Antibiotics for meningitis: list of drugs, indications, prevention
HomeBrain diseasesMeningitis Antibiotics for meningitis: list of drugs, indications, prevention
Meningitis is an acute infectious disease that is characterized by the occurrence of an inflammatory process in the membranes of the brain. The pathology has a progressive course and quickly leads to complications. Therefore, when symptoms of the disease appear, emergency treatment is required. The most effective method is antibiotics for meningitis, which affect the cause of the disease.
Epidemiological surveillance
Surveillance, from case detection to investigation and laboratory confirmation, is critical to the control of meningococcal meningitis.
Main objectives of surveillance:
- detection and confirmation of disease outbreaks;
- detection and confirmation of disease outbreaks;
- assessing the burden of disease;
- monitoring antibiotic resistance profiles;
- monitoring the circulation, spread and evolution of individual meningococcal strains (clones);
- assessing the effectiveness of strategies to control meningitis, in particular preventive vaccination programs.
How does meningitis develop?
Meningitis is an infectious disease, the etiological factor in the development of which is pathogenic microorganisms. Particles of the pathogen penetrate the bloodstream and reach the brain through the arteries, where they settle on its membranes.
Reproduction of the pathogen triggers an active reaction of local immunity, which leads to local tissue swelling and exudation of protective elements. This contributes to the development of the inflammatory process, which is externally manifested by the clinical picture of meningitis.
Symptoms are often caused by viral infections. These include:
- Flaviviruses;
- Enteroviruses;
- Cytomegaloviruses, Epstein-Barr virus;
- In rare cases - human immunodeficiency virus, encephalitis viruses, herpes simplex, varicella-zoster virus.
Another causative agent of the disease is a bacterial infection, and the following microorganisms may be involved in the development of the pathology:
- Meningococci;
- Hemolytic streptococci;
- Pseudomonas aeruginosa;
- Staphylococcus aureus or epidermal Staphylococcus;
- Escherichia coli;
- Neisseria;
- Listeria.
In addition, among bacterial pathogens, pathogenic Mycobacterium tuberculosis can be especially noted. It penetrates into the tissues of the meninges from lesions in the lungs or other organs. Meningitis of this etiology has a particularly severe course and is quite difficult to treat.
A bacterial or viral infection enters the body against the background of suppressed immune activity. This condition is provoked by risk factors, among which are constant inflammatory processes in the body, hypothermia, and poor nutrition.
The disease is especially severe in elderly patients, as well as in childhood and adolescence.
Key Facts
Meningitis is caused by a variety of microorganisms, including bacteria, fungi and viruses. Meningococcal meningitis is a bacterial form of meningitis, a serious infection that affects the lining of the brain. It can cause severe brain damage and, if left untreated, is fatal in 50% of cases.
The bacterium Neisseria meningitidis, which causes meningococcal meningitis, is especially dangerous due to its ability to provoke large-scale epidemics. Twelve serogroups of N. meningitidis have been identified, 6 of which (A, B, C, W, X and Y) can cause epidemics.
The incidence of meningococcal meningitis varies from sporadic cases and small clusters to large epidemics worldwide, with seasonal variations. Anyone of any age can get the disease, but the disease mainly affects infants, preschool children and young adults.
Methods of infection
The spread of the main pathogens of the disease occurs through an aerogenic mechanism, by airborne droplets. Only sick people or bacteria carriers can be a carrier and distributor of pathology. A patient with meningitis has a cough that releases microparticles of sputum into the air. If there is an uninfected person nearby, then these elements containing meningococcus or other bacteria may enter his respiratory tract.
Despite this mechanism of infection transmission, the risk of infection with meningococcus is quite low. The microorganism is perceived only at close range in case of prolonged or even constant contact. This is especially true when staying in crowded places. Therefore, patients infected with the bacterium must be isolated from other people.
Treatment
Meningococcal disease is potentially fatal and should always be treated as a medical emergency. The patient must be admitted to a hospital or health center, but does not need to be isolated. Appropriate antibiotic treatment should be started as early as possible, ideally immediately after a lumbar puncture if such a puncture can be performed immediately. If treatment is started before CSF testing, growing bacteria from the CSF and confirming the diagnosis may be difficult. However, the need to confirm the diagnosis should not be a reason for delaying treatment.
The infection can be treated with a range of antibiotics, including penicillin, ampicillin and ceftriaxone. In epidemic settings in areas of Africa with weak health infrastructure and limited resources, ceftriaxone is the drug of choice.
How to treat?
The main method of treating bacterial meningitis is etiotropic therapy with antibacterial drugs. To relieve the symptoms of inflammation and suppress the proliferation of microorganisms, massive and long-term treatment with antibiotics is required. If the patient has a viral disease, then antiviral drugs are prescribed.
In addition to etiotropic therapy aimed at eliminating the cause of the disease, the patient is prescribed pathogenetic and symptomatic treatment aimed at improving the general condition of the person. For this purpose the following are used:
- Detoxification solutions - drugs that relieve symptoms of intoxication and help reduce temperature;
- Steroidal anti-inflammatory drugs and diuretics are medications needed to prevent cerebral edema;
- Anticonvulsant therapy - drugs that stop tonic-clonic muscle contractions.
According to indications, the regimen is supplemented with other means necessary for the prevention and treatment of complications.
Amoxiclav
Amoxiclav is an antibiotic, a combination drug. It contains amoxicillin and clavulanic acid.
Amoxicillin belongs to the group of penicillins, has a wide spectrum of action, and provides the main antibacterial effect. This medicine not only inhibits the growth and reproduction of bacteria, but also destroys them in a certain concentration.
Clavulanic acid also has some antibacterial effect, but it is weakly expressed. The main purpose of this component is to protect amoxicillin from destruction by bacterial enzymes (penicillinase).
Amoxiclav is a powerful remedy against gram-positive and gram-negative microbes, but it does not have an antiviral effect. Also, the medicine is not able to destroy fungi and intracellular parasites. Why is Amoxiclav prescribed for the flu?
As a rule, doctors pursue the following goals:
- Prevention of secondary infection.
- Treatment of developed bacterial complications - bronchitis or pneumonia.
Antibiotics for meningitis
Antibiotics form the basis of therapeutic treatment for meningitis. They should be prescribed as early as possible - immediately after a preliminary diagnosis has been established. Before using antimicrobial agents, it is necessary to take blood and cerebrospinal fluid for bacteriological analysis. This study allows you to determine the exact causative agent of the disease and select the optimal drugs for its treatment.
Despite the high information content of bacterial culture, the time frame for its implementation is quite long - the results of the study will be ready in a few weeks. Therefore, initially, antibacterial therapy is prescribed empirically - based on the assumption of the possible nature of the pathogen. The selection is made based on the prevalence of certain microorganisms in the region, as well as the characteristics of the clinical picture and the patient’s condition.
The most effective medications for treating meningitis are:
- Penicillins - amoxicillin, amoxiclav, oxacillin, ampicillin;
- Carbapenems – imipenem, meropenem;
- Vancomycin and its analogues;
- Aminoglycosides – amikacin, tobramycin;
- Fluoroquinolones – levofloxacin, ciprofloxacin, moxifloxacin.
Diagnostics
The initial diagnosis of meningococcal meningitis can be made by clinical examination followed by a spinal tap to identify purulent cerebrospinal fluid. Sometimes bacteria can be seen when cerebrospinal fluid is examined under a microscope. The diagnosis is supported or confirmed by growing bacteria from cerebrospinal fluid or blood samples based on an agglutination test or polymerase chain reaction (PCR). To determine infection control measures, it is important to identify serogroups and perform antibiotic susceptibility testing.
Preventive measures
To prevent bacterial meningitis, specific and nonspecific prophylaxis are used. Specific measures include vaccination against pneumococcus and meningococcus. It is carried out at an early age if the child has a high risk of developing an infectious process.
The spectrum of specific effects includes post-exposure chemoprophylaxis - the use of antibacterial drugs after contact with a patient suffering from meningitis. It involves a single administration of ceftriaxone (250 mg) or ciprofloxacin (500-750 mg). Prevention is recommended for those patients who spent a long time in the same room with an infected person - in boarding schools, barracks, hospitals.
Measures for nonspecific prevention of meningitis include:
- Timely treatment of colds and viral pathologies;
- Prevention of hypothermia;
- Normal nutritious nutrition with sufficient intake of vitamins and essential minerals;
- Adequate physical activity;
- Use a mask in case of contact with sick people.
The listed activities help maintain normal immune activity. Thanks to the good functioning of the body's defense system, the risk of developing an infectious process is reduced.
Thus, meningitis is an acute disease that requires massive antibacterial therapy.
Treatment of meningitis is quite a complex task, so it is carried out exclusively under the supervision of specialists in a hospital setting.
source
Causes
Meningitis develops when pathogenic microorganisms penetrate the soft membranes of the brain. They cause inflammation and suppuration of soft tissues. Depending on the nature of the course, there are 2 types of meningitis in adults:
- Primary is an independent disease. Meningitis infection develops when harmful organisms enter the mucous membrane of the nasopharynx or bronchi.
- Secondary. Pathogenic agents enter the brain through the bloodstream from another source of inflammation. Secondary causes of meningitis in adults are sinusitis, otitis media, and pneumonia.
The following factors can provoke the development of the disease:
- boils on the face or neck;
- head injuries;
- brain surgery;
- tick bites;
- chronic diseases;
- Iron-deficiency anemia;
- diabetes;
- oncological diseases.
Pathogens
The following microorganisms can cause the appearance of unpleasant symptoms of the disease:
- Bacteria – pneumococcus, group B streptococcus, meningococcus, tuberculosis, Escherichia coli and Haemophilus influenzae, listeria.
- Fungi - candida, cryptococcus.
- Viruses – enterovirus, herpes simplex, measles and rubella viruses, cytomegalovirus.
- Other organisms are the causative agents of syphilis and Lyme disease, Leptospira, Toxoplasma, and Plasmodium falciparum.
Routes of infection
There are 3 ways of contracting meningitis:
- Airborne. Infectious agents enter the body of a healthy person when communicating with a sick person - when talking, sneezing, coughing. Viral and meningococcal meningitis are most often transmitted this way.
- Hematogenous. The infection enters the blood during a blood transfusion, through the placenta from mother to child. This is characteristic of secondary forms of the disease and causes purulent meningitis in adults.
- Fecal-oral – through unwashed hands, dirty vegetables and fruits, unboiled water.
- Transmissible. The infection enters the body after an insect bite.
Signs
The incubation period of infection is up to 10 days. Signs of meningitis do not differ between women and men. In patients with good immunity, the disease occurs in the form of nasopharyngitis and is accompanied by signs of a mild cold.
Specific signs of inflammation of the meninges are:
- Muscle stiffness. When you try to bend your head from a lying position, your upper body rises.
- Unnatural posture in sleep. The patient is forced to lie with his torso arched, his head thrown back, his arms and legs pulled up to his stomach.
- Kernig's sign. The patient cannot straighten the leg, which the doctor bent at the hip and knee joints.
- Brudzinski's sign. When palpating the symphysis pubis, spontaneous flexion of the legs at the knees and hips occurs.
- Acute pain when pressing on closed eyelids , the anterior wall of the ear canal, or when tapping the skull.
Initial symptoms
During the first week of illness, an adult develops the following signs of meningitis:
- headache in the occipital and frontal lobes;
- chills, slight increase in body temperature to 37.5–38 ° C;
- pale skin;
- lack of appetite;
- dry cough;
- runny nose;
- throat congestion;
- weakness in the body;
- swelling of the nasal mucosa and larynx.
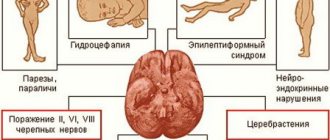
Signs of complications
As the infection progresses, symptoms in adults become more intense and are supplemented by the following manifestations:
- severe headaches that do not go away even when taking antispasmodics;
- inflammation of the mucous membrane of the eyes;
- increase in body temperature to 39–40° C;
- nausea and vomiting;
- photophobia;
- hallucinations, outbursts of anger;
- abdominal pain;
- double vision;
- a skin rash that does not go away with pressure;
- drowsiness, lethargy.
Medicines for meningitis
For meningitis infection, antibiotics are prescribed. They suppress the growth of bacterial flora and relieve inflammation of the meninges.
For purulent meningitis, the treatment period increases to 20–30 days. To relieve symptoms and alleviate the condition, adults are prescribed the following medications:
- Analgesics – relieve pain and have a moderate antipyretic effect.
- Diuretics – remove excess fluid from the body, relieve brain swelling.
- Antipyretics – used to reduce body temperature.
- Droppers with glucose solution and vitamins are prescribed to replenish the water-alkaline balance and maintain the body.
- Antifungal and antiviral agents - help speed up recovery and prevent the proliferation of viruses and fungi.
Antibiotics
At the initial stage of treatment, adults are prescribed Penicillin and Ampicillin in high dosages. Injections are performed intramuscularly every 4 hours.
This helps to quickly relieve inflammation and prevent complications. If penicillin antibiotics do not help, adults are prescribed the following drugs:
- Cefuroxime;
- Ceftazidime;
- Ceftriaxone;
- Meropenem;
- Abaktal;
- Ofloxacin;
- Ciprofloxacin;
- Amikacin.
Antifungal
This is a group of drugs that is prescribed as an adjuvant treatment for meningitis caused by candida and mycoses. Antifungal agents prevent spore division and eliminate the cause of the disease. The following medications are prescribed for adults:
- Fluconazole;
- Amphotericin;
- Mikosist.
Antiviral
With the help of these drugs, it is possible to slow down the process of interaction of viruses with brain cells at different stages of the disease. Antiviral drugs help improve immunity and eliminate headaches, weakness, nausea, and runny nose. For adults with meningitis, the following medications are prescribed:
- Acyclovir;
- Zovirax;
- Ribavirin;
- Abacavir.
Antipyretics
This group of medications helps normalize body temperature and eliminate some of the unpleasant symptoms. At the initial stages of treatment, antipyretic tablets are used, and injections are used for chills and fever. The following medications are prescribed for adults:
- Paracetamol;
- Panadol;
- Analgin;
- Drotaverine;
- Diclofenac;
- Ibuklin.
Painkillers
The drugs help get rid of headaches, muscle spasms and improve the course of the disease. Painkillers are prescribed in short courses. The following drugs are used in the treatment of meningitis in adults:
- Ibuprofen;
- Nurofen;
- Aspirin;
- Analgin;
- Ketanov.
Hormonal
Medicines in this group normalize the functioning of the endocrine system, suppress the body’s allergic reaction and quickly relieve inflammation. Hormonal medications are taken in short courses of 5–10 days. The following medications are used to treat meningitis in adults:
- Prednisolone;
- Dexazone;
- Advantan;
- Metipred.
Prevention
Meningitis infection is dangerous with serious consequences. To prevent the development of the disease, preventive measures are taken. The mainstay of protection against meningitis is vaccination. Vaccinations can be of several types:
- Meningococcal vaccine. It is administered to children 10–12 years old, students, soldiers, and tourists when traveling abroad.
- Vaccination against Haemophilus influenzae type B. Prescribed for children from 2 months to 5 years.
- Pneumococcal vaccination. Indicated for children under 5 years of age and adults over 50 years of age.
- Injections against measles, rubella, mumps, chickenpox.
To avoid illness, follow these rules:
- visit your doctor regularly;
- use individual household items;
- eat a balanced diet;
- wash your hands before eating;
- do not eat dirty vegetables, do not drink water from public sources;
- vaccinate;
- lead an active lifestyle;
- When outdoors, wear a hat, closed clothing, and use insect repellent sprays.