Chronic cerebrovascular accident (cerebral vascular insufficiency) is characterized by a decrease in blood supply to the brain. This condition is very common among older people in developed countries due to the high prevalence of atherosclerosis. In most cases, the carotid artery is damaged. A pair of carotid arteries, one on each side of the neck, running parallel to the jugular vein, are the main arteries that supply blood to the brain.
As a rule, cerebral vascular insufficiency develops in the area of the bifurcation of the carotid artery - the splitting of the carotid artery into internal and external branches. This splitting is similar to a stream that has split into two streams. In bifurcation, as well as during bifurcation in a water flow, accumulation of slag occurs. Severe symptoms begin to appear in most cases only when the artery blockage reaches 90 percent. This situation is similar to what happens with coronary heart disease.
Symptoms of chronic cerebrovascular accident are caused by decreased blood flow and oxygen supply to the brain. Stopping the flow of blood and oxygen leads to a stroke. The official definition of stroke is "loss of nerve function for at least 24 hours due to lack of oxygen." Some strokes are mild; others result in paralysis, coma, or speech impairment, depending on what part of the brain is involved. Mini-strokes, or transient ischemic attacks, can result in loss of nerve function for an hour or more, but less than 24 hours. TIAs can lead to transient symptoms of cerebral vascular insufficiency: dizziness, ringing in the ears, blurred vision, confusion, and so on.
Atherosclerosis is one of the main causes of cerebrovascular insufficiency. As this process progresses, high cholesterol levels combined with inflammation in the walls of the arteries in the brain can cause cholesterol to accumulate on the vessel wall in the form of a thick, waxy plaque. This plaque can restrict or completely prevent blood flow to the brain, causing stroke, transient ischemic attacks, or dementia, which can lead to a variety of other health complications.
The most common forms of cerebrovascular disease of the brain are thrombosis (40% of cases) and cerebral embolism (30%), followed by cerebral hemorrhages (20%).
Another form of cerebrovascular disease includes aneurysms. In women with defective collagen, weak key arterial branch points result in ridges with a very thin endothelial covering that can easily rupture with minimal increase in blood pressure. It can also occur with poor capillaries caused by cholesterol deposition in tissues, especially in hypertensive patients with or without dyslipidemia. If bleeding occurs, the result is a hemorrhagic stroke in the form of subarachnoid hemorrhage, intracerebral hemorrhage, or both.
A drop in blood pressure during sleep can lead to a marked decrease in blood flow in narrowed blood vessels, causing ischemic stroke in the morning. Conversely, a sharp increase in blood pressure due to daytime agitation can lead to rupture of blood vessels, resulting in intracranial hemorrhage. Cerebrovascular disease primarily affects people who are elderly or have a history of diabetes, smoking, or coronary heart disease.
Symptoms
Symptoms of a cerebrovascular accident depend on the degree of damage to brain cells and the location of the area of the brain with impaired blood flow. In acute cerebrovascular accidents (hemorrhagic or ischemic stroke), movement disorders such as hemiplegia or hemiparesis develop.
In chronic cerebral circulatory disorders (also called discirculatory encephalopathy), symptoms develop gradually and are manifested by symptoms such as memory impairment, dizziness, headaches. At first, the patient does not have any impairment of intellectual abilities. But as there is a chronic lack of oxygen in the brain tissue, memory impairment begins to progress, personality disorders arise, and intelligence decreases significantly. Subsequently, the patient develops severe intellectual-mnestic and cognitive impairments and dementia develops; extrapyramidal disorders and cerebellar ataxia may also develop.
Consequences of cerebral circulatory disorders
The brain is the organ most vulnerable to lack of oxygen. The circulating blood volume in the brain remains virtually unchanged and is about 750 ml. Since nervous tissue is not able to retain oxygen, its reserve lasts for 8–10 seconds. When brain cells are deprived of blood supply, that is, there is no access to vital nutrients and oxygen, they die - a stroke occurs.
The consequences of a stroke can vary widely depending on the area of the brain, the severity of the impairment, and the general health of the person.
Cerebral circulatory disorders include:
- cerebral hemorrhage,
- thrombosis,
- embolism (blockage),
- subarachnoid hemorrhage.
They are usually the result of pre-existing vascular disease, congenital pathology, or may be triggered by trauma.
Causes
Chronic cerebral circulatory failure is most often associated with atherosclerosis, hypertension, and heart disease accompanied by chronic circulatory failure. In addition, CNMK may be associated with vascular anomalies and diseases (vasculitis), venous anomalies, diabetes mellitus and various blood diseases, which result in chronic cerebral hypoxia.
Also, chronic cerebrovascular accident occurs as a consequence of acute cerebral circulatory disorders such as ischemic or hemorrhagic stroke.
An ischemic stroke occurs when a blood vessel that supplies blood to the brain is blocked by a blood clot. A clot can form in an artery that is already narrowed. Also, a clot can break off from the wall of a vessel somewhere in the body and travel through the bloodstream to the brain.
Ischemic strokes can also be caused by blood clots that form in the heart. These clots travel to the brain through the bloodstream and can become lodged in small arteries in the brain.
Certain medications and medical conditions can increase blood clotting and cause blood clot formation and increase the risk of ischemic stroke. A hemorrhagic stroke occurs when a blood vessel in a certain part of the brain becomes weak and ruptures, causing blood to leak into the brain and the blood damages brain cells. Some people have defects in the blood vessels in the brain that make a hemorrhagic stroke more likely.
Causes of deterioration of blood circulation in the brain
In some pathologies, stenosis (narrowing) of the lumen of the vessel or its obstruction (blockage) occurs. As a result, the speed of blood flow slows down, ischemia (oxygen starvation of the tissue) occurs in certain areas of the brain, leading to necrosis (death) of the tissue.
Risk factors are:
- hypertension;
- cardiac ischemia;
- diabetes;
- hormonal imbalance, including the use of contraceptives;
- atherosclerosis;
- overweight;
- physical inactivity;
- stress;
- alcohol abuse, smoking;
- lipid metabolism disorder.
Diagnostics
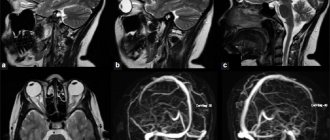
The diagnosis of chronic cerebrovascular accident is made based on a combination of examination data, symptoms, neurological signs, results of brain neuroimaging (MRI, or MSCT), and angiography of cerebral vessels.
The doctor may detect the presence of certain neurological, motor, and sensory deficits, such as changes in vision or visual fields, abnormal reflexes, abnormal eye movements, muscle weakness, decreased sensation, and other changes. In addition, certain tests help determine the presence of intellectual-mnestic disorders.
Laboratory research methods are prescribed for the diagnosis of somatic diseases.
How to recognize a stroke?
It often happens that pedestrians, disgustedly swearing at a fallen “drunkard,” pass by, not even suspecting that the person is not drunk at all, but has suffered a stroke.
It is no less difficult to understand what is happening to a loved one who suddenly falls, begins to speak “through cotton wool” or loses consciousness.
A simple “ test ” will help you recognize a stroke in time, which you should remember in order to possibly have time to save the life of a loved one or a stranger.
So, we ask the patient...
- Just smile . Yes, from the outside it may seem like a mockery, but a “clumsy” smile will immediately indicate the development of a stroke, in which the corners of the mouth will rise “crookedly” - unevenly, and asymmetry will be noticeable on the face.
- Speak . Another obvious symptom of a stroke is impaired speech. The patient simply will not be able to speak as usual, and even simple words will be difficult to speak.
- Show tongue. A sign of a stroke will be the curvature of the tongue and its deviation to one side.
- Raise your hands. If a person has a stroke, his arms will be raised asymmetrically or he will not be able to raise them at all.
If all the signs coincide, there is no doubt about a stroke - and urgently call an ambulance .
Naturally, the dispatcher should be warned about the stroke!
Treatment
If there are diseases such as hypertension, diabetes mellitus or other diseases, then, first of all, it is necessary to compensate for the underlying disease.
To treat chronic cerebrovascular accidents, various medications are used - vascular drugs (Trental, Cavinton, Sermion, etc.), nootropics, metabolic drugs, antioxidants. To prevent the formation of blood clots, antiplatelet agents such as aspirin, dipyridamole are prescribed. For high cholesterol levels in the blood Statins may be used.
Sometimes surgical treatment is required to eliminate the blood flow disorder - for example, carotid endarterectomy. Treatment methods such as carotid angioplasty and stenting are also used.
Hemodynamic disturbances are caused by the degree of decrease in heart rate, an increase in diastolic filling and an increase in systolic pressure in the ventricles, aorta and pulmonary artery, as well as the presence and degree of myocardial damage and dysfunction. Systolic blood pressure can reach 170-200 mmHg. Art. An inadequate increase in stroke volume with a rare heart rate (especially if there are organic changes in the myocardium) does not provide compensation, and a decrease in MOS is observed. When the heart rate is above 40/min and in the absence of myocardial damage, MVR at rest remains within normal limits. For example, in elderly patients, disturbances in intracardiac blood pressure due to valvular dysfunction due to atherosclerosis, calcification and valve deformation may have a certain significance - most often it is mitral insufficiency, stenosis and insufficiency of the aortic valve.
Morgann-Adams-Stokes attacks occur with complete AV block and ventricular asystole (blockade at the output of impulses from the autonomous center in the ventricles) or a progressive decrease in the ectopic rhythm (up to 20-15 beats/min). Their cause may also be ventricular fibrillation against the background of complete AV blockade during acute myocardial infarction. (Morgagni-Adams-Stokes syndrome - see page 60.)
Subjective symptoms:
- sometimes absent if there is compensation for HD (with AV block of the first degree, proximal AV block of the second degree, type II or congenital AV block of the third degree with a nodal replacement rhythm of 40-60 per minute), or may be due to other reasons (acute coronary insufficiency, increased blood pressure, etc.)
- palpitations, feeling of cardiac arrest
- severe weakness, fatigue
- headaches, dizziness, dark circles before the eyes, fainting
- feeling of heaviness, pain in the heart, angina pectoris
- increased pulsations in the neck and head
- shortness of breath and other manifestations of heart failure
- Objective symptoms of AV block II (type II) and III degree:
- bradycardia with regular rhythm (heart rate usually less than 40 per minute)
- intermittent accentuation of the 1st tone (Strazhesko's cannon tone) and individual strong pulsations of the neck veins, coinciding with the 1st tone (with complete AV block)
- dull atrial sounds and weak pulsations of the jugular veins during diastole
- arterial pulse equal to heart rate, good filling, steep difference in pulsation frequency of the neck veins and arterial pulse
- arterial systolic hypertension with low diastolic blood pressure
- attacks of Morgagni-Adams-Stokes syndrome with a sharp slowdown in heart rate (heart rate is usually less than 20 per minute)
- signs of underlying heart disease and circulatory failure
Varieties of PNMK
Transient disturbances of cerebral blood flow can occur as transient ischemic attack and hypertensive cerebral crisis. A transient ischemic attack (popularly called a microstroke) is an acute disruption of the blood supply to the brain tissue due to blockage of a small arterial vessel. Patients with such disorders begin to feel neurological symptoms characteristic of damage to the brain centers, which are precisely what the “problem” artery supplies with blood. Hypertensive cerebral crisis is a sharp increase in blood pressure (in hypertensive patients above their usual high pressure), accompanied by temporary neurological disorders and various symptoms of cardiac dysfunction.
What should emergency doctors do after arriving at a patient?
- After assessing the patient’s condition, he must be hospitalized.
- The patient is hospitalized only in the “lying” position.
- In case of ischemic stroke, they are usually taken to the neurology department, and in case of hemorrhagic stroke, they are taken to neurosurgery. But first of all - to the intensive care unit.
- Immediately after hospitalization, diagnostics are carried out to quickly determine the type of stroke and its location.
- As first aid, drug therapy is carried out aimed at reducing blood pressure, eliminating vasospasm, and restoring impaired functions.
- The measures also include restoring breathing using certain systems and connecting equipment to monitor the patient’s condition.
The sooner treatment begins - and, further, rehabilitation - the higher the patient’s chances!
The site Colady.ru warns: self-medication can harm your health! The diagnosis should only be made by a doctor after an examination. Therefore, if you notice any alarming symptoms, be sure to consult a specialist!
First emergency aid for stroke before doctors arrive at home
Regardless of whether the patient is conscious or not, it is important, first of all, to turn him on his side so that the person does not choke on vomit.
The head should be slightly raised (approx. - above the level of the bed or surface on which the person is lying!). What's next?
- We call an ambulance, REPORTING A STROKE! It is important that a neurological team arrive; a regular ambulance will not be of much use. Tell the dispatcher that you know for sure that the person is having a stroke, because... “the neighbor-doctor said,” “the pedestrian who turned out to be a doctor said,” and so on.
- We loosen the patient’s belt, collar and anything else that may impede breathing and prevent free access of oxygen.
- Open the windows (if the patient is indoors).
- We measure the pressure (if possible).
- For high blood pressure, we give the drug prescribed to the patient by the doctor.
- If there is no medicine, you can immerse the person’s feet in hot water.