Babinski's asynergia is a symptom of a disease such as cerebellar ataxia, which is characterized by a disturbance in the functioning of the limbs performing combined movements.
Simply put, asynergia manifests itself in a complete or partial inability to control certain muscle contractions to perform complex motor processes.
The patient is unable to perform several complex movements at the same time. These actions will be divided into several simple ones, performed sequentially one after another.
Such processes include walking, which is very different from the ordinary gait of a healthy member of society. Outwardly, one might think that a person is in a state of alcoholic or drug intoxication, but this is the so-called “drunk” gait of the patient.
In some cases, the patient may experience a tilt of the torso in the direction on which the cerebellum is more affected.
Positive and negative Babinski's sign
The Babinski sign is checked as part of a routine neurological examination. The test does not require any equipment, so it is also used by doctors of other specialties who want to determine the general condition of the patient and make the diagnosis more detailed.
The Babinski sign is examined on both legs of the patient. To cause a symptom on the exposed plantar part of the foot, it is necessary to drag something from the heel to the base of the little toe. The object and pressure should be chosen so that it does not cause pain or damage to the skin, but so that the tester clearly feels the effect of the tester. In young children, using your finger is enough to trigger a reaction.
Babinski's sign in adults should be negative. This means that the reaction to the triggering of the reflex should be a rapid flexion of the sole (down) of all the toes of the irritated foot. This reaction is temporary and should not turn into spasmodically bent fingers.
Some people do not experience movement in response to irritation. Then they say that Babinski's symptom is absent. This condition does not directly indicate a brain disease. This may have another cause, such as loss of sensation in the leg (even in the process of polyneuropathy), destruction of the nerve due to injury, or various types of motor dysfunctions that prevent the patient from moving the fingers. Loss of the reflex can also be caused by paralysis of a limb (such as a stroke).
The positive Babinski reflex is a condition in which, after irritation of the sole of the foot, the toe bends toward the dorsal side of the foot (up). This may also be accompanied by a brief spreading of the other fingers (they rise slightly upward and spread apart so that free spaces appear between them). The symptom occurs unilaterally or bilaterally.
By analyzing the observed response, in combination with other symptoms and reflexes, the doctor can usually determine where exactly the brain damage has occurred and how large the changes are.
Cardiac hypertrophy - what is it?
It is important to know! An effective remedy for normalizing heart function and cleaning blood vessels exists!
... One of the characteristic symptoms of hypertrophic cardiomyopathy is hypertrophy of the IVS (interventricular septum). When this pathology occurs, thickening of the walls of the right or left ventricle of the heart and the interventricular septum occurs. This condition itself is a derivative of other diseases and is characterized by an increase in the thickness of the walls of the ventricles.
Despite its prevalence (IVS hypertrophy is observed in more than 70% of people), it is most often asymptomatic and is detected only during very intense physical activity.
After all, hypertrophy of the interventricular septum itself is its thickening and the resulting reduction in the useful volume of the chambers of the heart.
As the thickness of the cardiac walls of the ventricles increases, the volume of the heart chambers also decreases.
In practice, this all leads to a reduction in the volume of blood that is released by the heart into the vascular bed of the body. To provide the organs with a normal amount of blood under such conditions, the heart must contract stronger and more often. And this, in turn, leads to its early wear and tear and the occurrence of diseases of the cardiovascular system.
Symptoms and causes of hypertrophic cardiomyopathy
A large number of people around the world live with undiagnosed IVS hypertrophy, and only with increased physical activity does their existence become known.
As long as the heart can ensure normal blood flow to the organs and systems, everything proceeds hidden and the person will not experience any painful symptoms or other discomfort.
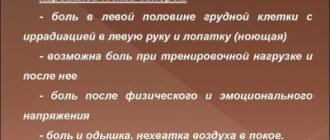
But you should still pay attention to some symptoms and contact a cardiologist if they occur. These symptoms include:
chest pain; shortness of breath with increased physical activity (for example, climbing stairs); dizziness and fainting; increased fatigue; tachyarrhythmia that occurs for short periods of time; heart murmur on auscultation; labored breathing.
It is important to remember that undiagnosed IVS hypertrophy can cause sudden death even in young and physically strong people. Therefore, a medical examination by a therapist and/or cardiologist should not be neglected.
The causes of this pathology lie not only in an incorrect lifestyle. Smoking, alcohol abuse, excess weight - all this becomes a factor contributing to the increase in severe symptoms and the manifestation of negative processes in the body with an unpredictable course.
Babinski's sign in children
Babinski's sign in children should be interpreted very individually. Due to the immaturity of the developing brain and the ongoing myelination of nerve fiber sheaths, Babinski's sign may be positive in healthy children .
Some researchers believe that the occurrence of this reflex indicates the disease in children older than one year, while others push this limit to 3 years.
A positive result should always be interpreted by taking into account all elements of the medical history, clinical status and clinical trial results.
Ventricular septal defect
Ventricular septal defect is a congenital intracardiac anomaly characterized by the presence of communication between the right and left ventricles. A ventricular septal defect is manifested by shortness of breath, retarded physical development, fatigue, rapid heartbeat, and the presence of a “heart hump.”
Instrumental diagnosis of ventricular septal defect includes ECG, echocardiography, chest radiography, ventriculography, aortography, catheterization of cardiac chambers, MRI. For ventricular septal defects, radical (closing the defect) and palliative (narrowing of the pulmonary artery) interventions are performed.
A ventricular septal defect (VSD) is a hole in the septum separating the cavities of the left and right ventricles, the presence of which leads to pathological shunting of blood.
In cardiology, ventricular septal defect is the most common congenital heart defect (9–25% of all congenital heart defects). The incidence of critical illness with ventricular septal defect is about 21%.
The defect is found with equal frequency in newborn boys and girls.
A ventricular septal defect may be a single intracardiac anomaly (isolated VSD) or be part of the structure of complex defects (tetralogy of Fallot, truncus arteriosus, transposition of the great vessels, tricuspid valve atresia, etc.). In some cases, the interventricular septum may be completely absent - this condition is characterized as a single ventricle of the heart.
Ventricular septal defect
Most often, a ventricular septal defect is a consequence of a violation of embryonic development and is formed in the fetus due to disorders of organ formation.
Therefore, ventricular septal defect is often accompanied by other cardiac defects: patent ductus arteriosus (20%), atrial septal defect (20%), aortic coarctation (12%), aortic stenosis (5%), aortic insufficiency (2.5-4. 5%), mitral valve insufficiency (2%), less often - abnormal drainage of the pulmonary veins, pulmonary stenosis, etc.
In 25-50% of cases, the ventricular septal defect is combined with malformations of extracardiac localization - Down's disease, anomalies of the kidneys, cleft of the hard palate and cleft lip.
The direct factors causing disruption of embryogenesis are harmful effects on the fetus in the first trimester of gestation: diseases of the pregnant woman (viral infections, endocrine disorders), alcohol and drug intoxication, ionizing radiation, pathological course of pregnancy (severe toxicosis, threat of spontaneous abortion, etc.) . There is evidence of a hereditary etiology of ventricular septal defect. Acquired ventricular septal defects can be a complication of myocardial infarction.
The interventricular septum forms the inner walls of both ventricles and makes up approximately 1/3 of the area of each of them. The interventricular septum is represented by membranous and muscular components. In turn, the muscular section consists of 3 parts - inflow, trabecular and outflow (infundibular).
The interventricular septum, along with other walls of the ventricles, takes part in the contraction and relaxation of the heart. In the fetus, it is fully formed by the 4-5th week of embryonic development.
If this does not happen for some reason, a defect remains in the interventricular septum.
Hemodynamic disturbances with a ventricular septal defect are caused by communication between the left ventricle with high pressure and the right ventricle with low pressure (normally, during systole, the pressure in the left ventricle is 4–5 times higher than in the right).
After birth and the establishment of blood flow in the systemic and pulmonary circulation, due to a ventricular septal defect, a left-to-right shunt occurs, the volume of which depends on the size of the hole.
With a small volume of shunted blood, the pressure in the right ventricle and pulmonary arteries remains normal or increases slightly.
However, with a large flow of blood through the defect into the pulmonary circulation and its return to the left parts of the heart, volumetric and systolic overload of the ventricles develops.
A significant increase in pressure in the pulmonary circulation with large ventricular septal defects contributes to the occurrence of pulmonary hypertension. An increase in pulmonary vascular resistance causes the development of blood discharge from the right ventricle to the left (reverse or cross-shunt), which leads to arterial hypoxemia (Eisenmenger syndrome).
Long-term practice of cardiac surgeons shows that the best results in closing a ventricular septal defect can be achieved by shunting blood from left to right. Therefore, when planning the operation, hemodynamic parameters (pressure, resistance and volume of discharge) are carefully taken into account.
The size of the ventricular septal defect is assessed based on its absolute size and comparison with the diameter of the aortic opening: a small defect is 1-3 mm (Tolochinov-Roger disease), a medium one is equal to approximately 1/2 the diameter of the aortic opening, a large one is equal to or greater than its diameter .
Taking into account the anatomical location of the defect, the following are distinguished:
- perimembranous ventricular septal defects – 75% (inflow, trabecular, infundibular) are located in the upper part of the septum under the aortic valve and can close spontaneously;
- muscular defects of the interventricular septum - 10% (inflow, trabecular) - located in the muscular part of the septum, at a considerable distance from the valve and conduction systems;
- supracrestal defects of the interventricular septum - 5% - are located above the supraventricular crest (the muscle bundle that separates the cavity of the right ventricle from its outflow tract) and do not close spontaneously.
The clinical manifestations of large and small isolated ventricular septal defects are different. Small ventricular septal defects (Tolochinov-Roger disease) have a diameter of less than 1 cm and occur in 25-40% of all VSDs. They manifest themselves as mild fatigue and shortness of breath on exertion.
The physical development of children, as a rule, is not impaired. Sometimes they have a weakly expressed dome-shaped protrusion of the chest in the area of the heart - the “heart hump”.
A characteristic clinical sign of small defects of the interventricular septum is the presence of a rough systolic murmur over the heart area, which is detected already in the first week of life.
Large ventricular septal defects, measuring more than 1/2 the diameter of the aortic orifice or more than 1 cm, manifest themselves symptomatically already in the first 3 months of life of newborns, leading in 25-30% of cases to the development of a critical condition.
With large defects of the interventricular septum, malnutrition, shortness of breath during exercise or at rest, and increased fatigue are observed. Feeding difficulties are typical: intermittent sucking, frequent separation from the breast, shortness of breath and pallor, sweating, oral cyanosis.
Most children with ventricular septal defect have a history of frequent respiratory infections, prolonged and recurrent bronchitis and pneumonia.
At the age of 3-4 years, as heart failure increases, such children begin to complain of palpitations and pain in the heart area, a tendency to nosebleeds and fainting.
Transient cyanosis is replaced by constant oral and acrocyanosis; I am worried about constant shortness of breath at rest, orthopnea, cough (Eisenmenger syndrome).
The presence of chronic hypoxia is indicated by deformation of the phalanges of the fingers and nails (“drumsticks”, “watch glasses”).
The examination reveals a “heart hump”, developed to a lesser or greater extent; tachycardia, expansion of the boundaries of cardiac dullness, rough intense pansystolic murmur; hepatomegaly and splenomegaly. Congestive wheezing is heard in the lower parts of the lungs.
Methods for instrumental diagnosis of ventricular septal defect include ECG, PCG, chest radiography, EchoCS, cardiac catheterization, angiocardiography, ventriculography.
An electrocardiogram for a ventricular septal defect reflects ventricular overload, the presence and severity of pulmonary hypertension.
In adult patients, arrhythmias (extrasystole, atrial fibrillation), conduction disturbances (right bundle branch block, WPW syndrome) may be recorded.
Phonocardiography records a high-frequency systolic murmur with a maximum in the III-IV intercostal space to the left of the sternum.
Echocardiography allows you to detect a ventricular septal defect or suspect it based on characteristic hemodynamic disturbances.
X-ray of the chest organs with large defects of the interventricular septum reveals an increase in the pulmonary pattern, increased pulsation of the roots of the lungs, and an increase in the size of the heart.
Probing of the right cavities of the heart reveals increased pressure in the pulmonary artery and right ventricle, the possibility of inserting a catheter into the aorta, and increased oxygenation of venous blood in the right ventricle. Aortography is performed to exclude concomitant congenital heart disease.
Differential diagnosis of ventricular septal defect is carried out with an open atrioventricular canal, common truncus arteriosus, aortopulmonary septal defect, isolated pulmonary artery stenosis, aortic stenosis, congenital mitral regurgitation, thromboembolism.
The asymptomatic course of the ventricular septal defect, given its small size, allows one to refrain from surgical intervention and carry out dynamic monitoring of the child.
In some cases, spontaneous closure of the ventricular septal defect is possible by 1-4 years of life or at a later age.
In other cases, surgical closure of the ventricular septal defect is indicated, usually after the child reaches 3 years of age.
With the development of heart failure and pulmonary hypertension, conservative treatment is carried out with the help of cardiac glycosides, diuretics, angiotensin-converting enzyme inhibitors, cardiotrophs, and antioxidants.
Cardiac surgical treatment of ventricular septal defect can be radical and palliative.
Radical operations include suturing small defects of the interventricular septum with U-shaped sutures; synthetic plastic for large defects (Teflon, Dacron, etc.)
) patch or biological (preserved xenopericardium, autopericardium) tissue; X-ray endovascular occlusion of the ventricular septal defect.
In infants with severe malnutrition, large left-to-right shunting of blood and multiple defects, preference is given to palliative surgery aimed at creating artificial stenosis of the pulmonary artery using a cuff. This stage allows you to prepare the child for radical surgery to eliminate the ventricular septal defect at an older age.
Women with a small ventricular septal defect are usually able to carry and give birth to a child normally.
However, with a large defect size, arrhythmia, heart failure or pulmonary hypertension, the risk of complications during pregnancy increases significantly. The presence of Eisenmenger syndrome is an indication for artificial termination of pregnancy.
Women with a ventricular septal defect have an increased likelihood of having a child with the same or another congenital heart defect.
Before planning a pregnancy, a patient with a heart defect (operated or not) needs to consult with an obstetrician-gynecologist, cardiologist, or geneticist. Management of pregnancy in women with ventricular septal defect requires increased attention.
The natural history of ventricular septal defect as a whole does not allow one to hope for a favorable prognosis. Life expectancy with this defect depends on the size of the defect and averages about 25 years.
With large and medium defects, 50-80% of children die before the age of 6 months. or 1 year from heart failure, congestive pneumonia, bacterial endocarditis, cardiac arrhythmias, thromboembolic complications.
In rare cases, VSD does not have a significant impact on the duration and quality of life.
Spontaneous closure of the ventricular septal defect is observed in 25-40% of cases, mainly when it is small.
However, even in this case, patients should be under the supervision of a cardiologist due to possible complications from the conduction system of the heart and a high risk of infective endocarditis.
Source: https://www.KrasotaiMedicina.ru/diseases/zabolevanija_cardiology/ventricular-septal-defect
Positive Babinsky symptom - causes
A positive Babinski sign is associated with damage to the pyramidal system in the brain. The combination of these changes is also called corticospinal tract or central motor neuron damage. Because the pyramidal tracts intersect, Babinski's sign (depending on the height at which the changes appear) may occur on the same or opposite side of the body than the current disease process.
The cause of a positive Babinski reflex may be:
- stroke (this cause is the most common)
- trauma to the skull and brain, especially around the frontal lobes
- cancer of the brain or meninges
- multiple sclerosis or amyotrophic lateral sclerosis
- meningitis
Epilepsy can also cause the short-term appearance of Babinski's sign.
There are also reports of a positive symptom in healthy people during certain stages of sleep. The reason for this phenomenon has not yet been satisfactorily explained.