Akathisia is a periodic or constantly present motor restlessness, an urge to move or change position. It manifests itself as the impossibility of staying calmly for a long time in one position or without moving. It is manifested by fussiness, aimless movements, restlessness. People suffering from the disorder being analyzed are unable to sit or stand quietly. In some cases, motor activity is observed during sleep. The often described illness is a consequence of the use of antipsychotics. Non-drug variation of akathisia is caused by iron deficiency syndrome and carbon dioxide intoxication.
Signs and symptoms
Symptoms of akathisia range from mild feelings of restlessness or anxiety to feelings of fear. People walk for hours because putting pressure on their knees reduces discomfort. When the legs get tired, they sit or lie down, but this does not relieve the symptoms.
If misdiagnosis occurs with antipsychotic neuroleptic-induced akathisia, more antipsychotics may be prescribed, worsening symptoms.
Many patients describe symptoms of neuropathic pain similar to fibromyalgia and restless leg syndrome. While side effects disappear quickly and markedly when the medication is stopped, late persistent akathisia may continue long after the offending drug is stopped, sometimes for several years.
Symptoms:
- voltage;
- insomnia;
- feeling of discomfort;
- motor restlessness;
- severe anxiety;
- panic.
Additionally, not all observed restless movements represent a syndrome. For example, mania, excited depression, and attention deficit hyperactivity disorder may look like akathisia, but the movements are felt voluntarily and not due to anxiety.
Burns scale
During the examination, the patient sits and then takes arbitrary positions, in each of which he needs to remain for about two minutes. At the same time, the doctor carefully records the emerging symptoms and subjective sensations of the patient.
The data obtained is assessed on a special scale and conclusions are drawn.
So, joint movements: 0 - normal, 1 - there is slight motor restlessness (shuffling, stamping), 2 - symptoms are quite pronounced, 3 - vivid manifestations, the patient cannot remain motionless.
The patient’s awareness of the presence of motor restlessness: 0 - normal, 1 - no awareness, 2 - inability to keep his legs at rest, 3 - constant need to move.
How does the patient assess motor restlessness: 0 - normal, 1 - weak, 2 - moderate, 3 - severe.
Determination of the patient’s general condition: 5 - pronounced, 4 - clear, 3 - average, 2 - weak, 1 - doubtful.
Causes
Akathisia is often associated with the use of dopamine receptor antagonist antipsychotic drugs. Associated with medications that block the transmission of dopaminergic substances to the brain. In addition, drugs with successful therapeutic effects in the treatment of drug-induced akathisia have provided additional insight into the involvement of other systems.
These include benzodiazepines, β-adrenergic blockers, and serotonin antagonists. Another important reason is withdrawal syndrome. Because dopamine deficiency plays an important role in the development of the leg-focused form of the disease, sudden discontinuation or rapid reduction in dosage of medications that increase signaling hastens the onset of the disease.
This is why sudden cessation of opioids, cocaine, serotonergics, and other euphoric substances usually causes the syndrome as a side effect.
The disorder is associated with Parkinson's disease. It is unclear, however, the cause of the disease or the medications used to treat it, such as carbidopa, levodopa (levocarb).
Antidepressants also cause akathisia by increasing serotonin signaling in the central nervous system. This explains why serotonin antagonists are often very effective treatments. In clinical trials of antidepressants, the disorder is often incorrectly coded as “agitation, emotional lability, hyperkinesis (hyperactivity).”
Akathisia has been found to be associated with elevated levels of the neurotransmitter norepinephrine, which regulates aggression, vigilance, and arousal.
Find out more Bloating: causes of abdominal syndrome
The table shows factors grouped by type, with examples and brief explanations for each:
| Category | Examples |
| Antipsychotics | Haloperidol, amisulpride, risperidone, aripiprazole, lurasidone, ziprasidone; |
| SSRIs | Fluoxetine, paroxetine, citalopram, sertraline; |
| Antidepressants | Venlafaxine, tricyclics, trazodone, mirtazapine; |
| Antiemetics | Metoclopramide, prochlorperazine, promethazine; |
| Refusal of medications | Antipsychotic effect; |
| Serotonin syndrome | Harmful combinations of psychotropic drugs |
Akathisia: is it possible to get rid of it?
The term “akathisia” is more familiar to narrow specialists than to a wider audience. To an ordinary person far from medicine, this word means nothing. Until he comes face to face with the disease.
What is akathisia and how does it manifest itself?
Akathisia is a syndrome of chronic restlessness in adults combined with a feeling of severe internal anxiety. It manifests itself as a constant thirst for movement, in making aimless movements that can interfere with the person himself and those around him.
The patient cannot sit still, he is burdened by being in a calm state, he constantly moves his legs, jumps up, walks from corner to corner along the same route.
This can happen not only during the day, but even at night, when a person gets up during sleep to walk aimlessly. As a result, night sleep is disrupted, an inversion of day and night sleep occurs, and the rhythm of life and daily routine are disrupted.
Gradually, this leads to the inability to live a normal life, increased anxiety, asocialization of the individual, and the development of various mental disorders.
Akathisia can occur as a side effect of taking certain medications (this will be discussed below). The syndrome is often associated with other pathologies. Initially, the term “akathisia” was introduced and described by the Czech psychiatrist L. Gaskovec as a phenomenon accompanying certain mental disorders in 1901.
Later, French doctors fleshed out this theory, linking the development of akathisia with the disease of secondary parkinsonism. We were talking about a disease that occurs as a complication of encephalitis. Over time, thanks to the discoveries of scientists, the list of risks has been expanded.
It turned out that people with Parkinson's disease, chronic alcoholics, drug addicts, as well as patients taking a number of psychotropic medications are often susceptible to symptoms of akathisia.
Causes of akathisia
The reasons for the development of akatizive syndrome are divided into several types.
- Taking psychotropic drugs.
The most common side effect of chronic anxious restlessness occurs from taking antipsychotics: haloperidol, droperidol, pimozide.
A similar effect is less common after atypical antipsychotics (olanzapine, aripiprazole) and antidepressants (mirtazapine). Sometimes sedatives (chlorpromazine) also lead to akathisia.
The syndrome can also be caused by excessive use of sleeping pills, especially the barbiturates group.
Mental changes towards the development of akathisia are characteristic of patients with opium and cocaine addiction. These drugs are strong poisons that depress nerve conduction in the brain. The list of substances that provoke akathisia also includes drugs from the amphetamine group, methylphenidate.
Long-term systematic consumption of alcohol has a detrimental effect on nerve endings and inhibits the functions of the subcortex of the brain. Neuromediation is disrupted, which negatively affects the functioning of the entire central nervous system.
- Parkinsonism, other mental disorders.
Both primary and secondary parkinsonism can cause akathisia. Science has not yet established exactly how great the role of concomitant medication is in treating the disease. The influence of two factors is likely to occur simultaneously. Chronic restlessness also occurs among patients with schizophrenia, anxiety and affective disorders.
Factors that increase the risk of chronic restlessness:
- genetic predisposition; in particular, science associates it with the gene of the first chromosome DRD2;
- various pathologies of the central nervous system;
- suffered traumatic brain injuries;
- dementia.
In addition, cases of akathisia are possible with abrupt withdrawal of psychoactive substances. An example would be someone waking up from anesthesia. Stopping treatment with antipsychotics and antidepressants can also cause a similar effect.
Characteristic symptoms
The picture of the disease consists of two characteristics: subjective (the patient’s internal sensations) and objective, or motor (excessive motor activity).
At the first stage, restlessness manifests itself in leg movements. A person cannot sit, stand, or lie quietly. He stomps, shuffles, jumps up, walks, shakes his leg, fidgets, tosses and turns from side to side.
Symptoms then spread to other parts of the body. This manifests itself in antics, jumping, darting glances, head shaking, constant meaningless, aimless movements.
The subjective component of the syndrome is expressed in anxiety, a painful feeling, often for no apparent reason. When complaining to a doctor, it is difficult for such a person to describe in words his internal sensations. They can be both sensory and psychological.
The patient may feel a burning sensation, itching, aching inside the muscles and joints, but the diagnosis does not confirm any diseases of the musculoskeletal system. A person complains of psychological discomfort coming from within, a vague anxiety that forces him to move somewhere.
The calmer the body position, the greater the feeling of anxiety.
In the later stages, the patient's character changes. He becomes irritable, suspicious, ingratiating. The pathology causes sleep disturbances in him. If akathisia is caused by an underlying mental disorder, then if left untreated it will only get worse.
Classification of the disease, forms
Based on the prevalence of symptoms, akathisia is divided into the following forms:
- Motor akathisia. Patients experience movement disorders without anxiety. But at the same time they constantly move, mark time, walk, jerk their legs, etc. For example, a patient may stomp his foot in place without noticing, even when writing something.
- Mental form. Restlessness is almost reduced to zero, but subjective sensations are a source of discomfort. Most often it is constant anxiety, restlessness, and strong internal tension.
- Sensory. A person feels itching, muscle contraction, and other unpleasant sensations (usually in the lower extremities). He constantly scratches himself, rubs his knees, changes his position, etc.
Classic akathisia combines all of the above symptoms. The patient's complaints usually coincide with observation data of his behavior. The patient experiences a feeling of anxiety for no reason, which pushes him to move in an unknown direction and for what reason.
There is also a classification based on etiology, i.e. origin of the syndrome:
- Parkinsonian akathisia;
- Iatrogenic;
- Withdrawal symptoms;
- Caused by psychoactive substances;
- Post-stroke;
- Spontaneous (due to mental disorders).
The disorder varies in the timing of symptoms:
- Acute form. Develops in the first days, sometimes hours after the influence of a provoking factor. For example, a patient is taking antipsychotics, and the dosage of the drug has been increased. In such cases, reduce the dose or replace the drug with another. The syndrome gradually subsides after this.
- Chronic form. It is observed in a quarter of patients treated with antipsychotics. Occurs after taking the medicine for a month or more. It also gradually regresses after changing the drug.
- Late form. Symptoms of the disease appear months or years after the onset of exposure to the substance. In this form, discontinuation of the drug causes a deterioration in the condition. A person gets better only with an increase in dose, but not for long. Such akathisia may persist for the rest of life or gradually disappear after stopping taking the substance.
- Withdrawal syndrome. Familiar to any person who has quit drinking, smoking, using drugs, taking potent medications such as antipsychotics, sleeping pills, etc. It appears during the first two weeks after stopping taking the substance, but may persist longer (4-7 weeks). If withdrawal akathisia does not disappear after two months, a late form of the syndrome cannot be ruled out.
Basic principles of diagnosis
Neurologists and psychiatrists are involved in the diagnosis and treatment of akathisia. Making a diagnosis is often difficult due to dementia, an unclear description of subjective sensations by the patient himself, and his lack of understanding of what is happening.
In addition, at the very beginning of the pathology, patients can still control hyperkinesia through willpower: do not jump up, do not swing their legs, etc. Some patients have a negative attitude towards doctors and the treatment process.
In practice, there are cases when such negativism is the only visible manifestation of akathisia.
Diagnostics today uses many modern methods: MRI, CT, MSCT, EEG, REG of the brain. However, they allow us to exclude other diseases, nothing more.
The doctor needs to interview the patient about the sensations he is experiencing and observe the patient’s behavior.
Since the patient may hide symptoms and restrain movements, it may be necessary to interview relatives.
The patient's condition is assessed using a special Burns scale, which includes three points each to characterize the subjective and objective components.
The degree of a person’s worries about the manifestations of his disease is separately assessed.
Akathisia should be distinguished from other conditions and pathologies with increased motor activity (anxiety, psychomotor agitation, Tourette's syndrome, etc.).
Treatment of akathisia
The therapeutic method is prevalent in the treatment of the disease. If acasative syndrome is caused by taking medications, you need to immediately change the dosage or replace the drug.
Patients are prescribed magnesium drugs, which, depending on the etiology and symptoms, are combined with medications from other groups. It can be:
- Beta blockers;
- Central anticholinergics;
- Antiadrenergics;
- GABAergic drugs;
- Dopaminergics;
- 5-HT-2 blockers.
With timely treatment, the prognosis is good. The course of treatment for withdrawal syndrome lasts about three weeks, for other forms – up to 8 months. The patient's relatives need to carefully monitor his condition.
Akathisia and insomnia
Symptoms of akathisia prevent the patient from sleeping peacefully. Patients experience constant difficulty falling asleep, roll over in bed, and have restless thoughts entering their minds.
There are known cases of awakening from sleep in order to walk around the house or street. Constant lack of sleep at night leads to daytime sleepiness. After some time, “confusion between day and night” occurs, i.e.
sleep time inversion.
If you take sleeping pills to combat insomnia, they do not always help and may even worsen the problems. The patient spends a lot of strength and energy on meaningless movement, without restoring strength through night sleep. Exhausted, some people see no way out and, in desperation, try to commit suicide.
Prevention
The best prevention of chronic restlessness syndrome is not to take psychotropics, sleeping pills and antidepressants. To do this, you need to lead a lifestyle so as not to bring your body to a state that requires taking them. Try to avoid stress if possible, learn to experience it adequately, perceive life philosophically, and look at it positively.
In cases where drug correction of pathologies is still necessary, it is important to use medications rationally, avoiding overdoses. Experts try to prescribe medications with the least extrapyramidal potential, starting with small doses.
Do not under any circumstances self-medicate for insomnia, depression, chronic fatigue syndrome, vegetative-vascular dystonia and other unpleasant syndromes. Wrong choice of drug without taking into account general medical history and drug interactions can lead to serious consequences.
It sounds like a hackneyed truth, but it’s worth saying again about the benefits of a healthy lifestyle . First of all, you need to completely give up alcohol and drugs.
A person who has nothing to give up will never experience akathisic drug withdrawal syndrome.
Relatives and friends of a person at risk need to provide him with all possible support. It is also extremely important to set this person up only for positive changes.
Source: https://onevrologii.ru/sindromy/akatiziya
Diagnostics
Akathisia usually develops within the first 2 weeks of antipsychotic therapy. Patients describe feeling restless with a desire to move. Objectively, the manifestation of anxiety through stimulation, rocking, and shifting of position is observed. People often feel overwhelmed and uncomfortable.
To assess the severity of symptoms, health care providers use tools such as the Barnes Akathisia Rating Scale (BARS). It evaluates objective and subjective criteria. There are no adequate laboratory or radiological tests to aid diagnosis. Clinical observation should be relied upon.
Internal anxiety often causes extreme anxiety and dysphoria in a person. In chronic cases, akathisia is associated with a high risk of self-harm or suicidal behavior. The doctor should obtain a history of depression, anxiety, and suicidal thoughts.
Accurate assessment is problematic because it is difficult to distinguish from many disorders with similar symptoms. In a study of movement disorders caused by antipsychotics, akathisia was found in only 26% of patients.
The main distinguishing feature is a feeling of inner restlessness. May be mistaken for agitation secondary to psychotic symptoms, mood disorders, antipsychotic dysphoria, restless legs syndrome (RLS), insomnia, drug withdrawal states, tardive dyskinesia, and other neurological and medical conditions.
Sometimes, the controversial diagnosis of pseudoakathisia is made, as noted by Mark J. Garcia. In his article discussing it among adults with severe to profound mental retardation, he describes pseudoakathisia as “including all the symptoms of abnormal movements seen in akathisia, but without the feeling of restlessness.”
Akathisia caused by neuroleptics
Neuroleptics are a group of psychoactive substances that have a depressant effect on the nervous and mental systems. Long-term use or incorrect dosage may cause side effects and complications. One of the consequences is akathisia.
This is a pathological condition characterized by causeless anxiety, involuntary motor activity with a regular need to change positions. Akathisia is a complex term borrowed from the Greek language, which literally translates as “restlessness.”
Description of the problem
Akathisia caused by neuroleptics is accompanied by internal restlessness and a craving for constant physical activity, which helps to smooth out the feeling of internal restlessness and discomfort.
The term was first introduced in 1901 even before the advent of antipsychotic drugs. However, after the advent of antipsychotics, the number of patients with the clinical syndrome increased significantly.
In most cases, akathisia from antipsychotics is combined with depressive disorders.
The disease can occur in acute and late forms. Acute akathisia is diagnosed in 5-50% of patients within 7 days of starting to take an antipsychotic or when its dosage is increased. As a rule, with a decrease in daily volume or withdrawal, a gradual regression of the pathology occurs.
With late akathisia, symptoms appear 3-12 months after the start of a therapeutic course at stable dosages. This form of complication also occurs when an antipsychotic is discontinued or the dosage is reduced.
In this case, the clinic disappears when the previously consumed volumes are resumed. The late form of the pathological condition lasts a long time and can become lifelong, since even with the abolition of the antipsychotic, the symptoms go away slowly.
Tardive akathisia is diagnosed in 30% of patients.
The most terrible consequence is irreversible mental degradation
It is necessary to recognize addiction as early as possible and begin to treat it.
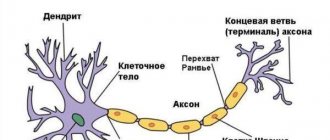
The development of akathisia is associated with dysfunction of dopaminergic pathways responsible for feeding certain areas of the brain. The formation of the pathological condition is based on a disturbance in the serotonin networks, noradrenergic, opioid and GABA systems and neurokinin receptors. Such transformations provoke oxidative stress in neurons.
A decrease in dopaminergic dynamics of the central nervous system leads to the inclusion of adaptation mechanisms to changes. One of these processes is an increase in the level of noradrenergic activity of the central nervous system, which leads to an increase in the secretion of adrenaline by the adrenal glands.
An increase in the neurotransmitter in the systemic bloodstream leads to an increase in the psycho-emotional state, the appearance of anxiety and fear.
Patients at risk include those with a history of:
- treatment with high dosages of antipsychotics or a sharp increase in dosage
- therapy with long-acting or atypical antipsychotics
- mood disorders
- mental disorders
- oncology
- pregnancy
- organic brain lesions
- chronic alcoholism
- deficiency of iron, magnesium
Also at risk are women, elderly patients and children.
Symptoms
A characteristic symptom is an internal feeling of restlessness and restlessness, which causes the need to move. The clinical picture of akathisia is accompanied by a sensory and motor component.
Sensory signs include unpleasant sensations of internal activity that cause the patient to move. At the same time, it is impossible to cope with motor excitation. Sensory symptoms can be general or somatic. The first group includes:
- alarm
- internal tension
- increased irritability
- causeless fear
- inability to relax
- sleep disturbance, worsening of the process of falling asleep, insomnia
The somatic clinic is difficult to convey in words, so problems often arise with diagnosing the condition. Somatic sensory symptoms include:
- heaviness and tingling in the legs
- feeling of twisting, twisting in the joints
- muscle aches
- burning, itching in muscles and joints
The motor component of akathisia is accompanied by pathological motor activity.
For example, patients may cross their legs, shuffle, march in place, stroke their face, tap their fingers, or unbutton/fasten a button.
Mild akathisia is characterized by erased symptoms, so it may be outwardly invisible to others. In this case, the patient is able to suppress external motor signs through willpower.
Consequences
Severe akathisia causes severe discomfort and, as the condition progresses, can cause a feeling of hopelessness, which leads to the formation of depressive disorder and the appearance of suicidal thoughts. Even mild akathisia is unpleasant and often forces the patient to stop taking the drug on his own. If the medication is abruptly discontinued, there is a risk of developing withdrawal syndrome and depression.
Akathisia caused by neuroleptics can aggravate the course of the disease for which therapy was carried out and provoke psychopathic symptoms and psychosis. In this case, anxiety increases, thinking and behavior are disrupted. Possible hallucinations, delusions, depressive or manic symptoms. The risk of harm to yourself and others increases.
Diagnostics
Akathisia is difficult to diagnose because anxiety, restlessness and other signs may be mistaken for psychosis, depression or signs of a medical condition. The inability to make a correct diagnosis leads to an increase in the dosage of the antipsychotic drug, which aggravates the course of akathisia.
Due to incorrect diagnosis of the root cause of the pathological condition, some specialists prescribe anti-anxiety drugs that do not help cope with the disease, but only mask it.
Abnormal motor activity may also be misinterpreted. Instead of a diagnosis of akathisia, the patient may be given dyskinesia or other psychoneurological pathologies.
In this regard, differential diagnosis comes to the fore.
Currently, there are no objective neurophysiological, neuroimaging or laboratory methods that can confirm or refute the presence of akathisia in a patient or help in its diagnosis, so the clinician should rely only on their own judgment and experience. Timely and correct diagnosis of akathisia and a more objective assessment of the degree of its severity are facilitated by the use of formalized scales, such as the Burns Akathisia Scale.”
When the first signs of akathisia appear, the antipsychotic drug should be discontinued, its dosage reduced, or replaced with other drugs. Therapeutic tactics are selected individually, based on each clinical case.
If symptoms of akathisia persist despite discontinuation or reduction of the antipsychotic dosage, the attending physician may prescribe a course of medications:
- Antihistamines and anticholinergics have a sedative effect, but do not suppress the activity of the nervous system. Helps reduce excitability and restore sleep. Often prescribed for a combination of akathisia and parkinsonism.
- Tranquilizers can reduce anxiety, excitability, and insomnia.
- Anticonvulsants help reduce feelings of anxiety and restlessness. They are highly effective, but can cause psychological dependence.
- Beta blockers to relieve anxiety and other side effects of antipsychotic medications.
Vitamins B, C, E, omega-3 fatty acids, as well as hormonal drugs are used as auxiliary therapy. If treatment fails, opioids and electroconvulsive therapy may be used.
conclusions
Akathisia develops as a complication during treatment with high dosages of antipsychotics, use of incorrect amounts of the drug, or its withdrawal. The condition is difficult to diagnose, which leads to difficulties in making a diagnosis.
To eliminate symptoms, it is enough to stop taking the antipsychotic or reduce the dosage. If this approach is ineffective, drug therapy is used. To prevent side effects of antipsychotics, you should not prescribe the drug yourself and adjust its dosage.
Antipsychotics are heavy drugs that can lead to complete depression of motor and cognitive functions.
Bibliography:
Source: https://nasrf.ru/baza-znaniy/spravochnik-zabolevaniy/akatiziya-vyzvannaya-neyroleptikami
Classification
Acute
Chronic
| Pseudoakathisia
Late akathisia
Returnable
|
Clinical systematization
Akathisias are also classified according to the predominance of certain symptoms into the following types:
Treatment
Antipsychotic-induced akathisia is managed by reducing the dose of the offending agent or switching to an alternative drug. Beta blockers such as propranolol and benzodiazepines have historically been used to treat akathisia.
Find out more Withdrawal syndrome - symptoms, how to overcome them
Anticholinergic agents such as benztropine are used in the presence of concomitant pseudoparkinsonism.
Mirtazapine may also be used. Low doses of mirtazapine have been found to be as effective as beta blockers. May be considered as first line therapy. Caution is advised with this drug as there are reports that high doses of mirtazapine worsen akathisia.
When using beta blockers, clinicians should be aware of the risk of bradycardia and hypotension.
Research shows that benzodiazepines, propranolol, and anticholinergics are helpful in the treatment of acute akathisia. Less effective for chronic. A gradual reduction in the dose of antipsychotic drugs as an initial response to drug-induced akathisia helps.
Vitamin B 6 is effective for treatment.
Additional pharmacological interventions that have anti-akathisic effects (especially in neuroleptic-induced akathisia) include β-adrenergic antagonists (propranolol), benzodiazepines (lorazepam), anticholinergics (benztropine), serotonin antagonists (cytagonine).
Diagnostic measures
Diagnosis and treatment of akathisia is the task of a neurologist. To make a diagnosis, no instrumental studies are needed; the doctor only needs a visual examination (that is, external motor manifestations), anamnesis (antipsychotic therapy) and patient complaints.
However, diagnosing the pathology is significantly complicated by the fact that the patient is not able to explain what is happening to him. To accurately describe a patient's condition, doctors use the Burns scale.
Pathophysiology
The pathophysiology of akathisia is poorly understood. Extrapyramidal side effects, especially acute dystonia and pseudoparkinsonism, are thought to be caused by an imbalance of dopamine and acetylcholine in the nigrostriatal pathway of the brain. Due to blockade of dopamine type 2 receptors.
Dystonia and pseudoparkinsonism are eliminated by concomitant anticholinergic agents such as benztropine. Akathisia occurs with antipsychotics that block dopamine type 2 receptors.
Does not respond to anticholinergic agents as strongly as dystonia, pseudoparkinsonism, suggesting an alternative pathophysiological mechanism.
Risk factors
A high risk of developing akathisia caused by neuroleptics or therapy with other antipsychotic drugs is present in patients of elderly or young age, with dementia, a history of neurological, anxiety or affective disorders, oncological pathologies, brain injuries, during pregnancy, the presence of a genetic predisposition, lack of magnesium and iron , high dosages of medications taken or a combination thereof.
In addition, other factors and conditions can cause the syndrome:
Forecast
The prognosis is good if the condition is recognized and the drug causing it is stopped. If the disease is not treated, it can lead to suicidal ideation. May cause disability if not recognized. Many people with the disease develop severe anxiety and dysphoria.
In most cases, akathisia occurs from the use of antipsychotic drugs. Once a movement disorder has begun, treatment is not always easy. Stopping the drug is not always the solution, as patients rely on medications to treat the underlying disorder.
It may take several months for the disorder to go away. There are case reports indicating that movement disorder increases the risk of suicide. Therefore, all patients should be closely monitored and the family should be made aware of the possibility of suicide. (Level V)
Watch a video about the features of the disorder
Preventive measures
Prevention of the disease involves limiting the use of typical antipsychotics, in particular in the presence of contraindications (for example, patients with severe affective disorders).
Before prescribing antipsychotics, the patient should be carefully examined, since inadequate therapy can cause extrapyramidal disorders. When a patient takes antipsychotics, he should not only be examined, but also be under the constant supervision of a doctor, because even a slight increase in the dose can lead to akathisia. Both the patient and his relatives can prevent this process, and at the slightest manifestation of the disease, visit a specialist in order to exclude the development of akathisia.
Neuroleptics quite often lead to changes in consciousness, that is, they cause the opposite effect (increase excitability), and therefore treatment with such drugs should be controlled, and the dosage should be as precise as possible.
Data
This is a movement disorder that occurs from the use of antipsychotic drugs. The main movement disorders caused by antipsychotic agents are: acute dystonia; pseudoparkinsonism; tardive dyskinesia. Rarely occurs with antidepressants.
May appear soon after starting antipsychotics or when the dose is increased.
Akathisia is known to be associated with calcium channel blockers, antiemetics, antivertigo drugs, and sedatives used in anesthesia. Observed after cocaine abuse. The condition can be acute or chronic, with symptoms often lasting many months or even years.
By Jason Patel; Philomena Y. Galdikas; Raman Marwaha.
Complications
Akathisia very often becomes the reason for the patient to refuse treatment due to a negative attitude towards the procedures. Due to restlessness, the patient simply cannot carry out the entire necessary range of therapeutic measures. The syndrome very often provokes depression, aggressive behavior, and suicidal thoughts. Such patients may even pose a danger to people around them. Sometimes patients try to help themselves on their own: to relieve all manifestations of the pathology, they begin to abuse alcohol and smoking, which over time leads to the development of addictions, but in no way to the disappearance of the pathology.