Neurocirculatory dystonia (NCD) is a disorder in the functioning of the cardiovascular system, which is associated with certain pathologies of physiological neuroendocrine regulation. Most often, NCD is observed in women of reproductive age and adolescents due to severe stress or severe physical strain. This disease is much less common among people under fifteen years of age and over forty years of age.
Despite the variety of types and symptoms of the disease, it proceeds quite benevolently, and in most cases does not lead to the further development of serious heart problems. Usually, if the patient applies in a timely manner, a favorable prognosis is noted (in most clinical cases, complete recovery is noted). Quite often, neurocirculatory dystonia is confused with certain diseases of the nervous and cardiovascular systems. For example, the course of this disease is very similar to panic attack syndrome, some types of cardiopathy, tonsillocardial or hyperkinetic syndromes. Symptoms of this disease in most cases arise sharply and suddenly, their frequency is unpredictable, and they also appear unexpectedly. But it is quite possible that the disease will last a long time and become chronic. In this case, periods of exacerbation and stagnation of symptoms alternate. Often exacerbations are associated with the seasonality of the seasons.
NCD of the hypertensive type: what is it?
The NDC classification was developed by Professor Makolkin. It is based on the human body’s responses to the altered functioning of the autonomic nervous system, which regulates the activity of internal organs and systems. There are 2 departments:
- sympathetic;
- parasympathetic.
Attention!
When the parasympathetic system is activated, the work of internal organs accelerates. The sympathetic department is responsible for reducing the speed of functions performed by the organ. The balance of these systems ensures the coordinated functioning of the whole organism.
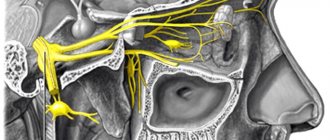
NCD is an imbalance between the sympathetic and parasympathetic divisions of the NS. There is a predominance of one of the types of regulation, which affects the function of organs. For example, the situation requires acceleration of the contraction of the heart muscle, but it, on the contrary, slows down. NCD develops when there is a predominance of parasympathetic regulation. The functional activity of organs depends on the volume of incoming blood. The larger it is, the faster the work is done. This mechanism underlies the control of the life activity of the system. It is carried out with the help of vasodilators and vasoconstrictors, which contribute to the expansion or narrowing of the lumen of blood vessels. This is how the blood flow to the somatic organs and the autonomic nervous system is controlled.
The hypertensive type is formed when there is a failure of the sympathetic regulation of the ANS. During normal functioning of the body, vascular tone increases when a particular organ requires more nutrients and oxygen. The disease is characterized by frequent and untimely increases in vascular tone, which causes an increase in systolic blood pressure.
How NDC is developing
The development of this disease lies in the interaction between the central nervous system and cardiovascular autonomic reflexes:
- predisposing and producing factors change the normal secretion of mediators released by the brain at the level of the GABAergic, serotonergic and adrenergic systems;
- the functional relationship between the limbic-reticular zone, cortex and hypothalamus is disrupted;
- the relationship between the hypothalamus, pituitary gland and adrenal glands changes - this is manifested by significant changes in hormonal activity;
- as a result, there is a release of adrenaline into the blood, increased activity of the microcirculatory bed appears, which causes metabolic and regulatory disorders in the heart and blood vessels.
With proper treatment of NCD, acute symptoms of dystonia disappear quickly, and in some cases disappear on their own without treatment when the action of the provoking factors ceases. But most often the course of the disease resembles a chronic organic pathology with alternating periods of exacerbations and remissions.
Types of disease
Neurocircular dystonia is divided into types:
- Hypertensive. Blood pressure is constantly elevated, its numbers do not depend on the age aspect.
- Hypotonic. Characterized by low blood pressure and pulse. Patients complain of constant lethargy and apathy.
- Mixed type. Combines the characteristics of the previous two types. It is impossible to predict which option will prevail in a particular situation.
According to the etiology of the disease, the following types are distinguished:
- essential (the leading role is played by the factor of heredity);
- psychogenic (the disease is provoked by a traumatic situation or stress);
- infectious-toxic;
- constant physical stress;
- features of the patient's profession.
According to the severity of the course, NCD is divided into:
- light;
- moderate severity;
- heavy.
Causes
The disease is based on a combination of various factors. But the pathology is not associated with the occurrence of organic disorders of the endocrine system or structures of the nervous system. The reasons are:
- frequent overwork;
- chronic lack of sleep;
- physical inactivity;
- regular overexertion due to excessive physical activity;
- psycho-emotional stress;
- somatic diseases;
- traumatic brain injury;
- acclimatization;
- disruption of endocrine regulation;
- acute infectious process.
Attention! A certain role is played by genetic predisposition to the disease and the individual characteristics of the patient’s body. The risk of developing NCD is higher in those people whose relatives suffer from diseases of the cardiovascular system.
Frequency of occurrence of NDC
The diagnosis of NCD is extremely common. Due to the busy pace of life, NCD is more often detected in the urban population of working age and ranges from 25 to 79% of the total number of volunteers examined.
In patients with cardiovascular complaints, this diagnosis is made in 40% of cases. In adolescence, when the cardiovascular and nervous systems have not yet reached their maturity, such disorders prevail over organic diseases and account for up to 75% of cases. The most common age of diagnosis is between 20 and 40 years. Mostly women are affected.
Signs
Pathology can manifest itself in different ways. The clinical picture consists of a combination of the following symptoms:
- weaknesses;
- chronic fatigue, which manifests itself after minor physical exertion;
- occurrence of pre-fainting conditions;
- changes in heart rate parameters;
- headaches;
- difficulty breathing, shortness of breath;
- insomnia;
- pain, discomfort in the heart area, behind the sternum;
- tendency to weather sensitivity, weather dependence.
Heart rate rises to 100 beats/minute. Patients note increased sweating and coldness of the skin of the upper extremities. Hyperhidrosis can occur locally or affect the entire body. There is a tendency to cutaneous dermographism. It is characterized by a change in skin color after mechanical impact. If you rub it with a sharp object, it leaves a white mark that does not disappear for a long time.
Attention! The patient has a different combination of clinical signs, which alternate periodically. It is usually not possible to record all symptoms at the same time. Over time, their combination may change.
Crises and symptoms of neurocircular dystonia
The development of the disease is based on disruption of the heart and blood microcirculation, expressed in a decrease in blood pressure. The body, using available resources, tries to neutralize the problems that have arisen. At the same time, oxygen starvation of tissues manifests itself, the resistance of peripheral vessels decreases, and drops in venous pressure occur.
Disease syndromes:
- General weakness. Accompanied by fatigue, exercise intolerance, and minimal efficiency.
- Orthostatic manifestations. There is a sharp decrease in pressure, even to the point of fainting. When changing body position, flickering appears in the eyes, the urge to vomit, and dizziness.
- Cardiac syndrome. This symptom occurs in 30% of patients with NCD and is marked by short-term painful squeezing sensations in the area of the heart or stabbing pain radiating to the left side of the back and arm. The pulse is usually slow, and disturbances in the rhythm and duration of the heartbeat are recorded.
- Cerebral symptoms. This includes dull headaches in the forehead area, aggravated by any type of stress. It is often combined with dizziness and further fainting.
- A reflex type of disadaptation (numbness of the hands, decreased thermal balance of the body, cyanosis on the extremities).
- Combined syndrome combines several of the above manifestations.
NDC sometimes has a crisis course. The picture of the phenomenon is a sharp drop in blood pressure followed by fainting (collapse). Additional symptoms are unpleasant symptoms in the heart, headache. A characteristic feature of patients with NCD is an increased emotional and anxiety level.
Features during pregnancy
Carrying a child is a physiological condition, but this period has pitfalls - diseases that previously had a latent course are revealed. This also applies to neurocirculatory dystonia. During gestation, a woman's hormonal levels change. The growing uterus leads to displacement of internal organs, changing their normal position. The changes in organ function that occur often become pathological. This is due to a violation of autonomic nervous regulation.
If a woman has neurocirculatory dystonia, the first sign of pregnancy is syncope. At this time, the symptoms become more pronounced, which negatively affects the well-being of the pregnant woman. The main manifestations of circular dystonia of the hypertensive type during gestation are:
- tearfulness;
- hysterics;
- pain in the heart area;
- blood pressure fluctuations;
- feeling of lack of air.
Establishing a diagnosis
The most important task is to differentiate neurocirculatory dystonia from myocarditis, hypertension and neurotic conditions. To establish a diagnosis, the doctor conducts an instrumental examination.
Table 3. Diagnosis of NCD.
| Diagnostic method | Description |
ECG tests | The method includes medicinal, orthostatic and physiological tests with hyperventilation. |
Bicycle ergometry | Helps identify deterioration in exercise tolerance in a person. |
Blood analysis | Performed after exercise. Helps identify increases in blood pressure and lactic acid. |
Note! An echocardiogram is not a 100% accurate diagnostic method. Typically, it only detects concomitant diseases.
Treatment
Before starting therapy, the causes that are responsible for the occurrence of exacerbations of the disease should be identified. If possible, they need to be eliminated. Often the disease is caused by psycho-emotional overload, which is caused by the work schedule and working conditions. In this situation, the solution would be to refuse overtime work and reduce the overall workload on the employee. When negative factors are eliminated, the doctor prescribes medication support. Its tasks include the normalization of autonomic nervous regulation.
Attention! It is important for such patients to adhere to a healthy lifestyle. It consists of giving up harmful addictions (alcohol, nicotine, drugs), proper nutrition, combating physical inactivity, including gymnastic exercises in the daily regimen, and normalizing daily biorhythms.
Drug therapy
To improve the functioning of the nervous system, it is recommended to take:
- multivitamin complexes (B vitamins, magnesium);
- sedatives (Novo-passit, Persen, alcohol tincture of valerian, motherwort, peony);
- antidepressants;
- medications that improve microcirculation (Glycine, Cinnarizine);
- tranquilizers;
- antihypertensive drugs (ACE inhibitors, calcium antagonists).
Physiotherapy
The goal of physiotherapeutic treatment is to consolidate the results that were achieved by taking medications, improving blood circulation in the structures of the brain, and metabolic processes. The following treatment options may be prescribed:
- acupuncture;
- electrophoresis;
- massage;
- magnetotherapy.
A course of massage of the cervical-collar area can significantly improve the patient’s well-being. A good effect can be achieved using current techniques. One option is electrophoresis on the cervical-collar area using nicotinic acid. It causes vasodilation and improves cerebral circulation. During treatment, the severity of negative symptoms decreases and the function of the central nervous system normalizes.
Non-drug treatment
As an alternative therapy or adjunct to therapy, the primary care provider may recommend:
- infusion of medicinal plants that have a sedative effect;
- breathing exercises;
- physical therapy;
- yoga classes;
- swimming in the pool.
Medicinal herbs you can use:
- pharmaceutical chamomile;
- valerian root;
- lemon balm;
- sage.
NDC and age
According to statistics, NCD is often diagnosed in childhood and adolescence. Its cause is considered to be high rates of growth and development of the child. Patients in these age groups are characterized by low blood pressure, so they are diagnosed with hypotonic type NCD.
Medications are rarely used to treat the disease in adolescents and children. Usually the signs disappear after the active growth phase ends. If the manifestations of the disease reduce the quality of life or negatively affect academic performance, the doctor may recommend non-drug therapy. But only if there is no positive effect, he will prescribe pharmacological agents.
NDC and the army
The patient receives a medical exemption from military service for several reasons:
- persistent hypertensive state (increased blood pressure more than 160/100 mm Hg);
- presence of constant complaints;
- decreased performance;
- heart rhythm disturbance.
If the diagnosis is detected for the first time, the conscript is sent for examination in a hospital setting. After six months, the young person must re-pass the selection committee. If there are no significant changes in well-being within six months, blood pressure remains elevated, and he is considered unfit for service.
Neurocirculatory dystonia in a child
Neurocirculatory dystonia in a child
Neurocirculatory dystonia (NCD) in children is a syndrome of functional (lately considered structural-functional) disorders of the cardiovascular system, caused by inadequacy of its regulation.
This is a polyetiological disease, the main symptom of which is lability of pulse and blood pressure, as well as cardiac and respiratory discomfort, vegetative and psycho-emotional disorders, disturbances of vascular and muscle tone, low tolerance to stressful situations, benign course and prognosis.
This is a fairly common disease in both children and adults. NCD is based on a violation of the neuro-endocrine regulation of cardiovascular activity, a violation of adaptation mechanisms to rapidly changing exo- and endogenous factors.
The reasons causing the development of NCD are the following:
- Hereditary predisposition matters. These are individual characteristics of the functioning of the nervous and endocrine systems, individual psychophysiological characteristics of the body.
- Social factors - alcoholization of the family, single-parent family, improper upbringing of the child (over- or hypo-custody).
- Mental trauma of varying degrees, especially in children with a weak type of nervous activity.
- Infectious diseases, chronic intoxications.
- Age-related features associated with puberty (endocrine changes in the body), excess body weight and associated dissonance of the cardiovascular system.
Clinical manifestations and principles of diagnosis of NCD
In patients with NCD, with varying degrees of frequency, a wide variety of subjective and objective symptoms are observed, and their division is quite arbitrary. Local symptoms of the cardiovascular system and general neurotic signs are distinguished.
The most typical and frequent complaints are pain and discomfort in the heart area. Cardiac syndrome with NCD in its typical form is easily differentiated from pain in the heart of another origin.
There are two types of pain in the heart area:
- The first type is in patients with hyperreactivity: “point” pain, limited, often in the area of the apex of the heart, intensifies with inspiration and decreases with exhalation. Patients are forced to hold their breath. The pain is not associated with physical activity.
- The second type of pain in the heart area is pain that is also limited in area, but usually “dull”, prolonged, can last up to a day, is not associated with physical activity, or minor physical activity can relieve cardialgia, and can radiate to the shoulder or armpit.
Palpitations can be a subjective symptom in the form of a feeling of palpitations. In some patients, bradycardia may be detected. disappearing with little physical activity. A number of children experience tachycardia, which is sometimes paroxysmal in nature under the influence of emotional factors or extrasystole.
The second important sign of NCD is respiratory disorders, which have nothing to do with breathing disorders in heart or pulmonary failure. This is a feeling of “lack of oxygen” (as patients put it), especially manifested in stuffy rooms or during excitement, when there is a need to increase breathing. Inhalation becomes difficult, incomplete, a feeling of compression appears behind the sternum, the patient is forced to take forced deep breaths, which sometimes bring relief. In some cases, respiratory crises occur.
The next cardinal sign of NCD is extreme lability of the main hemodynamic parameters in the form of unusual fluctuations in pulse rate and blood pressure, which occur spontaneously and can be detected with Holter monitoring. These shifts are easily provoked by excitement, minor physical effort, prolonged vertical position of the body, and forced breathing.
The accuracy of determining blood pressure using the Korotkoff method depends on the correct measurement of blood pressure. The correct choice of cuff size is important. Currently, they are produced in several types (M-35, M-55, M-85, M-130), where the number corresponds to the width of the pneumatic chamber. When using one standard cuff (usually M-130), it is necessary to correct the blood pressure value.
Normal blood pressure should be considered its values when systolic and diastolic blood pressure are in the zone of the 10-90th centile of the blood pressure distribution curve. Blood pressure values between the 90th and 94th centiles are conventionally called “high normal blood pressure.” Despite the somewhat unfortunate formulation, he warns against hasty diagnosis of hypertension, which can cause unnecessary mental trauma to the child and his parents.
The diagnosis of arterial hypertension is made when, with three measurements of blood pressure, it is in the 95th centile zone. The diagnosis of arterial hypotension is made when blood pressure readings are in the 10th centile zone.
Among the factors that determine blood pressure levels in children are the following:
Body weight - there is a direct correlation between body weight and blood pressure (especially in girls),
Genetic factors - increased blood pressure is more often observed in children who carry the histocompatibility antigen HLA-A -11, B-22.
Environmental factors - family relationships, relationships at school
Autonomic dysregulation, especially the prevalence of the sympathetic-adrenal system
Dietary errors - excessive consumption of table salt and insufficient potassium
Increased production of uric acid.
As the child ages, blood pressure increases. This increase varies by gender. SBP in boys increases by an average of 2 mm. rt. century per year, in girls - by 1 mm. rt. Art. The annual increase in DBP is on average 0.5 mm. rt. Art. At 10–13 years of age, SBP is usually higher in girls, and after 13 years of age – in boys.
Based on the above, diagnostic criteria for NCD were formulated (V.I. Makolkin 1996).
The “main” criteria (signs) are identified. These include:
- Peculiar cardialgia, characteristic only of NCD, which are easily relieved by taking the so-called. “heart” remedies, such as Corvalol, Valocordin, valerian, motherwort
- Characteristic respiratory disorders in the form of a feeling of “oxygen starvation”, a feeling of insufficient inhalation, tachypnea, a decrease in maximum pulmonary ventilation and an increase in residual air,
- Extreme lability of pulse and blood pressure
- Changes in the final part of the ventricular complex in the form of negative “T” waves, mainly in the right precordial leads, layering of the U wave on the “T” wave, as well as the syndrome of early ventricular repolarization. Extrasystoles may appear
- The characteristic lability of the “T” wave and the “S-T” segment during a series of functional tests (tests with potassium, obsidan, etc.)
Additional criteria (signs) are as follows:
- Signs of a hyperkinetic state of blood circulation,
- Vegetative-vascular symptoms (vegetative-vascular “crises”, dizziness, headaches, low-grade fever, temperature asymmetries, myalgia, feeling of internal trembling,
- Psycho-emotional disorders in the form of anxiety, restlessness, irritability, cardiophobia, sleep disturbances,
- Asthenic syndrome (weakness, low maximum oxygen consumption, reduced tolerance to physical activity),
- The course is benign, without signs of the formation of “gross” pathology of the cardiovascular system, neurological and mental disorders.
A reliable diagnosis of NCD is established if two or more criteria of the “main” group and at least two criteria of the “additional” group are present. Or another diagnostic option - you need to have 3 syndromes out of 4 - cardiac, impaired blood pressure, respiratory and neurasthenic. A prerequisite for diagnosing NCD as a nosological form is the mandatory exclusion of organic pathology.
Hypertensive form of NCD - along with general symptoms, there are periodic rises in blood pressure to the borderline level and above, and predominantly systolic blood pressure increases. There are no signs characteristic of essential hypertension or essential hypertension (changes in the fundus vessels, myocardial hypertrophy, etc.).
The hypotensive form of NCD - along with the general symptoms, there is reduced blood pressure, decreased performance, and a tendency to faint.
Cardiac form - general symptoms in combination with cardialgia with normal blood pressure. The course is without crises or permanent and with crises. The occurrence of crises is facilitated by mental trauma, emotional stress, and heart rhythm disturbances.
Sympatho-adrenal crises develop in sympathicotonic people. Typically - anxiety, severe headaches. mainly in the temple area, pulsating, pallor and dryness of the skin and mucous membranes, white dermographism, dilated pupils, increased shine of the eyes, tachycardia, increased blood pressure, tremor, increased body temperature in the presence of cold extremities. Strengthening the functions of automaticity and conductivity. contractility, excitability, the “P” wave increases in standard leads 11 and 111, S-T shifts below the isoline. The “T” wave becomes flattened. In the blood - leukocytosis, hyperglycemia, hypercoagulation, acidosis, hypercalcemia, increased levels of ketone bodies and decreased acetylcholine. After a crisis, polyuria with low urine density and asthenia are possible.
Vago-insular crises - in patients with initial vagotonia - narrow pupils. Pronounced skin hyperemia, sweating, hypothermia, decreased blood pressure, bradycardia, arrhythmias. reduction of the “P” wave, A-B blockade, S-T interval above the isoline, widening of the QRS complex. There is a urge to urinate, swelling, and abdominal pain. rumbling in the stomach, profuse diarrhea. Sometimes, at the height of the crisis, paraallergic reactions appear in the form of Quincke's edema. In the blood - hypoglycemia, leukopenia, lymphocytosis, hypocoagulation, slowing of ESR, alkalosis, hypocalcemia, increased acetylcholine levels.
Mixed crises are combined symptoms.
Hyperventilation crisis—lack of air, tachypnea up to 30 per minute. decrease in “CO 2” in the blood with the development of respiratory alkalosis, increased blood pressure, tachycardia. Hyperventilation tetany develops - “obstetrician’s hand”, carpopedal spasm. extremities are cold. wet.
Vegetative-vestibular crisis occurs against the background of hypotension and allergies. These crises are provoked by sudden turns of the head and changes in body position (orthostasis). They arise suddenly and are accompanied by hypotension, dizziness, nausea and vomiting. In the mechanism of occurrence of these crises, a sharp increase in the activity of beta-2 adrenergic receptors is important, with dilation of skeletal muscle vessels, a sharp drop in total peripheral resistance and a drop in blood pressure and a decrease in cerebral blood flow.
The severity of crises is determined primarily by their duration. The severity of NCD (mild, moderate and severe).
Mild NCD - neurasthenic syndrome is mild, cardialgic syndrome is rare and mild, crises occur very rarely. The patients' physical activity and performance were preserved.
Moderately severe form of NCD - there is a polymorphism of clinical manifestations, crises are mild and moderately severe, changes on the ECG are possible, physical performance is reduced by 50%. These patients require drug therapy.
Severe form of NCD - there are multiple persistent symptoms. Cardialgic syndrome is pronounced, crisis states are frequent. The physical activity and performance of patients is significantly reduced. They need hospital treatment.
Differential diagnosis of NCD is carried out with the following pathology:
The cardiac form of NCD is differentiated from diseases accompanied by pain:
- carditis, coronaritis
- myocardial dystrophy
- congenital heart and vascular defects
- with pathology of the ribs, muscles, peripheral nerves (myositis, Tietze syndrome, costoclavicular syndrome, “sliding costal cartilage” syndrome), with pathology of the pleura, lungs, mediastinal organs.
The hypertensive form of NCD is differentiated from secondary hypertension:
1) Renal hypertension
- OGN, CGN.
- Amyloidosis of the kidneys - manifested by severe proteinuria, in the absence of pathological changes in the urine sediment and clear signs of the inflammatory process according to blood parameters (significant acceleration of ESR, dyspteinemia)
- Pyelonephritis. polycystic kidney disease, interstitial nephritis, renal tuberculosis, kidney tumors, reflux pathology in the form of reflux nephropathies of varying severity
- Vaso-renal hypertension - general signs of vasorenal hypertension are: a) a decrease in the size of the kidney on the affected side by 0.7-1.0 cm. b) delayed appearance and long-term preservation of the nephronogram on the side of stenosis, c) hyperconcentration of contrast on the affected side , d) segmental atrophy of the kidney, e) absence of kidney function with a normal morphological picture according to retrograde pyelography, f) spirilization of the ureter
- atherosclerosis of the renal arteries, fibromuscular dysplasia
- Takayasu's disease or aortoarteritis of the renal arteries or polyarteritis nodosa (characterized by clinical signs of collagenosis),
- aneurysm or hypoplasia of the renal artery
- nephroptosis - leads to orthostatic hypertension, this pathology can be suspected when hypertension appears after the patient has been in an upright position for 30 minutes
- Freyley's syndrome is a typical classic triad of signs - 1) abdominal pain, 2) hematuria, 3) superior calyx syndrome (according to excretory urography)
- External compression of the renal artery
2) Endocrine hypertension:
- acromegaly
- Itsenko-Cushing's disease
- pheochromocytoma – there is increased urinary excretion of vanillylmandelic acid (VMA)
- Conn's syndrome or primary hyperaldosteronism is characterized by polyuria, hyposthenuria, neutral or alkaline urine reaction. Muscle weakness, paresthesia, and convulsions are typical. The ECG shows signs of hypokalemia (decreased S-T interval, decreased “T”, appearance of a “U” wave
- diffuse toxic goiter
- hyperaparathyroidism
- adrenogenital syndrome is a congenital dysfunction of the adrenal cortex. It is characterized by early sexual and physical development, rapid growth in children up to 11-12 years of age, followed by its cessation and closure of growth zones. Hirsutism, an abnormal structure of the external genitalia in girls (significant enlargement of the clitoris). Increased levels of 17-hydroxyprogesterone (17-HOPS) in urine and blood
- Pubertal basophilism - or hypothalamic syndrome of puberty or pubertal dyspituitarism - typically obesity. good physical development, accelerated puberty, cutaneous striae, as well as diencephalic disorders - thirst, bulimia, thermal asymmetry, increased urinary excretion of 17-KS and 17-OX
- Cerebrogenic AG tumors or other organic processes in the central nervous system
3) Cervical osteochondrosis
4) Hemodynamic hypertension - coarctation of the aorta, hypoplasia of the aorta, aortitis, aortic insufficiency. PDA, 111th degree AV block, congestive hypertension in heart failure
5) Hypertension of medicinal origin - taking steroids. NSAIDs, etc.
6) In the hypotensive form, it is necessary to exclude:
- physiological hypotension (in athletes, as an individual variant of the norm, adaptive hypotension in tropical residents),
- symptomatic hypotension – chronic adrenal insufficiency. hypothyroidism
Principles of therapy:
- timeliness,
- complexity,
- duration of therapy,
- pathogenetic impact taking into account the form of the disease,
- psychotherapy (not only for the child, but also for the parents)
- participation of a neurologist in the treatment process.
Main types of therapy:
- Normalization of work and rest, daily routine. Daytime rest (sleep) is required
- Normalization of child nutrition (timeliness, quality)
- Psychotherapy
- Acupuncture
Physiotherapy - for NCD in the hypertensive form, warm pine baths, sea baths, electrophoresis on the collar area with papaverine, dibazole, euphilin are indicated. For NCD in the hypotensive form - contrast baths, showers (Charcot, circular) and electrophoresis on the collar area with calcium, mesatone. caffeine, massage this area.
Drug therapy - Therapy of metabolic disorders, especially of the cardiovascular system - (vitamins, potassium preparations, ATP, phosphadene) or nootropic drugs - aminalon, glutamic acid, nootropil.
Psycholytics - tranquilizers (seduxen, elenium) or neuroleptics (sonapax, teralen). Dehydration agents - diacarb according to the scheme. Absorbable agents - lidase For the hypertensive form - sedatives (valerian, motherwort), for the hypotensive form - adaptogens (Eleutherococcus, Schisandra, Aralia, Pantocrine), for the mixed form - bellataminal, belloid. During crises - sympatho-adrenal - papaverine. dibazol, antidepressants. vagoinsular crisis - caffeine, adrenaline.
Need a doctor? We will choose the best!
Prevention
To avoid the development of the disease, you must:
- to refuse from bad habits;
- avoid overload (emotional, psychological, physical);
- do not forget to do simple gymnastics and play sports;
- maintain a daily routine;
- adhere to the principles of proper nutrition;
- spend more time outdoors.
Doctors recommend periodically undergoing a course of general massage and manual therapy. If a cold or other infectious process occurs, seek medical help in a timely manner. If you have chronic stress, visit a psychotherapist. Patients with hormonal imbalances should be treated by an endocrinologist.
Prognosis and possible complications
Complications of neurocirculatory dystonia of the hypertensive type include the occurrence of a crisis. Its symptoms come on suddenly. There are several types of it:
- vagoinsular;
- sympathetic-adrenal;
- mixed.
The prognosis for the disease is favorable; it does not pose a threat to human life. If the development of symptoms is influenced by any provoking factor, they go away on their own. In elderly patients, due to the disease, low performance and decreased reaction speed may be observed.
Neurocirculatory asthenia of the hypertensive type can be considered a fairly harmless disease (compared to other nosoological forms). But if the patient does not pay attention to the manifestations of the disease and does not receive appropriate treatment, over time this will lead to a decrease in quality of life and impaired performance.
Diagnostics
Due to the very high prevalence of the disease and the similarity of its symptoms with some other diseases, diagnosis by neurologists, pediatricians or therapists cannot be done without additional examinations using:
1. MRI and cardiac CT.2. 24-hour blood pressure measurement.3. ECG test with exercise.4. Cardiography.5. Radiography.
In addition, a standard examination is prescribed:
- General blood analysis.
- General urine analysis.
- Blood chemistry.
- Ultrasound of all major organs.