Focal neurological symptoms
(
focal neurological deficit
) is a term that refers to neurological symptoms characteristic of local damage to certain structures of the central or peripheral nervous system. Focal neurological symptoms in many cases are combined with general cerebral symptoms, which are a manifestation of diffuse damage [1]. Focal neurological symptoms allow not only to identify the presence of local damage, but also to carry out topical diagnostics, that is, to fairly reliably determine the area of damage based on knowledge of neuroanatomy.
Focal neurological symptoms are characteristic of a number of diseases, including traumatic brain injury[2], brain tumors, strokes, etc.[3]
Lesions of the cerebral cortex
Frontal cortex lesion
Left frontal lobe highlighted in red
Frontal lobe damage usually involves the motor system and can present with a variety of symptoms, depending on which part of the frontal lobe is affected:
- unsteady gait (unsteadiness when walking);
- muscle rigidity, difficulty in passive movements in the limbs (hypertonicity);
- paralysis of one limb (monoparesis) or two limbs on one side of the body (hemiparesis);
- paralysis of the head and eye movements
- a speech disorder in which a person has difficulty finding words, synonyms, cases, sound order, grammatical tense, that is, motor aphasia (Broca's aphasia);
- focal epileptiform Jacksonian seizures, that is, tonic or clonic spasms of the fingers or toes that are not accompanied by loss of consciousness;
- grand mal epileptic or tonic-clonic seizures;
- the appearance of “frontal psyche”, that is, personality changes such as disinhibition, foolishness (inappropriate jocularity), causeless rage, lack of initiative and indifference, apathy, akinetic mutism (“waking coma”, in which the patient does not speak, does not answer questions and does not comes into contact with others while maintaining consciousness), general lethargy, tendency to antisocial acts (arson, attacks);
- “frontal signs”, that is, a return to primitive reflexes such as the proboscis, grasping and palmo-oral reflexes;
- unilateral loss of smell (anosmia).
Damage to the parietal lobe cortex
The left parietal lobe is highlighted in red.
Damage to the parietal lobe is manifested by disturbances in sensitivity and perception, including:
- impaired tactile sensitivity;
- violation of kinesthesia, that is, postural sensations (the sensation of changing the position of the body in space) and the sensation of passive movement;
- syndromes of sensory and visual neglect, that is, the inability to pay attention to things in certain parts of the sensory or spatial environment of a person, in its extreme form this can be “abandonment of a limb”;
- loss of the ability to read, write or count (dyslexia, dysgraphia, dyscalculia);
- loss of ability to find a specific place (geographic agnosia);
- loss of the ability to recognize familiar objects when feeling them with closed eyes (astereognosia - a type of tactile agnosia).
Damage to the temporal lobe cortex
The left temporal lobe is highlighted in red.
Signs of damage to the temporal lobe are manifested by defects in auditory perception, convulsive syndrome, hallucinations, etc., in particular, the following may be observed:
- deafness without damage to ear structures (cortical deafness);
- tinnitus, auditory hallucinations;
- loss of the ability to understand music or language - sensory aphasia or Wernicke's aphasia;
- amnesia (loss of long-term and/or short-term memory);
- other memory disturbances such as déjà vu;
- complex multimodal hallucinations;
- complex partial seizures (temporal lobe epilepsy).
Damage to the occipital lobe
The left occipital lobe is highlighted in red.
When the occipital lobe is damaged, the cortical part of the visual analyzer usually suffers, as evidenced by:
- complete loss of vision (cortical blindness);
- loss of vision with denial of loss (Anton-Babinsky syndrome);
- loss of perception of the same right or left halves of the visual field (homonymous hemianopsia);
- visual agnosia - inability to recognize familiar objects, colors or faces;
- visual illusions such as micropsia (objects appear smaller) and macropsia (objects appear larger);
- visual hallucinations displaying elementary forms, such as zigzags and flashes in one half of the visual field for each eye separately; they should be distinguished from temporal visual hallucinations, which display complex shapes and fill the entire visual field.
• Neurological symptoms
NEUROLOGICAL SYMPTOMS
1) DISORDERS OF CONSCIOUSNESS.
There are several forms, differing in depth and accompanying clinical manifestations.
Coma
The severity of the condition is divided into three degrees:
I – light,
II – moderate severity
III – deep – an unconscious state in which the functions of the brain stem are impaired with respiratory distress, cardiac activity and a sharp decrease in reflexes.
There is no contact with such patients; a reaction to sharp painful stimuli persists in the form of a grimace of pain or simple movements.
The pathogenetic mechanisms of comatose states are extremely diverse (traumatic brain injury, stroke, meningitis, meningoencephalitis, tumors, exo- and endogenous intoxications, status epilepticus, somatic diseases, endocrine disorders).
The decisive sign of cerebral coma is the establishment of focal neurological symptoms (oculomotor disorders, paresis, paralysis, decreased tone).
In deep coma, the characteristic symptoms are severe atony, areflexia with lack of pupillary response to light against the background of significant respiratory impairment and a sharp impairment of cardiovascular activity.
Confusion and disorientation
They are characterized by the patient’s inability to really assess his condition, he does not understand where he is, disoriented in place and time (encephalitis, traumatic brain injury, tumors).
Pathological drowsiness.
The patient constantly falls asleep, and a state close to normal sleep develops, which is most common in acute drug intoxication and encephalitis.
Stun
Characterized by sudden silence, indifference to surrounding people and surroundings (tumors, progressive dementia).
Sopor.
The depth of switching off consciousness is less pronounced than in comatose states.
The patient can react to treatment and mechanical stimuli, opening his eyes and making response actions with his limbs, but when the stimuli stop, he quickly falls into his previous state.
It is most common in severe brain lesions such as brain tumors, traumatic brain injury, encephalitis, and strokes.
Twilight disturbances of consciousness
A deep disorder of mental activity, most characteristic of genuine epilepsy and organic diseases of the brain occurring with epileptiform syndrome.
2) DISORDERS OF HIGHER NERVOUS ACTIVITY.
The ability to speak correctly, read, the ability to express one’s logical thinking, and demonstrate the wealth of one’s intellect takes part in the entire human brain. At the same time, there are certain centers of the cerebral cortex (the left hemisphere in right-handed people), the defeat of which causes a variety of speech disorders, as well as reading, counting and writing.
Motor aphasia
Impaired ability to pronounce words and phrases. The speech and meaning of the words of others are understood correctly.
, literal and verbal paraphasia (rearrangement of letters and words) are sometimes observed .
Motor aphasia is often combined with a reading disorder - alexia
, as well as
with a writing disorder - agraphia.
Sensory aphasia
Impaired understanding of oral speech, when the patient hears speech addressed to him, but cannot understand its meaning.
Amnestic aphasia.
The patient does not remember the names of objects that are well known to him. The doctor's suggestion of the first letters of a forgotten word often helps to remember the name of the object.
Apraxia
Violation of purposeful movements of a domestic or professional nature (impossibility to comb one's hair or light a match).
A distinction is made between motor apraxia (impaired spontaneous movements and imitation movements)
, often limited to one limb;
constructive apraxia (the inability to construct a whole from parts - to make a figure from matches)
;
Agnosia
Impaired recognition while the function of the sensory organs is preserved is often combined with apraxia. Visual agnosia is characterized by the fact that the patient, while maintaining vision, does not recognize familiar objects or people. Sometimes objects are perceived incorrectly (enlarged or reduced).
Astereognosis
Impaired recognition of objects by touch while maintaining superficial and joint-muscular sensitivity. Often the patient feels “extra legs” (three), six fingers (pseudomelia)
or confuses the right and left sides of the body
(autotopagnosia)
3) MOTOR DISORDERS.
Normal human motor activity is determined by the coordinated interaction of the cortical centers of the brain, subcortical nodes, cerebellum and spinal cord.
Central paralysis or paresis
Characterized by the inability to make voluntary movements due to weakness in the limbs.
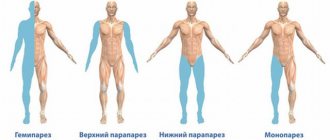
Hemiparesis
Weakening of voluntary movements of the limbs on one side
monoparesis - weakness of one limb
paraparesis upper or lower - weakness of the upper or lower limbs
Hemiplegia
Damage to both limbs on one side
Cross paralysis
The same paresis or paralysis of the upper limb and the opposite lower limb is observed.
Bilateral spastic paralysis, or paraplegia
Damage to all four limbs - occurs when the upper parts of the spinal cord are affected.
Spasticity
Increased muscle tone, tendon and periosteal reflexes, combined with clonus of the patellas and feet, as well as the appearance of pathological foot reflexes of an extensor (Babinsky reflex) and flexion (Bechterew reflex) nature. Increased muscle tone is characteristic of pyramidal disorders.
Rigidity
A condition of muscles characterized by tightness, tension, and resistance to passive movement.
Myoclonus
Fast rhythmic contractions, usually of small muscles of the face and limbs. Occurs with encephalitis, head injuries, intoxication with certain industrial poisons or together with epileptic seizures
Spasmodic torticollis
Torticollis caused by contraction of the neck muscles: the head is turned to the side or strongly tilted towards the shoulder due to convulsive contraction of the neck muscles. It is also observed as torsion dystonia in inflammatory or vascular diseases of the central nervous system, but may have a psychogenic basis.
Facial hemispasm or paraspasm
Periodically recurring clonic-tonic spasms of the muscles of half or the entire face, respectively.
Blepharospasm
Bilateral convulsive contractions of the orbicularis oculi muscles. Observed in cases of damage to the brain stem, subcortical nodes (rheumatic chorea, epidemic encephalitis, atherosclerosis).
Tremor
Rhythmic small-scale tremors in the fingers of the limbs
Intentional tremors
Trembling that occurs or intensifies with purposeful movements, often turning into pronounced hyperkinesis in patients with multiple sclerosis.
Ataxia
Impaired coordination of movements, when movements become awkward, balance is disturbed when walking, moving (dynamic ataxia) and standing (static ataxia).
4) SENSITIVITY DISORDERS.
Hyperpathy
Inappropriate perception of cold, heat or touch in the form of a burning, unpleasant irritation
Anesthesia
Complete loss of sensation. If anesthesia affects the right or left half of the body, then they speak of corresponding hemianesthesia
Damage to the brain stem (strokes, tumors, neuroinfection) is manifested by hemianesthesia on the opposite side, and in the facial area - on the side of the lesion
Tetraanesthesia
Loss of sensation in all limbs and trunk
Paraanesthesia
Loss of sensation in both legs and lower torso
Monoanesthesia
Anesthesia for one arm or leg
Hypesthesia
Incomplete loss of superficial sensitivity. Thus, with polyneuritis and polyneuropathy of infectious or toxic-metabolic origin, when the distal parts of the peripheral nerves of the extremities are affected, hypoesthesia or anesthesia is distributed in the form of gloves and socks.
Neuralgia
Damage to predominantly sensory nerves, manifested by constant or short-term (1-2 min) attacks of excruciating pain, localized in the zone of innervation of the corresponding nerve trunks
5) VISUAL DISORDERS.
Amaurosis
Complete loss of vision in one eye, impairment of the pupillary reflex with preservation of the pupillary reflex of the affected eye when the healthy eye is illuminated (damage to the optic nerve).
Amblyopia
Decreased visual acuity not caused by refractive error or eye disease.
Scotomas
small defects in the visual field or narrowing of the visual field (the limits of the visual field are normal for white color: outer - 80°, inner - 60°, lower - 70°, upper - 60°). Occurs during inflammatory processes in the area of the optic chiasm.
Hemianopsia
The loss of one half of the visual field acquires a different (heteronymous) character with the development of an inflammatory process in the area of the optic chiasm.
6) HEARING IMPAIRMENTS.
Hypacusia
Decreased hearing, often on one side, reaching complete deafness (anacusia), especially for high-pitched sounds; indicates damage to the sound-receiving apparatus located in the inner ear (cochlea, auditory nerves, brainstem nuclei).
Hyperacusis
A sharp painful perception of sound with an unpleasant tint, indicating damage to the sound-conducting apparatus (middle ear - eardrum, auditory ossicles). Most often, hyperacusis is observed in patients with damage to the facial nerve in the facial (fallopian) canal above the origin of the stapedii.
Source: https://emhelp.jimdofree.com/%D1%88%D0%BF%D0%B0%D1%80%D0%B3%D0%B0%D0%BB%D0%BA%D0%B8-03 /%D0%BD%D0%B5%D0%B2%D1%80%D0%BE%D0%BB%D0%BE%D0%B3%D0%B8%D1%8F/%D0%BD%D0%B5 %D0%B2%D1%80%D0%BE%D0%BB%D0%BE%D0%B3%D0%B8%D1%87%D0%B5%D1%81%D0%BA%D0%B8%D0 %B5-%D1%81%D0%B8%D0%BC%D0%BF%D1%82%D0%BE%D0%BC%D1%8B/
Damage to the extrapyramidal nervous system
Cerebellar lesion
Cerebellar lesions usually cause problems with balance and motor coordination and may present with the following symptoms:
- ataxia - unsteady and clumsy movements of the limbs or torso;
- inability to coordinate fine motor skills (tremor, poor finger-nose test);
- dysdiadochokinesia - the inability to perform rapid alternating movements, for example, quickly bend and straighten fingers; voluntary eye movements are inhibited in extreme positions and lead to saw-tooth movements (nystagmus).
General cerebral symptoms and syndromes
Arise due to:
increased intracranial pressure
· increase in brain volume
Difficulty in the outflow of cerebrospinal fluid through the cerebrospinal fluid pathways
liquorodynamic disorders
General cerebral symptoms include:
· Impaired consciousness
.
· Headache is the most common symptom of nervous system diseases. Depending on the cause, the headache can be acute or dull, squeezing, bursting, throbbing, constant or paroxysmal, and can intensify with sudden turns of the head, walking, or shaking.
· Dizziness is often observed with anemia, cerebral vascular diseases, cerebral hemodynamic disorders, and volumetric processes.
· Vomiting is one of the most common cerebral symptoms. It should be remembered that “cerebral vomiting” does not always occur without preceding nausea and can improve the patient’s well-being. It is important to take into account the connection between vomiting and headaches and the simultaneity of their occurrence.
Seizures
may be focal symptoms. As a general cerebral symptom, they are more often observed in hypertension syndrome and cerebral edema.
Meningeal symptoms
Meningeal symptoms are a consequence of irritation of the meninges directly by trauma (bruises, ruptures), pressure from bone fragments, foreign bodies, hematomas, blood, infection, etc.
Typical severe meningeal symptoms can be identified during an external examination of the patient:
- forced position, lying on your side with your head thrown back and legs bent at the knees and hip joints ("trigger" pose)
- photophobia.
- increased excitability, an extreme reaction to harsh stimuli can be a convulsive seizure
- intense headache, aggravated by moving the head, nausea and vomiting.
There are more than 30 clinical symptoms that help diagnose meningeal syndrome. The most widely used among neurologists and general practitioners are the following:
· Kernig's sign - with the patient lying on his back, the lower limb is passively flexed at the hip and knee joint. Subsequent attempts by the doctor to straighten the leg at the knee are impossible due to tonic contraction of the shin flexor muscles.
· Brudzinski's symptoms - in the supine position, there is an involuntary pulling of the lower extremities towards the abdomen when bending the patient's head (upper), pressing on the pubis (middle), checking Kernig's sign (lower).
· Edelman's sign – extension of the big toe when examined using the Kernig method.
· Netter's sign - in a sitting position with legs extended in bed, pressing on the knee of one leg causes flexion of the other.
· Kholodenko's symptom – bending of the knees when the doctor tries to lift the patient by the shoulders.
· Guillain's sign - with the patient in the supine position with straightened legs, compression of the muscles of the anterior surface of one thigh leads to flexion of the second leg.
· Lessage's sign - when holding a child in the air in a vertical position by the armpits, the legs are pulled towards the stomach. Characteristic for young children.
The most important role in the diagnosis of meningeal syndrome is played by lumbar puncture .
Focal symptoms
Focal neurological symptoms ( focal neurological deficit ) is a term that refers to neurological symptoms characteristic of local damage to certain structures of the central or peripheral nervous system.
· Frontal cortex lesion
Frontal lobe lesions usually involve the motor system and can present with a variety of symptoms, depending on which part of the frontal lobe is affected:
- unsteady gait;
- muscle rigidity, difficulty in passive movements in the limbs (hypertonicity);
- paralysis of one limb (monoparesis) or two limbs on one side of the body (hemiparesis);
- paralysis of the head and eye movements
- a speech disorder in which a person has difficulty finding words, synonyms, cases, sound order, grammatical tense, that is, motor aphasia (Broca's aphasia);
- focal epileptiform Jacksonian seizures, that is, tonic or clonic spasms of the fingers or toes that are not accompanied by loss of consciousness;
- grand mal epileptic or tonic-clonic seizures;
- the appearance of “frontal psyche”, that is, personality changes such as disinhibition, foolishness (inappropriate jocularity), causeless rage, lack of initiative and indifference, apathy, akinetic mutism (“waking coma”, in which the patient does not speak, does not answer questions and does not comes into contact with others while maintaining consciousness), general lethargy, tendency to antisocial acts (arson, attacks);
- “frontal signs”, that is, a return to primitive reflexes such as the proboscis, grasping and palmo-oral reflexes;
- unilateral loss of smell (anosmia).
· Damage to the parietal lobe cortex
Damage to the parietal lobe causes disturbances in sensitivity and perception, including:
- impaired tactile sensitivity;
- violation of kinesthesia, that is, postural sensations (the sensation of changing the position of the body in space) and the sensation of passive movement;
- syndromes of sensory and visual neglect, that is, the inability to pay attention to things in certain parts of the sensory or spatial environment of a person, in its extreme form this can be “abandonment of a limb”;
- loss of the ability to read, write or count (dyslexia, dysgraphia, dyscalculia);
- loss of ability to find a specific place (geographic agnosia);
- loss of the ability to recognize familiar objects when feeling them with closed eyes (astereognosia - a type of tactile agnosia).
· Damage to the temporal lobe cortex
Signs of damage to the temporal lobe are manifested by defects in auditory perception, convulsive syndrome, hallucinations, etc., in particular, the following may be observed:
- deafness without damage to ear structures (cortical deafness);
- tinnitus, auditory hallucinations;
- loss of the ability to understand music or language - sensory aphasia or Wernicke's aphasia;
- amnesia (loss of long-term and/or short-term memory);
- other memory disturbances such as déjà vu;
- complex multimodal hallucinations;
- complex partial seizures (temporal lobe epilepsy).
· Damage to the occipital lobe
When the occipital lobe is damaged, the cortical part of the visual analyzer usually suffers, which may be evidenced by:
- complete loss of vision (cortical blindness);
- loss of vision with denial of loss (Anton-Babinsky syndrome);
- loss of perception of the same right or left halves of the visual field (homonymous hemianopsia);
- visual agnosia - inability to recognize familiar objects, colors or faces;
- visual illusions such as micropsia (objects appear smaller) and macropsia (objects appear larger);
- visual hallucinations displaying elementary forms, such as zigzags and flashes in one half of the visual field for each eye separately; they should be distinguished from temporal visual hallucinations, which display complex shapes and fill the entire visual field.
· Cerebellar lesion
Cerebellar lesions usually cause problems with balance and motor coordination and may present with the following symptoms:
- ataxia - unsteady and clumsy movements of the limbs or torso;
- inability to coordinate fine motor skills (tremor, poor finger-nose test);
- dysdiadochokinesia - the inability to perform rapid alternating movements, for example, quickly bend and straighten fingers; voluntary eye movements are inhibited in extreme positions and lead to saw-tooth movements (nystagmus).
· Limbic system damage
Damage to the limbic system includes memory loss or impairment and may include symptoms such as:
- loss or confusion of long-term memory to focal neuropathy (retrograde amnesia);
- inability to form new memories (anterograde amnesia);
- loss or decrease in emotionality (apathy);
- loss of smell (anosmia);
- loss of ability to make decisions and learn new skills.
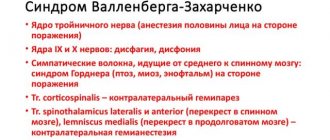
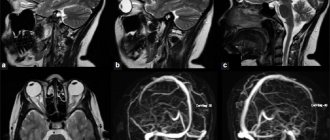
· Brain stem damage
Signs of brainstem damage can manifest as a combination of a variety of sensory and motor disturbances, depending on which fiber pathways and which cranial nerve nuclei are affected.
Spinal cord lesion
A sign of spinal cord damage is unilateral paralysis with contralateral (that is, on the opposite side) loss of pain sensitivity.
In some cases, paresthesia occurs - tingling, crawling sensation, numbness.
The degree, nature and location of the disorders depend on the anatomy and degree of damage to the spinal cord structure.
Limbic system damage
The left half of the limbic system is highlighted in red.
Damage to the limbic system includes memory loss or impairment and may include the following symptoms:
- loss or confusion of long-term memory to focal neuropathy (retrograde amnesia);
- inability to form new memories (anterograde amnesia);
- loss or decrease in emotionality (apathy);
- loss of smell (anosmia);
- loss of ability to make decisions and learn new skills.
Notes
- Lovell MK, Franzen MD.
Neuropsychological assessment // Neuropsychiatry of Traumatic Brain Injury / Silver JM, Yudofsky SC, Hales RE. - Washington, DC: American Psychiatric Press, 1994. - P. 152–3. — “Although brain injuries are often described as diffuse or focal in nature, in reality many traumatic brain injuries have both focal and diffuse components.” — ISBN 0-88048-538-8. - Thiruppathy SP, Muthukumar N.
Mild head injury: revisited // Acta Neurochir (Wien). - 2004. - Vol. 146. - P. 1075-1082. - PMID 15744844. - Thal GD, Szabo MD, Lopez-Bresnahan M. et al.
Exacerbation or unmasking of focal neurologic deficits by sedatives // Anesthesiology. - 1996. - Vol. 85. - P. 21-25. - PMID 8694368.
| This is a draft article on neurology. You can help the project by adding to it. |