Hundreds of people die every day due to cardiac arrest. Death occurs due to cardiac pathologies or due to normal physiological causes, such as old age or violent processes - accident, drowning. Is it possible to prevent a person's death in case of cardiac arrest? And if so, how can this be done? Let's take a closer look at the reasons that cause cardiac arrest and how can a human life be saved with such a diagnosis?
Clinical picture: how are the consequences of TBI classified?
All consequences of TBI can be classified into early (acute) and long-term. Early ones are those that occur immediately after receiving damage, while late ones appear after some time, perhaps even years later. Absolute signs of head injury are nausea, pain and dizziness, as well as loss of consciousness. It occurs immediately after injury and can last for a variable period of time. Early symptoms also include:
- facial redness;
- hematomas;
- seizure;
- visible bone and tissue damage;
- liquor leakage from the ears and nose, etc.
Depending on how much time has passed since the injury, the severity of the injuries, as well as their location, various types of long-term consequences of traumatic brain injury are distinguished.
| Location of damage | Possible consequences |
| Temporal lobe | convulsive attacks throughout the body; speech and vision disorder. |
| Frontal lobe | tremor (shaking) of the upper and lower extremities; slurred speech; unsteady gait, weakness in the legs and possible falls on the back. |
| Parietal lobe | sharp deterioration of vision up to the formation of blindness; lack of manifestation of sensitive reactions on one half of the body. |
| Cranial nerve injuries | hearing impairment; pronounced asymmetry of the oval of the face; the appearance of strabismus. |
| Cerebellar region | nystagmus (involuntary eye movements from side to side); disturbances in coordination of movements; hypotonia of muscle mass; “shaky” gait and possible falls. |
Glasgow scale - what to expect from TBI
Doctors usually classify the consequences of traumatic brain injury using a special system - the Glasgow scale. So, the result of the damage received is as follows:
- The patient experiences absolute recovery and, as a result, recovery, after which he returns to his usual life and work.
- Moderate disability. The patient has mental and neurological disorders that prevent him from returning to work, but his self-care skills are preserved.
- The disability is severe. The patient is not capable of self-care.
- Vegetative states. Inability to perform certain movements, sleep disturbances and other autonomic symptoms.
- Death. Termination of activity of vital organs.
The outcome of the injury can be judged as early as a year after it was received. All this time, rehabilitation therapy must be present, including physical therapy, medication, physiotherapeutic procedures, a vitamin and mineral complex, work with neurologists and psychiatrists, etc.
First aid for cardiac arrest
Today, cardiac arrest is considered, unfortunately, a very common cause of death. And this, despite the fact that timely measures can save many lives. This type of pathology occurs suddenly, often during sleep, and affects not only people with diseases of the cardiovascular system, but also healthy people. When you are around a victim whose heart has stopped, you need to be sure what kind of situation people are facing and what can be done.
- How to detect if the heart has stopped
- Is it possible to save a person, and how much time is there for this?
- Basic measures and treatment
- Possible reasons for the occurrence of pathology
- Possible pathological results
How to detect if the heart has stopped
Doctors know certain basic indicators, knowing which, it is possible to determine whether cardiac arrest has actually occurred, and what measures can be taken to save the victim.
- One of the first indicators is the absence of a pulse (it cannot be felt in the area of large arteries). To accurately determine the absence/presence of a pulse, you need to place your middle and index fingers on the area of the carotid artery; if it cannot be felt, you must immediately begin resuscitation without waiting for emergency help to arrive (by first calling a team).
- Symptoms also include the unusual sound of a heartbeat.
- Doctors call cessation of breathing activity a very important sign. The presence/absence of respiratory function can be determined using any mirror surface that is at hand (pocket mirror) - it is brought to the mouth or nose, and, in addition, visually - by the presence or absence of respiratory movements in the chest area.
- Dilated pupils that do not respond to light rays are also one of the signs. To identify this, it is best to direct the light of a flashlight or lighter into the eyes, and if there is no reaction (no constriction of the pupils is detected), we can conclude that the myocardium is not functioning.
- A change in natural complexion is evidence of a clear violation of the circulatory system. As a rule, the face takes on a bluish or gray tint.
- Loss of consciousness lasting 10 to 20 seconds or more is one of the symptoms of cardiac arrest. This usually indicates disturbances in the functioning of ventricular fibrillation or the onset of asystole. This condition can be detected by gently patting the face or making noise (claps, loud noises, screaming).
Is it possible to save a person, and how much time is there for this?
When you are near a victim who has suffered a pathological cardiac arrest, the main thing for those around you is not to hesitate, and to understand that competent first aid in case of cardiac arrest is the only chance for salvation. Doctors believe that there are only seven minutes to save a life, and in such a way that there will be no serious consequences in the future.
Technique for performing indirect cardiac massage
In a situation where it is possible to save a person’s life in only 7-10 minutes, the victim’s risk of mental and neurological pathologies in the future increases. Delayed or ineptly provided assistance, as a rule, leads to disability of the victim, and even to complete incapacity, that is, the consequences can be very severe and unpredictable.
The main focus of assistance is the restoration of respiratory activity, the rhythm of the heartbeat, as well as the launch of the blood flow system. This is extremely necessary, since the blood flow provides cells and tissues with oxygen, in the absence of which the functioning of organs, especially the brain, and therefore human life itself is impossible. So in case of short-term cardiac arrest, everything depends only on the speed of actions of the surrounding people or doctors.
To make sure of this, you need to gently shake the victim and call him loudly several times. As soon as signs of cardiac arrest (one or more) are identified, resuscitation must be started immediately. Help consists of several stages.
- First of all, the victim must be carefully placed on a flat and hard surface, and then his head should be tilted back.
- If possible, clear (clear) the airways from accumulated mucus (before doctors arrive, only the nasal passages and oral cavity are cleared).
- At the next stage, it is necessary to perform artificial ventilation of the lungs (so-called mouth-to-mouth or nose-to-mouth breathing).
In case of sudden cardiac arrest, doctors also recommend external (so-called indirect) massage. But before this you need to carry out a “precordial stroke”. This is a punch directly to the middle area of the sternum. In this case, it is important to strike in such a way that the blow is not directed directly at the heart area, otherwise the victim’s situation may seriously worsen. Despite the fact that doctors call this a preparatory measure, in some cases such a blow can resuscitate the victim without the use of other measures.
In any option, it maximizes the results of the massage. If this event did not help to resuscitate the victim, and the ambulance has not yet arrived, you need to perform an external massage. It is necessary to act quickly and clearly, since resuscitators believe that it is assistance in case of cardiac arrest, provided on time, that is the hope for a person to get out of this condition and reduce the negative consequences.
Basic measures and treatment
When providing assistance, it is imperative to check the basic indicators of the victim’s condition every 2-3 minutes - feel the pulse, check the presence/absence of respiratory activity, the reaction of the pupils to light. Doctors warn that resuscitation measures can be stopped if breathing has been restored, but under no circumstances should it be stopped when the pulse has just returned. In this case, it is necessary to continue artificial ventilation. External massage is performed until the skin color becomes natural.
It is also necessary to know that if no measures lead to saving a life, then resuscitation measures can be completed only after the arrival of a doctor who has the right to allow resuscitation to be stopped. Of course, the above measures are only the initial stage of saving the life of the victim, which is provided to him by the people around him, without waiting for an emergency resuscitation team. Professional resuscitation measures are much more serious.
Resuscitation of a patient using a defibrillator
In order to remove the victim from this pathological condition, and with the least losses and consequences, emergency doctors use special methods in case of sudden cardiac arrest. But the main task of resuscitators also remains restoring the patient’s respiratory function. For this use:
- ventilation using a special mask;
- in situations where this does not bring results, or it is not possible to use a mask, then tracheal incubation is indicated. This method is the most effective, as it clears the airways and restores breathing function. But only a specialist doctor should install the incubation tube.
To start the heart, professional resuscitators use a defibrillator as an emergency measure - a device that applies an electric current to the heart muscle. In addition to such measures, resuscitators use special medications (for specific cases, their own drug). The most effective ones include:
- for asystole, atropine is recommended;
- to strengthen and increase the frequency of contractions of the heart muscle, adrenaline (epinephrine) is prescribed;
- Several drugs are used as antiarrhythmic drugs - amiodarone, bretylium tosylate, lidocaine;
- sodium sulfate is recommended to stabilize cardiac activity and stimulate cell functioning;
- In the presence of hyperkalemia, calcium is effective.
Possible reasons for the occurrence of pathology
The main causes of cardiac arrest are not very diverse. In medical practice, ventricular fibrillation disorder takes first place - these cases occupy from 70% to 90%. This is due to a sudden contraction of the muscle fibers of the ventricles of a chaotic nature. This pathology causes interruptions in blood flow to tissues and organs.
Other causes include types of cardiac arrest that also require resuscitation for cardiac arrest, such as:
- paroxysmal ventricular tachycardia – in the absence of a pulse in large vessels;
- bioelectrical activity in the absence of ventricular contractions - electromechanical dissociation;
- genetic predisposition - inherited Romano-Ward disease.
In addition, reflex cardiac arrest occurs in completely healthy people, and there is also a predisposition or relevant factors for this:
- Sudden hypothermia (temperature drop below 28 °C).
- Electrical injury.
- Incorrect use of medications such as glycosides, analgesics, adrenergic blockers, as well as unsuitable anesthesia drugs for individual reasons (pathology can occur during sleep).
- Lack of oxygen, such as from drowning or suffocation.
- Diagnosed coronary artery disease (at the same time, people with such a diagnosis who constantly drink alcoholic beverages are at high risk of death from such a pathology - 30% of cases).
- Abuse of tobacco products.
- Diseases with atherosclerosis, arterial hypertension or diagnosed left ventricular hypertrophy.
- Age-related changes
What determines the severity of TBI and its types?
All, including long-term types of consequences of traumatic brain injury, are subject to many factors:
- Nature of injury. The stronger and deeper it is, the greater the likelihood of complications and, as a result, long-term treatment.
- Patient's age. The younger the body, the easier it is for it to cope with the injuries received.
- Speed of medical care. The sooner the victim is shown to a doctor and the stage of treatment begins, the easier it will be for him to recover.
As already mentioned, there are mild, moderate and severe forms of damage. According to statistics, there are almost no complications with minor injuries in young people aged 20–25 years.
Consequences in mild form
A mild form of head trauma is the most favorable option of all existing ones. Treatment usually does not take much time, and patients recover quickly. All complications are reversible, and symptoms are either early (acute) or last a short time. The following signs can be noted here:
- dizziness and headaches;
- profuse sweating;
- nausea and vomiting;
- irritability and sleep disturbance;
- weakness and fatigue.
Typically, therapy, after which the patient returns to normal life, takes 2 to 4 weeks.
Consequences in moderate form
Moderate severity is a more serious reason for concern about the patient’s health. Most often, such conditions are recorded with partial brain damage, severe bruise or fracture of the base of the skull. The clinical picture can last for quite a long time and includes symptoms:
- speech impairment or partial loss of vision;
- problems with the cardiovascular system, or more precisely with heart rhythm;
- mental disorders;
- paralysis of the cervical muscles;
- seizures;
- amnesia.
Rehabilitation after a traumatic brain injury can take from 1 month to six months.
Consequences in severe form
Severe injuries are the most dangerous and are the most likely to cause death. Most often, this type of injury is recorded after open skull fractures, severe brain contusions or compression, hemorrhages, etc. The most common type of complication after severe TBI is coma.
According to statistics, every second person in severe cases will experience the following types of consequences:
- Partial or complete disability. In case of partial disability, the ability to work is lost, but self-care skills are retained, mental and neurological disorders are present (incomplete paralysis, psychosis, movement disorders). With complete disability, the patient requires constant care.
- Coma of varying degrees of manifestation and depth. Coma due to traumatic brain injury can last from several hours to several months or years. At this time, the patient is on artificial life support devices or his organs are working independently.
- Death.
Also, even the most effective treatment and a favorable outcome of the measures taken necessarily entail the appearance of the following signs:
- problems with vision, speech or hearing;
- abnormal heart rhythm or breathing;
- epilepsy;
- seizures;
- partial amnesia;
- personality and mental disorder.
They can be combined and appear immediately after a head injury or years later.
It is impossible to give an accurate assessment of the patient’s recovery, because each organism is individual, and there are multiple examples of this. If in one case, even with severe injuries, patients endured rehabilitation with resilience and returned to normal life, then in other situations, even a mild head injury did not have the best effect on the neurological status and health in general. In any case, rehabilitation and psychological support play an important role in cases of traumatic brain injury.
– the most common cause of damage to the structures of the central nervous system. If severe damage to cerebral tissue occurs, coma may occur, which can lead to disability or death.
Birth of a child
It's a terrible scene to imagine, but there were times when women died during pregnancy and were not buried, leading to the coining of a term called "posthumous fetal expulsion." Gases accumulating inside the body, combined with softening of the flesh, lead to expulsion of the fetus.
Although such cases are very rare and the subject of much speculation, they have been documented in the period before proper embalming and rapid burial. All this seems like a description from a horror movie, but such things really happen, and this makes us once again glad that we live in the modern world.
Ecology of consciousness: Life. Scientists say that the last moments of consciousness may be accompanied by something amazing and mysterious happening inside your brain.
You may imagine yourself walking through an endless field or being surrounded by your loved ones.
Or perhaps you are walking down a long, dark tunnel with a bright, inviting light shining at the end.
In any case, when the end comes, your final experiences will be shrouded in a secret known only to you
However, scientists say that these last moments of consciousness may be accompanied by something amazing and mysterious that is happening inside your brain.
Back in 2013, researchers from the University of Michigan found that after clinical death in rats, brain activity increased rapidly, displaying electrical impulses reflecting the processes of consciousness that were higher than the signals recorded in the same animals in a state of wakefulness.
“We believed that because near-death experience is related to brain activity, neural correlates of consciousness should be identifiable in humans and animals even after cerebral circulation has ceased,” said neurologist Jimo Borjigin, who was part of the research team.
This is what they found in the experiment: anesthetized rats showed highly synchronized bursts of brain activity within 30 seconds of induced cardiac arrest, comparable to what would be seen in a highly aroused brain.
The discovered phenomenon was an unexpected discovery that may refute the prevailing idea that, due to the cessation of blood flow as a result of clinical death, the brain must be completely inert at this moment.
“This study showed that a decrease in oxygen levels or both oxygen and glucose during cardiac arrest can stimulate brain activity characteristic of conscious activity,” said Jimo Borjigin. “It also provided the first scientific basis to explain the various near-death experiences reported by many cardiac arrest survivors.”
Of course, although the results obtained by scientists do indeed create a new basis for interpreting the causes and nature of these “events” after death, it is not at all certain that people will be found in the same cognitive flashes as rats who made the journey to the next world.
At the same time, if it turns out that our brains are activated in a similar way at the moment of clinical death, it could help explain the feeling of awareness that many patients who successfully undergo resuscitation from critical illness report.
One person who knows a thing or two about this is SUNY Stony Brook critical care researcher Sam Parnia
, who published the world’s largest scientific work devoted to the analysis of people’s feelings in a state of clinical death and being “out of the body.”
In interviews with more than 100 cardiac arrest survivors, 46 percent retained memories of their encounter with death. Most of these memories had the same general themes, including bright lights, family members, and fear.
However, what is much more surprising, two out of a hundred patients surveyed were able to recall events related to their resuscitation that occurred after they had died, which completely contradicts the generally accepted views on the possibility of maintaining consciousness in a state of clinical death.
“We know that the brain cannot function after the heart stops beating. But in this case
Consciousness appeared to persist for about three minutes after the heart stopped beating
,
“Parnia told the National Post, “ although the brain usually stops functioning 20 to 30 seconds after the heart stops.”
This sounds amazing, but it's worth noting that this phenomenon was recorded in only 2 percent of patients, and Parnia himself later admitted that "the simplest explanation is that it is probably an illusion." This “illusion” may result from a neurological response to physiological stress during cardiac events. In other words, cognitive experience precedes, rather than accompanies, clinical death as such. And it is this that is retained in the patient’s memory.
Of course, this is what many in the neurobiological scientific community tend to think. “You know, I’m skeptical,” Cameron Shaw, a neuroscientist at Deakin University in Australia, told Vice earlier this year. “I think that the out-of-body experience is simply a fiction, since the mechanisms that create visual sensations and memories do not work in this state.”
Because the blood supply to the brain comes from below, brain death occurs from the top down, Cameron said.
“Our sense of self, our sense of humor, our ability to think about the future—all of that goes away within the first 10 to 20 seconds,” Julian Morgan told Vice. “Then, as the wave of dead brain cells spreads, our memories and language centers are switched off, and at the end only the nucleus remains.”
Not a very reassuring point of view, but it is worth noting that it also contradicts the results of experiments on rats. And scientists are still finding evidence of amazing biological processes that continue very actively even several days after death.
So we still don't have the answers, and while science has given us amazing new insights into what happens to the brain in the final moments, the research isn't conclusive yet.
As has already been said, we have no clear idea of what we will see and feel when the curtain comes down. But we can rest assured that we will find out eventually.
published .
If you have any questions on this topic, ask them to the experts and readers of our project
PS And remember, just by changing your consciousness, we are changing the world together! © econet
Doctors usually distinguish between two forms of oxygen deprivation. First, anoxic injuries which occur when the brain is completely deprived of oxygen due to sudden cardiac arrest, suffocation, suffocation and other sudden injuries. Second, hypoxic damage occurs when this organ receives less oxygen than it needs, but is not completely deprived of it. Because the effects of the two injuries are similar, many brain experts use the terms interchangeably.
A few seconds of oxygen deprivation will not cause long-term harm, so a child suffering from respiratory distress or a diver who needs a few extra seconds to come up for air are unlikely to suffer brain damage. The exact timeline of anoxic injury to this organ depends on a number of personal characteristics, including general brain and cardiovascular health, and the level of blood oxygenation at the time of injury. Generally speaking, injuries begin at the one-minute mark, steadily worsening after that:
- Between 30 and 180 seconds of oxygen deprivation, you may lose consciousness.
At the one minute mark, brain cells begin to die.
After three minutes, neurons suffer more damage and long-term brain damage becomes more likely.
After five minutes, death becomes inevitable.
After 10 minutes, even if the brain remains alive, coma and long-term brain damage are almost inevitable.
After 15 minutes, survival becomes almost impossible.
Of course, there are exceptions to every rule. Some training routines help the body use oxygen more efficiently, allowing the brain to go longer periods without this vital element. Free divers usually train to go without oxygen for as long as possible and the current record holder holds his breath for 22 minutes without suffering any organ damage.
Impaired consciousness: mechanism of occurrence
After damage to the central nervous system due to a traumatic brain injury, a person loses the ability to respond to any external stimulus. The psycho-emotional state is completely disrupted, the victim cannot contact the people around him. Coma sets in.
Coma due to TBI is characterized by the immersion of a person in a specific state, which is associated with inhibition of certain zones. The victim does not respond to pain, bright light and loud sound, and has no reflexes.
Consciousness is impaired when certain parts of the brain that are responsible for speech, thinking, wakefulness, and reasoning are damaged. Based on the degree of damage, loss of consciousness can have different durations:
- mild traumatic brain injury (for example, bruise): loss of consciousness does not occur or lasts no more than 5 seconds;
- moderate injury (for example, open head injury): duration of disturbance of consciousness – 2 hours-2 days;
- severe injury: deep coma and vegetative states occur.
Coma after TBI is not a separate disease, but only a consequence of damage to the central nervous system. If there is a serious general condition that threatens a person’s life, he can be immersed in. This condition allows you to cause a controlled decrease in the activity of reflexes and vital functions.
An artificial coma involves the introduction of special medications into the body. In this case, the respiratory function is performed by a ventilator.
Consequences of TBI after recovery from coma
Coma is one of the most severe consequences that occurs after a traumatic brain injury.
Let's consider the types of comatose state after TBI and how to determine its depth, and also talk about treatment methods and rehabilitation measures used after the return of a conscious state.
Why can coma occur after a TBI?
With TBI affecting the central nervous system, the response to external stimuli is lost, which leads to a disturbance in the psycho-emotional state. Suppression of large areas of the brain deprives the victim of reflex function, putting him in a comatose state. After an injury, a person stops feeling pain, does not react to loud sounds, and his pupils lose sensitivity to bright light.
Depending on the duration of loss of consciousness, there are:
- Severe traumatic brain injury. It is accompanied by intracranial pressure, which disrupts the functionality of the brain and interferes with the work of nerve impulses. The injury is accompanied by a long coma.
- Moderate injury. Loss of consciousness lasts from 2 hours to 2 days.
- Minor injuries. With bruises, consciousness is impaired for a few seconds or remains normal.
Types of coma and their symptoms
Coma that occurs due to traumatic brain injury is divided into 3 types, differing in the severity of symptoms:
- deep;
- actual coma;
- superficial.
Superficial coma
After a traumatic brain injury, the victim remains in a state of deep sleep. The person reacts to others by opening his eyes, slightly moving his limbs, and is able to carry on conversations with sluggish speech.
Actually coma
If with a superficial loss of consciousness the patient reacts to external stimuli, then in the case of an ordinary coma the reaction is spontaneous. The sudden opening of the eyes, the utterance of sounds and the contraction of limbs are not controlled by the patient, so for his safety, doctors can limit the mobility of the body using restraints.
Interesting: Providing first aid for TBI
Deep coma and vegetative state
Traumatic brain injury is accompanied by impaired reflex function. The victim, who is in a deep coma, requires a device to maintain respiratory function. The person does not respond to light and pain.
Determination of the depth of coma
The depth of coma is determined using the Glasgow scale, consisting of 3 tests for:
- motor activity, assessed from 1 to 6 points;
- speech reaction, rated from 1 to 5 points;
- eye opening reaction, graded from 1 to 4 points.
In addition to the Glasgow scale, the following are used in the diagnosis of TBI:
- CT and MRI scans that determine the location of tumors or hematomas compressing parts of the brain that control the heart rhythm and respiratory system.
- An EEG, which records the electrical activity of brain cells and the degree of damage to the functions of the central nervous system.
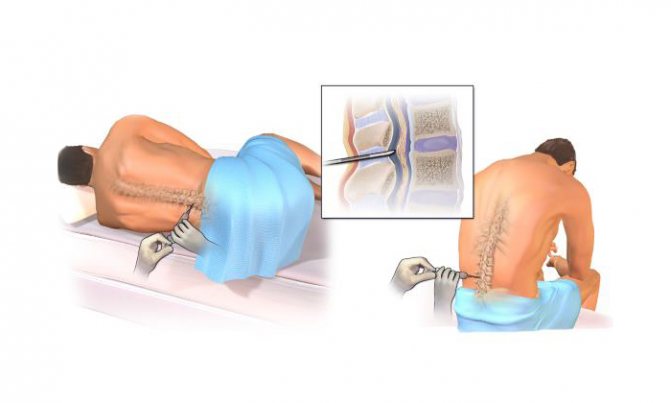
- Lumbar puncture for TBI. Analysis of the cerebrospinal fluid allows you to understand the cause of the coma.
- X-ray to track injuries to the spine and skull.
How does one recover from a coma?
Regardless of the severity of the traumatic brain injury, the patient is required to undergo a mandatory course of rehabilitation measures.
The primary task when recovering from a coma is to restore brain function.
Memory and attention deteriorate in all victims, and in some cases amnesia of varying duration develops. Confused consciousness and loss of spatial orientation make independent movements difficult. During the rehabilitation period, the patient is helped not only to move, but also to maintain a sitting position.
The procedure for further rehabilitation is individual and lasts from several months to several years.
Rehabilitation after traumatic brain injury
During the initial period of rehabilitation, a patient with a TBI is helped with self-care, restoring memories of lost skills.
The rehabilitation course is carried out under the guidance of:
- a psychologist who normalizes the psyche and allows you to re-enter society;
- a neurologist and physiotherapist responsible for carrying out massage procedures and exercise therapy that restore muscle tone;
- a neurospeech therapist who helps restore speech function;
- occupational therapist developing memory, speech and motor skills.
During rehabilitation after TBI, it is important to maintain consistency and frequency. The first improvements are an indicator of treatment effectiveness, but not effectiveness. Cancellation of restorative measures occurs only after agreement with the attending physician.
Long-term forecasts
Depending on the degree of damage to the central nervous system, the patient after TBI is diagnosed with the level of depression of consciousness:
- Stupor. Superficial coma, accompanied by a reaction to external stimuli, is treatable. With timely assistance, the victim comes out of a coma with minimal deviations.
- Sopor. Movements are carried out at the level of reflexes, and there is a violation of brain impulses. A rapid deterioration of symptoms is dangerous due to the transition to stage 3 damage to the central nervous system, but timely treatment and high-quality rehabilitation leave a high chance of a full life.
- Severe degree of central nervous system depression. The patient is in a vegetative state and needs hardware assistance. Disability cannot be avoided even with successful treatment.
- Death. Irreversible disorders in the central nervous system lead to extensive hemorrhages or hemorrhagic stroke.
The prognosis worsens when the coma is protracted, lasting for several years.
If the coma lasted several weeks or months, and after the return of consciousness there is a gradual restoration of lost functions, then the prognosis is favorable. Such patients are able to return to their normal lives without complications.
To normalize the patient’s condition, it is important to follow the actions recommended by the doctor throughout the entire period, even if its duration is more than a year.
( 1 rating, average 5 out of 5 )
Source: https://golovaibolit.ru/chmt/posledstvija-pri-chmt-posle-vyhoda-iz-komy
Characteristic symptoms
Coma after traumatic brain injury is primarily characterized by impaired consciousness. All symptoms of this condition can be divided according to the degree of its severity:
- Superficial disturbance of consciousness. The person falls into deep sleep. When trying to talk to the victim, he may open his eyes and sometimes start a conversation. Speech with punctuation. The patient can make slight movements of the limbs.
- Ordinary coma. The patient is able to make sounds, unintentionally open his eyes and make sudden movements with his hands. The doctor can fix the victim’s limbs with special devices to prevent physical harm.
- Deep coma. Reflexes, mobility and respiratory function are completely absent. There is no reaction to pain, just like there is to the light of the pupils.
The feasibility of maintaining body functions
Modern medicine makes it possible to artificially maintain the vital functions of the body for quite a long time, but the question often arises about the feasibility of these measures. This dilemma arises for relatives when they are informed that the brain cells have died, that is, in fact, the person himself. Often a decision is made to remove artificial life support.
Coma, from ancient Greek, means deep sleep, drowsiness. It is characterized by a lack of consciousness, motor activity and reflexes, inhibition of the vital processes of breathing and heartbeat. A patient in a coma is deprived of an adequate response to external stimuli, for example, touch or voice, or pain.
Treatment during coma
Once a diagnosis of coma due to traumatic brain injury has been made, appropriate treatment is begun. First of all, measures are taken to increase blood flow to the brain. Emergency treatment begins already in the ambulance.
Artificial ventilation is used and medications are introduced into the body to help normalize blood pressure. It requires the introduction of drugs that improve the functioning of organs such as the liver and kidneys.
In case of respiratory arrest, the emergency doctor inserts a special tube into the tracheal cavity, which is a conductor of oxygen air coming from the breathing apparatus.
Since, while in a coma, a person cannot eat on his own, nutrients are administered by tube. To prevent secondary infections of the urinary tract and lungs, powerful antibacterial drugs are prescribed.
Treatment
Treatment should always begin with identifying the source of oxygen deprivation, as the longer the absence, the more serious the damage can be. The doctor may use a tracheotomy to ensure adequate oxygen flow. Other treatment options may include surgery to remove the blockage or lesion, and steroids to reduce swelling in the brain.
A few days after injury, the focus should be on long-term recovery. Gray matter is highly adaptive to its environment, so ongoing challenges are the best way to help it recover and circumvent any resulting trauma. The treatment plan may include:
- Physical therapy to increase blood flow to the brain and restore motor function.
Occupational therapy to help you find new ways to complete everyday tasks.
Speech therapy to help restore lost speech and language.
Psychotherapy to help you learn to cope with trauma.
You may also need follow-up treatments, such as chemotherapy to further shrink brain damage, medications to prevent blood clots, or regular MRI scans to assess brain damage.
Every person can face a situation where someone suddenly feels ill. Having come to the rescue, first of all we feel for the presence of a pulse, thus checking whether the person’s heart is working or not.
Further first aid to the person will depend on whether the heart has stopped or not. The maximum time during which the body remains viable with further recovery is 15 minutes.
Rehabilitation period
Not all cases of impaired consciousness require a long rehabilitation period. According to statistics, recovery from a coma caused by diabetes, high doses of drugs or alcohol does not last long. In such cases, impaired consciousness is present before the toxic substance is eliminated from the body.
Coming out of a 3rd degree coma after a TBI or 1st degree equally requires rehabilitation measures. First of all, measures are taken to restore brain function. Not in every case, amnesia develops, but there is a deterioration in memory and attention.
How do you recover from a coma after a TBI? During this period, the ability to sit and walk without assistance and available means is lost. Confusion of consciousness is observed, the person loses orientation in space. The following specialists help correct such disorders caused by prolonged impairment of consciousness:
- neurologist (helps restore speech);
- psychologist (normalizes the psycho-emotional state);
- occupational therapist (helps improve motor skills);
- neurologist, physiotherapist, etc.
When recovering from a coma after a TBI, there is no need to immediately subject the patient to physical and mental stress on the first day. Rehabilitation should take place gradually. How many months or years it will take to fully restore the activity of the central nervous system, and what the prognosis will be, depends on the severity of the traumatic brain injury.
Rehabilitation after a coma consists of assisting the patient in all everyday activities: eating, going to the toilet and showering. Developmental games are required to help restore motor skills, memory, and speech. It is important to normalize your diet so that it includes all useful vitamins and microelements.
To restore muscle tone, massage procedures are prescribed, which are carried out in a specialist’s office and subsequently at home. During the massage, you can use any essential oil. The procedure also helps improve blood circulation. The main condition is continuity of therapy, even if the first positive changes are visible.
What is the danger of coma after a stroke?
» Articles from an expert » Brain
Coma after a stroke is a state between life and death associated with complete damage and disruption of the brain and all physiological systems. This is a kind of protective reaction of the body, which has an unsatisfactory prognosis. The likelihood of recovery from coma is rarely recorded and requires long-term rehabilitation.
Why does the patient fall into a coma?
Coma during a stroke is a consequence of an apoplexy, accompanied by cerebral hemorrhage and leading to an unconscious state with partial loss of reflexes.
There are hemorrhagic and ischemic strokes, characterized by damage to the blood vessels of the brain.
A person can reach this state due to a number of factors:
- internal cerebral bleeding that occurs when pressure increases in one of the segments;
- ischemia - insufficient blood supply to any organ;
- cerebral edema as a consequence of hormonal dysfunction and hypoxia of brain cells;
- atheroma (degeneration) of vascular walls;
- intoxication of the body;
- collagenoses, characterized by changes in connective tissues (capillaries);
- deposition (angiopathy) of beta-amyloid protein in the cerebral vessels;
- acute lack of vitamins;
- blood diseases.
Coma in ischemic stroke is diagnosed less frequently and is mainly accompanied by spontaneous recovery from it. With hemorrhagic hemorrhage, a coma is dangerous, as it leads to necrosis of large areas of the brain.
How to determine who
The literal meaning of the word coma is deep sleep. Indeed, a patient in a coma after a stroke looks like someone who is sleeping. The person lives, but it is impossible to wake him up, since there is no reaction at all.
There are a number of signs that allow you to distinguish coma from clinical death, fainting or deep sleep. These include:
- prolonged unconsciousness;
- weak brain activity;
- barely pronounced breathing;
- barely palpable pulse;
- lack of pupillary reaction to light;
- barely perceptible heartbeat;
- heat exchange disturbance;
- spontaneous bowel movements and urination;
- non-response to stimuli.
The above symptoms manifest themselves individually in each person. In some cases, the manifestation of basic reflexes continues. Partial preservation of spontaneous breathing sometimes does not require connection to devices, and the presence of swallowing functions allows you to refuse feeding through a tube. Often coma is accompanied by a reaction to light stimuli with spontaneous movements.
The comatose state develops rapidly. However, with ischemic stroke, early recognition of coma is possible.
The consequences of a stroke can be predicted if a person has the following symptoms:
- dizzy;
- vision decreases;
- drowsiness appears;
- consciousness is confused;
- yawning does not stop;
- severe headache;
- limbs go numb;
- movement is disrupted.
Timely response to alarming signs provides people with an additional chance at life and subsequently a favorable prognosis for the course of the disease.
Degrees of coma during stroke
Post-stroke coma is a fairly rare phenomenon (recorded in 8% of cases). This is a very serious condition. You can correctly predict the consequences by determining the degree of coma.
In medicine, there are 4 degrees of development of coma during strokes:
- The first degree is characterized by lethargy, manifested by a lack of response to pain and stimuli. The patient is able to make contact, swallow, roll over slightly, and perform simple actions. Has a positive prognosis.
- The second degree is manifested by suppression of consciousness, deep sleep, lack of reactions, constriction of the pupils, and uneven breathing. Spontaneous muscle contractions and atrial fibrillation are possible. The chances of survival are doubtful.
- The third, atonic degree is accompanied by an unconscious state and a complete absence of reflexes. The pupils become constricted and do not respond to light. Lack of muscle tone and tendon reflexes provokes cramps. Arrhythmia, decreased pressure and temperature, and involuntary bowel movements are recorded. The prognosis for survival is zero.
- The fourth degree is characterized by areflexia, muscle atony. Pupil dilation and a critical decrease in body temperature are recorded. All brain functions are impaired, breathing is irregular, spontaneous, with long delays. Restoration is not possible.
In a coma after a stroke, a person does not hear or respond to stimuli.
It is almost impossible to determine how long the comatose state will last. This depends on the severity and extent of brain damage, the location of the pathology and the cause of the stroke, its type, as well as the speed of treatment. Most often, the prognosis is unfavorable.
The average duration of a person's stay in a coma is 10-14 days, however, in medical practice, cases of many years of being in a vegetative state have been recorded.
It has been proven that if there is no oxygen supply to brain cells for more than a month, a person’s vitality is not restored.
Most often, death occurs 1-3 days after entering coma. The following factors determine the lethal outcome:
- a repeated stroke led to immersion in “deep sleep”;
- lack of reactions to sounds, light, pain;
- the patient's age is more than 70 years;
- decrease in serum creatinine to a critical level - 1.5 mg/dl;
- extensive brain disorders;
- necrosis of brain cells.
Laboratory blood tests, computer diagnostics or magnetic resonance imaging can provide a more accurate clinical picture.
Introduction to an artificial coma after a stroke
Sometimes it is necessary to switch off a person's consciousness with medication to prevent life-threatening brain changes.
In the event of compression pressure on brain tissue, swelling, or hemorrhages and bleeding resulting from traumatic brain injuries, the patient is placed in an artificial coma, which can replace anesthesia during times of crisis.
Long-term analgesia allows you to constrict blood vessels, reduce the tension of cerebral flow, and avoid necrosis of brain tissue.
Sedation is caused by the administration of a controlled high dose of special drugs that have a depressant effect on the central nervous system in intensive care conditions.
This condition can last a long time and requires constant monitoring of the patient's condition. Any reactions to external stimuli or movements indicate the possibility of returning consciousness.
The task of the medical staff is to provide assistance in recovering from a coma.
Introduction to sedation has side effects, including complications of the respiratory system (tracheobronchitis, pneumonia, pneumothorex), hemodynamic disorders, renal failure, and neurological pathologies.
Care and treatment of patients in a coma
With impaired consciousness, post-stroke coma is accompanied by spontaneous breathing and heartbeat. The duration of coma during a stroke cannot be predicted, so special care is required for the patient.
Here are some recommendations:
- Nutrition. Since comatose patients are fed through a special tube inserted into the stomach, the food must have a liquid consistency. Baby food is ideal for this: formula milk or fruit and vegetable purees in jars.
- Hygiene. To prevent the development of ulcers and bedsores and maintain body cleanliness, it is necessary to treat the patient’s skin daily with soapy water or special products, as well as clean the patient’s oral cavity with wet gauze wipes. Comb your hair daily (especially long hair) and wash your hair at least once a week.
- Change of position. To prevent bedsores, the patient should be systematically turned in different directions.
In case of extensive hemorrhagic stroke, surgical removal of the hematoma inside the brain is indicated, increasing the chances of recovery.
Coma resulting from an ischemic stroke is treated in a specialized intensive care unit of the neurological department. If life-support functions are impaired, the patient is connected to an artificial lung ventilation device (ALV) and a monitor that records the body’s parameters. Euthanasia is prohibited in Russia, so a person’s life will be maintained for as many days as required.
For ischemic stroke the following is prescribed:
- anticoagulants (aspirin, heparin, warfarin, trental);
- nootropic drugs (Cavinton, Mexidol, Actovegin, Cerebrolysin).
Recommendations for relatives of patients
A person emerging from a coma requires increased attention.
To avoid the recurrence of apoplexy, the following recommendations must be observed:
- inspire hope for recovery;
- create a favorable psychological climate and comfortable environment;
- motivate for daily exercise and praise for success;
- master manual massage skills.
Only love, care and attention can work miracles. Love and take care of yourself and your loved ones, and a favorable prognosis will not be long in coming.
Stroke
Complications
If the central nervous system was affected at the time of the traumatic brain injury, complications are likely to occur. Coma is one of them. With severe TBI, the consequences can be so serious that the patient will no longer be able to care for himself, stand up, or sit. In such cases, outside help and special medical equipment will be required.
Coma is not always accompanied by such severe consequences. In some cases, a person quickly recovers from injury and impairment of consciousness, and basic functions and reflexes return to normal.
The most common consequences of coma include amnesia or incomplete memory loss, impaired concentration, loss of the ability to independently care (eating, taking water procedures, etc.).
Being in a lying position for a long time, a person may begin to suffer from bedsores, which require other specific therapy using medications.
Causes
The sources causing damage to cerebral structures can be different.
The main ones are closed or open craniocerebral injuries caused by trauma.
Today, depression of the central nervous system caused by cancer, strokes and hemorrhage of various pathogenesis has become increasingly widespread.
The third most common causes are bacterial and viral infections that provoke inflammation and disruption of brain activity.
Distortion of consciousness can be caused by diabetes, hormonal disorders, abnormal changes in the functioning of the kidneys and liver.
Also, factors contributing to the development of a coma include intoxication and poisoning with potent poisons and substances: alcohol, drugs, medications.
Read also: Oxygen tube for breathing
Other consequences of TBI
The consequences of traumatic brain injury include not only coma. These depend on the severity of the damage. Complications do not always occur in the first weeks or months after injury. Sometimes negative consequences develop after a long time, which is more typical for children. In old age, TBI is often fatal.
The consequences of traumatic brain injury include:
- external manifestations: hematoma, tissue swelling, pain, fever, general malaise, etc.;
- partial or complete paralysis of the legs and/or arms;
- loss of sensitivity of the skin in the lower and/or upper extremities;
- chronic pain in the head;
- loss of visual, auditory, speech function, memory;
- impaired respiratory function, swallowing;
- inability to control urination and bowel movements;
- post-traumatic epileptic syndrome with the development of convulsive seizures, impaired consciousness;
- upper and lower extremities;
- impaired concentration;
- increased irritability.
Despite such a large list of negative consequences, this does not mean that a person will have all of them. The type of consequences depends on the exact location of the head and brain injury, as well as its severity.
Good afternoon I understand that it is too early to talk about results, but I would like to tell my story, maybe it will add faith to someone, because the most important thing is to believe. I got into an accident in a taxi from work. I was sitting in the back, but still found myself in an unlikely situation - another car flew into the taxi from the side - one might say, into me. The taxi driver is not to blame; he was driving according to the rules. My diagnosis: combined trauma. CCI. Severe brain contusion with the formation of ICH in the insular region on the right. SAC. Contusion of the soft tissues of the face and scalp. Coma 2 (SH 6 b.); ZTG. Lung contusion. Bilateral hydrothorax. Heart bruise. Multiple fractures of the pelvic bones. Fracture of the lateral mass of the sacrum on the right. I can’t describe what my loved ones experienced while I was in a coma (14 days), but it’s clear that nothing good. For me, it all started 14 days later, when I regained consciousness. At first I thought that I was flying on a plane (my work involves flying) and something happened to it and I was in another city. Then they told me more than once a day that I had been in an accident (and I immediately forgot and asked again what happened), I even pretended for a time that I believed it. In fact, I thought I was being deceived for some reason. And yet nothing is possible. Even sit. The brain realized its sad situation about a month after the accident, by the time of discharge from the first hospital. I was sent home to wait for the “bones to heal.” They grew together after 2 months, I stood up and felt the full weight of my legs. I was immediately sent to neurorehabilitation. A very good impression of it, a place where you don’t feel like you’re some kind of abnormal, everyone there is in a difficult situation. You work on recovery almost around the clock. For me, it was important to get up early and start helping myself recover earlier, and go to bed later for the same purpose. I got enough sleep and didn’t sleep during the day—the accompanying nootropic drugs helped with this. Even while I was waiting in line for physical procedures (or any line), I stood on one leg as best I could, because... There was hemiparesis with all the consequences. I was discharged from rehabilitation in a state of “walking almost straight”, the progress was enormous. But in rehabilitation I worked hard: I walked up the stairs if I had a free minute, juggled (I read somewhere that this is how brain cells grow) as best I could, wrote as best I could, etc. I limited visits to loved ones, because... it took up so much valuable time from me. Then I plowed at home: the home gym grew larger (stepper, 2 and 5 kg weights, leg weights (1.5 kg each), elastic band for resistance. Walking up stairs. Don’t feel sorry for yourself - it won’t change anything! Tears (and their at first I poured it in buckets) won’t help either! You have no choice - nothing will change without your efforts, you simply have no choice! Now: the bones have fused - sometimes I walk in 12 cm heels even on the street; the hemiparesis has almost gone away - I go to the gym hall already, I feel a little paresis in two fingers in front of the nails. There is still paresis of the vocal cords (the voice has not yet returned to normal - like a cold, breathing is suffering - but it has already become better) - Laura does not know whether it is from prolonged mechanical ventilation, or from a brain catastrophe, There is no damage to the larynx. I went through acupuncture, physical procedures, I do phonetic exercises - no one will do them for me - I work hard. Result - 5 months on sick leave. Today I was discharged, I go to work on Monday) I really miss work))) And most importantly - believe. A person can do almost anything - the main thing is motivation. The only thing he can be limited in is time. Don't force it, this is important. 03/19/2017 16:36:53, Helena59
I would like to chat with you. Please write to me at 89050247349 12/26/2018 13:39:53, Fluffy
Until now, despite the achievements of modern intensive therapy, more than 40% of victims die from cerebral coma, and many of the survivors remain deeply disabled
.
The severity of brain damage depends on the nature of the injury itself (impact, gunshot wound, fall from a height, sudden braking while driving a car). Depending on the direction of the blows and other factors, different parts of the brain are damaged to a greater or lesser extent. The severity of the damage is also determined by the occurrence of general reactions of the body to the injury (shock, respiratory failure, infection).
If the brain is damaged in the area of its trunk, where the centers of respiration and blood circulation are located, the victim usually dies at the scene of the disaster
. If even very large areas of the brain and other parts are damaged, recovery can be achieved if the harmful effects of secondary factors are prevented. Brain tissue reacts to injury with circulatory disorders and swelling. This leads to an uneven increase in its parts and the so-called wedging. When respiratory failure occurs, blood circulation worsens, respiratory failure worsens blood circulation and harmful reactions intensify many times over, which leads to irreversible changes in the brain and its death.
Clinical picture
Traumatic brain injury can cause concussion, contusion and hemorrhages into the cranial cavity and directly into the brain tissue
. It is these injuries, together with cerebral edema, that determine the clinical picture (a greater or lesser degree of loss of consciousness, paralysis, focal symptoms).
In case of severe traumatic brain injury, the functions of vital organs are always affected: breathing, blood circulation, hemostatic system, protective mechanisms; trophic disturbances rapidly increase
.
Impaired respiratory function in TBI occurs due to cerebral edema and dislocation of the brain stem, obstruction of the upper respiratory tract due to inhibition of protective reflexes against the background of impaired consciousness. The protective reflexes of the respiratory system include pharyngeal, laryngeal and cough, when suppressed there is a high probability of aspiration (saliva, blood, gastroduodenal contents) with the subsequent development of aspiration pneumonia or acute respiratory distress syndrome.
In patients with TBI, ventilation failure occurs due to hypoventilation or pathological breathing rhythms (bradypnea, tachypnea, Kussmaul, Cheyne-Stokes, Biotta), hypoxia and hyper- or hypocapnia
. Hypoxia leads to disruption of cerebral hemodynamics and increased intracranial pressure.
When examining patients in this case, pale skin (especially the face), vomiting, involuntary urination and defecation, and bradycardia are noted. In some types of lesions (traumatic epidural and subdural hematoma), a so-called lucid interval is observed when the patient regains consciousness. Then his condition sharply worsens, anisocoria, increasing hemiparesis are noted, and convulsions may develop. Unfortunately, in approximately half of the cases, the picture of traumatic brain lesions can be erased by concomitant alcohol intoxication. In this case, a traumatic coma can be suspected on the basis of concomitant lesions: wound surfaces, hematomas, bruising in the orbital area may be observed - a “symptom of glasses”, bleeding and leakage of liquor from the ears, nose, mouth. The most severe are open craniocerebral injuries.
Diagnostics
Examination of the fundus of the eye (congestive optic disc, radiography of the skull in two projections, electroencephalography and echoencephalography) helps in diagnosis.
Emergency care and treatment
The main task at the scene is to improve breathing and circulation to prevent secondary brain damage.
For this you need:
- free the airways from foreign bodies;
- ensure their free passage throughout the entire transportation to the hospital. Ensuring the patency of the upper respiratory tract consists of preventing tongue retraction: positioning the victim on his side, moving the lower jaw, freeing the upper respiratory tract from mucus, blood, vomit, installing an air duct. Removable dentures should be removed;
- in case of ventilation problems, mechanical ventilation is performed using manual or automatic devices, preferably with the addition of oxygen;
- when shock develops, plasma-substituting solutions are administered, but care is taken to ensure that there is no excessive increase in pressure, since the brain with TBI is very sensitive to high blood pressure, which can increase edema.
It is necessary to strive to deliver the victim to a hospital where there is a computed tomograph, angiography equipment and a neurosurgical department
. In the hospital, they continue to ensure sufficient gas exchange and maintain the necessary blood circulation. The patient undergoes tracheal intubation while receiving atropine and muscle relaxants.
One of the main methods of treating victims with TBI is mechanical ventilation, which allows normalizing gas exchange and blood flow. In case of severe TBI, there is a need for prolonged mechanical ventilation, which is a reliable way to prevent and treat cerebral edema.
See comatose states
Saenko I. A.
Sources:
- Nurse's Handbook for Care/N. I. Belova, B. A. Berenbein, D. A. Velikoretsky and others; Ed. N. R. Paleeva. - M.: Medicine, 1989.
- Zaryanskaya V. G. Fundamentals of resuscitation and anesthesiology for medical colleges (2nd ed.) / Series “Secondary vocational education”. - Rostov n/D: Phoenix, 2004.
Many people die at a young age.
The reasons may be different, but most often it is injury.
Among all types of injuries, 50% belong to skull injuries.
Traumatic brain injury is a violation of the integrity of the skull
and intracranial formations such as vessels, nerves, brain tissue and membranes.
Ischemic stroke: symptoms, consequences, treatment
Ischemic stroke is not a disease, but a clinical syndrome that develops due to general or local pathological vascular damage. This syndrome accompanies diseases such as atherosclerosis, coronary artery disease, hypertension, heart disease, diabetes mellitus, and blood diseases. Ischemic cerebral stroke (or infarction) occurs when cerebral circulation is disrupted and is manifested by neurological symptoms within the first hours from the moment of occurrence, which persist for more than a day and can lead to death.
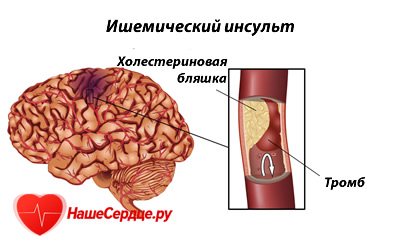
Of the three types of strokes: ischemic, hemorrhagic stroke and subarachnoid hemorrhage, the first type occurs in 80% of cases.
Forms of ischemic stroke
The appearance of this syndrome is caused by the shutdown of a certain part of the brain due to the cessation of its blood supply. The classification reflects the reason for its occurrence:
- thromboembolic - the appearance of a blood clot clogs the lumen of the vessel;
- hemodynamic - prolonged vascular spasm causes the brain to receive less nutrients;
- lacunar - damage to a small area, no more than 15 mm, causes minor neurological symptoms.
There is a classification according to the lesion:
- Transient ischemic attack. A small area of the brain is affected. Symptoms disappear within 24 hours.
- Minor stroke – restoration of function occurs within 21 days.
- Progressive – symptoms appear gradually. After restoration of function, neurological residual effects remain.
- Complete or extensive ischemic stroke - symptoms continue for a long time and after treatment there are persistent neurological consequences.
The disease is classified according to severity: mild, moderate and severe.
Causes of ischemic stroke
Most often, stroke occurs in men between 30 and 80 years of age who smoke and are constantly exposed to stress. The causes of ischemic stroke include the following diseases: obesity, hypertension, coronary artery disease, various arrhythmias, blood coagulation disorders, vascular diseases (dystonia), diabetes mellitus, atherosclerosis, pathology of the neck and head vessels, migraine, kidney disease.
When these factors combine, the risk of stroke increases significantly. From the medical history: ischemic stroke occurs during and after sleep, and can often be preceded by: psycho-emotional overload, prolonged headache, alcohol consumption, overeating, blood loss.
Main symptoms
Symptoms of ischemic stroke are divided into general cerebral, characteristic of any stroke, and focal - those symptoms that can be used to determine which area of the brain is affected.
With any stroke, the following always occur:
- loss of consciousness, less often - agitation;
- disorientation;
- headache;
- nausea, vomiting;
- fever, sweating.
These symptoms are accompanied by signs of ischemic stroke. The severity and extent of the lesion is determined by the severity of focal symptoms. There are violations:
- Movement – weakness or inability to make normal movements of the upper and (or) lower limbs on one or both sides – paresis.
- Coordination – loss of orientation, dizziness.
- Speech – inability to understand speech (aphasia) and use the speech apparatus: slurred pronunciation – dysarthria, reading impairment – alexia, “lack” of writing skills – agraphia, inability to count to 10 – acalculia.
- Sensitivity - a crawling sensation.
- Vision – decreased, loss of visual fields, double vision.
- Swallowing - aphagia.
- Behavior – difficulty in performing basic functions: combing one’s hair, washing one’s face.
- Memory - amnesia.
With an ischemic stroke of the left hemisphere, sensitivity is impaired, muscle tone decreases and paralysis of the right side of the body occurs. It is when this area is damaged that patients may either lack speech or incorrectly pronounce certain words. If a stroke occurs in the temporal lobe, patients become depressed, do not want to communicate, their logical thinking is impaired or absent, so sometimes difficulties arise in making a diagnosis.
All these symptoms appear over a period of time, so several periods are distinguished in the development of a stroke: acute - up to 6 hours, acute - up to several weeks, early recovery - up to 3 months, late recovery - up to 1 year, period of consequences - up to 3 years and long-term consequences – more than 3 years.
Diagnosis of stroke
Timely and accurate diagnosis of this disease makes it possible to provide correct assistance in the acute period, begin adequate treatment and prevent serious complications, including death.
First, basic studies are carried out: a clinical blood test, an ECG, a biochemical blood test to determine urea, glucose, its electrolyte and lipid composition and the coagulation system. It is necessary to examine the brain and cervical spine using CT and MRI. The most informative method is MRI, which will accurately indicate the site of the lesion and the condition of the vessels supplying this area. A CT scan will show the area of the infarction and the consequences of the stroke.
Basic principles of treatment
Treatment of ischemic stroke should be timely and long-term. Only with this approach is it possible to partially or completely restore brain functionality and prevent consequences. Early consequences after an ischemic stroke of the brain include: cerebral edema, congestive pneumonia, inflammation of the urinary system, thromboembolism, bedsores.
Within the first 6 hours, patients are hospitalized in specialized wards of the neurological or intensive care unit. Treatment of ischemic stroke begins with the elimination of acute disorders of the respiratory and cardiovascular systems. If necessary, the patient is intubated and placed on artificial respiration. It is important to restore blood supply to the brain, normalize acid-base and water-electrolyte balance. 24-hour monitoring of respiratory function, cardiac and vascular activity, homeostasis is carried out - monitoring of blood pressure, ECG, heart rate, hemoglobin content in the blood, respiratory rate, blood sugar, body temperature. The main measures are aimed at reducing intracranial pressure and preventing cerebral edema. Prevention of pneumonia, pyelonephritis, thromboembolism, and bedsores is carried out.
Specific treatment for ischemic cerebral stroke consists of improving cerebral microcirculation and eliminating the causes that interfere with the delivery of nutrients to neurons.
Thrombolysis for ischemic stroke is the most effective technique if it is carried out in the first 5 hours after the onset of the stroke. It is based on the concept that during a stroke, only a part of the cells are irreversibly damaged - the ischemic core. Around it there is an area of cells that are turned off from functioning, but remain viable. When prescribing drugs that act on the blood clot, liquefy and dissolve it, blood flow is normalized and the function of these cells is restored. In this case, the drug used is Actilyse. It is prescribed only after confirmation of the diagnosis of ischemic stroke intravenously, depending on the patient’s weight. Its use is contraindicated for hemorrhagic stroke, brain tumors, a tendency to bleeding, decreased blood clotting, and if the patient has recently undergone abdominal surgery.
The main drugs for the treatment of ischemic stroke are:
- Anticoagulants – heparin, fragmin, nadroparin.
- Blood thinners - aspirin, cardiomagnyl.
- Vasoactive drugs - pentoxifylline, vinpocetine, trental, sermion.
- Antiplatelet agents – Plavix, Tiklid.
- Angioprotectors – etamsylate, prodectin.
- Neurotrophics – piracetam, cerebrolysin, nootropin, glycine.
- Antioxidants – vitamin E, vitamin C, mildronate.
Treatment of ischemic stroke on the right side does not differ from the treatment of ischemic stroke on the left side, but therapy must have an individual approach and various combinations of medications that are prescribed only by a doctor.
Nutrition after stroke
In addition to drug therapy and proper care, the success of recovery depends on what products the patient consumes. Nutrition after an ischemic stroke should be such as not to provoke another attack and prevent possible complications.
You need to eat 4-6 times a day. Food should be low in calories, but rich in proteins, vegetable fats and complex carbohydrates. To prevent constipation, it is necessary to consume large amounts of plant fiber. Raw vegetables - spinach, cabbage, beets - improve biochemical processes in the body, so they should be on the menu in sufficient quantities. It is necessary to consume blueberries and cranberries daily, as they help quickly remove free radicals from the body.
No special diet has been developed after ischemic stroke. Basic recommendations: less salt, consumption of smoked, fried, fatty, flour products is excluded. And therefore, the main products for patients are: lean meats, fish, seafood, dairy products, cereals, vegetable oils, vegetables, fruits.
Rehabilitation measures after a stroke

Stroke is one of the important medical and social problems of the state due to high mortality, disability of patients, difficulty, and sometimes impossibility of adapting to normal life. Ischemic stroke has dangerous consequences: paresis and paralysis, epileptic seizures, impaired movement, speech, vision, swallowing, and the inability of patients to care for themselves.
Rehabilitation after an ischemic stroke is measures aimed at the social adaptation of the patient. Treatment with drugs during the rehabilitation period should not be excluded, since they improve the prognosis of recovery after ischemic cerebral stroke.
The recovery period is an important period in treatment measures after cerebral infarction. Since after a stroke most of the body’s functions are impaired, the patience of the family and time are needed for their full or partial recovery. For each patient after the acute period, individual rehabilitation measures after an ischemic stroke are developed, which takes into account the characteristics of the course of the disease, the severity of symptoms, age and concomitant diseases.
It is advisable to carry out recovery after an ischemic stroke in a neurological sanatorium. With the help of physiotherapy, exercise therapy, massage, mud therapy, acupuncture, motor and vestibular disorders are restored. Neurologists and speech therapists will help in the process of restoring speech after an ischemic stroke.
Treatment of ischemic stroke with folk remedies can only be carried out during the recovery period. It may be advisable to include dates, berries, citrus fruits in your diet, drink a tablespoon of a mixture of honey and onion juice after meals, tincture of pine cones in the morning, take baths with rosehip infusion, drink mint and sage infusions.
Treatment after a stroke at home is sometimes more effective than hospital treatment.
Prevention and prognosis of ischemic cerebral stroke
Prevention of ischemic stroke is aimed at preventing the occurrence of a stroke and preventing complications and recurrent ischemic attacks. It is necessary to promptly treat arterial hypertension, conduct an examination for heart pain, and avoid sudden increases in blood pressure. Proper and nutritious nutrition, quitting smoking and drinking alcohol, and a healthy lifestyle are the main things in preventing cerebral infarction.
The prognosis for life with ischemic stroke depends on many factors. During the first weeks, 1/4 of patients die from cerebral edema, acute heart failure, and pneumonia. Half of the patients live 5 years, a quarter – 10 years.
Video about ischemic stroke:
Consequences of injury
Traumatic brain injury can have serious consequences.
Our brain receives and processes a large amount of information, so the consequences of injury can be completely different. In some cases, it is impossible to draw a conclusion, since symptoms may appear only after a day.
For example, or cerebral edema.
Doctors classify the consequences into acute disorders that occur immediately after injury and long-term consequences of traumatic brain injury that occur after a certain period.
Pinching of the facial and trigeminal nerves occurs no less often.
Classification of traumatic brain injury
If during injury the skin of the skull is not broken and the intracranial cavity remains closed, this is a closed injury.
Open injury
is a consequence of severe mechanical damage, as a result of which the processes of interaction with the external environment are disrupted, the meninges are damaged with a high probability of infectious infection.
A closed head injury has less dire consequences than those that can occur with an open injury, since the head cover remains intact and injuries of this type are aseptic.
An open head injury can have more severe consequences. Most often, severe conditions manifest themselves in the form of:
- Concussions (commotion).
Occurs when struck by a wide object, within a couple of seconds. As a rule, the scalp is not damaged, but attacks of vomiting and dizziness may occur. There are disturbances in the interaction between different parts of the brain. Loss of consciousness and amnesia of varying degrees of duration are possible. - Brain contusion (concussion)
comes in three degrees of complexity: mild, moderate and complex. It is damage to the brain in a specific location and can cause both minor hemorrhages and rupture of brain tissue. Contusion occurs when one of the cranial fragments damages the bones of the skull. Clinical symptoms appear instantly: prolonged loss of consciousness, amnesia, local neurological symptoms. In particularly severe cases of injuries of this type, consequences may occur at certain intervals. For example, epilepsy, speech disorders or coma. - Compression in the cranium
of the brain due to swelling, effusion of blood, or when the bone is pressed into the cavity. Headaches, drowsiness and nausea occur, and heart function may be impaired. - Diffuse axonal brain injury
, which manifests as a coma for up to three weeks, which can progress to a vegetative state.
Emergency medical care for traumatic brain injury:
Symptoms and signs
The manifestations of symptoms depend on the location of the hematoma, its type, size, and growth rate.
Increased intracranial pressure and brain displacement play a dominant role in the symptoms. In the acute course of the disease, symptoms appear immediately. Manifestations of subacute hematomas are usually milder. In a chronic course, signs of the disease appear gradually; the process can take from several weeks to several months.
In acute subdural hematoma the following are observed:
- increase in blood pressure,
- convulsions,
- paresis and paralysis,
- breathing disorders,
- loss of consciousness,
- coma,
- different pupil sizes (anisocoria),
- headaches accompanied by vomiting.
The most dangerous consequences
All traumatic brain injuries are usually divided into three degrees of severity
: mild, moderate and severe traumatic brain injury, the consequences of which are almost always irreversible.
Severe traumatic brain injury has the most dangerous consequences, such as
diffuse axonal damage, contusion and compression of the brain, falling into a coma and a vegetative state.
Severe contusion of the telencephalon is when a person is unconscious for 2 weeks
, while vital functions also change the rhythm of their activity.
From a neurological point of view, the brain stem is especially damaged, as a result of which unclear movements of the eyeballs, a violation of the swallowing reflex and muscle tone may be observed.
Severe injury is often accompanied by a fracture of the skull vault and hemorrhage into the cavity of the cranium.
Nothing more than a consequence of compression of the brain.
Hematomas most often occur epidermal and subdural.
The most important thing in such a situation will be diagnosis carried out on time. If the hematoma is not complicated and has a “light period,” then the victim will begin to come to his senses after some time.
Hematoma against the background of coma is much more difficult to recognize, and it can only be explained by bruise of brain tissue. As hematomas form and grow inside the skull, a tentorial hernia can develop, which is a protrusion of the brain into the opening through which the brain stem passes.
If the compression continues for a long period, the oculomotor nerve is affected, without the possibility of recovery.
The absence of normal physiological functioning of the cerebral cortex is called a vegetative state of the brain.
Only the functions of the brain stem and reticular formation are preserved, so the changes in the phases of sleep and wakefulness continue to work as usual. When awake, a person lies with his eyes open, but is not in contact with the world around him.
If the dysfunction of the cortex is reversible, then the patient’s consciousness can gradually be restored, then psychosensory and psychomotor activity is reintegrated, and after some time the person returns to full consciousness.
Unfortunately, damage is not always reversible. In such cases, a persistent vegetative state of the large brain rapidly develops.
Human life continues only with the help of artificial drugs
, which support the normal functioning of the respiratory, cardiovascular and excretory systems.
Death is almost inevitable.
Traumatic brain injury and coma
Falling into a coma is also a dangerous consequence of traumatic brain injury. In a state of coma, a person is unconscious, the functions of the central nervous system are suppressed, consciousness is lost, and all vital human systems are gradually suppressed.
There are three types of coma:
Determination of the level of coma
Restoration of impaired or lost functions of the central nervous system is possible only after establishing the cause of the coma and its type. The first assessment of the victim’s condition is carried out before emergency care is provided.
Diagnosis of a patient with TBI in a coma includes:
- collecting anamnesis - interviewing the victim’s relatives, witnesses of the accident, collecting data from the patient’s medical record;
- physical examination - examination of the skin and mucous membranes, assessment of the functioning of the respiratory and circulatory system, checking the fundus of the eye and the reaction of the pupil to light. Additionally, the likelihood of spinal injuries is determined, and certain types of palpation and percussion of the body are used. They are necessary to exclude pathological enlargement of organs and the presence of internal bleeding;
- neurological tests - include checking the level of unconsciousness, eye reaction, establishing the degree of motor activity and tendon reflexivity. Muscle tone is assessed, asymmetry of the facial areas is excluded;
- laboratory and hardware tests - X-ray of the skull, MRI, CT, EEG, angiography, lumbar puncture, measurement of intracranial pressure.
If necessary, the attending physician may prescribe additional diagnostic tests. The manipulations are repeated regularly to monitor the dynamics of the patient’s condition.