Causes and symptoms
Why does the abducens nerve become damaged?
What diseases can become provocateurs? Some types of infections and intoxications have a very negative effect on the central system. As a result, the abducens optic nerve also suffers.
What infections pose a huge danger? These are diphtheria, encephalitis, neurosyphilis, influenza and others.
Paresis is divided into two types: organic and functional. The second group usually causes difficulties in determining the cause of the disease.
Paresis of the abducens ophthalmic nerve associated with ischemic damage to small vessels is more common in adults. Diseases such as hypertension and diabetes have an impact here. The disease disappears on its own after three months.
Abducens nerve palsy manifests itself as isolated paralysis. In this case, a person cannot fully avert his eyes and a double image of one object appears (diplopia). This phenomenon occurs due to a violation of the innervation of the lateral muscle, for which the abducens nerve is responsible. Similar symptoms are characteristic of diseases of the orbit, so you should undergo detailed diagnostics to make a diagnosis.
The abducens nerve is damaged due to the following factors:
- Aneurysm;
- Damage to the carotid artery;
- Traumatic brain injuries;
- Infectious diseases;
- Oncological diseases;
- Microinfarctions and strokes;
- Pathologies of the nervous system;
- Multiple sclerosis.
The abducens nerve in children is also injured due to the above factors. However, other reasons are also common for children:
- Gradenigo syndrome;
- Mobius syndrome;
- Duane's syndrome.
Damage to the trochlear nerve causes partial paralysis of the eye and the person has a double image in an oblique or vertical plane. This symptom intensifies when the eye is lowered down, so people suffering from this pathology often walk with their heads tilted to the healthy side to reduce the manifestation of diplopia. During diagnosis, myasthenia gravis (autoimmune pathology of nerve and muscle tissue) and diseases of the orbit should be excluded.
Oculomotor nerve palsy usually occurs in conjunction with disruptions of the facial, abducens, and trochlear nerve pathways. A separate form of pathology appears extremely rarely. This nerve is damaged primarily due to an aneurysm. It arises on the posterior communicating artery and gradually compresses the nervous tissue.
The nerve can be damaged by a growing tumor, as well as manifestations of stroke and multiple sclerosis. In most cases, such factors affect the nucleus of the nerve tract and the posterior longitudinal fasciculus. Sometimes neuropathy of the oculomotor nerve, caused by the above reasons, manifests itself in the form of bilateral drooping eyelids (ptosis). In more rare cases, paresis of the superior rectus muscle of the eye is observed. It is localized on the reverse side of the main site of damage.
According to statistics, the oculomotor nerve is often damaged due to a microinfarction. It can occur due to vascular pathologies, such as diabetes and hypertension. Such diseases usually do not immediately lead to disruptions in cerebral circulation and they should be predominantly in an advanced state. Neuritis of this nerve does not affect the reaction of the pupil to light, but in rare cases it is slightly weakened.
You should consult a doctor if you notice several symptoms characteristic of paresis of the eye muscles, especially when it comes to children. Among the common manifestations of optic neuropathy, the most basic can be identified:
- Diplopia;
- drooping eyelid;
- Strabismus;
- Decreased pupil reaction to light;
- Inability to turn the eyeball inward;
- Loss of the ability to quickly look at objects located at different distances from each other;
- Protrusion of the eye.
Oculomotor nerve palsy: causes, symptoms, diagnosis, treatment – Case history
The combination of neurological pathologies of the visual apparatus poses a great danger to humans, so it is important to monitor not only the state of vision, but also the health of the eye itself.
One of the most serious diseases in this regard is paresis of the oculomotor nerve, which causes paralysis of the eyeball and other complications. In turn, the problem can only be a symptom of other diseases.
It is difficult to treat and stop, so when you detect the first signs of a disorder, it is important to consult a doctor as soon as possible.
Abducens nerve function
The nerve originates in the nucleus, located in the middle part of the medulla. Its fibrous structure crosses the pons and the brain center, passing its surface, called the basal. Then the path of the fibers flows along a groove located in the medulla oblongata.
Next, the fibrous threads of the nerve cross the membrane of the brain region, pass close to the carotid artery, move to the upper part of the orbital fissure and end their path in the orbit, firmly attached to the eye.
Nerve fibers control the rectus externus (lateral) muscle, which moves the eye outward and makes it possible to move the eyes to the sides without turning the head. The muscle is the opposite of the internal muscle tissue that pulls the eye toward the center. They balance each other out.
If one of the two muscles is affected, strabismus develops, since the other muscle pulls the eye organ towards itself, and the affected one cannot maintain balance. It is impossible to check the abducens nerve in isolation; it is examined together with the other two nerves.
Causes and symptoms
Symptoms of neuropathies are very varied and depend on which nerve is affected. It is customary to distinguish between cranial and peripheral neuropathy. With cranial nerves, any of 12 pairs are affected. Here we distinguish optic neuropathy (
with damage to the optic nerves
In peripheral neuropathy, the nerve endings and plexuses of the limbs are affected. This type of neuropathy is characteristic of alcoholic, diabetic, and traumatic neuropathy.
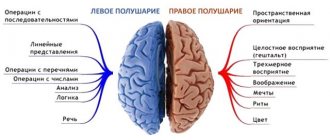
Also, the symptoms of neuropathy depend on the type of fibers that make up the nerve. If motor fibers are affected, movement disorders develop in the form of muscle weakness and gait disturbance.
In mild and moderate forms of neuropathies, paresis is observed, in severe forms - paralysis, which is characterized by a complete loss of motor activity. Moreover, after a certain time, atrophy of the corresponding muscles almost always develops.
So, if the nerves of the lower leg are affected, atrophy of the lower leg muscles develops; if the nerves of the face, then the facial and chewing muscles atrophy.
sensation of cold, warmth, goosebumps
Disruption of the exocrine glands (
for example, salivary
) is caused by damage to autonomic fibers, which also form part of various nerves or are represented by independent nerves.
Nerve pathology
Pathology of the abducens nerve
The fibers of the abducens nerve are located superficially, so during injuries they can easily be pressed to the base of the skull. Damage to the nerve is expressed in paresis - limited outward movement of the eye organ or complete paralysis.
https://www.youtube.com/watch?v=N9PkMdnhavE
With normal functionality of the abducens nerve, the edge of the cornea should touch the outer edge, the junction of the eyelids. If this is not observed, then there is nerve pathology. It has the following signs:
- movement of the eye organ is limited;
- objects inspected are split into two;
- repeated deviation of the eye;
- forced position of the head, which can be involuntary;
- dizziness, disorientation in space, staggering gait.
Nerve damage can be caused by infections:
- disease with encephalitis;
- previous syphilis;
- diphtheria disease;
- influenza and its complications.
As a result of intoxication:
- ethyl alcohol;
- toxic metals;
- combustion products;
- a consequence of botulism.
Paralysis of the abducens nerve occurs for the following reasons:
- previous meningitis;
- presence of tumor inclusions;
- the presence of hemorrhage, with pressure surges;
- thrombosis;
- purulent diseases of the nasal passages;
- eye socket injuries;
- temple bruises;
- metabolic disease;
- multiple sclerosis;
- stroke.
Nerve damage is distinguished by location:
- Cortical and conductive – diseases are localized in the medulla and brainstem.
- Nuclear defeat.
- Radicular lesions are observed within the medulla. This lesion is called Fauville's palsy, when, on the one hand, there is damage to the abducens and facial nerves, and on the other hand, there is damage to the limbs.
Peripheral paralysis is divided into:
- intradural is located inside the dura mater;
- intracranial is localized in the cranial cavity;
- orbital is located in a circle.
The oculomotor nerve is part of the third pair of cranial nerves and consists of viscemotor and somatomotor (motor) fibers. Its main function is to provide motor ability to the eyeball. The nerve controls the following systems:
- Ciliary muscles;
- Sphincter of the pupil (provides its ability to expand and contract depending on the lighting);
- Optical-kinetic nystagmus (the ability to follow moving objects);
- Muscles to regulate the movement of the upper eyelids;
- Vestibulospectral reflex (the ability of the pupil to move when the head turns);
- Accommodation (change in the curvature of the eye lens depending on surrounding objects and phenomena).
Thus, damage to the optic nerve always entails a limitation in the functionality of the visual apparatus. The movement of the eye and pupil is limited or lost.
In turn, the lesion has its own reasons for occurrence or acts as a sign of another disease.
Men and women of all ages are at risk, but statistics show that children are more likely to suffer from oculomotor nerve palsy.
In the early stages of oculomotor nerve paresis, there are practically no symptoms, which complicates its diagnosis and further treatment. With a longer course of the disease, the following symptoms gradually begin to appear:
- Drooping of the upper eyelid (partial or complete);
- Lack of reaction (constriction/dilation) of the pupil;
- Diplopia (double vision due to loss of motor ability of the eye);
- Divergent strabismus (occurs due to lack of resistance of the upper and lower muscles of the eyeball);
- Loss of focusing and adaptation to changes in the distance between the eye and the object;
- Loss of motor ability;
- Protrusion of the eye.
With extensive damage, immobility can become only part of the entire symptomatology of the disease if other cranial nerves are also damaged. In addition, oculomotor nerve palsy itself may be a symptom of a more serious systemic disease. Most often, the lesion affects only one eye.
In medical practice, there are two main forms of the disease:
- Congenital. Occurs as a result of intrauterine disorders of the development of muscles and nerves, as well as damage or damage to the facial and oculomotor nerves during development;
- Acquired. May have neurological, mechanical (traumatic injuries, consequences of surgical operations), aponeurotic prerequisites.
Paresis also occurs as a result of the progression of systemic diseases. In such cases, therapy should be aimed not only at eliminating paralysis, but also at relieving its causes.
Systemic pathologies that can cause paresis and paralysis:
- Diabetes;
- Arterial hypertension, instability of blood pressure;
- Benign tumors and oncology;
- Cervical osteochondrosis and other diseases of the spine;
- Aneurysm;
- Long-term use of Amiodarone, anticancer drugs and medications for the treatment of cardiovascular diseases;
- Hematomas;
- Traumatic eye injuries, foreign body entry;
- Inflammatory diseases of the brain (encephalitis, meningitis);
- Ophthalmoplegic migraine;
- Flu;
- Diphtheria;
- Syphilis;
- Brain hemorrhage, stroke;
- Vasculitis;
- Myocardial infarction.
The presence of at least one of the listed diseases is a reason for a systematic medical examination with a mandatory examination by a neurologist and ophthalmologist.
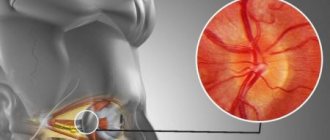
First of all, the examination should be performed by an ophthalmologist. During the diagnostic process, he must check:
- The presence or absence of deviation in the position of the eyeball;
- Absence or presence, strength of the pupil’s reaction to light exposure;
- The presence or absence of ptosis (paralysis of the upper eyelid);
- Eye focusing quality;
- The reaction of the pupil and eyeball to the movement of an object in space.
Thus, the doctor determines the probable site of the lesion, which further magnetic resonance imaging, superposition electromagnetic scanning, and X-ray examination will help to accurately determine. It is also necessary to collect anamnesis and information from the medical history. Additional research:
- Visometry;
- Ophthalmoscopy;
- Measuring intraocular pressure;
- Examination of the condition of the fundus.
Often, additional consultations with specialists in other areas are required: endocrinologist, neurologist, surgeon, infectious disease specialist, etc. In turn, they can prescribe additional hardware and laboratory tests.
One of the most important measures in the treatment of oculomotor nerve palsy is constant monitoring of the patient. In this case, a therapeutic effect on the root cause of paralysis is mandatory. If intervention is unavoidable, the doctor selects one of the more radical methods.
The main task of the computer program is to strengthen the muscles of the eyeball during the broadcast of special pictures. When viewing, patients experience increased nerve tension, due to which the body’s resources are mobilized and directed to improve their functioning. With systematic sessions, positive dynamics of treatment are observed.
Electrophoresis
Electrophoresis also gives good results of therapy. Before the session, electrodes are applied to the patient's closed eyes around the perimeter, as well as to the back of the head. The course of treatment consists of 15-20 sessions, the duration of which is no more than 20 minutes.
Surgery as a therapeutic method in the treatment of oculomotor nerve palsy is not always used. Typically, such a measure is required in two cases:
- If conservative therapeutic measures are insufficiently effective;
- With the progression of deterioration in the quality of vision, a decrease in acuity.
The operation is usually performed under local or general anesthesia (depending on the situation). After this, the patient must undergo a recovery period with a decrease in the load on the visual apparatus, as well as the introduction of a special regime of rest, sleep and physical activity. Additionally, the use of exercises and preventive medications is required.
Drug treatment in relieving paresis is ineffective. At the same time, to improve the patient’s condition, special eye drops that improve blood supply and tissue nutrition, physical therapy, and vitamin complexes can be used. Patients are also prescribed wearing bandages, sessions of viewing stereo images, proper rest and nutrition.
As a rule, it is possible to eliminate the pathology within three to six months with timely and correct therapy. First of all, conservative methods are used for this. If no improvement is observed during the specified period, other therapeutic measures are also added. Congenital pathologies, as a rule, cannot be completely cured.
In order to prevent congenital anomalies of the visual system, a pregnant woman must follow the prescribed regimen and undergo routine examinations by the attending physician and ultrasound examinations. To prevent acquired lesions, it is necessary:
- Observe safety precautions at work;
- Avoid traumatic situations;
- Avoid complications in the event of infectious diseases;
- Systematically undergo examinations by an ophthalmologist (at least once a year);
- Monitor and promptly treat systemic diseases.
If you experience discomfort, pain, or deterioration in focusing, you should consult a doctor as soon as possible. A positive treatment outcome is possible if the disease is detected only in the early stages of its development.
Conclusion
Paresis of the oculomotor nerve is one of the most dangerous diseases of the visual apparatus for humans. The disease is difficult to stop and treat, but its timely detection usually increases the chances of recovery. In addition, proper prevention of pathologies of the nervous system and visual organs will help to avoid complications.
Prices for services *
*The information on the site is for informational purposes only. All materials and prices posted on the site are not a public offer, defined by the provisions of Art. 437 Civil Code of the Russian Federation. For accurate information, please contact the clinic staff or visit our clinic. The list of paid services provided is indicated in the price list of the Yusupov Hospital.
*The information on the site is for informational purposes only. All materials and prices posted on the site are not a public offer, defined by the provisions of Art. 437 Civil Code of the Russian Federation. For accurate information, please contact the clinic staff or visit our clinic.
As a result of head injuries and other unfavorable factors, paresis of the oculomotor nerve occurs. The condition is accompanied by drooping of the upper eyelid, double vision, and lack of pupillary response to light. At the first symptoms, you should consult a doctor who will conduct a diagnosis, prescribe medications and therapeutic exercises for the eyes, perform surgery and give preventive recommendations.
Diagnostics
The main method for diagnosing neuropathies is a neurological examination. In addition to it, instrumental and laboratory methods are also used. Of the instrumental diagnostic methods, electrophysiological study of peripheral nerves, namely electromyography, is of particular importance.
Laboratory methods include tests to detect specific antibodies and antigens that are characteristic of autoimmune and demyelinating diseases.
It consists of a visual examination, examination of reflexes and identification of specific symptoms for damage to a particular nerve.
Visual examination and questioning for facial neuropathy
The doctor asks the patient to close his eyes tightly and wrinkle his forehead. With neuropathy of the facial nerve, the fold on the forehead on the side of the injury does not gather, and the eye does not close completely. Through the gap between the non-closed eyelids, a strip of sclera is visible, which gives the organ a resemblance to the eye of a hare.
Next, the doctor asks the patient to puff out his cheeks, which also does not work, since the air on the affected side comes out through the paralyzed corner of the mouth. This symptom is called sails. When you try to bare your teeth, there is an asymmetry of the mouth in the shape of a tennis racket.
When diagnosing facial neuropathy, the doctor may ask the patient to do the following:
- close your eyes;
- frown;
- raise eyebrows;
- bare teeth;
- puff out your cheeks;
- try to whistle, blow.
Next, the doctor asks about the presence of taste disorders, and whether the patient has problems with chewing (
does food get stuck while eating
The doctor pays special attention to how the disease began and what preceded it. Was there a viral or bacterial infection? Since the third type of herpes virus can persist in the nerve ganglia for a long time, it is very important to mention whether or not there was an infection with the herpes virus.
It is easiest to recognize the lesion, since this pathological process is characterized by drooping eyelids, dilated pupils and abnormal deviations of the eyes. Based on such signs, making a diagnosis will not be a problem, but often they are combined with each other in various combinations, so the doctor suspects the secondary nature of the disease.
- Fundus examination;
- Determination of visual acuity and degree of mobility of the eyeball;
- Light reflex test;
- Angiography (to identify vascular pathologies);
- Magnetic resonance imaging (checks brain tissue for abnormalities).
Sometimes a consultation with a neurologist may be required. If it was not possible to determine the cause of the pathology, then the patient should be registered with a doctor and periodically examined. To prevent the condition from getting worse, your doctor may recommend special sets of exercises and other treatment methods.
The trochlear nerve innervates the oblique muscles of the eyeball, but what else does it do?
Probably every adult has heard about the presence of 12 pairs of nerves in the skull, which are the most important in the entire human nervous system. The position of these nerves is so key that any damage to them provokes the development of pathology in another node of the body.
The fourth pair of twelve has a trochlear nerve, which carries out a huge number of important functions for humans. We will talk about them, location, purpose and other features of the trochlear nerve in the material presented below.
Anatomical features
Trochlear nerve - 4th pair of cranial nerves
The trochlear nerve is a representative of the fourth pair of cranial nerves. It has a rather complex anatomy, but if we simplify the information for understanding, we can highlight the following:
- the nuclei of this nerve are located in the position of the lower colliculi of the midbrain cover (the anterior part from the central gray matter, the lower part from some nuclei of the oculomotor nerve);
- along its length, the trochlear nerve goes around the central parts of the gray matter from the outside, then organizes a kind of cross relative to the top of the medullary velum, after which it leaves the midbrain (the lower part from the lower colliculi);
- exits from the medulla relative to the dorsal part of the brainstem (the only one of 12 pairs of nerves that exits the brain in this way);
- The trochlear nerve also passes around the lateral part of the cerebral peduncle, dissects the temporal lobes along the fissure, pierces the meninges and goes into the ocular cavity, where it is located not far from the optic and oculomotor nerves.
Thanks to such a complex but well-thought-out nature of the organization, the trochlear nerve is fully capable of performing its basic functions without entering into confrontation with other cranial elements.
Functional purpose
The trochlear nerve provides visual function of the eye
The functions of the trochlear nerve are quite important for the stable functioning of the human eyes and, accordingly, the organization of uninterrupted visual function. First of all, we note that the trochlear nerve innervates the superior oblique muscle of the eye.
It is this innervation that determines the main function of this nerve - moving the eye along the axis downwards and outwards. That is, one of the six muscles that control the human eyeballs is controlled by the trochlear nerve. Thanks to it and a number of other nerves, people can:
- move both eyes simultaneously;
- turn them towards the temple;
- move the eyeball relative to the upper and lower positions.
Thus, the trochlear nerve is responsible for:
- lack of isolation in the movement of the eyeballs (you cannot move them differently);
- organization of contractions of the eye muscles and, accordingly, stable visual function.
Any deviation in the functioning of the trochlear nerve provokes a violation of visual function, which directly affects a person’s ability to see.
The video material will familiarize you with the anatomy of the oculomotor nerves in more detail:
Possible nerve damage
The trochlear nerve, like any other node in the human body, is susceptible to certain types of dysfunction. In general, the pathological condition of this nerve is that it cannot perform its functions correctly, as a result of which the following appear:
- inability to move the eyes or one of them in some directions;
- making the eyeballs or one of them incorrectly positioned;
- development of other dysfunctions associated with the specification of the trochlear nerve.
As a rule, a separate lesion of the trochlear nerve is a rarity, which practically does not occur in modern medicine.
However, it happens that the fourth pair of cranial nerves, along with the third, are affected at the genetic level, as a result of which their congenital pathologies develop.
But this phenomenon is quite rare, so most pathologies of the trochlear nerve are associated with its acquired lesions.
Most often, damage to the trochlear nerve appears in patients who already have such ailments as:
- Microangiopathy. Causes spontaneous and systematic contraction of the muscle controlled by the trochlear nerve, or problems with the vessels adjacent to it. An illness of this type is always accompanied by pain and is distinguished by the severity of its appearance.
- Intracranial aneurysm. Causes complete or partial dysfunction of pairs of the cranial nerve system, the symptoms of which are similar to those observed with microangiopathy.
- Traumatic brain injury of any type. In the presence of such a problem, the trochlear nerve is paralyzed, as a result of which the symptoms described above are observed.
- Glaucoma of most formations. Accompanied by the same phenomena that are inherent in damage to the trochlear nerve due to traumatic brain injury.
- Pathology of the cavernous sinus. Accompanied by the same phenomena that are inherent in damage to the trochlear nerve due to traumatic brain injury.
- Hemorrhage into the medullary velum, through which the trochlear nerve passes. Accompanied by the same phenomena that are inherent in damage to the trochlear nerve due to traumatic brain injury.
- Tumor of the thyroid gland (less commonly, the epiphyses and cerebellar regions), diabetes mellitus, infectious pathologies of the eye (encephalitis, meningitis, etc.) and trauma to the eyeball. These problems cause partial or gradually developing damage to the trochlear nerve, so irreversible consequences can often be avoided.
Pathologies of the trochlear nerve are quite dangerous for a person’s visual function, as they can provoke irreversible damage to it, which in turn affects a person’s ability to see.
In order to minimize the risks of such outcomes, if any problems with the eyes appear, it is important to get rid of them, and immediately.
Symptoms of trochlear nerve pathologies
Trochlear nerve pathologies will not go unnoticed
It is important to understand that the symptoms of the pathological condition of the trochlear nerve may vary in cases with different histories of the problem. However, there are three main symptoms that accompany most pathologies of the fourth pair of cranial nerves. These include:
- Diplomia is pronounced double vision. This dysfunction occurs when concentrating on a certain object with both eyes. If it is the trochlear nerve that is affected, diplomacy appears in absolutely all directions of gaze, with the exception of the top.
- Tilt of head to shoulder. This phenomenon is provoked by the fact that the central nervous system tries to compensate for double vision by adjusting the human body to look. Almost always the head deviates to the side that is opposite to the affected one.
- Strabismus. When the trochlear nerve is affected, the affected eye or both of them deviate towards the nose. This type of strabismus is called convergent.
The appearance of these symptoms, especially in combination, is a sure sign of damage to the trochlear nerve. It is impossible to hesitate in such a situation, so postponing and, even more so, ignoring a visit to an ophthalmologist is simply unacceptable.
Diagnosis of dysfunctions
Trochlear nerve: schematically
Due to the specificity of damage to the human trochlear nerve described above, their diagnosis is carried out in a special order. In particular, the following must be carried out:
- Empirical examination methods:
- examination of the width of the palpebral fissure, the size of the pupil and the fit of the eyeball;
- checking the reaction of the pupil to light;
- diagnostics of the correct convergence of apples and accommodation (focusing on objects close and far away).
- Specialized examination techniques related to “visiting” the internal region of the brain (MRI, CT, etc.).
- Conducting a series of tests on the patient (blood, urine, etc.).
- Eye examination by an ophthalmologist using special equipment.
- Analysis of the patient's symptoms.
Only in combination will the diagnostic methods described above make it possible to identify not only the damage to the trochlear nerve itself, but also the cause of its appearance. It is the latter that determines how the treatment will be carried out and whether it is possible in principle.
If the functioning of the trochlear nerve is subject to complete or at least partial restoration, then the following types of therapy are possible:
- Medication (for viral pathologies).
- Surgical (if the lesion is traumatic in nature).
- Restorative (with partial damage to the nerve).
A more accurate treatment option is determined exclusively by a professional ophthalmologist, taking into account all the features of a particular patient’s case, so it will not be possible to get rid of the pathology of the trochlear nerve on your own. In general, summarizing the material presented today, it is worth noting that:
- Firstly, the oculomotor nerve performs very important functions for organizing stable human visual function.
- Secondly, any damage to it negatively affects the body, provoking extremely unpleasant pathologies.
- Thirdly, when the latter appear, it is important to start getting rid of them immediately, since any delay increases the risk of developing irreversible consequences.
We hope today's article was useful to you and provided answers to your questions. Good health to you!
Select it and press Ctrl+Enter to let us know.
Source: //glaza.online/anatomija/innerv/blokovyj-nerv.html
Treatment of paresis and abducens nerve palsy
The abducens nerve as a component of the nervous system
Recovery after paralysis occurs over a long period of time throughout the year. A well-known method of treatment is the use of physiotherapy - exposure to low-frequency electromagnetic field pulses and electric current stimulation.
https://www.youtube.com/watch?v=h_NgYBnbXpc
The treatment method has an analgesic, anti-inflammatory, calming effect. The disadvantage is that recovery is very slow, and in some cases does not occur at all.
The oculo-occipital method of administering the drug (neuromidin) is also used to increase muscle contractility and influence defects in the connective muscles.
The method of using electrophoresis with a solution of 15% neuromidine has proven itself well. The duration of the sessions is 15 minutes daily for 15 days. After completing the procedure, it is recommended to lie down with your eyes closed for 10 minutes.
If improvement and restoration of the functioning of the abducens nerve is not observed after treatment, and the lesion does not go away on its own, surgical intervention is used. The essence of the method is as follows: an injection of ultracaine is made under the conjunctiva, and a half-circumference incision is made.
The superior external and inferior straight nerves are split into two bundles lengthwise and the lower fibers are sutured to the upper fibers. This allows you to rotate the eyeball by more than 15–20° within a day after surgery, in some patients up to 25°; binocular vision was restored in every fourth person operated on.
To alleviate the condition of impaired binocular vision, Fresnel prisms are used, which are attached to glasses. Prisms have different angles and are selected individually. Possibly also closing one eye.
Most nerve diseases are associated with a disorder of the central nervous system, so treatment is prescribed accordingly. After suffering infections and successful treatment, the nerve damage is restored. In rare cases, when the tumor is inoperable, there is serious injury to the skull and the nerve itself, recovery may not occur.
Noticed a mistake? Select it and press Ctrl Enter to let us know.
A person is able to move the eyeball thanks to 3 cranial nerve pathways. The main role in this process is played by the oculomotor nerve, which goes under number 3. It is responsible for the movements of the eyelid and eye, as well as its reaction to exposure to light. The abducens nerve controls the abduction of the eyeball, and the trochlear nerve turns it outward and downward. These nerve pathways are numbered 6 and 4.
Any disturbances in the innervation of the extraocular muscles affect the ability to see fully. Among such disorders, one can highlight paresis of the eye muscles in children, since in addition to the main causes that are characteristic of adults, they often exhibit congenital anomalies.
They are usually treated using a whole range of procedures, and in especially severe cases, surgery is used.
Causes and symptoms
Abducens nerve palsy usually manifests as isolated paralysis. In this case, a person cannot fully avert his eyes and a double image of one object appears (diplopia).
This phenomenon occurs due to a violation of the innervation of the lateral muscle, for which the abducens nerve is responsible.
However, similar symptoms are characteristic of diseases of the orbit, so you should undergo a detailed diagnosis to make a diagnosis.
Damage to the trochlear nerve causes partial paralysis of the eye and the person has a double image in an oblique or vertical plane.
This symptom intensifies when the eye is lowered down, so people suffering from this pathology often walk with their heads tilted to the healthy side to reduce the manifestation of diplopia.
During diagnosis, myasthenia gravis (autoimmune pathology of nerve and muscle tissue) and diseases of the orbit should be excluded.
Oculomotor nerve palsy usually occurs in conjunction with disruptions of the facial, abducens, and trochlear nerve pathways. A separate form of pathology appears extremely rarely. The oculomotor nerve is damaged primarily due to an aneurysm. It often occurs on the posterior communicating artery and gradually compresses the nervous tissue.
The oculomotor nerve can be damaged by a growing tumor, as well as manifestations of stroke and multiple sclerosis. In most cases, such factors affect the nucleus of the nerve tract and the posterior longitudinal fasciculus.

Sometimes neuropathy of the oculomotor nerve, caused by the above reasons, manifests itself in the form of bilateral drooping eyelids (ptosis). In more rare cases, paresis of the superior rectus muscle of the eye is observed.
It is localized on the reverse side of the main site of damage.
According to statistics, the oculomotor nerve is often damaged due to a microinfarction. It can occur due to vascular pathologies, such as diabetes and hypertension. Such diseases usually do not immediately lead to disruptions in cerebral circulation and they should be predominantly in an advanced state.
Neuritis of the oculomotor nerve does not affect the reaction of the pupil to light, but in rare cases it is slightly weakened. A microinfarction occurs near the cavernous sinus or in the area of the interpeduncular fossa. It takes about 3 months for the oculomotor nerve to recover after suffering a disorder.
Diagnostics
It is easiest to recognize damage to the oculomotor nerve, since this pathological process is characterized by drooping eyelids, dilated pupils and abnormal eye deviations.
Based on such signs, making a diagnosis will not be a problem, but often they are combined with each other in various combinations, so the doctor suspects the secondary nature of the disease.
Sometimes a consultation with a neurologist may be required. If it was not possible to determine the cause of the pathology, then the patient should be registered with a doctor and periodically examined. To prevent the condition from worsening, your doctor may recommend special sets of exercises and other treatment methods.
Course of therapy
Treatment methods for paresis of the eye muscles in children are not particularly different from those in adults. However, it must be borne in mind that most congenital anomalies are corrected through surgery.
If the operation is successfully performed, the extraocular muscles are partially or completely restored.
If the problem is compression of the nerve pathway, then the main task is to eliminate the cause.
For this purpose, exercises that strengthen the oculomotor muscles are often used. They serve as the basis for the treatment of minor injuries and are a good preventive measure.
In severe cases of the disease, therapeutic exercises well complement the main course of therapy.
Drug therapy for paresis of the eye muscles may include the following:
- Vitamin complexes;
- Preparations for strengthening the extraocular muscles and restoring their innervation;
- Eye drops;
- Medicines that improve blood circulation;
- Corrective glasses and bandages.
The pathology can be treated with medications only according to the regimen prescribed by the doctor, so as not to aggravate its course and not to impair vision, especially if the child is sick. It is recommended to combine drug therapy with other methods, namely:
- Steriopictures. By watching them, the extraocular muscles are trained and blood flow improves. The nerve tissues that innervate the muscles of the eye are extremely tense during the procedure, due to this the lost innervation is restored. The procedure must be carried out under the supervision of a specialist so as not to cause complications;
- Electropheresis. This physiotherapeutic procedure is carried out with a 1.5% solution of Neuromidin. The duration of one session of electropheresis usually does not exceed 20 minutes, and it acts directly on the synapses (junctions) of the muscle and nervous tissue of the eyeball. After a course of such therapy, the patient’s severity of paresis decreases and the innervation of the eye muscles improves.
It is impossible to eliminate some causes of paresis of the eye muscles in children, for example, congenital anomalies, without surgical intervention. Their duration and degree of risk depend on the type of operation and the factor that influenced the development of the pathology. In the case of severe damage to the optic nerves, it will not be possible to completely eliminate the problem, but there will be a chance to save the child’s vision.
Due to paresis of the extraocular muscles, many complications develop, such as strabismus, ptosis, etc. In children, this pathological process is often a consequence of congenital anomalies. It may not appear immediately, but only over time. This is why it is important to see an ophthalmologist and other doctors, especially in the first years of a child’s life.
The most common pathological conditions from damage to the abducens nerve are limited mobility (paretic state) or complete loss of motor ability (paralysis).
In a normal state, the edge of the iris of the eye is able to touch the commissure of the eyelids on both sides - the section of the eye is closer to the ear and to the nasal septum on the opposite side.
If this ability is impaired, a diagnosis of the onset of a pathological condition of the abducens nerve can be made.
Pathologies are characterized by the following conditions:
- The eyeball has limited mobility;
- Double vision, slight trembling of the eyelid;
- Peripheral deviation of one of the eyeballs;
- The position of the head is inclined towards the damaged eyeball;
- Damage to the vestibular apparatus, loss of coordination.
In a simplified way, the state of the abducens nerve is checked by an independent attempt to maximally abduct the eyeball: right-to-right, left-to-left. If it is impossible to abduct the right one, then a lesion of the right abducens nerve has occurred and similarly for the left nerve.
Is the trochlear nerve connected to the brain?
There are 12 pairs of nerve tracts in the human skull.
The proper functioning of the entire nervous system in the body depends on them. Any, even minor, disruption of their work leads to various malfunctions in the organs and systems of the body. Among all cranial pairs, there is the trochlear nerve.
In order to understand its role in the performance of the body, it is necessary to consider in detail the location of the nerve.
Anatomical features of the trochlear nerve tract
The trochlear nerve is the fourth of twelve pairs. This is the only pathway that extends beyond the back of the brain stem. In the region of the inferior colliculi of the midbrain there are two nuclei of the trochlear nerve pathway. If we consider the location in relation to the oculomotor nerves, then the trochlear nerve is located lower.
This pair forms a kind of crosshair on a gray plate, which in medicine is classified as a sail that forms the lid of the stomach. The trochlear nerve tract then exits through the midbrain and is directed inferiorly from the inferior colliculi. Each pair goes around the cerebral peduncle from the sides.
At this point, the trochlear nerve pathway penetrates through the temporal fissure, which is located between the lobe of the cerebral hemisphere and its peduncle. Then it goes anteriorly and penetrates the membrane of the brain. Thus, the nerve path reaches the outer wall of the cavernous sinus.
At this point, its path does not end; it penetrates through the superior palpebral fissure, reaching the very orbit, where it exits directly to the superior oblique muscle tissue of the eye.
Functional significance of the trochlear nerve
The main function of the fourth pair of cranial nerves is to ensure forward and downward movement of the eyeballs. During normal operation of the visual organ, several axes of rotation of the apple are distinguished. Six muscles are involved in this process. Thus, the following movements are distinguished:
- Movement of the eyeballs towards the temple;
- Turn to the nose;
- Lifting up, or rolling the eyes;
- Lowering down.
A unique feature of the human eye is its symmetrical movement. During normal operation of the visual organ, the eyes are always directed in one direction. The trochlear nerves are part of the group of oculomotor nerve tracts, along with the abducens and oculomotor.
If a person’s correct functioning of at least one of these areas is disrupted, then the entire visual function is immediately disrupted. Thus, both eyes should move symmetrically with each other, excluding rotations in different directions (the eyeballs should not move independently, each rotating along its own axis).
A pair of extraocular muscles on the left and right sides should always contract simultaneously.
Research methods
Since the trochlear nerve innervates the visual organ of the human body, research methods must include all procedures that study the correct functioning of the eyes. In order to accurately determine whether a given pair of cranial nerves is working correctly, doctors use special study methods:
- First of all, it is checked how a person sees, whether there is a feeling of double vision in the surrounding world;
- the width of the palpebral fissures is carefully studied;
- the size of the pupil is determined and compared with normal values;
- the position of the eyeballs in the orbit is studied;
- it is very important to check the reaction of the pupil to light;
- the convergence of the eye is examined using a hammer (the object approaches the tip of the nose, at this time the doctor examines whether the movements of the eyeballs are correct when bringing them to the center);
- accommodation is tested (to do this, close one eye, and the second looks first at a distant object, then at a near one, while describing its sensations).
The trochlear nerve, like any other, can be damaged. As a result, diseases develop. Since the main task of this path is to bring the organ into movement, that is, it causes contraction of muscle tissue, the pathology consists of paralysis - lack of movement.
The patient's eyeball stops moving upward and inward. This becomes especially noticeable if the patient climbs stairs. Another common symptom of trochlear nerve damage is double vision. All objects repeat their outlines, which significantly interferes with a person’s ability to look.
Desync results in the image being projected twice on different parts of the retina.
In severe cases, the entire group of oculomotor nerve pathways may be affected. In this situation, the person’s eye will not move at all, and the pupil will dilate significantly and stop responding to light.
If such a picture is observed in both eyes at once, then we can conclude that the nuclei of the nerve pathways are affected. Most often, such problems are observed after illness with neurosyphilis, meningitis, thrombosis, or aneurysm.
In modern medicine there is no effective therapy that could completely restore the functioning of the motor nerves of the eye. Therefore, a person must try to maintain his health, including his nervous system in order. It is better to prevent a disease than to treat it for a long time.
Source: //anatomiy.com/blokovoy-nerv.html