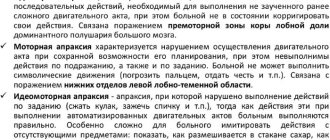
Paresis is a decrease in tone and strength in a muscle group. Paresis is incomplete paralysis. Typically, paresis occurs secondary to an illness accompanied by circulatory disorders - stroke, brain tumors, birth trauma. Paresis is not selective in terms of gender and age. They occur in both children and adults.
Paresis can be either left-sided or right-sided. Depending on the location of the lesion in the brain - the right or left hemisphere - cross-response paresis occurs. The right hemisphere is responsible for the occurrence of left-sided paresis, and the left hemisphere is responsible for the occurrence of right-sided paresis. According to statistics, left-hemisphere lesions are more common than right-hemisphere lesions - about 60% of cases.
Classification
Paresis based on damage to the nervous system is divided into:
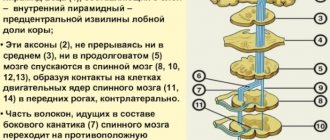
- Central paresis (spastic) – damage to the central nervous system (brain and spinal cord);
- Peripheral (flaccid) paresis – damage to the peripheral nervous system;
- Mixed paresis is a combination of damage to the central and peripheral nervous systems;
- Psychogenic (psychosomatic) paresis is the presence of a symptom of decreased muscle strength without organic damage to the nervous system.
Paresis by number of affected limbs (by prevalence):
- Monoparesis – involvement of one of the limbs (one arm or one leg);
- Hemiparesis – involvement of the arm and leg on one side;
- Paraparesis – involvement of two arms or two legs;
- Tetraparesis - involvement of all four limbs (arms and legs), less often - three limbs (two arms and a leg or two legs and an arm - you can come across the concept of triparesis).
Paresis according to severity:
- Mild paresis;
- Moderate paresis;
- Deep paresis.
Assessment of muscle strength in paresis:
- 5 points – full range of motion in the arms and legs, sufficient muscle strength;
- 4 points – full range of motion, muscle strength slightly reduced;
- 3 points – range of movements is reduced, limbs are able to overcome gravity with the possibility of lifting off the surface;
- 2 points – the range of movements is extremely reduced, the limb does not overcome gravity and moves along a plane;
- 1 point – there is no movement in the joints, but some muscle contractions are still noticeable;
- 0 points – no voluntary movements, paralysis.
Causes
Paresis is not an independent disease; it is one of the symptoms of damage to the nervous system. Occurs when one of the sections of motor fibers is damaged. This reduces the ability of nerve impulses to travel from the brain to the organs and limbs, reducing the ability to move.
Central paralysis in diseases of the spine is associated with the involvement in the process of both the spinal cord itself and the nerve nodes and endings extending from it. These can be spinal injuries, tumor formations, inflammatory and purulent processes, foreign bodies, etc.
Also often, paresis has a combination of its two types - central spinal and psychosomatic. As a rule, organic damage to the spine is accompanied by the patient’s family difficulties, and such a disease is more difficult to treat and requires longer time and effort.
Left-sided and right-sided hemiparesis
Neurologists were able to establish a certain relationship between symptoms in a certain part of the body and the brain hemisphere in which the abnormal focus is present. This connection is inverse.
If a feeling of weakness is present in the right limbs, right-sided hemiparesis is diagnosed, but if the symptoms are localized on the left, left-sided hemiparesis is diagnosed.
Moreover, each hemisphere of the brain is responsible for performing certain functions of the body. So, if left-sided hemiparesis develops as a result of a traumatic injury or stroke, the person often experiences serious speech impairments.
It is the right-sided hemiparesis that is one of the most common complications of stroke, since circulatory disorders often occur in the left artery of the brain. These processes provoke loss of sensitivity and motor activity.
If a person has a left-sided form of the disorder, then the patient may experience mental disorders. This is due to the fact that in the right hemisphere of the brain there is a maximum number of nerve centers that are responsible for mental functions. It is important to note that the left-sided form of the disease is much less common.
Symptoms of paresis
The signs and symptoms of paresis of different origins do not differ from each other (it is possible to determine the type only by special diagnostic measures).
- Hanging of the head, often forward, inability to keep the head straight;
- Weakness in the arms, up to their free hanging: difficulties in holding objects, in raising the arms, in keeping them suspended;
- Change in gait - waddling from one leg to another, lameness;
- Weakness of the legs, up to the inability to move independently;
- Difficulty when trying to stand up on your own;
- Weakness of the feet: “cock” or “chasing” gait – high raising of the foot with simultaneous sagging;
- Strengthening or, less frequently, weakening of reflexes from the limbs (depending on the location of the lesion).
Rehabilitation period
Of great importance in the treatment of spastic tetraparesis, in particular with cerebral palsy, are rehabilitation measures, the task of which is to improve the physical condition of the child and adapt him to living conditions as much as possible. Rehabilitation includes the following methods:
- Occupational therapy – develops motor skills and sense of touch, regulates movement and orientation. Fine motor skills also develop separately. In occupational therapy, play methods, techniques of physical contact, holding, and copying are used.
- Speech therapy exercises . The purpose of the classes is to develop correct pronunciation. Special methods can eliminate the problem of non-verbal communication and swallowing reflex disorders. Also, thanks to these programs, coordination and hearing are improved, and previously formed speech disorders are eliminated.
- Aquatherapy . Helps relieve pain symptoms by relaxing spastic areas, as well as strengthen muscles. This treatment has a beneficial effect on the emotional state of the child. The procedure is carried out by lowering the child into the water using special chairs. The water temperature should be approximately 35 degrees.
- Hippotherapy . A very effective method in which the horse serves as the therapeutic agent. This procedure stimulates motor reflexes and increases activity. Sometimes therapy gives very good results when the child gradually learns to sit in the saddle and control a horse independently.
Diagnostics
Diagnosis of paresis includes a set of measures:
- Interview in the office of a neurologist, vertebrologist, neurosurgeon - complaints are collected at the time of treatment and at the onset of the disease, the visible causes that led to paresis are determined;
- Examination of the patient - determination of visible changes in gait and other movements in the joints;
- Neurological examination - determination of reflexes, assessment of muscle strength;
- Complete blood count - detection of inflammatory processes (increased ESR, leukocytosis);
- Biochemical blood test - increased creatine kinase (a metabolic product of muscle tissue);
- Test with Prozerin - the administration of this drug allows you to determine or exclude myasthenia gravis;
- Blood test for toxicology - identification of toxic substances in the blood;
- X-ray of the spine - examination of the spinal column for its integrity and location of bone structures;
- CT (computed tomography) of the spinal cord or other damaged structures - layer-by-layer examination of the structure of the spine, spinal cord and adjacent organs and structures to identify tumors, fractures, displacements, etc.;
- MRI (magnetic resonance imaging) of the spinal cord and other damaged structures is a more accurate research method, including, in addition to bone and muscle tissue, also nervous tissue (determines the integrity of the spinal cord, nerve endings, etc.);
- Electroneuromyography (ENMG) - determination of the activity of muscle tissue, the conduction of nerve impulses along the fibers and the places through which these impulses are not transmitted.
Complex of therapeutic measures
Treatment of tetraparesis should be comprehensive and carried out in a hospital setting. Conservative, neurosurgical, orthopedic methods and rehabilitation are used.
Therapy is carried out to achieve the following goals:
- reduction of spasticity;
- prevention of dysfunction of the musculoskeletal system;
- formation of the correct motor stereotype.
Conservative treatment primarily includes two main aspects:
- Drug therapy - prescribed drugs, for example, Baclofen and Botulinum toxin, help reduce the spastic effect, resulting in increased impulse conduction and improved metabolic processes in the brain, while increasing the number of passive movements of the limbs.
- Physical therapy – focuses on movements, exercises and poses that strengthen muscles.
The treatment package also includes:
- reflexology;
- hirudotherapy;
- acupuncture;
- exercise therapy;
- massage;
- gymnastics on special simulators;
- kinesitherapy.
Surgery
For more effective correction of spastic tetraparesis, surgical treatment is required. The operation is performed to restore the functions of a specific damaged area.
An orthopedic procedure corrects contractures and stretches muscles. Plastic surgery of muscles and tendons is also performed. This correction method brings very good results.
Diseases in which paresis occurs
Diseases of the spinal column and spinal cord, which may be accompanied by paresis:
- Spinal stroke;
- Spinal stenosis;
- Tumors (both malignant and benign) of the spine and spinal cord;
- Spondylitis;
- Injuries to the spinal cord and spine: fracture, bruise, dislocation, etc.
- Severe radiculitis;
- Severe kyphosis;
- Abscess (abscess) in the spinal cord;
- Spondylosis;
- Myelitis (inflammation of the spinal cord);
- Vertebral instability;
- Spinal tuberculosis;
- Brown-Séquard syndrome;
- Retrolisthesis (as its complication);
- Spondyloarthrosis;
- Osteoporosis.
Diseases of other organs and systems, the symptom of which is paresis:
- Brain stroke;
- Brain tumors;
- Head and brain injuries;
- Abscess (abscess) of the brain;
- Encephalitis (inflammation of the brain);
- Multiple sclerosis;
- Poisoning with poisons, salts of heavy metals;
- Guillain-Barre syndrome;
- Myasthenia;
- Epilepsy;
- Botulism;
- Amyotrophic lateral sclerosis (ALS);
- Myopathy;
- Mild cerebral palsy (cerebral palsy) and other congenital pathologies;
Treatment of paresis
Treatment of paresis in diseases of the spine and spinal cord must be comprehensive, individual and aimed at eliminating the underlying disease that caused this paresis.
Drug treatments
- The use of broad-spectrum antibiotics to fight infection, especially purulent ones. Ceftriaxone is most often prescribed (dosage depends on the pathological condition);
- B vitamins to normalize nerve conduction;
- Prozerin is a drug that restores nerve patency.
Physiotherapeutic treatments
- Massage. Normalizes blood flow, nerve transmission, relieves increased muscle tone and stabilizes the spine;
- Electrical stimulation. Restores broken nerve connections, improves nerve conduction in sensory and motor branches of nerve endings;
- Gymnastics and exercise therapy. Restores movement in the limbs, strengthens and stabilizes the spine and muscular frame of the back. All exercises are selected and developed by the doctor individually and adjusted in the process of changes;
- Swimming. Being in the water and performing special exercises, and, if possible, swimming with the use of auxiliary objects, quickly relieves the vertebrae from the load, aligns and stabilizes the spinal column, strengthens the muscular frame of the back, improves blood flow and nerve conduction;
- Consultations with a psychotherapist and psychologist. They help find and solve psychosomatic problems, increase self-confidence, adapt to temporary or permanent movement disorders, and much more. This long-term work is quite effective if the patient takes an active part in it, and is not just a listener to the specialist’s stories.
Surgery
It is used quite often in cases of paresis and spinal pathology to eliminate the main cause of this symptom:
- Removal of the tumor;
- Removal of a foreign body (bone fragments, bullets, glass, etc.);
- Vascular operations (removal of a blood clot, suturing of a vessel, etc.);
- Removal of purulent foci, their sanitation and tissue cleansing;
- Installation of vertebral implants.
Traditional methods of treating paresis
Traditional medicine is a fairly good and effective aid to the main treatment, traditional. It strengthens the body, accelerates the effects of medications, improves the processes of restoration of nervous tissue, normalizes blood flow and has many other effects. However, its use as monotherapy is not advisable and threatens to worsen symptoms.
Tea from a collection of herbs. Mix 2 tablespoons of chamomile flowers, garden marjoram, rose hips and roots, thyme, medicinal veronica, laurel leaves and tannic sumac. Brew like regular tea. Drink 3-4 times a day, with the addition of honey to taste. The duration of treatment is at least 2 months.
Pine baths. You should take 1.5-2 kg of spruce, pine or other coniferous tree needles, fill them with 5 liters of water and boil for 30 minutes. Then leave for about 10-12 hours, filter and store in the refrigerator. Add 1.5-2 liters of this decoction to a warm bath (with a comfortable water temperature) and take a bath for 20 minutes daily. The course of treatment is 20-30 days.
Stroke, right side, consequences, how long they live after a lesion, how they are treated
A stroke is a lesion that occurs due to circulatory problems in the brain. Regardless of which side is affected, it is equally dangerous, since cell death occurs in the brain.
What is a right-sided stroke?
There are 3 types of brain damage. A right side stroke may be:
- ischemic;
- hemorrhagic;
- mixed.
The ischemic type is characterized by blockage of a blood vessel or a number of vessels in the brain, which leads to oxygen starvation and the process of neuronal death. The hemorrhagic type is more dangerous, as hemorrhage occurs in the brain tissue due to a ruptured vessel. The mixed type manifests itself through signs of ischemic and hemorrhagic stroke.
Depending on what caused the syndrome, atherothrombotic, cardioembolic, hemodynamic and lacunar subtypes of ischemic stroke are distinguished.
The root cause of the first subtype is atherosclerosis, the second subtype manifests itself due to blockage of blood vessels in the head. Hemodynamic occurs in the presence of heart disease.
And lacunar is characterized by the presence of voids or lacunae, which after some time are filled with liquid, and due to their size, squeezing the vessels, disrupting blood circulation.
The hemorrhagic type is divided into epidural, subdural, parenchymal, subarachnoid and intraventricular. The first subtype is characterized by the outpouring of blood from the vessels into the brain, which are located above its hard shell.
The second is a consequence of hemorrhage in the tissue under the dura. Parenchymal is diagnosed due to bleeding into the soft tissue of the brain. The next subspecies is characterized by outpouring into the subaranoid space.
The intraventricular type speaks for itself, as it is caused by effusion into the ventricles of the brain.
Causes
The etiology of a stroke on the right side of the brain can have many causes. More often it is influenced by a group of symptoms. The main influencing factors are:
- tumors or other neoplasms in the brain - an increase in their size leads to pressure on blood vessels, causing blood to stop circulating normally;
- obesity – excess weight puts additional stress on the heart;
- atherosclerosis of blood vessels - poor nutrition leads to the formation of plaques, which, accumulating in the vessels, lead to poor circulation;
- thrombositosis - pathological thickening of the blood leads to the development of blood clots in the form of blood clots that close the lumen of the blood vessel;
- arterial hypertension - this disease leads to constant expansion of veins and capillaries, which makes them less dense and elastic, which can lead to their rupture;
- exhaustion of the body due to lack of adequate sleep, frequent stress;
- unbalanced diet - frequent consumption of fast food, carbonated drinks, fatty foods;
- the presence of an autoimmune disease such as diabetes mellitus and others;
- long-term use of medications that lead to blood thickening;
- alcohol abuse.
Symptoms of a stroke in the right hemisphere
Harbingers and immediate signs of a stroke on the right side of the brain can be:
- sharp, intense pain in the head;
- blurred vision, mainly in the left eye;
- hearing, smell and touch are dulled;
- nausea with vomiting;
- dizziness;
- loss of balance;
- increased heart rate;
- manifestation of numbness and tingling in the left side of the body;
- excess of normal blood pressure levels.
In addition, the following signs will help you understand that a person is having a stroke on the right side:
- curved lip line when trying to smile, the left side does not move;
- confused consciousness, inability to navigate in space;
- the victim cannot raise both arms at the same time;
- speech is slurred, incoherent, the patient cannot clearly answer questions and formulate sentences.
How to recognize a right-sided stroke?
It is difficult to recognize a right-sided stroke at the stage of the first signs if a person is not a specialist. It is easier to do this when the symptoms have subsided and the patient is in a post-stroke state. Damage to the right side is characterized by:
- decreased sensitivity and coldness in the upper and lower extremities;
- stiffness in the left side of the body;
- impaired facial expression due to damage to the facial nerve;
- dryness of mucous membranes;
- numbness of the tongue.
Useful information: During damage to the right side of the brain, which is responsible for the left side of the body, disturbances are observed on the left side of the body. If we are talking about a left-sided stroke, the right side is affected.
Damage to the right hemisphere of the brain also causes:
- paralysis of the left side of the body;
- the ability to speak normally remains;
- disorientation;
- memory lapses regarding doing ordinary things (inability to dress or put on shoes independently).
Why is it dangerous?
Regardless of whether we are talking about a right-sided stroke or a left-sided one, the same lesion is dangerous for health and can be fatal. Even if your physical health is no longer in danger, your mental health suffers. A stroke does not go away without consequences.
After the negative symptoms have passed, the recovery period begins. People have to relearn how to walk, move, dress, hold a spoon, a pen. Often the patient becomes apathetic and withdraws into himself, which leads to the activation of various types of mental disorders.
Consequences of a right-sided stroke
A right hemisphere stroke can be either ischemic or hemorrhagic. Depending on which one occurred, the consequences after it may be different. The intensity of the consequences depends on the age of the patient, the type of injury, and the speed of first aid provided.
Ischemic stroke
The main side effects of a right-sided ischemic attack include:
- motor dysfunction;
- disturbance of touch;
- deterioration of vision if the occipital part was affected during a stroke on the right side;
- possible loss of ability to swallow;
- lack of movement control;
- inability to control urination;
- frequent nausea, vomiting;
- disruption of the functionality of internal organs and systems due to intense brain damage.
The presented consequences may manifest themselves partially or fully. This list may be supplemented by other possible consequences, such as the occurrence of epileptic seizures.
Hemorrhagic stroke
A hemorrhagic stroke on the right side can be fatal. It is difficult even for specialists to predict what will happen to the patient some time after. The fact is that this type of lesion is dangerous in any part of the brain and at any age.
Blood circulation in the brain when a vessel ruptures is difficult to eliminate with medication. Often, during a hemorrhagic attack, the problem is solved surgically. But if the operation was not performed promptly, there is a risk of death.
If the consequences of this type have been eliminated, a right-sided stroke can manifest itself through convulsions, severe pain in the head, frequent attacks of nausea and vomiting, and fainting. In this case, shortness of breath is observed.
Treatment
Treatment of stroke depends on the type being diagnosed and the severity of the patient’s condition. Hemorrhagic right-sided stroke and its therapy are strikingly different from that which occurs after an ischemic attack. For such damage, the following groups of drugs are used:
- anticonvulsants;
- hypotension;
- antibiotics;
- neuroprotectors with nootropics.
The first lead to the relief of convulsive attacks and relax the muscles. Hypotonics help reduce pressure to reduce the size of hematomas in the brain.
Antibacterial agents are aimed at eliminating inflammation, which could be caused by the presence of blood in the brain tissue.
Neuroprotectors and nootropics are aimed at restoring the conduction of impulses and the flow of oxygen into cells.
Ischemic right-sided stroke is treated using the following means:
- thrombolytics;
- anticoagulants;
- nootropics.
Thrombolytics are aimed at eliminating blood clots in the blood vessels of the head, thinning the blood. The second drug prevents unnatural thickening of the blood and improves its circulation. Nootropic drugs are aimed at restoring neural connections and improving impulse conduction.
Rehabilitation
After the right-sided stroke and its consequences have been eliminated, and there is no threat of a second attack, a series of rehabilitation periods begins. Rehabilitation is aimed at restoring the patient’s normal functioning through training in lost skills, physiotherapeutic procedures, and diet.
In addition, the patient needs to do daily therapeutic exercises and massage. If the cause of the attack is known, it must be eliminated. To restore activity, they use not only physical therapy, but also visit the pool, practice acupuncture, magnetic therapy, and electrophoresis.
In addition, you need to give up bad habits, cure chronic diseases, and adjust your diet. To avoid a recurrent attack, which can be fatal, it is worth eliminating foods high in cholesterol, reducing the consumption of salt, fatty, and fried foods.
Important information Also during the recovery period after a right-sided stroke, it is important to consult not only a neurologist, but also a psychologist or psychotherapist, in order to avoid depression, which will only worsen the situation. The rehabilitation process can take from several months to several years.
Prognosis, and how long do they live after a right-sided stroke?
The prognosis after a right-sided stroke is not entirely favorable. But to a greater extent it depends on the extent of damage to brain tissue. Also, the duration of life after a lesion is influenced by the root cause, the presence of concomitant diseases, the level of the body’s resistance, and the fight against the disease.
A major stroke in a quarter of cases leads to the death of a person, either immediately after the attack, or in the next two weeks. Due to the fact that during an ischemic or hemorrhagic stroke the central nervous system is destroyed, most people subsequently become incapacitated.
How long the patient will live after the injury depends on how quickly and effectively the medical care was provided. Statistics say that only 30% return to normal life. The rest remain disabled. Death overtakes a person within a year.
A right-sided lesion brings a lot of troubles and difficulties, but if you provide qualified assistance in the first hours of the lesion, the life expectancy and general condition of the patient improves significantly.
: How to restore movement after a stroke
Source: https://nervy-expert.ru/insult/vidy-insulta/insult-pravaya-storona/