Fasciculations are contractions of several or one motor muscle, which can be noticed due to active muscle movement; these movements occur due to damage to the area of the anterior roots or anterior horns of the spinal cord.
In a relaxed state, the muscle should not involuntarily contract. The clinical significance of fasciculations is small, since they do not cause any serious harm.
Every person has experienced something similar at least once in their life. For example, after severe stress, people experience an involuntary twitching of the eyelid, which is commonly called a nervous tic. Such muscle contractions disappear as imperceptibly as they appear. Concerns arise only in those cases in which the patient experiences changes in reflexes and muscular dystrophy.
Fasciculations should be distinguished from fibrillations. The term fibrillation is used to refer to the spontaneous, discrete contraction of a muscle fiber. Contraction of the entire muscle or group of muscles does not occur. Unlike fasciculation, fibrillation cannot be seen under the skin. In exceptional cases, it can be seen when individual muscle fibers of the tongue contract.
The appearance of fibrillation can be observed with injuries to the axon of a motor neuron or with serious damage to the body. In addition, it can occur with primary muscle disorders. Fasciculations are not observed in the same cases.
Fasciculations occur due to damage to the anterior horns of the spinal cord
What pathologies are characterized by fasciculations?
Rhythmic and non-rhythmic, long-term and short-term involuntary muscle contractions can occur due to many reasons and diseases, for example:
- Facial hemispasm . Determining the presence of the disease is quite simple: during an attack, the affected part of the face becomes asymmetrical - the eye closes, the corner of the mouth rises. This occurs as a result of compression of the facial nerve. Among the causes of the disease are hereditary predisposition, multiple sclerosis, circulatory disorders, and exposure to toxic substances.
- Neuromyotonia . It occurs in both adults and children. Characterized by increasing muscle stiffness. Neuromyotonia begins to manifest itself in the extremities, then gradually spreads. The body loses its natural plasticity.
- Motor neuron diseases . Despite the fact that fasciculations are typical for this type of disease, the disease can only be diagnosed if the patient exhibits denervation. Motor neuron diseases include: Machado-Joseph disease, ALS, tumors (benign and malignant) of the brain and spinal cord, late manifestations of polio, etc.
- Peripheral nerve damage , which in most cases leads to myokymia. These symptoms may occur after surgical treatment of compressive radiculopathy.
Benign crampy-fasciculation syndrome
Crampy fasciculations syndrome is manifested by prolonged muscle twitching. Most often, twitching occurs in the muscles of the thighs and lower legs.
More than 75% of the population experiences this syndrome.
The symptoms are:
- Itching and trembling in the muscles;
- Involuntary muscle contractions or spasms;
- Stiffness;
- Weakness;
- Muscle pain;
- Symptoms of anxiety and stress.
Benign crampy-fasciculation syndrome and amyotrophic lateral and amyotrophic syndrome (ALS) have similar symptoms, but they are completely different diseases.
The main symptom of ALS is muscle atrophy. As a result of the damage, the muscles atrophy and decrease in size. This condition is accompanied by significant weakness.
In both cases, muscle fasciculation is observed, which is more common in benign crampy-fasciculation syndrome. Twitching occurs during rest, but stops during muscle activity. In ALS, twitching may start in one place and spread to other muscles nearby.
What are the types of fascicular twitches?
There are several types of fascicular twitches:
- Ballism . Characterized by sweeping and wide movements. This form develops due to damage to the globus pallidus, striatum or subthalamic Lewis nucleus. Ballism may also be based on vascular disorders of the brain.
- Progressive hemiballismus . Appears when a volumetric intracranial formation occurs. In case of circulatory failure in the basilar artery system, transit episodes of hemiballismus are observed.
- Myorhythmias . This is the name given to the rhythmic twitching of individual muscle groups that have a permanent localization. Myorhythmias are observed in the facial area. They may indicate disinhibited or damaged reflex activity of central structures in the brain stem. An example of myorhythmias is nystagmus (tremor) of the soft palate, which occurs with multiple sclerosis or after abdominal surgery.
- Myoclonus . They are characterized by short-term, irregular twitching of individual muscles and occur suddenly. There are 3 types of myoclonus: generalized, multifocal and focal. Myoclonus can develop as a result of metabolic disorders in the body. Possible combination with epileptic seizures. Seizures are observed in degenerative, infectious and inflammatory diseases, and in postanoxic brain damage. If attacks of myoclonus are accompanied by increased sweating, we are talking about cholinergic hyperactivity. In addition, muscle contractions are observed during the transition from the waking state to the sleep state. These are so-called benign myoclonus, which should not be considered as pathology or evidence of the presence of any diseases.
- Multiple paramyoclonus . This term refers to irregular, spontaneously occurring twitching of the muscles of the shoulder girdle.
- Myokymia . May develop after treatment with certain drugs. These are contractions passing through individual muscle groups and individual muscle fibers.
- Infantile polymyoclonus . It got its name because it occurs in childhood. Infantile polymyoclonus in a child can be determined by “dancing” eye movements. Over time it tends to progress.
- Fibrillary chorea (otherwise known as multiple fibrillary myoclonus). The probable cause is exposure to mercury salts. Fibrillary chorea is characterized by chaotic and irregular contractions of individual muscle areas. It can be distinguished from other forms by the appearance of drowsiness, hallucinations and mental disorders in the patient.
- Iatrogenic fasciculations . Caused by the bites of some poisonous insects. They have been described with overdoses of anticholinergics and the use of Penicillin.
The already mentioned benign muscle fasciculations are classified as a separate group. They are characteristic of the orbicularis oculi muscle and the muscles of the leg. They can occur in a completely healthy person. Benign fasciculations can last from several minutes to several years.
In the latter case, involuntary contractions may appear at regular intervals, for example, three to four times a day. With benign fasciculations, the EMG (electromyogram) does not record excessive deviations, sensitivity is not impaired, there is no decrease in the speed of excitation along the nerve, and no changes in reflexes are observed.
Muscle fasciculation
Fasciculation - contraction of one or more motor units (a single motor neuron and the group of muscle fibers supplied by it) leads to a rapid, visually visible, contraction of muscle bundles (fascicular twitching or fasciculations). On EMG, fasciculations appear as broad biphasic or multiphasic action potentials. The simultaneous or sequential contraction of multiple motor units produces a wave-like muscle contraction known as myokymia.
Normally, a relaxed muscle is not accompanied by bioelectrical activity. If fasciculations are the only symptom, that is, they are not accompanied by muscle atrophy and changes in reflexes, their clinical significance is small. With more severe motor neuron dysfunction, all muscle fibers that receive innervation from it suffer, which leads to muscle atrophy (denervation atrophy), decreased reflexes and is accompanied by fibrillation potentials, positive waves, fasciculations and changes in motor unit potentials.
Diagnostic criteria
A neurologist treats fasciculations and accompanying pathologies. If a person constantly feels muscle spasms and twitching, he should consult a doctor to determine the cause of their occurrence.
The specialist will usually ask a series of questions that will help determine whether the patient is suffering from a serious medical condition or whether the muscle twitching is benign. First of all, the doctor must know how long ago the patient started having involuntary contractions, and how long the twitching usually lasts.
The patient must also tell the doctor exactly which muscles are contracting. The doctor should also know about the nature of these contractions: rhythmic, non-rhythmic, etc. You need to tell the specialist about the presence of other symptoms and diseases, if any. If a woman knows she is pregnant, she needs to notify her doctor.
Depending on the symptoms, the doctor may prescribe one or another type of examination. In most cases, the patient undergoes an electromyogram, a nerve conduction study, and a blood test.
Prevention and treatment
Fasciculations are not a cause, but a symptom of one or another neurological disorder. That is why it is necessary to first identify the disease that led to the occurrence of muscle contractions and begin treating this pathology. In some cases, the disease cannot be found, in which case it is likely that the cause of fasciculations is a lack of magnesium. On the advice of a doctor, the patient should review his diet and include more foods containing the necessary element.
Benign fascicular twitches usually do not require treatment. It is enough just to wait for them to completely disappear.
Since in healthy people the cause of involuntary muscle contractions is stress, as a preventative measure you can
recommend relaxation practices. Such methods allow you to completely get rid of the consequences of stressful situations. The most effective in protecting the nervous system from negative external influences are considered to be sports, walks, trips out of town, yoga, etc.
Another reason for the appearance of benign fasciculations is excessive physical activity, especially those associated with running or lifting weights. That is why, trying to cope with the twitching of one muscle group through sports, you can get involuntary contractions of another muscle group.
Fasciculations that occur after active physical activity are most susceptible to poorly trained people who lead a passive lifestyle. They may notice twitching after the first run. That is why it is best to start classes with light exercises.
To avoid benign muscle contractions, it is necessary to protect your body from hypothermia, which is also considered one of the possible causes of spasms. You can overcool your body not only in the cold season due to wearing clothes that are out of season.
In the summer months, swimming in ponds leads to involuntary contractions. To avoid unpleasant consequences, you must follow the rules of behavior on the water. One of the possible causes of fasciculations is uncontrolled consumption of alcoholic beverages.
What is a motor unit?
The anatomical and histological unit of striated skeletal muscle is a fiber, which under a microscope looks like a long cylindrical cell with numerous nuclei distributed along its entire length. Numerous parallel fibers are combined into a bundle visible to the naked eye.
The functional unit of skeletal muscle is the motor unit, which includes:
- an anterior horn cell, the body of which is located in the ventral part of the gray matter of the spinal cord;
- its axon, emerging from the spinal cord from the ventral side and being part of the peripheral nerve covered with a myelin sheath;
- several “target” muscle fibers making up one bundle.
Thus, the minimal natural manifestation of muscle activity is considered to be the functioning of one motor neuron, causing contraction of the corresponding muscle fibers.
What is the difference between fibrillation and muscle fasciculation?
Fibrillation is the spontaneous contraction of a single muscle fiber. Fibrillation does not cause muscle contraction and cannot be seen through the skin (rarely it can be seen in the muscles of the tongue). It is detected by electromyographic study as an irregular asynchronous short (1-5 ms) low-voltage (20-300 μV) discharge in the muscle (usually 1-30 discharges occur in 1 s). Fibrillation typically occurs with injury to the body or axon of a motor neuron, but can also occur with primary muscle disorders such as myopathy.
Muscle twitching (fasciculations)
Have you started to notice that your muscles are twitching on some limb or in different parts of the body? Yes, this is a very unpleasant symptom that often frightens a person. In an attempt to understand the reasons, people often drive themselves into a dead end. The search for information about symptoms and the disease that could cause them inevitably leads to a description of serious diseases of the central nervous system: ALS, multiple sclerosis, etc. This, in turn, further weakens the nervous system of suspicious people and only worsens the course of the disease (in most cases, the last word should be put in quotation marks).
Syndromes involving the extrapyramidal system
Peripheral paralysis.
Peripheral paralysis
caused by damage to the peripheral motor neuron at any level. Clinically, the following symptoms are detected in the paralyzed limbs (on the side of the lesion):
1. Absence or limitation of voluntary and involuntary movements (akinesis or hypokinesis).
2. Atony or hypotension - loss or decrease in muscle tone.
3. Areflexia or hyporeflexia – absence or decrease in muscle tone.
4. Atrophy or hypotrophy - a decrease in volume or thinning of muscles, loss of their normal elasticity.
5. Fibrillar twitching - contractions of individual muscle bundles.
6. Reaction of rebirth. Violation of the electrical excitability reaction of the muscle.
Degree of severity of decreased strength in the limbs (depth of paresis)
examined in the Barre test (upper and lower). The patient, lying on his back, is asked to hold his arms extended forward or his legs bent at the knee and hip joints with his eyes closed. The paralyzed limb cannot be supported and falls faster. The test results are assessed in points:
5 points – normal – active movements in full, muscle strength is not reduced;
4 points – (mild paresis) – there is no restriction on the range of active movements, the limb is held in the Barre position for several minutes, then begins to slowly lower;
3 points – (moderate paresis) – slight decrease in muscle strength, in the Barre position the limb rises, but is held for a very short time;
2 points – (severe paresis) – a pronounced decrease in muscle strength, the patient cannot lift an extended limb or move on the surface of the bed;
1 point – (deep paresis) – there is no movement of the limb, only a contraction of individual muscle groups or bundles is noted;
0 points – (paralysis, plegia) – limb movement and muscle contraction are not noticeable.
The extrapyramidal (extrapyramidal) system includes a number of formations of the subcortical region and the brain stem, forming the striopallidal system: the caudate nucleus (n. caudatus) and the lentil nucleus (n. lenticularis), consisting of the globus pallidus (globus pallidus) and the putamen (putamen), red nucleus (n. ruber), substantia nigra (substantia nigra), subthalamic nucleus of Lewis.
According to the morphological structure, onto- and phylogeny, and functional significance, two parts are distinguished - the new one (neostriatum),
which includes the caudate nucleus, putamen and subthalamic Lewis nucleus, and
the ancient (paleostriatum),
which includes the globus pallidus and substantia nigra. The neostriatum consists predominantly of small cells, while the paleostriatum consists of larger cells.
The function of the extrapyramidal system is expressed in maintaining normal muscle tone, regulating involuntary, automated movements, providing diffuse, complex automated movements such as swimming, climbing, throwing, etc. The extrapyramidal system determines the smoothness and rhythm of movement, takes part in ensuring emotional manifestations (facial expressions of emotions).
An important mediator of the functioning of the extrapyramidal system is dopamine, the synthesis of which occurs mainly in the bodies of neurons in the substantia nigra, from where along the axons of these neurons dopamine reaches the new striatum, in particular the caudate nucleus. The caudate nucleus also contains a significant amount of other mediators: acetylcholine and serotonin. Dopamine enhances the phasic component (fast movement), acetylcholine and serotonin - the tonic component (slow movements).
All impulses entering the striopallidal system reach the globus pallidus, the axons of which are directed to the red nucleus, reticular formation, and substantia nigra.
Descending efferent pathways are sent to the spinal cord along the reticulospinal (ends on the y-motoneurons of the anterior horn), rubro-spinal, tectospinal, olivo-spinal (ends on the a-small motor neurons of the anterior horn) tracts.
When studying the function of the extrapyramidal system, it is necessary to study the appearance and posture of the patient, his gait, muscle tone, tendon and postural reflexes, facial expressions, writing, and friendly movements.
The clinical picture of lesions of the extrapyramidal system depends on the localization of the pathological process. Damage to the pollidar region is manifested by the development of hypertensive-hypokinetic syndrome. When the striatal region is damaged, a hypotonic-hyperkinetic syndrome occurs.
3.2.1. Hypertensive - hypokinetic syndrome (akinetic-rigid syndrome, amyostatic, parkinsonism syndrome). The main symptoms of parkinsonism are:
1. Increased muscle tone of the plastic (extrapyramidal) type, which is characterized by:
1.1. A uniform, waxy increase in tone in all muscle groups of the limbs - flexors and extensors, felt throughout the entire period of muscle stretching (“viscous, sticky” tone).
1.2. Increase in tone as research progresses.
1.3. Against the background of uniformly difficult passive movement, intermittent delays are observed, as a result of which the limb moves jerkily - the “gear wheel” phenomenon.
2. Akinesia, hypokinesia – absence or decrease in motor activity without paresis and paralysis. Manifestations of akinesia include:
2.1. Oligokinesia – poverty and decreased range of motion.
2.2. Bradykinesia is a slowdown in the pace of active movements due to high plastic tone.
2.3. Amimia – mask-like face, poor facial expressions.
2.4. “Flexor posture” - the neck, torso and limbs at the joints are slightly bent, pressed against the body.
2.5. Propulsion, retropulsion, lateropulsion - irresistible acceleration of the patient's movement forward, backward, to the side when walking or after a slight push, the inability to stop the movement started or change direction.
2.6. Gait with small, shuffling steps (senile, “doll-like”).
2.7. Acheirokinesis is the absence of friendly arm movements when walking.
2.8. Reduced modulation and emotional coloring of the voice, which becomes inexpressive, monotonous, and fading.
2.9. Micrography is a change in handwriting that becomes small, the letters are connected, and their size decreases towards the end of the sentence.
2.10. Paradoxical kinesia in patients who can barely move with assistance and are bedridden - the possibility of rapid movements (running, jumping, waltzing, etc.) under the influence of emotional factors.
3. Static tremor (rest tremor) - a symptom of “counting coins”, “rolling pills” - rhythmic trembling of the distal parts of the hands, especially fingers, of low amplitude and frequency, stopping during purposeful movements.
4. Facial skin greasiness, hypersalivation, hyperhidrosis.
5. Changes in character: importunity, tendency to repeat, slowed down thinking, viscosity.
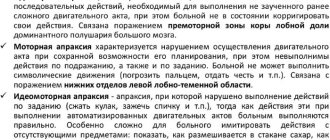
3.2.2. Hypotonic-hyperkinetic syndrome is characterized by the development of muscle hypotonia and involuntary movements (hyperkinesis). The most typical of them are:
1. Chorea – non-stereotypical, rapid, excessive movements in the limbs and face.
2. Athetosis – slow, worm-like, fanciful movements in the fingers and distal parts of the limbs.
3. Torsion spasm - slow corkscrew-like movements of the body.
4. Hemiballismus – sweeping throwing and irregular rotational movements in half the body.
5. Myoclonus - irregular, rapid twitching of individual muscle groups.
6. Facial paraspasm – tonic-clonic symmetrical spasms of the facial muscles.
7. Facial hemispasm is a convulsive contraction of the muscles of one half of the face, in which the corner of the mouth and eyebrow rise, and the palpebral fissure narrows.
8. Tics are short-term, stereotypical, monotonous, small twitches of individual muscles. They most often occur on the face and, mainly, with functional diseases of the nervous system.
9. Blepharospasm – tonic-clonic symmetrical spasms of the circular muscles of the eye.
When determining hyperkinesis, attention is paid to the state of muscle tone, rhythm, stereotypy, and range of movements.
Didn't find what you were looking for? Use the search:
Source: //studopedia.ru/2_74813_sindromi-porazheniya-ekstrapiramidnoy-sistemi.html