Symptoms of vascular dementia
Stroke is one of the most insidious and dangerous diseases, the consequences of which can be extremely severe.
One of them is dementia, when a person loses the ability to think and make decisions. The reason for such changes is the destruction of brain vessels in areas responsible for mental activity. Dementia can develop suddenly; the disease occurs in 10-40% of people who have had a stroke. The cause of dementia can be either hemorrhagic or ischemic stroke. If in the chronic form dementia manifests itself gradually, then after a cerebral hemorrhage it occurs suddenly. Before an attack, a completely adequate person turns into a helpless child. Typically, such consequences are observed in people from 50 to 65 years old, since a stroke damages not only parts of the brain, but the circulatory system.
Factors have been identified that influence the development of dementia after a stroke, when the patient’s body is weakened and unable to resist.
These factors are:
- diabetes;
- advanced atherosclerosis;
- hormonal imbalance;
- arterial hypertension;
- heart failure.
Not only existing diseases can become the impetus for the development of dementia. This list also includes bad habits: alcohol, smoking. Poor nutrition also has an effect, since fatty foods negatively affect the circulatory and cardiac systems. Doctors also name a reason such as a low level of intelligence; a highly developed person enters childhood more slowly.
Vascular dementia develops as a result of impaired blood flow in the brain, and this is similar to stroke. It often develops after a stroke. In other cases, the disease is the result of multiple “silent” microinfarcts in the brain. Individually they do not produce symptoms, but over time they overlap each other.
The main risk factor for the disease is age. Vascular dementia is most common in older people. Other conditions that increase your chances of getting sick:
- diabetes;
- smoking;
- high blood pressure;
- unhealthy diet: lots of animal fats, few fruits and vegetables;
- excess weight;
- lack of physical activity;
- love of alcoholic drinks;
- atherosclerosis;
- systemic lupus erythematosus;
- temporal arteritis;
- history of strokes and heart attacks;
- atrial fibrillation.
The best prevention of vascular cognitive impairment, Alzheimer's disease, stroke, heart attack and other cardiovascular diseases is to eliminate these risk factors and lead a healthy lifestyle.
Characteristic signs of the disease:
- Memory problems. The patient cannot recognize familiar faces, does not remember what he did today, and may get lost in his own home, on the way to the store.
- Difficulty performing usual actions. For example, an avid fisherman cannot remember how to use a fishing rod. A person who has worked as a driver all his life does not understand what to do next when he finds himself behind the wheel of a car.
- Impaired concentration. A person cannot concentrate on anything and is periodically in a state of confusion.
- Problems with thinking. The patient cannot make a decision for a long time, is unable to organize his thoughts and plan actions.
- Disorders in the emotional sphere. A person, for no reason, in an inappropriate situation, begins to cry or laugh.
- Speech problems. It may be difficult for the patient to find words, his speech becomes poor.
- Gait disturbance. She becomes insecure.
- Loss of bladder control. Frequent urge to urinate, urinary incontinence.
- Hallucinations and delusions.
The early stage of vascular dementia is signaled by symptoms such as impaired memory for recent events, changes in speech, and difficulty orienting oneself in a familiar area.
There are two specific forms of the disease:
- Post-stroke dementia develops after a stroke and has a clear connection with it.
- Mixed dementia is a condition in which vascular cognitive impairment is combined with other forms of dementia, most often Alzheimer's disease.
Course of the disease
Most often, senile vascular dementia occurs in stages. For some time the patient's condition stabilizes, then deterioration occurs. Gradually, more and more areas of the brain are involved in the process.
Sometimes the disease occurs acutely, and the disturbances are very pronounced from the very beginning. This usually occurs after a severe stroke. If the brain stroke was mild, or it was a mini-stroke, cognitive disorders increase gradually, slowly. In general, the course of dementia is divided into three stages:
- Early stage. At this stage, relatives often do not notice that their loved one is sick. Forgetfulness occurs, a person often loses things, cannot always tell what time it is, and gets lost in familiar places. From time to time, difficulties arise with the selection of words during a conversation.
- Middle stage. A person does not remember recent events, does not recognize familiar people, experiences serious difficulties in communication, gets lost in his own home, asks the same questions every now and then, and needs outside care.
- The last (launched) stage. The patient completely ceases to orient himself in time and space. He cannot recognize his relatives, cannot take care of himself and perform the simplest actions. Many patients change their behavior and become aggressive.
Post-stroke dementia belongs to the class of vascular dementias. This is a disease characterized by decreased cognitive function and neurological disorders due to acute or chronic cerebral circulatory disorders.
Stroke in a patient with dementia is the second most important cause of development of mental impairment. Usually people over 70 years of age are affected.
Vascular dementia occurs due to the following strokes:
- Extensive lacunar stroke in dementia. The pathology is characterized by damage to small vessels and subsequent damage to the white and gray matter of the brain.
- Multiple cerebral infarction. The condition occurs when medium-sized arteries and veins are affected.
- Single heart attack. It is characterized by an acute circulatory disorder in a certain area of the cortex or subcortical structures of the brain.
- Binswanger's disease. The pathology appears due to damage to small arteries and veins against the background of difficult-to-control hypertension.
The outcome of any stroke is insufficient blood circulation to the entire cortex or individual areas of the brain. Due to ischemia and hypoxia, brain cells die and atrophy over time. This leads to mental and neurological disorders.
Dementia has 4 degrees:
- Easy. It is characterized by minor social maladjustment and compensated disorders of cognitive functions. Such patients maintain their lifestyle: they continue to take care of themselves, go to the store, cook and do household chores. However, professional work is limited.
- Average or moderate. The ability to self-care is impaired, there are severe cognitive impairments.
- Heavy. The patient needs outside supervision by relatives. Patients with severe dementia cannot care for themselves and need help with nutrition and personal hygiene.
- Extreme. It is characterized by profound disorders of the cognitive sphere and neurological functions, accompanied by the disintegration of the personality core, and negative or deficient mental symptoms are formed.
Based on syndromes, dementia is divided into:
- Lacunar option. Individual mental processes are affected while the core of the personality is preserved. For example, the patient may not remember where he was yesterday, but emotions, compassion for loved ones, and the motivational sphere are preserved.
- Total option. Characterized by a disorder of most mental processes and personality disorders. It is accompanied by the disintegration of the core of personality: patients forget who they are, their own place of residence and even their own name.
Dementia after a stroke is characterized by a typical clinical picture for dementia, which develops sequentially.
After a stroke, the clinical picture is characterized by nonspecific mental disorders:
- Neurosis-like conditions: neurasthenia (weakness, irritability, headaches), depressive syndrome, disturbance of emotional reactions (temper, difficulty in maintaining affect).
- Exacerbation of hidden or less obvious personality traits. Habitual neatness can turn into extreme pedantry.
- Nonspecific disturbances of mental processes: decreased memory capacity, increased distractibility.
As atrophy progresses, the clinical symptoms intensify and new symptom complexes appear. Thus, mnestic activity (memory) suffers the most. Patients forget recent events, such as what they bought in a store or where they were. Over time, the memory disorder deepens: patients forget events of youth and adulthood.
Thinking is disrupted. It becomes viscous and rigid: patients have difficulty switching from one topic to another, and remember grievances for a long time. Also, thinking becomes thorough and detailed: patients find it difficult to separate the primary from the secondary, the main from the secondary.
In the later stages or extremes of dementia, acute psychotic states occur, accompanied by hallucinations, delusions and impaired consciousness. Delusions mainly have a paranoid component: patients claim that they were deceived somewhere, that they want to steal. At night they always check the door locks 5-10 times.
Dementia after a stroke is treated comprehensively:
- Ensuring patient safety. To do this, the degree of ability to work and the possibility of independent maintenance is determined. The problem is that the patient may simply get lost and not make it home, or lose the key to the front door. For this purpose, domestic workers, caregivers or private home health services are hired.
- Formation and organization of everyday life. Thus, patients are recommended to keep a diary, schedule or other methods of self-organization, where they could note taking pills, write down thoughts and upcoming events.
- Drug therapy. It is used in psychotic conditions when the patient poses a threat to his life and the lives of those around him.
Course of the disease
Vascular dementia after stroke
In the modern world, the third place in mortality after cancer and diseases of the cardiovascular system is occupied by acute cerebrovascular accident (stroke). Surviving patients recover physical and mental activity in 20% of cases; in the remaining 80%, the risk of developing dementia in the post-stroke period is incredibly high.
Statistical data
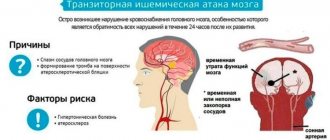
According to epidemiological data, there are 3 cases of stroke per 1000 people in the Russian Federation. The indicators do not take into account situations with an erased clinical picture or minor manifestations - microstroke (transient ischemic attack), due to the fact that patients stop the attack on their own at home.
With a stroke, it is natural to damage the brain substance with typical cognitive impairments (speech aphasia, dysgraphia, dyslexia and others).
If the subcortical structures are affected, it is customary to say that this is dementia after a stroke; the prognosis and treatment directly depend on the degree of prevalence of the pathological focus and the time of emergency medical care.
There is a phenomenon of disconnection - a disruption in the transmission of nerve impulses and communication between brain structures.
The risk of dementia after a cerebrovascular accident (CVA) increases to 70%, the probability of a repeat cerebral catastrophe within the first five years is 25%. Post-stroke cognitive impairment and dementia, which are diagnosed in the first three months after the lesion, are considered true manifestations.
Important! According to the observations of scientists, post-stroke dementia correlates with the location of the cerebral stroke, the degree of damage, the age and gender of the patient. It has been noticed that the risk of dementia in men is higher than in women.
According to Henon, the frequency of dementia after stroke is 20%, and the frequency in the world is 31%, which proves the presence of dementia in 11% of cases even before the stroke. Based on the meta-analysis, it can be concluded that on average the risk of dementia after acute cerebral vascular accident ranges from 7% to 41%.
The relationship between stroke and dementia
Traditionally, clinical manifestations after the onset of cerebral catastrophe are associated with neurological deficits.
In practical terms, they are given more attention during therapy to avoid the risk of disability and to improve the patient’s quality of life.
However, focal changes are almost always combined with mental and cognitive disorders. Additional domestic, social and professional adaptation is required.
Vascular dementia after a stroke is caused by disruption of normal blood flow and blood supply to the blood vessels. “Strategic” areas of the brain suffer from a lack of nutrients, vitamins, macro- and microelements. A cause-and-effect relationship proving a high risk of dementia after stroke:
- young people (up to 40-45 years old) after a single or multiple case of vascular accident, where the likelihood of Alzheimer's disease is reduced to zero;
- cognitive properties were preserved before stroke and were impaired immediately after the pathology, in addition, they continue to progress over the next 3-6 months;
- according to the results of a clinical examination, magnetic resonance or computed tomography, the lesion is located in a strategically significant area (areas of the brain under the cortex);
- a history of vasculopathy was diagnosed.
The risk of developing dementia depends on many predictors.
Risk factors for dementia: age, lifestyle, gender, low level of education, untreated hypertension and diabetes, heart and vascular diseases.
In addition, the risk of post-stroke dementia increases with repeated cerebral crisis, severe and extensive damage, and localization features affecting extremely important structures.
Important! In most cases, there is a combination of risk factors and increased mutual influence, but not their summation.
Dementia in the elderly after a stroke at the age of 60-70 years develops in 16-17% of cases, in patients aged 70-80 years the risk of complications is 29-30%, over 80 years - 37-40%.
Mechanism of development of cognitive impairment
Dementia and stroke inextricably accompany each other in varying degrees of clinical severity. There are two main pathogenetic links in acute cerebrovascular accident:
- As a result of blockage of the lumen of a blood vessel by an atherosclerotic plaque, thrombus or atherosclerotic masses, a lack of blood appears in the brain and an ischemic stroke is formed, vascular-type dementia in 30% of cases.
- When the wall weakens, a protrusion (aneurysm) appears, and arterial or intracranial pressure increases, the risk of hemorrhagic stroke with rupture of the hemovascular membrane is high.
Dementia after hemorrhagic stroke or ischemic cerebral infarction has an extremely high risk when more than 50 ml of brain volume is affected. Cognitive disorders manifest themselves acutely, noticeable in the first 3-6 months. The development of changes after six months can be attributed to another type of dementia.
Clinical relevance
After a single stroke, cognitive impairment may not change in severity, but in some cases there is a slow decline. A step-like course is typical and often has the same localization, severity and etiological factor.
People over 60 years of age may experience so-called “silent” strokes located in the white matter of the brain.
Etiologically they manifest themselves against the background of a sharp decrease in blood pressure (collapse), diseases of the heart and coronary vessels, and other severe somatic pathologies.
It is perceived as senile dementia, clinically manifested as forgetfulness, inability to dress independently, prolonged mindless walking, inability to recognize a close relative the first time, etc.
When dementia occurs after a stroke, how long they live is directly related to repeated episodes of acute cerebral circulatory disorders. High mortality with recurrent stroke after 3-6 months. The risk of death is in every 2-3 patients.
Flow options
Epidemiological observations show that the risk of dementia increases with recurrent stroke. Post-stroke cognitive disorders are heterogeneous. The heterogeneity of neurological, psychological characteristics and natural dynamics after an acute cerebral catastrophe is noted.
Variants of post-stroke cognitive impairment CauseDescription
| Single stroke | Damage to the so-called “strategic” zones and the sharp development of dementia after stroke are registered only in 5% of cases as a result of a single cause. This rare variant is characterized by neuropsychological characteristics when affecting a certain area:
|
| Decompensation of existing vascular dementia | This type of dementia is most often recorded, accounting for 40% of all cases after a stroke, the prognosis of the disease is relatively favorable. With additional rehabilitation measures, it is possible to maintain vital and cognitive functions. Clinically – slowing of motor speech and mental reactions. |
| Mixed vascular-degenerative lesion | Cognitive functions are simultaneously depressed, and the neurodegenerative process is often difficult to recognize. The mixed variant progresses rapidly, mnestic disorders are noticeable as in Alzheimer's disease (disadaptation, dysmnesia, amnesia, confabulation*), decreased intellectual productivity, apathy. |
*confabulation – replacing memory lapses with fictitious actions.
How to recognize vascular dementia
Behavior after a stroke varies among many patients, some lose practical skills and physical mobility, others become weaker mentally. A combination of different manifestations also occurs. The affected area plays an important role in the formation of symptoms:
- Focus in the cerebral cortex. Slurred speech, loss of practical skills, disorientation in space.
- The lesion is in the subcortex. Inattention, absent-mindedness, poor facial expressions, hysteria, slow and uneven gait, depression.
Sometimes the signs are combined, and the pathology can develop due to existing diseases.
Other symptoms characteristic of dementia after a stroke:
- A person has almost no control over half of his body.
- Urinary incontinence is observed in 30% of cases.
- Loss of intelligible speech, writing and reading skills.
- Progressive sclerosis.
- Agnosia is the loss of the ability to recognize people and objects and evaluate them.
- The patient cannot move on his own.
- Frequent mood swings, depression, tendency to panic attacks.
- The appearance of delusions or hallucinations.
Identifying dementia in the early stages helps preserve identity and make life easier for the patient after a stroke.
Symptoms of acquired vascular dementia
Complications after a stroke can be noticed quite easily. As with other cases of dementia, the person has significant problems with mental functioning, motor skills and memory. It is extremely important to notice the signs of disease development in time in order to begin timely treatment.
The most common symptoms of dementia after a stroke are:
- development of a disorder of human intellectual activity and his thinking;
- problematic orientation in space, because of this the patient can abruptly change the direction of his movement;
- problems with speech, reading and perception of information;
- progressive sclerosis;
- agnosia, a person loses the ability to recognize an object and identify it;
- the patient completely or partially loses the ability to move independently;
- a person’s personality changes dramatically, his mood becomes unstable, frequent attacks of aggression and neurosis are possible;
- the patient ceases to be a full-fledged member of society; a large number of people can cause a panic attack;
- cerebrospinal disease;
- delirium and hallucinations are possible.
It is important to notice the onset of the disease at an early stage of its development, this will help not only to begin timely treatment, but also to make life easier for the patient, because an illness such as dementia significantly affects a person’s personality, simply destroying it.
What diagnostic methods can a doctor prescribe?
To confirm the diagnosis, the patient is also examined by a neurologist and a psychiatrist. A diagnostic examination helps determine the number and location of foci of necrosis.
- Ultrasound, angiography. The condition of the cerebral arteries is determined.
- Electroencephalography.
- General and biochemical blood test.
There is no test or test that can immediately accurately diagnose vascular dementia. With the help of special tests, the doctor can detect dementia in the patient, then he will have to understand its causes. Diagnostics must be comprehensive. It is important for a neurologist to know how the patient’s cognitive impairment manifests itself, whether he has suffered a stroke, heart attack, or suffers from atherosclerosis, arterial hypertension or other cardiovascular diseases.
During neuropsychological testing, the patient is asked to perform some tests and tasks, based on the results of which a number of indicators are assessed:
- How well a person speaks, writes and understands what is said.
- How well can he operate with numbers, perform arithmetic calculations, and determine the date and time?
- How well does he remember new information and learn?
- How well can he plan his actions and implement his plans into reality?
- How does the doctor react to hypothetical situations?
Examination by a neurologist
Before examining a sick person, he will be examined by a neurologist, checking reflexes, movements, sensitivity, muscle strength and tone, vision, touch, sense of balance, and coordination of movements.
Head scan
In order to understand the causes of dementia, your doctor may prescribe the following diagnostic methods:
- Computed tomography can detect traces of strokes, transient ischemic attacks, vascular disorders, and intracranial tumors.
- Magnetic resonance imaging shows approximately the same thing, only, compared to CT, it provides the doctor with even more detailed information.
A blood test for cholesterol and sugar helps in diagnosing the causes of dementia. Sometimes you need to check your thyroid hormone levels and other substances.
Treatment of post-stroke dementia
The medications to be taken by the patient are prescribed by a neurologist and psychiatrist only after a comprehensive examination has been carried out. The most common drugs used are donepezil, rivastigmine, memantine and galantomine.
A person does not take only one type of drug. A specially developed system is used that combines medications.
Mainly:
- psychostimulants that act on the central nervous system, thereby increasing its stability under real loads;
- nootropic drugs, they are taken to enhance mental activity and improve memory. They are also ways to influence uncontrolled aggression, reducing the frequency of its occurrence;
- medications to improve blood supply to the brain, thereby preventing the expansion of areas of necrosis.
- antidepressants and vitamin preparations, which improve the general condition of the patient.
To summarize, we can say that vascular dementia is a very dangerous disease, which is a complication after a stroke. Do not neglect your own health and the health of your family and friends!
First of all, therapy should be aimed at the causes of the disease, which are located in the cardiovascular system. The following goals must be achieved:
- Maintaining blood pressure at an optimal level with antihypertensive medications.
- Controlling cholesterol levels in the blood. To reduce it, statin drugs are prescribed.
- Normalize blood clotting and prevent the formation of blood clots. The simplest measure that doctors prescribe to many patients is taking aspirin daily.
- If the patient suffers from type II diabetes mellitus, it is necessary to monitor blood sugar levels and take special medications.
For the treatment of vascular dementia, the same drugs are prescribed as for Alzheimer's disease. Cholinesterase inhibitors (galantamine, donepezil, rivastigmine) and memantine are used. All patients are prescribed a rehabilitation course, which involves a team of different specialists.
Dementia after stroke
Advice from lawyers:
1. A disabled person of group 1 (dementia after a stroke) requires the service of a notary to certify a power of attorney for his representative (son) to the Pension Department to waive the social package. How much does the service cost in Rostov-on-Don, how to carry out this procedure?
1.1. Hello! With such an illness, it is not a fact that a notary will certify the power of attorney. A notary can be called to your home. Contact a notary. If the notary refuses, then only declare him incompetent and formalize guardianship.
Did the answer help you?YesNo
1.2. Tariffs for services are established by law and when they are provided outside the office, they increase by 1.5 times. Certain categories of the population have the right to count on benefits. These are pensioners, disabled people, WWII participants and some other social groups. For them, the cost of home services is 30-50% of the base price. Call the notaries of Rostov-on-Don and ask about this procedure. Good luck and all the best to you.
Did the answer help you?YesNo
1.3. You need to directly contact the notary and find out all the prices from him, but it is not a fact that the notary will issue a power of attorney in case of this disease.
Did the answer help you?YesNo
Consultation on your issue
8
Calls from landlines and mobiles are free throughout Russia
2. The power of attorney to receive a pension for my mother ends. We received it from Sberbank. Now my mother is a bedridden invalid with dementia after a stroke. Notaries do not certify; it takes a very long time to formalize guardianship. Is there any other way out in this situation) They won’t bring the pension home either, since mom can’t sign for it?
2.1. Hello, Elena! You need to invite a notary to your home in order to issue this power of attorney.
Did the answer help you?YesNo
2.2. From 01/01/2020, pensions and social payments will be credited only to the MIR card. In any case, you need to apply for a card. If the power of attorney is valid, then check with Sberbank whether they can use it to fill out an application to transfer a pension to another bank account linked to the MIR card. They forward the application to the Pension Fund themselves.
Did the answer help you?YesNo
3. Mom has dementia after a stroke. Lives in a purchased communal apartment (owner). The bathroom is in the apartment. The kitchen and toilet are shared. Mom is in a paid clinic. There is a power of attorney to carry out all matters on her behalf. We want to rent out her apartment. The neighbor says to install an electric stove and a toilet. Is this legal? Is this considered a redevelopment? Do we have the right to rent out an apartment on behalf of our mother?
3.1. You have every right.
Did the answer help you?YesNo
Can it be cured?
Modern medicine cannot yet boast of a panacea for dementia; we are only talking about rehabilitation to alleviate symptoms and stop the development of the disease. A remedy has not yet been invented that could slow down the destruction of nerve cells, block the deposits of abnormal proteins in brain neurons and restore tissue damaged by necrosis.
The course of treatment is prescribed comprehensively, according to a specially developed scheme, with a combination of different drugs.
Medicines
It is very important to take medications during this period:
- Psychostimulants. Increases the stability of the central nervous system against possible stress.
- Nootropic substances. Activate mental activity, improve memory, reduce aggression. Provide nutrition to brain tissue. The most common: piracetam and nootropin.
- Antidepressants.
- Vitamins. Help restore lost brain functions.
- Series to improve blood supply to the brain, which prevent areas of necrosis from expanding. Tavegil and Cavinton are most often prescribed.
- Medicines to improve memory. Mamantin has proven itself well.
Physical therapy sessions are also prescribed, which help restore blood circulation and relieve muscle tightness.
Proper nutrition also helps keep the patient in an acceptable condition. Some medical experiments have proven that with the help of products, the development of dementia can even be slowed down.
It is necessary to include in the diet:
- Curcumin. A substance found in curry seasoning. It is believed that Indians are not susceptible to Alzheimer's disease because they consume these spices daily. Curcumin prevents amyloid plaques from developing in the brain.
- Natural antioxidants: vitamins E, C, coenzyme Q 10, lycopene and beta-carotene.
- Vegetables, fruits, legumes, nuts.
- Olive oil.
- Fish or seafood.
- Cottage cheese, kefir, cheese.
- Red wine in modest quantities.
It is important to know that in the early stages of dementia, appetite can be greatly reduced, and in the moderate stages it can greatly increase. Therefore, the patient needs to be fed in small portions.
Treating dementia after multiple strokes
Home»Articles»Treatment of dementia after several strokes
Published: December 16, 2014 at 06:03
The development of multi-infarct dementia occurs with repeated strokes and is a consequence of cerebral embolism. With this condition, signs of arteriosclerosis appear in every part of the cardiovascular system. This includes focal signs, such as increased reflexes, pseudobulbar palsy, extrapyramidal symptoms and extensor reflexes. Moreover, such phenomena are detected more often than in cases of Alzheimer's disease. Multi-infarct dementia is characterized by a pronounced softening of the brain substance, and it is this factor that differs from the characteristics of Alzheimer's disease, which is typical of the predominance of senile plaques.
As usual, the onset of multi-infarct dementia is observed after the age of fifty; earlier cases are rare. Representatives of both sexes are equally susceptible to the disease. There are signs that distinguish dementia from the well-known Alzheimer's disease. This is a stepwise progression, and when examining the somatic condition, signs of arteriosclerosis are detected. Moreover, patients not only complain of poor memory, but there are also somatic complaints; patients are often bothered by headaches, fainting, ringing in the ears, and dizziness.
It happens that transient hemiparesis develops, vision or speech is impaired. At the initial stage of the disease, such disorders can be restored, but over time the process intensifies, making dementia deeper. Multi-infarct dementia is caused by various cognitive impairments. It is known that the strokes that cause it can be lacunar, that is, limited, or extensive. Since localization occurs in different parts of the brain, the severity of dementia is always determined by the size of the affected area. Scientists have found that if the left hemisphere is affected, then dementia is more common. This is not associated with damage to the speech centers.
Neurological disorders in the disease
With multi-infarct dementia, a number of neurological disorders always occur, which appear gradually. The development of the disease occurs against the background of diabetes mellitus, arterial hypertension, widespread atherosclerosis, and coronary artery disease. Typically, a neurological examination reveals focal type disorders. When performing an MRI or CT scan for multi-infarct dementia, multiple cerebral infarcts are detected. That is, for a differential diagnosis with Alzheimer's disease, the basis is the medical history and the results of computed tomography. It should be taken into account that a combination of these two common diseases often occurs.
In the vessels of the brain with age, beta-amyloid protein accumulates, thus developing amyloid angiopathy. Although this condition does not directly lead to dementia, the risk of intracerebral hemorrhage increases. For example, in elderly patients with Alzheimer's disease, arterial hypertension and amyloid angiopathy, the risk of ischemic stroke increases. Among the causes of multi-infarct dementia, experts name not only atherosclerosis, hypertension, but also some diseases that are hereditary. Under their influence, the aging of arterial walls occurs faster than is normal.
Repeated emboli may occur in the heart area, for example from damaged heart valves or from blood clots. As for the symptoms of multi-infarct dementia, in this case, gradual memory loss comes first. When such episodes occur, the patient experiences clouding of consciousness, and other signs of a stroke are also detected. Mostly, patients complain of speech problems, numbness, and weakness. At the same time, there is a gradual but confident degradation of personality, a person’s behavior, his attitude towards people and events around him changes. For example, increased lability is noticeable, tears or laughter are uncontrollable.
Treatment of multi-infarct dementia
Treatment of this type of dementia, although difficult, can achieve good results with adequately selected therapy. In addition, as with most diseases, timely treatment plays a significant role. Diagnosis is made based on physical examination and history. The doctor assesses the existing risk factors for stroke, and among them, arterial hypertension and cardiogenic thromboembolism are of primary importance. Often, a specialist will prescribe an additional neuropsychiatric examination. If the patient has had a heart attack and there is softening of the white matter, this is confirmed by computed tomography.
As a therapeutic option, attention is paid to the active correction of stroke risk factors. Among them are hypertension, hyperlipidemia, and smoking. Doctors prescribe warfarin as a preventative measure against cardiogenic thromboembolism. This is especially true for patients with atrial fibrillation and myocardial infarction. This includes antiplatelet therapy, usually clopidogrel or aspirin. To improve the condition of multi-infarct dementia, patients are prescribed acetylcholinesterase inhibitors.
It is known that life expectancy in multi-infarct dementia is shorter when compared with that in Alzheimer's disease. Mostly, death is caused by cardiovascular complications such as myocardial infarction. If a lacunar status is formed in this disease, then treatment of the resulting arterial hypertension at the stage of multi-infarct dementia is ineffective. However, if the disease is recognized at an early stage and treatment for hypertension is started on time, then the prevention of dementia will be successful.
What is subcortical vascular dementia?
Another name for the disease is Binswanger's disease. It is a subtype of vascular dementia in which the lesions are localized in brain structures located below the cortex. Cognitive disorders include symptoms such as:
- increased fatigue;
- decreased performance;
- headache;
- sleep disorders;
- difficulty pronouncing words and swallowing (pseudobulbar syndrome);
- fecal and urinary incontinence;
- walking disorder (abasia).
Vascular dementia
One type of vascular dementia is post-stroke dementia.
The problem of post-stroke dementia has been especially actively studied over the past two decades. It is believed that a stroke increases the risk of dementia by 4-12 times. In patients over 60 years of age, the risk of dementia in the first three months after a stroke is 9 times higher than in the control group of persons without a stroke. Dementia occurs in 10-17% of patients who have had a stroke and did not have significant cognitive impairment before the stroke. However, stroke can be considered as a direct cause of dementia in only 50% of patients with post-stroke dementia. In other patients, the nature of the cognitive defect and its subsequent progressive course suggests a primary degenerative (usually Alzheimer's) nature of dementia or a combination of vascular and Alzheimer's changes. Such cases are more correctly considered as mixed dementia.
Post-stroke vascular dementia (vascular dementia with acute onset) develops during the first month (but not more than 3 months) after a stroke, usually ischemic; in rare cases, the cause may be massive hemorrhage.
A cause-and-effect relationship between a stroke and subsequent dementia can be considered highly probable in the following cases:
- In young patients in whom dementia occurred after one or more strokes, and the presence of asthma seems unlikely.
- When cognitive functions were preserved before the stroke, they were impaired immediately after it and did not subsequently progress.
- When localizing outbreaks in strategically significant areas.
- When the diagnosis of vasculopathy is confirmed, which itself can be a cause of dementia.
Post-stroke vascular dementia may be associated with the following types of brain damage:
- infarction of the strategic zone of the brain that is most closely related to the regulation of mental functions (angular gyrus, thalamus, limbic structures, frontal lobe, basal ganglia);
- multi-infarction condition;
- intracerebral hemorrhage;
- a combination of infarctions with diffuse damage to the white matter;
- a combination of vascular brain damage and Alzheimer's changes in the brain.
Kushnir G.M. — Doctor of Medical Sciences Professor, Savchuk E.A. - Ph.D. Samokhvalova V.V. - Ph.D.
“Vascular dementia after stroke, development of post-stroke dementia” - article from the Dementia section
In most countries, the main cause of dementia is considered to be Alzheimer's disease and other diseases associated only with the death of nerve cells. However, symptoms of dementia can also be caused by problems with blood circulation in the brain. Such cases are called dementia of vascular origin (origin), or simply vascular dementia.
What is the mechanism of development of vascular dementia?
When blood vessels are damaged in certain areas of the brain, nerve cells do not receive the oxygen and nutrients necessary for their normal functioning, which leads to their death. For some time, the brain copes with compensation for the violations that occur, and they do not manifest themselves externally. But when the potential is depleted, negative changes begin to affect the state of memory, speech and thinking. Against the background of these cognitive disorders, the patient’s behavior also changes, and his independence decreases.
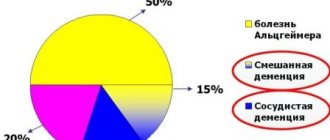
Vascular dementia in its pure form accounts for approximately 10–15% of all cases of dementia in the elderly. However, in addition, cases of mixed dementia are common, which are based on a combination of vascular dementia with Alzheimer's disease. By the way, scientists say that as people age, the risk of being diagnosed with vascular dementia in older people decreases, but the risk of developing Alzheimer's disease, on the contrary, increases.
Therefore, the vascular factor is recognized as especially dangerous in Russia (according to some estimates, up to 50%), where a significant part of the population simply does not live to see the onset of another type of dementia. In addition to Russia, countries in which vascular dementia is quite widespread compared to Alzheimer's disease include the countries of Southeast Asia (Japan, China), as well as Scandinavian countries (Sweden, Finland).
For a long time it was believed that the main cause of vascular dementia was acute cerebrovascular accident (stroke). Stroke occurs due to
blockage of an artery by a thrombus or embolus (ischemic stroke) or
when it ruptures and cerebral hemorrhage (hemorrhagic stroke). Both types of damage lead to irreversible consequences - the death of brain cells deprived of nutrition.
It has been established that a previous stroke significantly increases the risk of vascular dementia. During the first year after a stroke, vascular dementia develops in 20–30% of patients. The likelihood of symptoms appearing and the nature of their manifestation depend on which area of the brain the disorder occurs in.
The size of the affected area is also important. Vascular dementia usually develops when more than 50 ml of the brain is affected. However, if a circulatory disorder occurs in a key area for cognitive functions (this includes, for example, the visual thalamus, hippocampus, prefrontal frontal cortex, and others), then even a smaller infarction can lead to the development of vascular dementia. In other cases (if other areas are affected), movement disorders and other post-stroke complications occur.
Over time, scientists have discovered that vascular dementia is not necessarily associated with acute disorders. It also occurs due to chronic cerebral ischemia - blockage of smaller vessels, which can occur unnoticed by the patient. (This phenomenon is called “subcortical vascular dementia.”
) Today, these disorders are detected thanks to the spread of digital technology and the introduction of neuroimaging methods into practice. The devices make it possible to observe “silent” vascular lesions of the brain, which previously went unnoticed because they did not occur in an acute form (did not lead to a stroke).
Vascular dementia can also develop due to decreased blood flow to the brain. This occurs against the background of acute heart failure, a decrease in circulating blood volume, and a strong decrease in blood pressure. Weakening of blood flow leads to insufficient blood supply in the peripheral zones of the vascular basins and, as a consequence, to the death of nerve cells.
Thus, vascular dementia occurs as a result of two pathogenetic mechanisms: acute cerebrovascular accidents and chronic insufficiency of blood supply to the brain. Sometimes these disorders are combined and reinforce each other, which leads to a more noticeable manifestation of symptoms.
Symptoms of vascular dementia
Typically, a diagnosis of vascular dementia is made if cognitive impairment is preceded by an episode of stroke. Often, accompanying signs are symptoms of focal brain damage: for example, weakening of the strength of the limbs (hemiparesis), differences in the reflexes of the left and right limbs, the appearance of a pathological Babinski reflex.
The cause of vascular dementia is circulatory disorders in the brain. These disorders, as well as associated infarcts (cell death), can occur in different areas of the brain. Therefore, the symptoms of vascular dementia vary significantly in each individual case. We list only the most typical ones.
Dementia caused by damage to the midbrain. manifested by mesencephalothalamic syndrome. Its first manifestations are episodes of confusion and hallucinations. Then the person loses interest in various aspects of everyday life, withdraws into himself, stops caring about his appearance, and neglects personal hygiene. His psychophysical state is usually characterized by increased drowsiness. In some cases, speech is noticeably affected.
A symptom of dementia caused by damage to the hippocampus. It is generally accepted that, first of all, there is a violation of the ability to retain information about current events in memory (distant memories can be preserved).
An infarction in the prefrontal regions of the frontal lobes leads to general apathy of the patient (apathetic-abulic syndrome). The patient behaves inappropriately without realizing it. He repeatedly repeats either his own words and actions, or the words and actions of others.
When disorders are localized in the subcortical zones, voluntary activity is the first to suffer: it is difficult for the patient to concentrate on one object or maintain the same activity for a long time; Problems arise with planning activities, many things remain unfinished. Another symptom is a violation of the skills of analyzing information, separating the main from the secondary.
Among the stable markers of vascular dementia, we also note impaired urination, observed in almost all patients.
Vascular dementia manifests itself not only in the cognitive, but also in the emotional sphere. A general decrease in mood, emotional instability, depression - all these are symptoms of dementia of vascular origin. The patient's self-esteem decreases, self-confidence is lost, and pessimistic forecasts begin to prevail.
NINCDS–AIREN (G.Roman et al. 1993)
- Presence of dementia
- The presence of clinical, anamnestic or neuroimaging signs of cerebrovascular disease: previous strokes or subclinical episodes of local cerebral ischemia.
- The presence of a temporal and cause-and-effect relationship between brain damage of vascular etiology and cognitive impairment.
The cause is cerebrovascular disorders due to multiple or single, cortical or subcortical cerebral infarctions. Depending on the location and size of the ischemic lesion, in addition to dementia syndrome, neurological disorders are also observed, such as hemiparesis, disorders of speech and swallowing, walking and movement, or urination.
Prevention
To avoid relapses of stroke and manifestations of dementia, you need to give up bad habits and establish proper nutrition.
The most important recommendations:
- Select moderate physical activity that is feasible for the patient.
- Monitor blood pressure.
- Find time for mental and intellectual activities.
- Eat foods with low cholesterol levels.
Scientists have compiled a list of natural foods and herbs that help block the development of dementia. If you include them in your diet, the risk of developing dementia after a stroke is significantly reduced.
- Vitamin C. Found in green leafy vegetables and citrus fruits. Helps restore brain function.
- Folic acid. Found in oranges, strawberries, asparagus, peas, papaya.
- Almond. Includes vitamin E. To get the maximum effect, the product should be eaten on an empty stomach, after soaking in water in the evening.
- Sage. Slows down blood clotting, dilates blood vessels, improves blood flow. Relieves attacks of depression and anxiety.
- Ginseng. Helps damaged brain cells recover. You need to drink up to 600 grams of decoction per day; the herb is brewed like tea and left for 15 minutes.
- Milk thistle. The fruits contain seeds rich in silymarin, this substance prevents the loss of connections between brain cells, which manifests itself in dementia. You should take 420 milligrams of extract per day, available in the form of tinctures, tablets or capsules.
- Melissa. Improves the healing of affected brain cells, inhibits the process of memory deterioration, relieves anxiety, and normalizes sleep. Brew like tea: a teaspoon per glass of boiling water, drink 3 servings a day.
- Ginkgo biloba. Contains strong antioxidants that improve memory performance, increase blood flow to the brain, and inhibit the development of dementia. Brew 250 ml of boiling water leaves, 1 teaspoon per serving, drink twice a day.
Although, unlike age-related dementia, post-stroke dementia does not always lead to complete degradation, the risk of disease progression always remains very high. It is possible to avoid such manifestations if you recognize the symptoms in the early stages and immediately consult a doctor. With the help of medications, the patient’s condition can be regulated, keeping it at an acceptable level for existence.
Dementia after stroke: what kind of disease is it?
After doctors manage to stabilize the patient’s position in the intensive care ward, they conduct a comprehensive examination. At this stage, it is difficult to unambiguously diagnose dementia, since the patient’s body is under the influence of severe stress.
Further, during treatment, basic brain functions may be restored, but the risk of developing the so-called. vascular dementia, or post-infarction dementia. The areas of the brain affected by a stroke continue to be destroyed, while the functions they support gradually weaken.
Stages of development and life expectancy
At the first stage, this is expressed in forgetfulness and difficulty concentrating. The person still evaluates himself sensibly and understands that his opportunities are being reduced. Irritability increases, and outbursts of unmotivated aggression appear.
Further, memory weakens and, conversely, false memories arise. The patient accuses others of non-existent actions, and when they try to persuade him, he responds with aggression.
At the last stage of the disease, acute psychosis may develop, accompanied by delusions, hallucinations and severe agitation. In this state, a person poses a threat to himself and others. Living next to him is simply dangerous.
This journey takes varying amounts of time, from several weeks to several years.
How long do people with dementia live? Life prognosis depends on the timely detection of the disease and the presence of concomitant diseases. Many patients, as a result of the received therapy and supportive measures, restore cognitive functions to a sufficient extent and live to a ripe old age.
What should relatives do?
It is very important to recognize signs of developing dementia early. Before a psychotic state occurs, healthcare providers can help. A false model of behavior for loved ones is hushing up the problem, justifying inappropriate behavior with fatigue and past illness, and indulging the patient’s imaginations.
By contacting doctors in a timely manner, the situation can be brought under control.