible with knee bruises and other injuries of the knee joint, tibia fracture, isolated fracture of the fibula, dislocation, tendon damage or sprain of the ankle joint, iatrogenic damage to the nerve during reposition of the leg bones, operations on the knee joint or ankle. Compressive neuropathy (so-called tunnel syndrome) n peroneus most often develops at the level of its passage at the head of the fibula - superior tunnel syndrome. It may be associated with professional activities, for example, among berry pickers, parquet floor workers, etc., people whose work involves squatting for a long time. Such neuropathy is possible after prolonged sitting with legs crossed. When the peroneal nerve is compressed where it exits the foot, inferior tunnel syndrome develops. It may be caused by wearing excessively tight shoes. Often the cause of peroneal compression neuropathy is compression of the nerve during immobilization. In addition, compression of the n peroneus may have a secondary vertebrogenic nature, i.e., develop in connection with changes in the musculoskeletal system and reflex muscular-tonic disorders caused by diseases and curvatures of the spine (osteochondrosis, scoliosis, spondyloarthrosis). Iatrogenic compression-ischemic neuropathy of the peroneal nerve is possible after its compression due to incorrect position of the leg during various surgical interventions. More rare causes of peroneal neuropathy include systemic diseases accompanied by proliferation of connective tissue (deforming osteoarthritis, scleroderma, gout, rheumatoid arthritis, polymyositis), metabolic disorders (dysproteinemia, diabetes mellitus), severe infections, intoxication (including alcoholism, drug addiction), local tumor processes.
Peroneal nerve neuropathy - causes, symptoms, treatment
At a doctor’s appointment, you may hear three incomprehensible words addressed to you – peroneal nerve neuropathy. In medicine it is called peroneal neuropathy.
You can suspect a problem in yourself simply by standing on your heels.
If you can hold on easily, then the nerve is fine. If not, then you need to find out more about the disease. Perhaps it has already begun to imperceptibly undermine the body.
Neuropathy is damage to a nerve without inflammation.
The peroneal nerve is actually the muscle of the calves, the foot, and covers the lower extremities.
With the help of it, a person is able to move his fingers, the leg itself, bend and unbend it.
That is, this disease involves compression of the fibers in the nerve, resulting in a condition called “foot drop syndrome.”
In the International Classification of Diseases, neuropathy of the peroneal nerve belongs to class 6 - diseases of the nervous system, namely mononeuropathy, G57.8
Knowing the enemy by sight, you can fight him.
Causes of peroneal nerve neuropathy
The etiology of peroneal neuropathy is impressive. Doctors name the most common causes of the disease:
- Various injuries of the lower extremities. For example, a fracture resulted in a pinched nerve.
- Compression of fibers due to impaired blood supply. Varicose veins, blood clots, ischemia.
- Metabolic disease.
- Various infections.
- Severe general diseases.
- Malignant tumors in any organ of the body.
- Endocrine pathologies.
- Toxic poisoning.
- Blood diseases.
Neuropathy can occur with injuries of various locations. This is especially true for a fracture or bruise of the lower leg. The functioning of the peroneal nerve is significantly impaired. A fall or blow to any part of the leg or hip can also damage the nerve.
Stroke, various ischemia, osteoarthritis, joint inflammation lead to compression of the nerve with the subsequent development of neuropathy and neuralgia.
People who spend time in a bent position for a long time, for example, at work, risk getting nerve compression. This is the “sin” of farmers, harvesters and other people who are “fed by their feet.”
Patients suffering from diabetes mellitus or some kind of endocrine disorders receive a side effect of their illness. Blood sugar decreases, and “diabetic neuropathy” develops.
Alcoholism itself is a factor in the development of the disease. The chain is simple: alcohol - damage to the gastrointestinal tract and other body systems - metabolic disorders - neuropathy.
In oncology, symptoms arise as a result of cancer cell division and the appearance of metastases.
Injuries are the main reason. However, even frequent wearing of uncomfortable shoes or the habit of sitting cross-legged can lead to the onset of the disease. Such trivial situations are a provoking factor.
Symptoms of peroneal nerve neuropathy
The clinical picture shows that when the nerve fiber is damaged, the sensitivity of the limb necessarily suffers, to one degree or another.
When a leg is sharply injured, pain occurs, and all accompanying manifestations are clearly expressed.
Whereas with the chronic development of the disease there is a tendency for a gradual and slow increase in symptoms.
As a result of damage to the peroneal nerve, the following occurs:
- Impaired foot function. Inability to bend or straighten fingers normally.
- The leg is slightly concave inward.
- Inability to stand on your heels, much less walk on them.
- Edema.
- Loss of sensation in any part of the lower limb: feet, calves, or even thighs. It is especially noticeable between the first two fingers.
- Pain that gets worse when trying to sit up.
- A burning sensation in the toes or other part of the foot, as well as in the calf muscles.
- Weakness in one or both limbs.
- Feelings of heat are replaced by a feeling of cold in the lower part of the body.
- Feeling of "pins and needles".
With a long-term illness, atrophy of the muscles of the affected leg may occur.
Particular attention is paid to the patient's gait. The person “hangs” his leg, may pull it behind him, does not fully stand on his leg (first the toes, then the entire foot). At the same time, “squats” are noticeable - the knees bend too much when walking.
Diagnostics
Determining peroneal neuropathy begins with questioning. A neurologist or traumatologist listens to complaints and examines the patient.
If you suspect something is wrong, you can immediately use the “heel” test. It is not possible to stand on your heels normally - there is nerve damage.
The doctor tries to turn the foot towards the outside or straighten the toes. This is a simple test to detect neuropathy.
If this type of pathology is present, such an action will be extremely difficult (with effort) or not possible at all. Visually, you can also determine the “birdlike” gait, as well as muscle atrophy.
To determine the presence or absence of sensitivity, take a special needle and touch the desired limb.
After a preliminary diagnosis, the degree of nerve damage is clarified. To do this, electromyography is performed. They may prescribe an ultrasound of the nerve or vessels of the lower extremities, or an MRI.
If the disease arose as a result of grass, then an x-ray of the bone is taken. When the situation is not entirely clear, they resort to novocaine blockade for diagnosis.
It is important to correctly distinguish neuropathy from such pathologies as: polyneuropathy, neuropathy, PMA syndrome, as well as atrophy and tumors of the spine.
Peroneal nerve neuropathy - treatment
To literally put a person back on his feet, a complex treatment is usually selected: medication, physiotherapy, and surgery. Or just one method. The general condition of the patient and the “stage” of damage to the peroneal nerve are assessed.
Medication
Treatment tactics are aimed at reducing the activity of the disease, with which the patient has been living for many years. It was this that became the culprit of neuropathy in most cases. These are drugs against diabetes, kidney diseases and others.
Then the following is prescribed to help the patient:
- Anti-inflammatory drugs in tablets or injections. "Ketorol", "Diclofenac" and so on. They relieve pain, burning and other unpleasant symptoms.
- In tandem with analgesics, B vitamins. For example, Milgamma.
- Restoring and improving blood flow drugs. These are calcium channel blockers, such as Cordaflex; "Cavinton".
There is no need to constantly dull the pain with painkillers. Their long-term use has the opposite effect and will only worsen the situation.
Physiotherapeutic procedures
Conservative treatment includes proven methods.
Among them:
- a set of exercises from exercise therapy;
- electrophoresis;
- exposure to heat;
- massage;
- reflexology.
Massage and physical therapy should initially be carried out under the supervision of the attending physician. The principle of “do no harm” applies here. The specialist will tell you what exercises are allowed and what you should forget about.
Surgical intervention
Surgical treatment is a last resort. The decision to operate is used in cases of frequent relapses of the disease, ineffectiveness of medications and physiotherapy, as well as in cases of complete damage to the nerve fibers.
After the operation, the patient is prescribed bed rest, and after a while, exercise therapy.
There is no need to rush to get back on your feet. It is necessary to carefully monitor the operated limb. Ulcers and wounds should not form on it.
Consequences
What to expect from the diagnosis - a positive effect of treatment. In most cases it gives optimistic dynamics.
However, it is important to consult a doctor in time.
Then you can get by with physiotherapy and simple massage. A timely diagnosed disease is the key to a successful recovery.
on the topic
Source: https://neuro-logia.ru/zabolevaniya/nevropatiya/nejropatiya-malobercovogo-nerva.html
Symptoms
Clinical manifestations of peroneal neuropathy are determined by the type and location of the lesion. Acute nerve injury is accompanied by a sharp, almost immediate appearance of symptoms of its damage. Chronic injury, dysmetabolic and compression-ischemic disorders are characterized by a gradual increase in the clinical picture. Damage to the common trunk of the peroneal nerve is manifested by a disorder in the extension of the foot and its toes. As a result, the foot hangs down in a plantarflexed position and is slightly internally rotated. Because of this, when walking, moving the leg forward, the patient is forced to bend it strongly at the knee joint so as not to catch the toe on the floor. When lowering the leg to the floor, the patient first stands on his toes, then rests on the lateral plantar edge, and then lowers the heel. This gait resembles that of a rooster or a horse and has corresponding names. Difficult or impossible: raising the lateral edge of the sole, standing on the heels and walking on them. Motor disturbances are combined with sensory disorders extending to the anterolateral surface of the lower leg and dorsum of the foot. There may be pain on the outer surface of the lower leg and foot, which increases with squats. Over time, atrophy of the muscles of the anterolateral region of the leg occurs, which is clearly visible when compared with a healthy leg. Neuropathy of the peroneal nerve with damage to the deep branch is manifested by less pronounced foot drop, reduced extension strength of the foot and toes, sensory disorders on the dorsum of the foot and in the 1st interdigital space. The long course of neuropathy is accompanied by atrophy of small muscles on the dorsum of the foot, which is manifested by retraction of the interosseous spaces.
Neuritis of the peroneal nerve and tibial nerve: ICD-10 code, symptoms, treatment of inflammation
Neuritis is a pathology that is accompanied by intense pain and deterioration of mobility in the affected area.
This is mainly an inflammatory disease. It can affect one, but more often several peripheral nerves. Neuropathy of the lower extremities is included in a separate group of peripheral mononeuropathies. Since the clinical manifestations of neuritis are similar to the symptoms of injuries to the musculoskeletal system, diagnosis is jointly carried out by specialists not only in the field of neurology, but also in traumatology.
What is it and the ICD-10 code
When connections between the brain and organ nerves are disrupted and damaged, neuropathy develops. Its most common type is damage to the lower extremities - separately or both at once.
The disease develops as a result of damage to the nerve endings, as a result of which the brain loses control over the functionality of the legs.
Neuritis is an inflammatory process in nerve fibers, which in most cases is of infectious origin.
Damage to the peroneal nerve immediately affects the sensitivity of the leg . It is responsible for extending the leg, toes, and muscles responsible for turning the foot outward.
With neuritis of this nerve, the patient stops using the heel for support, the gait becomes shuffling, and the affected leg is thrown out noticeably higher than the healthy one when walking. The sensitivity of the lower leg is lost, the foot turns inward.
The functionality of the tibial nerve is the opposite of the peroneal nerve . It supplies impulses to the flexor muscles.
Symptoms of the lesion are the opposite of the previous disease: the patient steps on the heel, but cannot transfer the impulse to the toe when moving, the flexion functions of the foot and fingers are lost, the foot turns outward.
Neuritis affects different areas of the lower extremities, but these nerves converge in the lower third of the leg . Both diseases have similar causes, clinical presentation and treatment, so they are usually considered as one nosology.
In ICD-10, NMN neuritis of the tibial and peroneal nerve belongs to class 6 - diseases of the nervous system, namely mononeuropathy, its code is G57.8.
Causes of inflammation
Neuritis can occur for the following reasons:
- Nerve damage – limb injuries, nerve compression by colloid cords after surgery.
- Nerve compression - tunnel syndrome - prolonged stay in a position that is uncomfortable for the lower extremities, often occurs as a result of professional activity.
- Vascular pathologies and other blood supply disorders - this leads to tissue hypoxia, therefore, metabolic processes are disrupted.
- Toxic lesions - diabetic, kidney.
- Infectious lesions - one of the branches of the nerve fiber is involved in the inflammation process.
- Neuropathy of compression-ischemic etiology develops against the background of the presence of neoplasms - as the tumor increases in size and metastasizes.
Athletes are susceptible to neuropathy, especially runners , people who, due to their professional activities, are forced to lift heavy objects and injure their lower extremities.
It also affects overweight people - in this case, the load on the foot increases significantly, which leads to deformation or damage to the nerve fiber.
Women who wear high-heeled shoes for a long time , especially those with extra pounds and in old age, also risk the development of neuritis. Often the pathology occurs in people who walk barefoot or in shoes without heels at all - with thin soles.
Clinical picture
The symptoms of neuritis of the lower extremities certainly depend on the location of the nerve damage.
The main symptoms are as follows:
- problems with sensitivity;
- severe pain in the area of the affected nerve.
In addition, the disease is accompanied by:
- swelling of the legs;
- periodic sensation of pins and needles and numbness on the surface of the legs;
- convulsions and involuntary spasms may occur;
- patients have difficulty walking, mainly due to pain.
If the tibial nerve is damaged, flexion of the toes is impossible, the movement of the foot is limited - it is abducted outward.
Patients may complain of:
- feeling of coldness in the foot;
- burning;
- pain around the ankle that moves down to the toes;
- difficulty while walking.
Signs of peroneal nerve neuritis:
- loss of temperature, pain and tactile sensitivity of the spot on the back, side-front and in the area of the toes,
- pain in the lateral surface of the foot and lower leg, which intensifies when the limb is flexed,
- difficulty in straightening the toes,
- weakness, to the point of complete impossibility, in the concept of the outer edge of the foot,
- “cock gait” - the leg is bent at the knee and hip joint,
- sagging and turning of the foot inward,
- amyotrophy,
- change in skin color in the affected area - from blanching to a brown or bluish color.
Patients complain that while walking they are forced to step first on their toes and then on their heels.
In addition, it is not possible to straighten the toes and rotate the foot into an anatomically correct position. The patient cannot stand on his heels and walk on them .
How is the problem diagnosed?
Diagnosis begins with collecting an anamnesis, which can guide a specialist in the right direction to identify the cause of the pathology.
A detailed study of the motor function and sensory sphere of the nerve fibers of the affected limb is also carried out.
To do this, the doctor conducts special tests that give an idea of the muscle strength of different muscle groups of the foot and ankle . The specialist uses a special needle to carry out the tests.
Functional tests are carried out - the doctor asks the patient to bend his toes, stand on his heels, walk on his heels, and rotate his foot.
In addition, it is prescribed:
- Electromyography is an assessment of the movement of an impulse along a nerve fiber.
- Ultrasound – assessment of the choroid plexuses and soft tissues.
- MRI or CT - pictures are taken in different planes, and they display all the structures of the lower extremities. Necessary to clarify the localization of the pathological focus.
- X-ray – prescribed for injuries.
- Laboratory tests - blood tests and so on.
In some cases, thermography of the lower extremities is prescribed - this is a type of medical diagnosis that is based on the use of infrared rays.
During a thermal examination, abnormal areas differ in color from healthy tissues , which gives an idea of the localization and extent of the pathological process.
Neuritis must be differentiated from infectious lesions, injuries, cancer, and toxic effects on the body.
Principles of treatment
After identifying the causes that caused the neuritis, appropriate therapy is prescribed:
- if bacterial in nature - antibiotics and sulfonamides;
- for a viral infection - interferon and gamma globulin;
- for ischemic - vasodilator drugs;
- in case of trauma – immobilization of the limb, anti-inflammatory, diuretic, vitamin and painkillers.
If necessary, surgical intervention is performed. Physiotherapy, massage and special gymnastic exercises are also prescribed . Of all the physiotherapeutic techniques, electrophoresis, electromyostimulation, and magnetic therapy give the best results.
Massage therapy is carried out using smooth movements with minimal pressure from the periphery to the center. The “squeezing” technique is also used - the plantar and dorsal surfaces, as well as all tissues from the fingers to the knee, are compressed. Stretching procedures are carried out until a feeling of tolerance is felt - each toe and the base of the ankle.
Massage can relieve pain and improve the condition, but it can also aggravate the situation, so it should be performed by an experienced specialist as prescribed by a doctor.
Therapeutic gymnastics includes the following exercises:
- anaerobic;
- to maintain balance;
- for flexibility;
- power.
Gymnastics in water is very useful.
What consequences and complications can there be?
Neuritis of the lower extremities without modern and proper treatment can cause disability and partial loss of ability to work. A complication may be paresis, which manifests itself in decreased strength of the limbs.
Forecast and prevention of occurrence
The prognosis of the pathology depends on how soon the patient sought help from a specialist and how correct the treatment was. Irreversible changes significantly worsen the prognosis and lead to disability.
To prevent the occurrence of neuritis, it is recommended:
- maintain optimal body weight;
- protect your feet from injury;
- periodically give your legs a break during prolonged vertical or uncomfortable body positions;
- wear comfortable shoes with orthopedic insoles;
- do not wear high-heeled shoes on a regular basis;
- people involved in sports need to be regularly screened for compression-ischemic neuropathy (tunnel syndrome).
It is strictly not recommended to delay treatment of the pathology at the first symptoms , as this can aggravate the situation and lead to irreversible consequences. Ignoring the symptoms of pathology leads to incapacity and permanent disability.
The video will tell you about the symptoms and treatment of tibial nerve neuritis:
will talk about the manifestations and treatment of peroneal nerve neuritis:
Source: https://nerv.guru/zabolevaniya/nevrit/tipy-i-vidy/konechnostej/malobercovyj-i-bolshebercovoyj-nerv.html
Diagnostics
The diagnostic algorithm for peroneal neuropathy is based on the collection of anamnestic data that may indicate the genesis of the disease, and a thorough examination of the motor function and sensory sphere of the peripheral nerves of the affected limb. Special functional tests are performed to evaluate the muscle strength of various muscles of the lower leg and foot. Surface sensitivity analysis is carried out using a special needle. Additionally, electromyography and electroneurography are used, which make it possible to determine the level of nerve damage based on the speed of action potentials. Recently, nerve ultrasound has been used to study the structure of the nerve trunk and structures located next to it. In case of traumatic neuropathy, consultation with a traumatologist is required, according to indications - ultrasound or radiography of the knee joint, radiography of the lower leg bones, ultrasound or radiography of the ankle joint. In some cases, diagnostic novocaine nerve blocks can be used. Peroneal nerve neuropathy requires differential diagnosis with LV-SI radiculopathy, hereditary recurrent neuropathy, Charcot-Marie-Tooth disease, PMA (peroneal muscular atrophy) syndrome, ALS, polyneuropathy, other mononeuropathies of the lower extremities, cerebral tumors and spinal tumors.
ICD 10. Class VI (G50-G99)
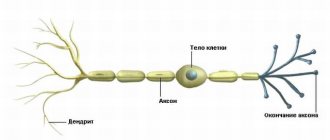
The femoral nerve Nervus femoralis is the largest of all the nerves of the lumbar plexus; its main function is to innervate the lower extremities. Like any nerve, the outside of Nervus femoralis is covered with a myelin sheath, which well protects the structure of the nerve fiber itself. When the surface layer of myelin is defective, a pathology develops called neuropathy or neuropathy. Femoral nerve neuropathy is a process in which degenerative-dystrophic disorders occur in the nervous tissue, mostly in its myelin sheath.
As a result, nerve impulses are conducted less well, which leads to pain in the innervated area and motor defects. In the ICD 10 world classification of diseases, this pathology is placed under the codes G56 - G These are the symbols that are written on the sick leave to indicate complete or partial neuropathy of the femoral nerves.
Any pathology of the nerve fiber can be asymptomatic for a long time. Both diabetes and chemical exposure, and even the notorious alcohol, take time to destroy the integrity of the tissue. Over time, pain and crunching in the back and joints can lead to dire consequences - local or complete restriction of movements in the joint and spine, even to the point of disability.
People who have learned from bitter experience use a natural remedy to heal joints, which is recommended by orthopedist Bubnovsky. A person may periodically experience discomfort when walking, tingling in the affected area, but such symptoms are rarely a reason to see a doctor. The patient sees a neurologist only when the symptoms become pronounced and complex treatment is required. Among the instrumental diagnostic methods, the most accurate for differentiating pathology is electroneuromyography.
You can see the equipment for carrying it out in the picture. The procedure is absolutely safe and painless for the patient. But this method is used only in specialized neurological institutions. Ultrasound of the nerve with additional dynamic tests is also used. In addition, the doctor conducts a visual examination, prescribes clinical tests and x-rays. Symptoms of neuropathy directly depend on the topic of pathology, i.e. Sometimes, even in the case of complete damage to the Nervus femoralis, muscle function is partially impaired, since there is alternative innervation in the iliopsoas region.
But in the knee area, the pathology manifests itself more clearly, with paresis of the quadriceps muscle. Have you ever experienced constant back and joint pain? Judging by the fact that you are reading this article, you are already personally familiar with osteochondrosis, arthrosis and arthritis. Surely you have tried a bunch of medications, creams, ointments, injections, doctors and, apparently, none of the above has helped you. And there is an explanation for this: it is simply not profitable for pharmacists to sell a working product, since they will lose customers!
Nevertheless, Chinese medicine has known the recipe for getting rid of these diseases for thousands of years, and it is simple and clear. A patient with neuropathy can be easily identified on the street by his altered gait. People suffering from mono- or polyneuropathies are characterized by shuffling steps and uncertain movement. Note that treatment of femoral nerve neuropathy is a lengthy process and not always successful.
Of course, integrated approaches are used that take into account, first of all, the cause of the disease. Drug treatment includes vitamins, analgesics, regenerating and metabolism-improving drugs.
Regular courses of physiotherapy are of great importance. For neuropathy of toxic etiology, treatment is aimed primarily at eliminating harmful effects. If this is work in harmful conditions, it is advisable to change it, but if the patient takes any medication for a long time, it may be necessary to replace it with a less toxic analogue.
The patient’s regimen and lifestyle is of great importance in the treatment of any pathology, including neuropathy. Healthy habits are the best prevention. This is an axiom. How to forget about back and joint pain?
We all know what pain and discomfort are. Arthrosis, arthritis, osteochondrosis and back pain seriously spoil life, limiting normal activities - it is impossible to raise an arm, step on a leg, or get out of bed. These problems begin to manifest themselves especially strongly after 45 years. When you are face to face with physical weakness, panic sets in and it is hellishly unpleasant.
But there is no need to be afraid of this - you need to act! Which product should be used and why - says leading orthopedic doctor Sergei Bubnovsky. The information presented on the site should not be used for independent diagnosis and treatment. Specialist consultation is required.
Copying materials is possible only with a hyperlink to the TvoyPozvonok website. Home Video lessons for doctors. Contents Causes of the disease Diagnosis: how to identify the disease Typical signs How the pathology is treated. Expert opinion Pain and crunching in the back and joints over time can lead to dire consequences - local or complete restriction of movements in the joint and spine, even to the point of disability.
A little about the secrets Have you ever experienced constant pain in your back and joints? Matveeva Maria - Medical journalist. First category nurse in the department of traumatology and orthopedics. If you liked the article, rate it: votes: 2 average: 3.00 out of 5.
We also recommend that you read: Arthralgia of the knee joint - the causes may be different Myogelosis of the cervical spine Causes, symptoms and treatment of cervicocranial syndrome, cervicocranialgia Polymyalgia rheumatica Myofascial pain syndrome.
List of diseases. Medicines and drugs. Take a spinal health test.
Femoral nerve neuropathy in ICD GG57 is manifested by inflammation or damage to its myelin sheaths, which leads to impaired impulse conduction. This disease is most often caused by compression of the nerve trunk.
Treatment
Patients with peroneal neuropathy are supervised by a neurologist. The issue of surgical treatment is decided upon in consultation with a neurosurgeon. An integral part of treatment is the elimination or reduction of the causative factor of neuropathy. In conservative therapy, the anti-edematous, anti-inflammatory and analgesic effect of NSAIDs (diclofenac, lornoxicam, nimesulide, ibuprofen, etc.) is used. Drugs in this group are combined with B vitamins, antioxidants (thioctic acid), and agents for improving nerve blood circulation (pentoxifylline, nicotinic acid). The prescription of ipidacrine and neostigmine is aimed at improving neuromuscular transmission. Pharmatherapy is successfully combined with physiotherapy: electrophoresis, amplipulse therapy, magnetotherapy, electrical stimulation, ultraphonophoresis, etc. To restore the muscles innervated by the n peroneus, regular exercise therapy is required. To correct foot drop, patients are advised to wear orthoses that fix the leg in the correct position. Indications for surgical treatment are cases of complete disruption of nerve conduction, lack of effect of conservative therapy, or relapse after it. Depending on the clinical situation, neurolysis, nerve decompression, suture or plastic surgery may be performed. In case of old neuropathies, when the muscles innervated by the peroneal nerve lose electrical excitability, surgical interventions are performed to move the tendons.
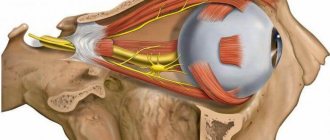
Causes and treatment of oculomotor nerve palsy
As a result of head injuries and other unfavorable factors, paresis of the oculomotor nerve occurs.
The condition is accompanied by drooping of the upper eyelid, double vision, and lack of pupillary response to light.
At the first symptoms, you should consult a doctor who will conduct a diagnosis, prescribe medications and therapeutic exercises for the eyes, perform surgery and give preventive recommendations.
Causes of pathology
Paresis can provoke a chronic inflammatory process of the ENT organs.
In a healthy organ, the oculomotor nerve provides innervation to the muscles that contribute to the mobility of the eyelid and eyeball. Under the influence of unfavorable factors, nerve conduction is disrupted, paralysis of the extraocular muscles develops and the eye becomes motionless. The main causes of pathology in adults:
- traumatic brain injury;
- cardiovascular diseases;
- aneurysm;
- diabetes;
- benign or malignant neoplasms of the head or face;
- rapid muscle fatigue (myasthenia gravis);
- autoimmune diseases;
- stroke.
At an early age, the pathology can be caused by meningitis.
Paresis of the eye muscles in children occurs under the following circumstances:
- birth injury;
- severe infectious diseases (meningitis, meningoencephalitis, measles);
- underdevelopment of the oculomotor muscles;
- heredity.
Symptoms: how to recognize the disease?
Healthy eyes move synchronously. Paralysis of the external muscles of the eye is characterized by the inability to fully move the organ of vision to the sides. If one eye moves normally, but the other lags behind, this may indicate the development of pathology. Paresis of the abducens ophthalmic nerve manifests itself as follows:
- splitting of objects;
- drooping upper eyelid;
- strabismus;
- unnatural dilation of the pupil and lack of its reaction to light;
- impaired eye mobility from side to side;
- inability to see objects that are at different distances;
- exophthalmos.
How is diagnosis carried out?
During an examination of the patient, a neurologist may suspect that he has such a problem.
An ophthalmologist can recognize oculomotor nerve palsy. If necessary, you should consult a neurologist. The doctor conducts a visual examination, takes a medical history, and performs diagnostic procedures, such as:
- angiography of eye vessels;
- magnetic resonance and computed tomography;
- ophthalmoscopy;
- friendly and direct reaction of the pupils to light;
- checking the mobility of the eyeballs.
Physiotherapy
To strengthen the eye muscles and improve vision, a set of eye exercises is recommended, which includes the following exercises:
Bringing the organs of vision to the nose will help strengthen their muscular system.
- Move your gaze from the ceiling to the floor without moving your head.
- Look diagonally from the top corner of the room to the opposite bottom corner.
- Perform circular rotation of the eyes and frequent blinking.
- Bring the visual organs to the nose.
- Intensively squeeze and unclench your eyelids at a fast pace.
- Move your eyeballs up and down.
- Fix a black circle on the window glass at a distance of 30 cm from the eyes. Move your gaze from this point to objects outside the window: houses, trees, vehicles.
Other methods
To treat abducens nerve palsy, doctors recommend the following treatment methods:
- Corrective glasses. They are prescribed to improve vision by a doctor individually, based on the patient’s health condition.
- Viewing stereo images. The benefit of the procedure is to strengthen the eye muscles, normalize blood circulation, increase the load on the nerve fibers, which improves the innervation of the eyes, and helps to speed up focusing when examining objects at different distances.
- Electrophoresis. It is characterized by the effect of electric current on nerve endings, which helps improve nerve conduction of the optic nerve.
Prevention
To avoid paralysis of the muscles and nerves of the left or right organ of vision, head and face injuries should be avoided.
People who have problems with the heart or blood vessels are advised to undergo a routine examination by a doctor and carefully take prescribed medications.
It is necessary to avoid stress - one of the main causes of stroke, which leads to paralysis of the eye structures. All chronic diseases that can cause pathology should be kept in remission.
Source: https://EtoGlaza.ru/bolezni/esche/parez-glazodvigatelnogo-nerva.html
Clinics for treatment with the best prices
Price
Total: 121in 13 cities
Source
- Excluded
: current traumatic lesions of nerves, nerve roots and plexuses - see nerve injuries by body region, neuralgia, neuritis (M79.2), peripheral neuritis during pregnancy (O26.8), radiculitis NOS (M54.1)
- G50 Trigeminal nerve lesions Includes
: 5th cranial nerve lesions - G50.0 Trigeminal neuralgia
- G50.1 Atypical facial pain
- G50.8 Other lesions of the trigeminal nerve
- G50.9 Trigeminal nerve disorder, unspecified
- Includes
: lesions of the 7th cranial nerve
: postherpetic inflammation of the knee ganglion (B02.2)
- Excluded
: disorders of the auditory (8th) nerve (H93.3), optic (2nd) nerve (H46, H47.0), paralytic strabismus due to nerve palsy (H49.0-H49.2)
- G53.0 Neuralgia after herpes zoster (B02.2)
- Excluded
: current traumatic lesions of the nerve roots and plexuses, lesions of the intervertebral discs (M50-M51), neuralgia or neuritis NOS (M79.2), neuritis or radiculitis: brachial NOS, lumbar NOS, lumbosacral NOS, thoracic NOS, radiculitis NOS, radiculopathy NOS (M54.1), spondylosis (M47.-)
- G55.0 Compression of nerve roots and plexuses due to neoplasms (C00 - D48)
- Excluded
: current traumatic nerve damage - see nerve injury by area of the body
- Excluded
: current traumatic nerve damage - see nerve injury by area of the body
: sciatica: NOS (M54.3) associated with intervertebral disc disease (M51.1)
- G58.0 Intercostal neuropathy
- G59.0 Diabetic mononeuropathy (E10 - E14 with common fourth character .4)
Description of the disease
Peroneal neuropathy, or peronial neuropathy, is one of the most common neurological diseases. Disease code according to ICD-10 G57 – mononeuropathies of the lower extremities.
Neuropathy occurs equally frequently on both the right and left peroneal nerves.
The myelin sheath of a thickened dense nerve is much thicker than that of others. It arises from the lower 1/3 of the ischial, descending through the popliteal fossa and passing on the anterior side of the leg, dividing into internal and external branches, innervating the dorsum of the foot. The anterior branch is divided into motor and cutaneous branches, innervating the skin of the leg, foot, interdigital spaces and fingers.
Thanks to them, the foot and toes are extended and its outer edge is raised. Often, trauma to the nerve occurs at the point where it enters the foot - in the area of the head of the fibula.
With acute or chronic hypoxia or compression, damage to the nervous tissue and demyelination occurs, as a result of which the passage of impulses through the fibers is disrupted until they are completely absent. Due to their absence, the functioning of the foot is disrupted: it is impossible to bend and straighten it - foot drop syndrome. The disease is also accompanied by impaired sensitivity of the back of the foot and the skin of the lower leg in front.
According to statistics, women are more susceptible to the disease. Pathology is more often detected in girls and girls aged 10-19 years.
Treatment of peroneal nerve neuropathy
The medical term “peroneal nerve neuropathy” (FMN) is quite well known, but knowledge about this serious disease usually ends with the mentioned phrase.
A test for the presence of pathology can be carried out by standing on your heels: if you can easily stand on them, there is no reason for concern, otherwise you should learn more about SUI.
Note that the terms neuropathy, neuropathy, neuritis are different names for the same pathology.
Anatomical certificate
Neuropathy is a disease characterized by nerve damage that is non-inflammatory in nature. The disease is caused by degenerative processes, injuries or compression in the lower extremities. In addition to SUI, there is tibial nerve neuropathy. Depending on the damage to motor or sensory fibers, they are also divided into motor and sensory neuropathy.
Peroneal nerve neuropathy leads in prevalence among the listed pathologies.
Let's consider the anatomy of the peroneal nerve - the main part of the sacral plexus, the fibers of which are part of the sciatic nerve, departing from it at the level of the lower third of the femoral part of the leg.
The popliteal fossa is where these elements separate into the common peroneal nerve. It bends around the head of the fibula along a spiral trajectory. This part of the nerve's "path" runs along the surface.
Consequently, it is protected only by the skin, and therefore is under the influence of external negative factors that affect it.
Then the peroneal nerve divides, resulting in its superficial and deep branches. The “area of responsibility” of the first includes the innervation of muscle structures, rotation of the foot and sensitivity of its dorsal part.
The deep peroneal nerve serves to extend the fingers, thanks to which we are able to feel pain and touch. Compression of any of the branches disrupts the sensitivity of the foot and its toes; a person cannot straighten their phalanges. The task of the sural nerve is to innervate the posterolateral part of the lower third of the leg, the heel and the outer edge of the foot.
ICD-10 code
The term “ICD-10” is an abbreviation for the International Classification of Diseases, which was subjected to its tenth revision in 2010.
The document contains codes used to designate all diseases known to modern medical science. Neuropathy in it is represented by damage to various nerves of a non-inflammatory nature.
In ICD-10, NMN is classified in class 6 - diseases of the nervous system, and specifically - mononeuropathy, its code is G57.8.
Cause of occurrence
In most cases, acute oxygen starvation up to anoxia leads to destructive processes in the myelin sheath, disrupting tissue metabolism. Often, this occurs for the following reasons:
- injuries;
- compression;
- vascular pathology;
- infections;
- toxins.
Peroneal nerve neuropathy occurs after injury to the knee, ankle, fibula, or lower leg. These can range from minor bruises to severe dislocations or fractures.
Compression occurs due to compression of the fiber by musculoskeletal structures. Often the compression form of the pathology occurs in people whose work activity requires prolonged squatting. For example, paving slab or parquet layers, berry and vegetable pickers, and others. In this position of the body, compression and disruption of trophism occurs. Another name for compression neuropathy is “tunnel syndrome.”
With vascular pathologies, a lack of oxygen and nutrients depletes the tissues of the lower limb.
Infections and toxins destroy the myelin sheath and tissue.
Reference . In some cases, damage occurs during surgery unrelated to neuritis. This complication is one of the most common when performing operations on the knee joint, lower leg and ankle.
Radial nerve neuropathy - what is it?
Radial neuropathy is a type of peripheral neuropathy and can develop even after minor exposure. Its function is to ensure flexion and extension of the arm in the area of the forearm, hand and phalanges, movement of the thumb and turning the palm with the back side up. In addition, sensory branches of the nerve provide innervation to certain parts of the hand.
The radial nerve stretches along the entire upper limb, and has several vulnerable points - on the back near the armpit, in the area of the humerus and elbow. The destruction of its structures and tissues occurs due to the inflammatory process, metabolic disorders and exposure to toxins, which causes discomfort and impaired motor functions.
According to the international classification of diseases ICD-10, neuropathy of the radial nerve was assigned code G56 - mononeuropathy of the upper limb.
For reference: the disease is considered one of the most common peripheral mononeuropathies, and occurs in patients of any age and gender.
Due to the anatomical structure and location of the radial nerve (it is quite close to the muscles and bones), even a slight impact on vulnerable points is enough to cause damage, so there can be quite a few causes of neuropathy.
- Squeezing (compression). Often the development of pathology is caused by incorrect posture during sleep, when the arm is under the head or body for a long time. As a rule, this position is typical for people in a state of extreme fatigue or intoxication.
- Fractures and injuries of the humerus. Neuropathy of the radial nerve after such injuries develops, according to various sources, in 3-1% of cases, and the nerve itself usually remains intact - the development of the disease is provoked by scars that appear on healed tissues.
- Medical errors. Negative effects on the radial nerve can be either traumatic or associated with certain medical procedures. This may be prolonged compression with a tourniquet to stop bleeding or an error when performing injections - incorrect insertion of a syringe needle into the shoulder area can damage the structures and tissues of the nerve. This category includes the incorrect use of crutches for leg injuries - constant pressure on the armpits and forearms causes compression of the radial nerve.
- Infectious diseases. Sometimes neuropathy acts as a complication of bacterial and viral infections, including measles, pneumonia, typhus, influenza, and herpes virus.
Less commonly, the causes of pathology are intoxication with heavy metals or alcohol, hormonal disorders and pregnancy in women, benign neoplasms, diabetes mellitus, inflammatory processes in muscles and nerves.
Interesting: Radial neuropathy is most often caused by compression of the arm during sleep, which is why it is called “Saturday night palsy.”
Symptoms
This is what a foot with damaged peroneal nerve looks like
Clinical manifestations of peroneal nerve neuropathy depend on the location of the lesion and the form of the disease. Thanks to specific signs, doctors are able to accurately determine the location of the pathological process.
Signs of high compression
A characteristic sign of compression of a nerve before its branching (in the area of the popliteal fossa) is inhibition of all its functions at once, since the impulse does not pass through any of its branches. The most frequently identified complaints are:
- pain on the lateral part of the lower leg, intensifying during squats;
- inability to straighten the foot and toes;
- violation of abduction of the outer edge of the foot;
- the foot droops down and bends inwards - “horse foot” syndrome;
- the patient cannot stand or walk on his heels, stepping only on his toes;
- loss of sensation on the front surface of the leg;
- Chronic compression leads to atrophy of the leg and foot muscles, causing the affected leg to lose weight.
Their severity and intensity depend on the intensity of compression. So, with strong compression, the nerve impulse does not pass through the tissues, completely stopping the performance of those functions for which the nerve is responsible. The gait changes completely, and a characteristic lameness appears. To move your leg, you have to bend your knee strongly to avoid damaging your heel.
Compression of the external cutaneous nerve
Symptoms are mild due to the additional innervation of this area by the tibial nerve. Patients complain of decreased sensitivity of the skin of the lower leg and may not perceive minor touches. There is slight numbness of the skin.
Damage to the superficial peroneal nerve
The main symptom is the appearance of pain and burning on the lower leg and the back of the foot and the first four toes. Due to decreased sensitivity, it is difficult to lift and abduct the heel, their gait takes on a characteristic appearance - in order not to catch the heel, the patient strongly bends the leg at the knee joint, moves it forward and stands first on the toes, and then on the heel.
Deep branch lesion
It is difficult for the patient to straighten the foot and its toes due to severe muscle weakness, which is accompanied by their drooping. There is a significant decrease in sensitivity on the back of the skin and the surface of the fingers. Light touches and tingling sensations are not felt, depression of sensitivity is accompanied by a feeling of numbness. Muscle atrophy and a decrease in leg size indicate a long period of disease.
How does facial neuritis manifest?
Symptoms of radial nerve neuropathy can be different - depending on the location and degree of the pathological process, the disease is manifested by disturbances in sensitivity, motor and autonomic functions of the hand.
- Motor manifestations. Patients with this diagnosis have difficulty extending the hand and elbow, and the ability to move the forearm is slightly impaired.
- Sensitive manifestations. Severe pain syndrome occurs in the area of the muscles of the forearm and elbow, manifests itself with intense movement of the hand and fingers (especially when trying to bend and straighten them), and burning pain in the area of the thumb is also possible, which spreads to the entire arm up to the forearm and shoulder.
- Vegetative manifestations. One of the symptoms of the disease is numbness and a crawling sensation on the skin; the most common is loss of sensation on the back of the hand and mild numbness of the shoulder.
- Radial tunnel syndrome. Carpal tunnel syndrome is a neurological disorder characterized by acute pain in the back of the hand and upper forearm that occurs when trying to move the fingers or wrist.
- Impaired supination of the hand and forearm. Supination of the hands and forearms is the ability to rotate the hand so that the palm faces down, parallel to the surface of the floor or thighs. With lesions of the radial nerve, impaired supination occurs quite often.
The symptoms of the disease vary depending on the location of the pathological process - it can be concentrated in the forearm, elbow or wrist.
For reference: one of the clear signs of pathology is the so-called “dropping hand” symptom (when trying to raise the arm up, the patient’s hand will hang down).
The symptomatic picture is bright, expressed in:
- pain in different facial areas, in the occipital region, ear, eye area; lips, gums, and tongue also hurt. The pain worsens when touching a hypersensitive area or exposure to cold;
- paralyzed state of one side of the facial area with muscle laxity.
The patient is hypersensitive to sound effects, he hears poorly, perceives taste poorly or does not feel it at all.
Facial paralysis, characteristic of this neuropathy, is easily diagnosed. The patient has:
- smoothness of the frontal fold of the inflamed facial area;
- skewed oral area;
- a symptom in which the patient cannot completely close the eyelids of the paralyzed area of the face, but when he looks up, the eyeball is observed to roll back.
The patient must urgently receive medical help if he is unable to move his eyebrows, puff out his cheeks, whistle or blow sharply, fill the mouth with water, blink one and the other eye, or close his eyes completely.
The disease is expressed in different degrees of severity. In its mild form, it is almost invisible visually, only a thorough medical examination, during which the doctor detects a difficult-to-close eye and oral asymmetry. The moderate and severe form is expressed by aggravation of the condition in the form of moderate, pronounced, severe, absolute weakness.
With an inflamed facial nerve, the patient may drool from the corner of the mouth in the paralyzed area, bite the inside of the cheek when chewing, and the cheek swells during a conversation. The patient's speech is slurred and it is difficult for him to speak. His mouth is dry and he is thirsty.
Treatment
Therapy is aimed at eliminating neuropathy, normalizing the functioning of muscle tissue and relieving symptoms. Often, this requires eliminating the cause of the pathology. Depending on the nature and course of the disease, doctors determine the tactics for managing the patient. In some cases, symptomatic drug therapy is sufficient, but an integrated approach is required to achieve the desired result.
Important! To improve the condition and prevent exacerbation, he recommends wearing only comfortable orthopedic shoes that ensure the anatomically correct position of the foot.
Drug therapy
With the help of drugs, it is possible to relieve inflammation and swelling after injury, improve blood circulation in the lower extremities and ensure normal trophism and oxygen supply to the nerve. Most often, patients are prescribed the following groups of drugs:
- non-steroidal anti-inflammatory drugs - by relieving inflammation, they eliminate swelling and pain;
- B vitamins – improve trophism of the nervous system;
- drugs that improve the passage of nerve impulses - help restore limb function;
- vascular agents – improve the condition of the vascular wall, improving blood circulation;
- antioxidants – necessary during the recovery period during rehabilitation.
Only the attending physician can prescribe medications and a regimen for their use after a thorough examination.
Physiotherapy
With the help of various physiotherapeutic procedures, it is possible to achieve a significant improvement in the condition of the nervous tissue and its functioning. The following physiotherapy procedures are most effective:
- therapeutic massage – improves blood circulation and oxygen saturation of tissues. Helps restore skin sensitivity, strengthens and restores atrophied muscles;
- magnetic therapy - activates the microvasculature and metabolic processes, helping to restore nerve conduction. Reduces pain, improves muscle condition;
- electrophoresis - used to achieve greater effect from drug therapy. Medicines are injected directly into the affected area using an electric current;
- electrical stimulation - electric current excites the cells of the neuromuscular system, helping to improve their functioning.
Mud, healing baths and other methods are also used.
Exercise therapy
Therapeutic exercises are necessary for patients with peronial neuropathy during the rehabilitation period. Active muscle contraction promotes increased blood circulation and saturation of the affected tissues with oxygen and nutrients. Thanks to this, inflammatory processes are eliminated, pain is reduced and skin sensitivity is improved. Enriching the MBN with oxygen improves its condition and ensures normal conduction of impulses.
Physical exercise is indispensable for muscle atrophy. By activating their work, they will help restore muscle mass.
Depending on the severity of the disease, the exercises are performed lying down or standing. One of the simple exercises while lying down is to imitate walking.
A rehabilitation specialist will help you choose the most optimal set of exercises, taking into account your physical fitness and general health.
In case of severe damage to the leg and severe muscle atrophy, patients are prescribed to wear special orthopedic braces: orthoses.
Watch a video about therapeutic exercises for peroneal nerve neuropathy.
Surgical treatment
Surgical correction of the pathology is carried out only in severe cases, when the innervation of the leg below the knee has completely ceased. Surgery is also indicated when other treatment methods are ineffective and for outdated neuropathies.
Surgery is also performed for post-traumatic neuropathy.
The purpose of the operation is to restore the integrity of the nerve structure if it is ruptured. If there is a tendency to compression, the location of the tendons or nerve may change.
G50-G59 Lesions of individual nerves, nerve roots and plexuses
The inability of the eye to rotate outward results in esotropia, the main symptom of which is diplopia, in which two images appear side-by-side.
The condition is usually unilateral, but can also occur bilaterally. Unilateral abducens nerve palsy is the most common of the isolated ocular motor nerve palsies.
Nerve dysfunction is caused by esotropia, a convergent strabismus at the fixation distance. At near fixation, the affected individual may have only latent deviation and be able to maintain binocularity or have less esotropia. Patients sometimes rotate their face toward the affected eye, moving the eye away from the affected lateral rectus muscle to control diplopia and maintain binocular vision.
Diplopia is typically experienced by adults with abducens palsy, but in children with this condition, diplopia may not occur due to suppression. Although this is a positive adaptation in the short term, in the long term it can result in a lack of proper development of the visual cortex, resulting in permanent vision loss in the suppressed eye; a condition known as amblyopia.
Because the nerve exits at the bottom of the brain, it is often the first to be compressed when intracranial pressure increases. Different representations of the condition, or combinations with other conditions, may help localize the site of injury along the abducens nerve pathway.
In children, Harley [5] reports typical etiologies, traumatic, tumor, most often brainstem glioma, as well as idiopathic in nature.
Abducens nerve palsy causes inward deviation of the eyes, see the pathophysiology of strabismus. Valle et al. The pathophysiological mechanism of abducens nerve palsy with increased intracranial pressure has traditionally been considered to be stretching of the nerve along its long intracranial path, or compression by the temporal bone ligament or temporal bone rib.
J Neurol Neurosurg Psychiatry; —Isolated lesions of the abducens nerve nucleus will not result in isolated abducens nerve palsy because the formation of paramedian pontine reticular fibers passes through the nucleus of the contralateral oculomotor nerve.
Thus, a nuclear lesion will result in ipsilateral gaze palsy. In addition, the fibers of the facial cranial nerve wrap around the abducens nerve, and if they are also affected, abducens nerve palsy will result in ipsilateral facial palsy.
In Millard Gubler syndrome, unilateral softening of brain tissue resulting from obstruction of the pontine blood vessels involving the abducens and facial cranial nerves and the corticospinal tract, abducens palsy and ipsilateral facial nerve palsy occur with contralateral hemiparesis. Because the abducens nerve passes through the subarachnoid space, it is adjacent to the anterior inferior and posterior inferior cerebellar and basilar arteries and is therefore vulnerable to compression against the clivus.
The nerve runs adjacent to the mastoid sinus and is vulnerable to mastoiditis, leading to inflammation of the meninges that can lead to Gradenigo syndrome. This condition results in abducens nerve palsy with associated ipsilateral hearing loss, as well as paralyzing facial pain and photophobia. Similar symptoms may occur secondary to fractures of the petrous portion or tumors of the nasopharynx.
The nerve passes into the body sinuses adjacent to the internal carotid artery and oculosympathetic fibers responsible for pupil control, so lesions here may be associated with pupillary dysfunctions such as Horner's syndrome. In addition, the involvement of the oculomotor, trochlear, V1 and V2 trigeminal nerves may also indicate sinus involvement, since all go to the sinuses of the orbital wall.
Lesions in this area can result from vascular problems, inflammation, metastases and primary meningiomas. Of course, the abducens nerve is short and an orbital lesion rarely results in isolated abducens nerve palsy, but it is more typical to include one or more of the other intraocular muscle groups in the features. Differential diagnosis is not difficult in adults.
The onset of the disease is usually sudden with symptoms of horizontal diplopia. Abduction limitations that mimic abducens nerve palsy may be secondary to surgery, trauma, or the result of other conditions such as myasthenia gravis or thyroid eye disease. In children, the differential diagnosis is more difficult due to the challenges associated with children being difficult to collaborate with to fully investigate eye movements.
As an alternative, a diagnosis of abduction deficiency is possible, which would include:. Cross-fixation, which develops in the presence of infantile esotropia or locked nystagmus syndrome and results in lateral rectus weakness. Iatrogenic injuries. Abducens nerve palsy is known to occur from the placement of halo orthoses. The resulting paralysis is identified by loss of lateral vision following orthosis placement and is the most common traumatic brain injury to the nerve associated with the device.
The first goals of management should be to identify the cause of the disease and treat it where possible or to relieve the patient's symptoms where they are present. In children who rarely notice diplopia, the goal will be to maintain binocular vision and thus promote proper visual development.
After this, an observation period of 9 to 12 months without further intervention is necessary, as some paralysis can be restored without surgery. This is usually achieved through the use of Fresnel prisms. These thin, flexible plastic prisms can be attached to the patient's glasses, or plain glasses if the patient does not have refractive errors, and serve to compensate for misalignment within the affected eye.
Unfortunately, the prism is correct up to a certain degree of misalignment, and since the affected individual's degrees of misalignment will vary depending on the direction of gaze, they may still experience diplopia when looking on the affected side. Prisms are available with different angles and must be selected for the individual patient. However, in patients with large deviations, the thickness of the required prism may reduce vision so much that binocularity is unattainable.
In such cases, it may be more appropriate to simply close one eye temporarily. Occlusion should never be used in children, firstly because of the risk of stimulus induction of amblyopia and thirdly because they do not experience diplopia. Other management options at this initial stage include the use of botulinum toxin, which is injected into the ipsilateral medial rectus muscle.
The use of BT serves a number of purposes. First, it helps prevent contractures of the medial rectus muscle that can occur as a result of resistance to its action over a long period. Secondly, by reducing the size of the deviation, a prismatic correction can be temporarily used, the use of which was not previously possible and, thirdly, the removal of traction on the medial rectus muscle can serve to determine whether the paralysis is partial or complete, by allowing any movement of the lateral rectus muscle.
Thus, the toxin works both therapeutically, helping to reduce symptoms and improve prospects for fuller ocular movements after surgery, and diagnostically, helping to determine the type of surgery most suitable for each patient. Conservative Treatment When the residual esotropia is small and there is a risk of surgical overcorrection, or when the patient is unfit or unwilling for surgery, prisms can be incorporated into his glasses to provide more consistent symptom relief.
Where the deviation is too great for effective prismatic correction, permanent occlusion may be the only option for patients unfit or unwilling for surgery.
The choice of procedure will depend on the degree of residual function in the affected lateral rectus muscle. In cases of complete paralysis, the preferred option is to perform a vertical muscle transposition procedure, such as the Jensen, Hummelheim, or total muscle transposition procedure, to utilize the function of the inferior and superior rectus muscles to achieve at least some degree of abduction.
This procedure is rarely used but may be appropriate for individuals with complete paralysis who, due to other health problems, are at increased risk for anterior segment ischemia associated with complex multimuscular transposition procedures. If some function remains in the injured eye, the preferred procedure depends on the extent of muscle complications. These changes serve to reduce variations in eye misalignment across different gaze positions.
Where this process is fully accomplished, the preferred option is simple recession, or weakening of the medial rectus muscle of the affected eye combined with resection of the lateral rectus muscle of the same eye. However, where delayed contralateral rectus paralysis has not occurred, there will still be a discrepancy between eye positions, more noticeable in the field of action of the affected muscle. Material from Wikipedia - the free encyclopedia. Abducens nerve palsy Figure showing the pattern of innervation of the rectus medialis and lateral muscles of the eye.
ICD H Abducens Nerve Palsy. October 9, Paralytic strabismus in children. Etiologic incidence and management of the third, fourth, and sixth nerve palsies. English translation in Wolf, The classical brain stem syndromes. Springfield, Thomas, Unaugmented vertical muscle transposition surgery for chronic sixth nerve paralysis.
Partial rectus muscle-augmented transpositions in abduction deficiency. Modified transposition procedure of the vertical recti in sixth nerve palsy.
Am J Ophthalmol. Eye diseases - eye pathology H00-H59, - Accessory structures. Dacryoadenitis Epiphora Inflammation of the lacrimal sac Xerophthalmia Malformations of the tear-producing apparatus Neoplasms of the lacrimal glands. Exophthalmos Enophthalmos Orbital cellulitis Orbital lymphoma Periorbital cellulitis. Conjunctivitis Allergic conjunctivitis Pterygium Pinguucula Subconjunctival hemorrhage Trachoma Dry eye syndrome.
Eyeball. Scleritis Episcleritis Sclerokeratitis. Keratitis Herpetic keratitis Acanthamoeba keratitis Fungal keratitis Corneal ulcer Photokeratitis Thygeson's superficial punctate keratopathy Dystrophies Corneal dystrophy Fuchs Meesmann's corneal dystrophy Juvenile epithelial corneal dystrophy Keratoconus Transparent marginal corneal degeneration Keratoglobus Megalocornea Keratoconjunctivitis sicca Keratoconjunctivitis Neovascularization of the cornea Kayser-Fleischer rings Corneal arch Band keratopathy.
Choroiderma Choroiditis Chorioretinitis. Cataract Aphakia Ectopic dislocations of the lens Anomalies in the development of the lens Artephakia. Retinitis Chorioretinitis Cytomegalovirus retinitis Retinal detachment Retinoschisis Ocular ischemic syndrome Central retinal vein occlusion Retinopathy Bietti crystalline dystrophy Coates disease Diabetic retinopathy Hypertensive retinopathy Purtscher retinopathy Retinopathy of prematurity Macular degeneration Stargardt disease Retinal pigment degeneration Cro retinal effusion Central serous retinopathy Macular edema Epiretinal membrane Macular pucker Vitelliform macular degeneration Congenital Leber's blindness Birdshot chorioretinopathy Retinal angiopathy.
Glaucoma Ocular hypertension Destruction of the vitreous body Leber's hereditary optic neuropathy Dry eyes Fungal keratitis Phthisis of the eyeball.
Refraction and Accommodation. Visual path. Optic neuritis Optic papillitis Papilledema Foster Kennedy syndrome Optic nerve atrophy Optic neuropathy Leber's hereditary optic neuropathy Kjaer's optic neuropathy Optic disc drusen Toxic and nutritional optic neuropathy Toxic lesions of the optic nerve Ischemic optic neuropathy Anterior ischemic optic neuropathy Posterior ischemic optic neuropathy.
Conjugate gaze palsy Convergence insufficiency Internuclear ophthalmoplegia One and a half syndrome. Eye infections are chronic generalized. Trachoma Onchocerciasis. Categories: Ophthalmology Eye diseases. Hidden categories: Wikipedia: Articles with overrides from Wikidata Wikipedia: Articles with sources from Wikidata. Namespaces Article Discussion. Views Read Edit Edit code History.
In other projects Wikimedia Commons. In other languages Deutsch English Polski Edit links. This page was last edited on October 15 at Text available under a Creative Commons Attribution-ShareAlike license; In some cases, additional conditions may apply.
Complications and consequences
Peroneal nerve neuropathy is not life-threatening for the patient and does not affect its duration. But its manifestations significantly worsen the quality of life.
Complications arise in the absence of proper comprehensive treatment of the problem. If innervation is not restored, muscle weakness will remain, a symptom of dropped leg. Progressive muscle atrophy can cause severe lameness and pain.
Important! The sooner you start restoring atrophied muscles, the greater the chance of returning them to their normal state. Completely atrophied muscles are extremely difficult to restore.
Disruption of innervation for a long time can be complicated by damage to the musculoskeletal system. The development of arthrosis significantly worsens the prognosis of recovery, accompanied by persistent severe joint deformation and severe pain.
What do you need to remember?
- Peroneal nerve neuropathy is a lesion of the nerve tissue in any of its areas.
- Most often, pathology occurs due to injury and compression of the nerve.
- The main manifestations are impaired expansion of the foot and fingers, impaired sensitivity of the anterior surface of the lower leg.
- The diagnosis is established after a thorough examination of the patient and a series of neurological tests.
- Complex treatment with drug therapy, physical therapy, exercise therapy and surgical correction allows you to completely restore the functioning of the affected structure.
- Often, the disease can be completely eliminated.
Literature
- Averochkin A.I., Shtulman D.R. Tunnel neuropathies // Journal. neuropathol. and psychiatrist, named after. S.S. Korsakov. -1991. No. 4. — P.3-6.
- Akimov G.A., Odinak M.M. Differential diagnosis of nervous diseases: A guide for doctors. St. Petersburg: Hippocrates, 2000. - 664 p.
- Voznesenskaya T.G. Pain syndromes in neurological practice //ed. AM V;yn. M.: Medpress, 2001. - 368 p.
- Flores LP, Koerbel A., Tatagiba M. Peroneal nerve compression resulting from fibular head osteophyte-like lesions. Surg Neurol 2005; 64(3):249-52.
- Perkins AT, Morgenlander JC Endocrinologic causes of peripheral neuropathy. Pins and needles in a stocking-and-glove pattern and other symptoms. Postgrad Med 1997;102(3):81-2, 90-2, 102-6.
Source