Schizophrenia is a severe mental illness characterized by a tendency to constant relapse and progression. There are several forms of pathology, differing in the predominant symptoms and course: fur-like, catatonic, etc. Therapy for schizophrenia is complex and is based on the use of medications that help stop the manifestations of the disease and increase a person’s social adaptation. Psychiatrists divide the treatment of the disease into several stages, in each of which it is recommended to use different tablets.
Basic principles of therapy
In psychiatry, schizophrenia is understood as a group of mental disorders characterized by disturbances in the emotional and mental sphere. Complete recovery is impossible, however, with the help of proper therapy, the symptoms of the pathology are eliminated and its recurrence is prevented in the future. This improves the patient’s social adaptation and ability to work.
Stages of therapy:
- Treatment in the acute period to eliminate symptoms of psychosis. The drugs used suppress delusions, hallucinations, catatonia and other positive symptoms.
- Stabilizing therapy consolidates the effect of the previous stage, eliminating remaining symptoms.
- Maintenance treatment is aimed at maintaining a stable state of the patient’s mental sphere and preventing the development of relapses.
Treatment in the acute period should be prescribed at the first manifestation of symptoms. This is due to the fact that when an attack lasts for a long time, stopping it requires large doses of medications and the use of combinations of psychoactive drugs. This may cause side effects.
The first stage of therapy against the background of acute psychosis is carried out during hospitalization of the patient. Subsequent stabilizing and maintenance therapy can be carried out on an outpatient basis. It is important to note that, despite the disappearance of symptoms with maintenance treatment, the patient should be under the supervision of a psychiatrist for the timely identification of precursors of exacerbation.
Schizophrenia medications
Advice from lawyers:
1. I did not always take medications, which contributed to the development of schizophrenia. There are Examples where a cause-and-effect relationship has not been established.
1.1. And what is the crux of the matter?
Did the answer help you?YesNo
Consultation on your issue
8
Calls from landlines and mobiles are free throughout Russia
2. My brother has schizophrenia, the doctor says that without registration we will not be granted disability, and that the medicine is very expensive.
2.1. Hello! Make a temporary registration.
Did the answer help you?YesNo
3. Disabled from childhood, group 3, free medicines this year. But they give almost nothing. At the same time there is schizophrenia. If the Pension Fund refuses free medications for the next year (in order to receive some money), will they continue to provide free medications for schizophrenia?
3.1. Please contact your local FSS department with this question.
Did the answer help you?YesNo
4. My brother has a group 2 disability with a diagnosis of schizophrenia. He is registered at a psychoneurological dispensary. We buy medicine ourselves, with our own money. We live in a rented house with stove heating... How much money should the state pay in benefits (pensions)? City, Pskov.
4.1. Contact the social security office at the place of residence of the disabled person and they will provide you with a list of benefits for both firewood and electricity costs.
Did the answer help you?YesNo
5. The psychiatric dispensary does not remove the diagnosis of schizophrenia. I have not been admitted to the hospital for 5 years and have not taken medications. I have never been to the dispensary. They refuse to conduct a VK commission, where to write complaints, to the prosecutor’s office, to the Ministry of Health, to the Federal Service for Healthcare Supervision, or to immediately file a claim in court. ?
5.1. Good evening! Get an expert opinion and go to court!
Did the answer help you?YesNo
5.2. And they won't take it off. If a diagnosis of schizophrenia is made, then it is forever. Schizophrenia is incurable in our country. There are long periods of remission, 5 and 10 and 15 years... But the diagnosis is not removed. It is useless to write complaints... And if you haven’t gone to the dispensary yet, there is no reason to conduct a commission... You need to be registered and come to the doctor on time...
Did the answer help you?YesNo
6. The doctor refuses to deregister him from the PND after 5 years. I didn’t take any medications, I found out by chance that I wanted to get a certificate from the police department, they don’t deregister the diagnosis, which I found out 25 years later, schizophrenia, whether the actions of the PND dispensary were legal, requests and correspondence with the dispensary about deregistration did not bring any results, what further actions to take to deregister?
6.1. Go to court under Article 131 of the Code of Civil Procedure of the Russian Federation. During the process, a medical examination will be appointed, which should confirm or refute the doctor’s conclusion about your illness, taking this into account, a decision will be made on the basis of which you will be removed from the register. You can also contact the personal account of any lawyer selected on the site and receive legal services by concluding an agreement under Article 779 of the Civil Code of the Russian Federation for drawing up a claim.
Did the answer help you?YesNo
6.2. You can have this account removed in court. The claim is filed in accordance with Article 131 of the Code of Civil Procedure of the Russian Federation at the location of the PND. For more detailed advice, please review your documents.
Did the answer help you?YesNo
7. I am disabled group 3 (indefinitely) I want to remove the group because I want to learn my license and drive! Diagnosed with F25 (schizophrenia), but for 6 years I have not taken medication and have not received either outpatient or inpatient treatment! Because of my disability group, I can’t get a good position, although my knowledge allows it?
7.1. Hello! Based on the requirements of the Ministry of Health, indefiniteness from group III can be removed if the patient’s condition improves. It should be noted here that even having the status of “lifelong disability” will force a person to be under the supervision of doctors all the time. Therefore, if the slightest signs of improvement in well-being are detected, the patient’s lifelong disability status is removed. Also, the following factors will be a reason for lifting the indefinite period: - violation of the test procedure; - fictitious, dubious documents; — gross delays in deadlines for patients; - positive dynamics of the course of the disease. Based on this, it follows that in order for you to have your disabled status removed, you must contact the state medical authorities with an application to convene an ITU to undergo it.
Did the answer help you?YesNo
8. I am diagnosed with paranoid schizophrenia. The last time I was in the hospital was three years ago. For three years I did not visit the dispensary and did not take medications. I feel great. I am convinced that I am healthy. I want to remove this disease from the register, since I will soon return from maternity leave and get a job. Last week I had a psychologist and a medical examination today. They told me to check in once every three weeks for three months. Can I get rid of this disease through the court?
8.1. You can go to court.
Did the answer help you?YesNo
9. We have a disabled child, diagnosed with schizophrenia. He is 10 years old. Doesn't want to go to school, tantrums. He began to attack me and my grandmother with his fists. In short, I can’t cope with it, I’m mentally exhausted. We take medicine. Is it possible to register him in a boarding school and take him away on weekends? What is needed for this and will the child and care pension be preserved? I'm not working right now, but I would like to get a job.
9.1. Good morning! If you place your child in a boarding school and pick him up on weekends, you will automatically lose your pension, because he will be on state support and his pension will go to the state.
Did the answer help you?YesNo
9.2. Hello! If your child is in a psychoneurological boarding school, you will only be paid part of the pension. To register, you need to go to the hospital where you are registered. All the best to you, with respect, Yulia Likhogray.
Did the answer help you?YesNo
10. In schizophrenia, you can get pregnant and give birth to a child and take psychotropic medications after birth, feed and continue psychotropic medications in the registry office, we didn’t say anything in marriage, who is guilty and who to appeal to in court, yes.
10.1. Good day, dear visitor. Of course, in this case, you need to contact the guardianship authorities with a statement. Good luck to you in resolving your issue.
Did the answer help you?YesNo
10.2. This is a medical issue, not a legal one. For all recommendations, you should contact your attending psychiatrist.
With schizophrenia, pregnancy and childbirth are quite possible, even while taking medications. There are no doctors at the registry office.
Did the answer help you?YesNo
11. Please tell me whether patients with schizophrenia are entitled to free medications for concomitant diseases such as high blood pressure and high cholesterol. Where can I find the relevant resolution? I am a group 3 disabled person.
11.1. Hello, Natalia What medications you are prescribed, your attending physician will tell you and give you a prescription to get them at the pharmacy, given that you are disabled. I wish you good luck and all the best!
Did the answer help you?YesNo
12. A friend’s brother is registered at a psychoneurological dispensary, after receiving his education he was not hired anywhere in the city at all, difficulties in communicating in a team, and a complex character, he does not communicate with anyone at all and did not communicate either at school or in educational institution. Diagnosed with schizophrenia, the medication makes him unable to drink well. He sits at home all day. What can you say about this?
12.1. “What can you say about this?” Hello! Anastasia, what can I say here?! The problem is not legal, but medical. Psychiatrists and psychologists should speak here. Good luck and good luck to you!
Did the answer help you?YesNo
13. What will happen if a disabled person of group 2 with schizophrenia does not pay child support for more than 2 years, he was ordered through the court to pay 3 tons of rubles monthly, can he be imprisoned, or something else, the trouble is that he does not have enough of this The pension itself, let alone medicine, even food.
13.1. If you put him in jail, he won’t put you in jail, even though he may not be held criminally responsible; schizophrenia – usually a person is declared insane during an examination and may be sent for compulsory treatment..
Did the answer help you?YesNo
Consultation on your issue
8
Calls from landlines and mobiles are free throughout Russia
14. Should a guardian live with the ward if: she is declared completely incompetent (schizophrenia) and cannot independently perform any actions (cook, shop, take medications, do housework, etc.)
14.1. Good afternoon. Must.
Did the answer help you?YesNo
15. Can a person refuse to take medication during outpatient treatment with a diagnosis of schizophrenia?
15.1. He may refuse.
Did the answer help you?YesNo
16. How, if you have a group 3 disability and are diagnosed with schizophrenia, get medications that are not on the list for free. Who to contact?
16.1. Decree of the Government of the Russian Federation of July 30, 1994 N 890 (as amended on February 14, 2002) “On state support for the development of the medical industry and improving the provision of medicines and medical products to the population and healthcare institutions” Appendix No. 1 to the Decree of the Government of the Russian Federation of July 30, 1994 N 890 LIST OF POPULATION GROUPS AND CATEGORIES OF DISEASES FOR WHICH OUTPATIENT TREATMENT MEDICINES AND MEDICAL PRODUCTS ARE DISCHARGED ACCORDING TO DOCTORS' PRESCRIPTIONS FREE OF CHARGE Schizophrenia and epilepsy - ALL medicines are free. Contact your doctor.
Did the answer help you?YesNo
17. What to do? I am being treated for paranoid schizophrenia. I took medications as prescribed by the doctor - an injection of Moden-Depo 1 ml every 3 weeks for a period of 1 year. I have a group 2 disability. At the reception, I asked to cancel the injection. But the doctor, without giving any reasons, increased the interval from 3 weeks to a month. I give the injection without feeling the need for it and was refused to cancel it.
17.1. This is a medical issue, not a legal one...
Did the answer help you?YesNo
18. I have this situation. My mother has been diagnosed with schizophrenia for more than 10 years. She stopped taking medication and began to experience an exacerbation, which manifests itself in the form of aggression towards all her friends and relatives. She was admitted to the hospital, but she refused to undergo treatment and began to behave calmly so that she could be released. A trial was scheduled. Please tell me what are the chances that she will be treated there and how to prove to the court that her condition has worsened?
18.1. Competent doctors, during the examination, can see the progress or regression of the disease, but on your part only witness testimony, if there are recorded bodily injuries or damage to property, then bring these facts to the attention of experts and the court.
Did the answer help you?YesNo
19. The husband, a 20-year-old patient with schizophrenia, was sent to the hospital, there was no medicine, they were told to bring azaleptin and haloperidol, do they have the right to this, they say that if the patient does not agree, they will not treat him, although there are already signs of aggression towards strangers. Are the doctors right?
19.1. Yes. they are right.
Did the answer help you?YesNo
20. The husband inherited part of the house and land of his parents. The other part of the house and plot goes to his brother's children. My husband is disabled, group 2 schizophrenia, but takes medication; he has a daughter who was adopted before his illness. The first wife does not know that she is not his own, she died. If he gives his share to his adopted daughter. Can my brother's children protest the deal? And what can be done to protect the interests of the child.
20.1. Let your spouse draw up a deed of gift for your daughter from a notary, and it will also be even better if the deed of gift is prepared by a notary. My brother's children don't need to know about this.
Did the answer help you?YesNo
My son was diagnosed with schizophrenia - how long should he stay in hospital?
This is the situation. A diagnosis of paranoid schizophrenia was made. Was treated at the dispensary for 0.5 years (took light pills)
Is it legal to keep a patient in a temporary detention facility until trial, i.e., until Monday morning?
My stepfather has schizophrenia and needs constant medication, but refuses to be treated; he is not dangerous to others, but he is a danger to himself.
I am diagnosed with recurrent schizophrenia. I currently live abroad.
The guy was drafted into the army - he was fit, after 3 months he was written off with a diagnosis of sluggish schizophrenia, he sits at home, does not go to doctors, without a pension, without a job, what should I do?
Tell me, is it possible to give a third disability group to a person who was diagnosed with low-grade schizophrenia 12 years ago?
Please tell me what to do if the PND refuses to hospitalize a chronic mental patient (since 1976)
How to pacify a drinking son with schizophrenia. Takes prescribed medication and drinks alcohol.
My mother is sick with schizophrenia and recently, due to the death of my father, she stopped taking her medications, which significantly worsened her condition.
I want to obtain guardianship over my grandfather. My grandfather was diagnosed with schizophrenia, was in a psychiatric hospital, and is registered with a psychiatrist.
Drug groups
Various pharmacological groups of drugs are used to treat schizophrenia. Most of them are neuroleptics or antipsychotics that eliminate productive symptoms. All antipsychotics are usually divided into the following subgroups:
- atypical: Risperidone, Amisulpride, Clozapine, etc.;
- the newest atypical antipsychotics: Sertindole, Blonanserin, Aripiprazole;
- neuroleptics with a pronounced sedative effect: Levomepromazine, Propazine, Chlorpromazine;
- antipsychotics that activate the brain: Haloperidol, Clopixol, Tioproperazine, Fluphenazine;
- drugs with a disinhibiting effect on the central nervous system: Carbidine and Sulpiride.
Tablets from this list are used in all patients with schizophrenia. They allow you to stop an acute attack, and are also used as anti-relapse treatment.
In addition to antipsychotics, the following groups of medications are used:
- antidepressants from the subgroup of selective serotonin reuptake inhibitors (Fluoxetine) and heterocyclic agents (Amitriptyline, Pirlindol);
- nootropics that improve thought processes and normalize memory: Pantogam, Piracetam, Phenotropil, etc.;
- in case of severe anxiety, tranquilizers are prescribed - Diazepam or Phenazepam;
- psychostimulant medications: Mesocarb, etc.
The use of homeopathic drugs to normalize night sleep and reduce anxiety (Tenoten, etc.) is contraindicated, since such drugs do not have proven effectiveness and safety of use.
Treatment of productive symptoms
The main group of psychotropic drugs for the elimination of hallucinations, delusions and other productive symptoms in schizophrenia are antipsychotics (neuroleptics). These medications have been used in psychiatry for 50 years and show good results. All antipsychotics are usually divided into two large groups: typical and atypical. They differ from each other in the severity of the effect and the risk of side effects. Typical antipsychotics (Aminazine, Haloperidol) can lead to the development of extrapyramidal disorders such as dystonia and parkinsonism, as well as other neurological symptoms and depression. Atypical antipsychotics (Risperidone, Clozapine, Amisulpride, etc.) have a higher level of safety for patients.

Typical antipsychotics Haloperidol and Aminazine
The main indications for the use of antipsychotics are productive symptoms in the form of delusions, hallucinations, illusions, behavioral disorders and mania. The drugs suppress these symptoms and promote clinical remission of schizophrenia. The following medications are most often used in therapy:
- drugs Risperidone and Amsulpride for patients who have signs of both productive symptoms and negative ones in the form of autism, depression, etc. (they allow you to increase the activity of certain areas of the brain, eliminating these manifestations);
- a universal drug - Olanzapine, which quickly relieves psychosis and is approved for use for most patients;
- when psychosis is accompanied by increased excitability and severe psychomotor agitation, it is recommended to use Quetiapine;
- catatonic and hebephrenic forms of schizophrenia require the appointment of Mazeptil, which eliminates motor disorders.
In severe forms of the disease, for example, with catatonic manifestations or prolonged psychosis, preference is given to classical antipsychotics, for example, Haloperidol. It effectively eliminates symptoms, however, it can lead to neurological disorders of an extrapyramidal nature. To prevent them, Cyclodol is used together with Haloperidol. New generation medications for schizophrenia combine the positive properties of both typical and atypical antipsychotics. These include Piportil and Clozapine.
Neuroleptics are used in standard dosages for 1-2 months. After relief of acute psychosis and stabilization of the patient’s condition, the patient is transferred to stabilizing therapy using lower doses of drugs or replacing them with “milder” ones.
If prescribed incorrectly, antipsychotics can lead to the following side effects:
- Drowsiness due to sedation. A similar effect can occur with the use of Clozapine, Olanzapine and Quetiapine.
- Extrapyramidal disorders in the form of akathisia and other types of disorders. Akathisia is manifested by a subjective desire to change position and a feeling of severe anxiety. Dystonia and parkinsonian symptoms are rare with the use of atypical antipsychotics.
- Taking Amisulpride or Risperidone tablets leads to an increase in prolactin levels. Other atypical antipsychotics also cause temporary hyperprolactinemia, however, its severity is less severe. A high level of prolactin in the blood affects the production of sex hormones in the body and can cause the development of pathological changes in the mammary glands and endometrium.
- Patients who use drugs for a long time increase the risk of developing obesity and associated negative consequences.
To prevent the development of side effects, the patient should be examined for existing contraindications before starting therapy. If adverse reactions occur during treatment, the medication used is changed to an analogue, preferably from a different pharmacological group.
By prescription only
According to statistics from the Ministry of Health, in 2020, 3,933,156 Russians went to hospitals with various mental disorders. Most of them probably received the help they needed: psychopharmacology today is moving quickly, and disorders that could not be treated 30 years ago are now successfully treated with medication. Revision N+1
together with talks about how psychopharmacology has developed and is developing and what awaits this area of research in the near future.
What was the treatment before?
At the beginning of the 20th century, at the dawn of psychopharmacology, researchers actively experimented with various substances in search of a drug to relieve the symptoms of mania, depression and other mental disorders. Before the discovery of antidepressants in the 50s of the last century, opium, as well as caffeine, ginseng and other tonic drugs of plant origin, were actively used to treat depression.
In 1949, the antimanic effect of lithium salts was discovered. Australian researcher John Cade injected lithium urate (lithium acid + uric acid) into guinea pigs, which were greatly sedated by the drug. The scientist came to the conclusion that mania in patients with various mental disorders is caused by a lack of lithium in the body, which at that time was already used in medicine as a medicine for gout and rheumatism, and since the mid-19th century - to relieve attacks of epilepsy.
The drug was tested on patients with manic-depressive psychosis: attacks became less frequent, but the side effects from an overdose were terrible - for example, the use of lithium as a substitute for table salt (lithium was added to it to compensate for its deficiency in the patient’s body) led to the death of patients.
In the United States, the use of lithium was banned until 1970. Today, lithium-based drugs are used to treat bipolar disorder and prevent its exacerbations. Mood stabilizer drugs, which today, in addition to lithium, include valproate, lamotrigine and other drugs, are collectively called mood stabilizers.
The first antidepressant was discovered by accident. In 1957, the drug iproniazid, which was used to treat tuberculosis, was found to have a side effect: patients receiving it experienced mild agitation.
In 1952, psychiatrist Jean Delais presented positive results for treating depression with isoniazid (another drug for tuberculosis), followed in 1953 by American psychiatrists Max Lurie and Harry Salzer who reported that the drug helped in 60 percent of cases of depression. The researchers called the effect antidepressant, and the drug an antidepressant.
It is worth noting that today in some countries isoniazid is withdrawn from circulation due to an unfavorable risk-benefit ratio in the treatment of depression. However, it remains in the arsenal of doctors as a drug for combination therapy of tuberculosis.
Surgical methods were also used. In 1942, neurologists Walter Freeman and James Watts published a report of 136 successful lobotomies. In their opinion, surgical intervention saved them from neuroses, psychoses and depression.
Only later did it become clear that a lobotomy essentially destroys and changes a person’s personality. Gradually this method was no longer used.
The first antipsychotic drug was chlorpromazine in 1952. It was originally used as an allergy medicine, but later became used to relieve the symptoms of schizophrenia.
Also in 1952, the drug reserpine was isolated from the Rauwolfia serpentine plant, which also began to be used as an antipsychotic. Over time, reserpine will give way to more effective drugs - synthetic neuroleptics and first-generation antipsychotics (haloperidol, triftazine and thioproperazine); a little later, modern atypical neuroleptics appeared, which patients tolerate better.
The modern round of development of psychopharmacology, which began in the mid-90s, is associated with studies of dopamine receptors and their role in higher nervous activity.
The active substance of the new drugs acts as a partial agonist and antagonist of some dopamine and serotonin receptors, which is effective for the treatment of schizophrenia, manic and depressive episodes of bipolar disorder and as an adjunctive therapy for major depressive disorder.
How to find new drugs
Since the late 1980s, high-throughput screening (brute force) methods have been used to search for new chemical compounds that can become the basis for drugs. The essence of the method is to search for compounds that best combine with target proteins—ligands—that determine the course of the disease.
The drug binds to the center of the protein and changes its functioning. Many diseases are caused by dysfunction of several proteins and the genes encoding them.
The interaction between the drug and the protein is similar to locking and opening a lock with a key. A molecule that can interact with the center of a target protein must meet a number of parameters (from the structure of the crystal lattice to physical requirements). Most often, it suppresses (inhibits) the activity of protein interaction with other molecules - and promotes healing.
A modern search method is virtual screening. With the help of supercomputers, drug developers can quickly search through tens or hundreds of thousands of compounds from databases in search of a ligand. But even taking into account the speed of the supercomputer, finding a suitable connection from all those recorded in the database would take too much time.
Therefore, in practice, researchers set conditions for the similarity of the desired compounds with existing drugs - this process is called drug-likeness.
For example, the molecular weight of the compound, hydrogen bond parameters, and so on are specified. Libraries containing millions of different substances are formed from compounds, with parameters for each of them.
The screening process looks simple: the test substances are distributed into a test system with thousands of wells containing the target protein. Further work is carried out with those wells where biological activity is detected.
Researchers identify active molecules (prototypes) and submit them for further research to medicinal chemists, pharmacologists, and molecular biophysicists. The necessary changes are made to the prototype, and then preclinical testing begins (on animals, then on groups of patients).
“I would like to dispel several myths regarding psychopharmacological drugs. Firstly, most psychotropic drugs do not cause addiction, except for a narrow group of drugs (benzodiazepines, tranquilizers and sleeping pills), as well as Corvalol and similar drugs containing phenobarbital. The main psychotropic drugs - antidepressants and antipsychotics - do not cause addiction or dependence, and long courses under the supervision of a doctor often make it possible to avoid the chronicity of mental illnesses and form a stable remission, and often completely recover,” says psychiatrist Igor Potapov, head of the department of non-drug methods treatment with an intensive care unit of the National Medical Research Center for Psychiatry and Narcology named after Serbsky (NMICPN) of the Ministry of Health of the Russian Federation.
According to Potapov, the second myth that haunts the mind is that psychopharmacological drugs “poison the body.” However, most medications, when used correctly, according to indications and under the supervision of a doctor, allow you to avoid side effects, which, of course, can occur.
“The fact is that doctors know the side effect profile and take it into account when selecting a specific drug for a patient. For example, some antidepressants may reduce appetite, while others may increase it. And this knowledge helps the doctor prescribe a drug that increases appetite to a patient whose depressive state is accompanied by severe weight loss due to decreased appetite, or even complete refusal to eat, which often happens to patients who suffer from depression. But, as I already said, modern psychotropic drugs have a favorable tolerability profile and are not much different from other drugs used in medicine,” explains the expert.

Share
The way to the counter
The path of a drug from the laboratory to the counter is long and thorny - it all starts with preclinical testing. In Russia, they can attract research organizations and educational institutions that have the necessary facilities and qualified specialists.
The drug is tested on animals: toxicity, allergenicity, mutagenicity, carcinogenicity, etc. are determined in order to minimize the likelihood of adverse reactions during clinical trials on groups of patients. At this stage, the possibility of further testing of the drug is determined.
Clinical trials of the drug in humans are extremely important, since many diseases, such as schizophrenia, have no analogues in the animal world. Often successful experiments on animals ended in unsuccessful tests on groups of patients.
Rules for engaging in clinical research are based on the 1947 Nuremberg Code, which prohibits experimentation on people without their voluntary consent, and on the ethical principles set out in the 1964 Declaration of Helsinki adopted by the World Medical Association.
The Constitution of the Russian Federation and a number of laws also prohibit medical interventions without the consent of the citizen.
To register a medicinal product, it is necessary to conduct successful clinical trials in Russia. Patients participating in such studies can thereby receive modern, effective and safe medications. On the website of the Association of Clinical Research Organizations you can find some data on clinical trials in the country.
It is possible to import unregistered drugs into Russia if a council of doctors from a federal medical institution prescribes the drug to a specific patient for health reasons.
To allow the sale of a medicine in Russia, state registration of the drug is required based on the results of the examination of the Scientific Center for Expertise of Medicinal Products. Specialists evaluate the benefits and risks of a new medicine, its quality, review the instructions and send a conclusion to the Ministry of Health.
The center operates exclusively on the instructions of the Ministry of Health - the institution is prohibited from providing services for the examination of medicines to individuals and companies.
On the portal of the Ministry of Health you can find information about issued permits for conducting clinical trials, a register of accredited medical organizations and similar materials.
If the medicine passes the examination and receives a positive conclusion, the Ministry of Health will include the drug in the State Register of Medicines and issue a registration certificate to the manufacturer. Registration is a long process; according to the law, it lasts 210 working days.
In 2020, a drug developed by . appeared on the market in the United States. It is intended for the treatment of schizophrenia, in particular for the treatment of positive and negative symptoms (you can learn more about what it is in our text “The Mind Thief”). In 2020, the drug began to be used in Europe, and in 2020 it was registered in Russia.
After a drug goes on sale, studies of its safety continue. The manufacturer carefully analyzes the identified side effects and reports them to Roszdravnadzor. In addition, physicians and patients can also report adverse events. Verified information can be added to the instructions.
“The development of any drug in medicine usually takes several decades. This is a very complex process - from the theoretical creation of a molecule to its synthesis and further many years of testing. Typically, it takes 20-25 years from the moment a molecule of a psychotropic drug is synthesized until the drug can be purchased at a pharmacy. In our country, the drug appears later, as additional tests are required to obtain registration. Usually, after registration of a drug in the USA and Europe, at least another 5-7 years pass before the drug appears in Russia, which allows the Ministry of Health to evaluate the clinical studies that have already been conducted before making such a responsible decision as registering the drug in the Russian Federation,” says Igor Potapov.
The future of psychopharmacology
Experts see the future of psychopharmacology in the development of personalized medicine, since a person’s unique physiological characteristics both play an important role in vulnerability to disease and predict response to specific treatment methods.
Unique characteristics of an individual include genetic changes and epigenetic modifications, clinical symptoms, biomarker changes, and environmental factors.
The goal of personalized medicine is to analyze a particular case of the body’s perception of a disease, make an accurate diagnosis and offer the most effective, yet safe treatment, based on the phenotypic profile (a unique set of the characteristics listed above for a particular patient). Unfortunately, there are still few examples of personalized medicine in psychiatry.
Among the trends at the 2020 Congress on Psychopharmacology are the problem of side effects of antipsychotics, the use of brain phenotyping to improve discoveries in psychiatry, therapies using artificial intelligence, and so on.
Igor Potapov says that modern pharmacological companies initially plan to create drugs with minimal side effects and better tolerability.
“Not everything can be planned, and setbacks may occur along the way to create a drug molecule. However, we can say with confidence that modern psychotropic drugs, when used correctly by an experienced psychiatrist, can help a person cope with mental illness without worsening his quality of life. Modern drugs in psychiatry are no different from drugs for the treatment of somatic diseases. Of course, when using any medicine, side effects may occur, but under the supervision of a doctor, they can usually be avoided,” the expert believes.
Maria Ruskova
Treatment of emotional disorders
A large number of patients with productive symptoms have an emotional component in the form of anxiety, aggression and other manifestations. To eliminate it, psychoactive drugs are selected that relieve emotional disorders:
- with severe manic agitation, a therapeutic effect is observed when using Quetiapine in standard dosages;
- Clopixol is used in patients with psychomotor agitation, anger and aggression; the drug is especially often used to treat patients with schizophrenia with withdrawal syndrome associated with refusal to take alcoholic beverages or drugs (there is a prolonged form of the drug - Clopixol-Acupaz, which allows you to take the medication less frequently) .

Psychoactive drugs Quetiapine and Clopixol
If atypical antipsychotics are ineffective during the first days of therapy, the psychiatrist transfers the patient to typical antipsychotics with a sedative effect. Their use lasts 10-14 days, during which psychomotor agitation disappears and the patient’s condition returns to normal. The main typical antipsychotics that exhibit a sedative effect are the following:
- Aminazine - used for psychoses accompanied by anger and aggression;
- if the symptoms of anxiety and restlessness predominate, it is recommended to prescribe Tizercin;
- Elderly patients, as well as patients with renal or liver failure, are prescribed Melperon and Chlorprothixene (these drugs do not affect the functioning of these organs and rarely lead to the development of side effects).
In addition to antipsychotics, antidepressants and mood stabilizers are prescribed to eliminate emotional disorders. Antidepressants normalize mood levels and reduce anxiety and restlessness in patients with schizophrenia. It is recommended to use selective serotonin reuptake inhibitors - Fluoxetine, Escitalopram and Zimelidine. Mood stabilizers, for example, lithium salts, reduce anxiety. These groups of drugs are used in the acute period of schizophrenia and during anti-relapse treatment.
Elimination of the depressive component
The main group of drugs to eliminate the depressive component are antidepressants. Preference is given to Fluoxetine and its analogues: Escitalopram and Venlafaxine. The latter medicine is recommended for use by patients who, in addition to depression, have increased levels of anxiety and restlessness. New drug trials show that the drug Ixel can eliminate depression with melancholy symptoms that create the preconditions for suicidal thoughts.
The use of heterocyclic antidepressants is limited due to low effectiveness and a high risk of side effects. Among them, Amitriptyline, Melipramine or Clomipramine are used as second-line therapy.
Treatment of the manic component
For severe mania, a combination of atypical antipsychotics and mood stabilizers is prescribed. It is recommended to continue such therapy during anti-relapse treatment, since schizophrenia is characterized by exacerbations of emotional disorders. The main sedative tablets are mood stabilizers Depakin and Valprocon. For mild mania, Lamotrigine is used, which has a weaker effect, but less often leads to side effects.
Lithium salts are considered universal drugs for eliminating the manic component of schizophrenia. Their use with typical antipsychotics is prohibited, as this may lead to adverse drug reactions due to interactions between the two groups of medications.
If psychosis is not relieved with the help of the specified list of drugs from the group of atypical and typical antipsychotics, then electroconvulsive therapy, insulin shock and other therapeutic approaches are possible.
Treatment of schizophrenia with anti-inflammatory and immunotropic drugs
Schizophrenia is considered a syndrome consisting of several disease phenotypes covering a number of underlying pathologies. One mechanism of this disease appears to involve immune dysregulation and neuroinflammation. While current antipsychotic drugs that block dopamine receptors reduce symptoms of psychosis and prevent relapse in most patients with schizophrenia, there is a great need to explore new options and treatments that target other parts of the pathogenesis. Such studies should be aimed at identifying reliable biomarkers for diagnosing and monitoring the immune biophenotype in schizophrenia and developing more effective anti-inflammatory and immunomodulatory drugs.
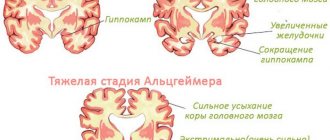
Immune dysregulation in schizophrenia has been found in numerous studies comparing patients with healthy controls, and meta-analyses show that patients with schizophrenia at the group level exhibit evidence of low-grade peripheral inflammation with upregulation of several proinflammatory cytokines and C-reactive protein (CRP). The main support for this hypothesis came from the results of genome-wide association studies (GWAS), which identified a strong genetic association between schizophrenia and the major histocompatibility complex (MCH) locus on chromosome 6. This genetic susceptibility may be partially explained by complement factor 4 (C4) variants. , possibly related to increased synaptic pruning during brain development. In addition, studies show an increased risk of developing schizophrenia in individuals with prenatal exposure to influenza or with elevated titers of IgG antibodies to Toxoplasma gondii, which likely work in conjunction with genetic background in etiopathogenesis. It is interesting to note that the pathological effect of prenatal infection may be a nonspecific effect of the inflammatory response and increased cytokine levels rather than a specific effect of a particular infectious agent. Moreover, studies of postmortem brains from patients with schizophrenia suggest increased microglial activity. It is likely that psychiatrists need theranostic biomarkers that predict the effects of treatment with anti-inflammatory or immunomodulatory drugs in patients with psychosis.
Although dopamine D2 receptor blocking antipsychotic drugs play an important role in the treatment of psychotic disorders, we urgently need new treatment options, primarily for the cognitive and negative symptoms of psychosis, particularly schizophrenia. Indeed, D2 blockers offer symptomatic relief of delusions and hallucinations and effective relapse prevention for most patients, but a disease-modifying effect of antipsychotics in schizophrenia has not been found. Immunomodulatory treatments can target pathological processes that are closer to the origins of the psychotic disorder than is the case with current D2 receptor blocking drugs and, accordingly, may only temporarily relieve the symptoms of psychosis.
Since 2002, several studies have been conducted examining the potential effect of nonsteroidal anti-inflammatory drugs (NSAIDS), estrogens, statins, EPA/DHA fatty acids, davunetide, minocycline, and N-acetylcysteine in schizophrenia. Additionally, research is emerging with monoclonal antibodies to cytokines or cytokine receptors, which may specifically target one component of the immune system and provide opportunities for precision therapy for psychosis. Note that this is a rapidly developing field of neuropsychiatry, which currently contains a number of well-established treatment options for various somatic and neurological disorders, such as multiple sclerosis.
Some authors emphasize that in most studies of inflammation in schizophrenia, about 40% of patients have some degree of inflammation. The proposal that immune dysregulation is involved in the pathogenesis of certain subgroups with schizophrenia is consistent with the concept that schizophrenia is a syndrome consisting of several disease phenotypes with a number of distinct pathogenesis links. One of these disease mechanisms may be related to immunity, while others may be more dependent on impaired energy metabolism or synaptic dysfunction. As several authors have already noted, we need reliable biomarkers to diagnose immune dysregulation in schizophrenia.
Tablets for stabilizing treatment
Stabilizing therapy is aimed at completely eliminating the productive symptoms of schizophrenia, as well as emotional disorders. The duration of treatment is 3-10 months, depending on the course of the disease in a particular patient. To stabilize the condition, atypical antipsychotics are used: Amisulpride, Quetiapine and Risperidone. They are used in smaller dosages than when eliminating acute psychosis. The drugs help eliminate apathy, speech disorders and changes in the emotional-volitional sphere.

Atypical antipsychotics Risperidone and Amisulpride
Psychiatrists distinguish long-acting forms of atypical antipsychotics, which are more convenient to use than their classical analogues: Fluanxol-Depot, Rispolent-Konsta and Klopiksol-Depot. The medications do not require frequent administration, which increases patient adherence to therapy and reduces the risk of missing pills. Fluanskol-Depot is recommended for patients with increased anxiety and various phobias. Rispolent-Konsta is used in patients who have residual productive effects in the form of hallucinations or delusions.
Typical antipsychotics are rarely used due to their pronounced effect and the risk of side effects. If atypical antipsychotics are not effective, Haloperidol, Triftazin, Montiden-Depot or Piportil are used. The latter is recommended for signs of catatonia or paranoid schizophrenia. The long-acting drug Montiden-Depot eliminates residual hallucinations and delusions.
Basics of treatment for schizophrenia
Every year, new generation drugs appear in the arsenal of doctors. The main part of therapy is the selection of medications. Drugs such as nootropics are used to stimulate brain function and enhance cognitive abilities. Below is a list of neuropleptics recommended by leading experts.
Reviews on them are also positive.
- Azaleptin . Clozapine is the active ingredient. Does not develop catalepsy or behavioral depression. In clinical settings, Azaleptin has a rapid sedative effect. The medicine is well tolerated by patients. Cost about 200 rubles.
- Galoper is an antipsychotic, neuroleptic, antiemetic agent. Prescribe with extreme caution to patients with cardiovascular pathology, predisposition to glaucoma, functional liver disorders, and those who experience epileptic attacks. The price, depending on the form of release, varies from 50 to 300 rubles.
- Zyprexa Zidis round tablets, yellow. A drug that affects a number of receptor systems. Price from 4000 rub.
- Clopixol-Acupaz – solution for injection. Used for the initial stage of treatment of acute mental, chronic psychosis (exacerbation). The cost of the drug is 2000–2300 rubles.
- Senorm – drops for oral administration. The active substance is haloperidol. Cost about 300 rubles.
- Propazine is a blue-coated tablet with inclusions and marbling. Has less pronounced side effects. Price about 150 rubles.
- Triftazin , solution in ampoules 0.2%. The active substance is trifluoperazine. Blocks dopamine receptors of various brain structures. Compatible with other neuroleptics, tranquilizers and antidepressants. The cost of 10 pieces per package is 50-100 rubles.
- Chlorprothixene 50 . Analgesic, antidepressant, neuroleptic, antiemetic, sedative. Average price – 350 rubles.

Schizophrenia is accompanied by a mood disorder. To bring the patient out of this state, mood stabilizers are used. Unlike antipsychotics prescribed for mania, mood stabilizers are used for bipolar affective disorder.
Relapse Prevention
Relapses of schizophrenia occur in most patients in the absence of supportive treatment. As a rule, the prescription of atypical antipsychotics (Risperidone, Clozapine) in a minimal dosage can reduce the risk of exacerbations, as well as disorders in the mental, emotional and volitional sphere. The dose of the drug to maintain remission is selected individually. As a rule, not only the dosage of the antipsychotic drug itself is reduced, but also the frequency of its administration.
For a single acute attack of any form of schizophrenia, maintenance therapy should last 2 years. If there were two attacks, then treatment with atypical antipsychotics takes 5 years. With 3 or more exacerbations, anti-relapse therapy continues throughout life.
New pills
Psychoactive drugs have been used in psychiatry for more than 50 years. During this time, several hundred different substances were created that were used to treat schizophrenia and other mental disorders. The main group of drugs are atypical or conventional neuroleptics (Haloperidol, Aminazine, etc.), leading to various side effects of the tablets. Most often, when using these drugs, patients experience extrapyramidal disorders, endocrine system disorders, depression and allergic reactions. The newest drugs for the treatment of schizophrenia, namely atypical antipsychotics, maintain a high level of effectiveness while significantly increasing the level of safety for the patient.
Risperidone and other atypical medications have a complex effect on the brain, regulating the level of neurotransmitters and the activity of its individual areas. This allows not only to ensure the elimination of productive symptoms, but also to improve cognitive functions and reduce the severity of emotional-volitional disorders in the form of depression, mania, apathy, etc. New antipsychotics include Quetiapine, Aripiprazole, Ziprasidone, Sertindole and Olanzapine.