Meningitis is an infectious disease in which an inflammatory process develops in the membranes of the brain. Infectious agents are transmitted from a sick person or carrier of microorganisms to a healthy person through contact or airborne droplets. Sometimes people become infected by eating food that is contaminated with animal excrement, water contaminated with microorganisms, or the bite of various insects.
The first signs of meningitis do not appear immediately after the patient becomes infected. The period of time between the entry of an infectious agent into the body and the appearance of the first symptoms of the disease is called the incubation period. For infectious meningitis, it varies from 4 to 10 days. Doctors at the Yusupov Hospital establish a diagnosis of meningitis using modern laboratory and instrumental studies.
Immediately after an accurate diagnosis is established, complex therapy begins. Infectious disease specialists prescribe the most effective antibacterial and antiviral drugs that quickly destroy pathogens. Detoxification therapy is carried out using modern infusion agents. To treat patients, drugs registered in the Russian Federation are used, which have a minimal range of side effects.
What is meningococcal meningitis?
Meningococcal meningitis is a form of meningitis caused by a specific bacterium known as Neisseria meningitidis. Meningitis is characterized by inflammation of the membranes around the brain or spinal cord. This inflammation may begin suddenly (acute) or develop gradually (subacute).
Symptoms may include fever, headache and a stiff neck, sometimes with aching muscles. Nausea, vomiting and other symptoms may also occur. Skin rashes occur in about half of all people with meningococcal meningitis. Meningococcal meningitis continues to be associated with high mortality rates and persistent neurological impairment, especially among infants and young children. Meningococcal infection is fatal without antibiotic therapy.
Signs and symptoms
Meningococcal meningitis is one of the three most common types of bacterial meningitis. The incubation period averages 3-4 days (range 1-10 days), which is the period of sociability. It progresses faster than any acute form of bacterial meningitis. Meningococcal meningitis affects the central nervous system. In adults and children, this is often preceded by a respiratory illness or sore throat. In its acute form, the disorder is characterized by fever, headache, neck stiffness, nausea, vomiting, and altered mental status such as confusion or coma. Adults can become seriously ill within a few hours. In children, the course of infection may be even shorter.
Meningococcal meningitis develops when the bacteria Neisseria meningitidis (N.meningitidis) progresses from initially attaching to the mucous membrane of the nasopharynx (nose and throat) to penetrating into the deeper layers of the mucosa (submucosa). These bacteria multiply quickly and can lead to a mild (subclinical) infection. However, in approximately 10-20% of cases, N. meningitidis enters the bloodstream, causing meningococcemia. This systemic form of the disease, meningococcemia, usually precedes the development of meningococcal meningitis by 24-48 hours.
Meningococcemia is characterized by severe, widespread vascular damage, with evidence of circulatory compromise and disseminated intravascular coagulation (DIC). Skin rash occurs in about half of all people with meningococcal meningitis. The rash is petechial (tiny, non-raised, purplish-reddish lesions that do not blanche with pressure and result from intravascular bleeding).
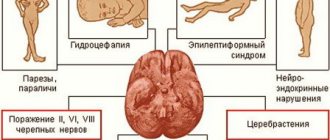
Swelling or inflammation of the brain (cerebral edema or ventriculitis) or hydrocephalus (a buildup of fluid in the brain cavity) may also occur. Additional symptoms may include:
- chills;
- increased sweating;
- weakness;
- loss of appetite;
- muscle pain (myalgia) in the lower back or legs;
- inability to tolerate bright light (photophobia).
Dehydration is common in people with meningococcal meningitis. In some cases, collapse of blood vessels can lead to shock (Waterhouse-Friedrichsen syndrome) when meningococcal bacteria spread in the blood (septicemia). Later symptoms may include paralysis on one side of the body (hemiparesis), hearing loss, or additional neurological damage.
Disease prevention measures
Prevention of the disease can be specific and nonspecific. As for the first, it is advisable only in the case of bacterial forms of the disease. Today, immunobiological drugs have been created for the prevention of meningococcal, hemophilic and pneumococcal meningitis.
Nonspecific prevention measures are important for combating viral meningitis. Today there are no other ways to prevent this form of the disease. Viral meningitis in children is prevented by maintaining personal hygiene.
Non-specific events
This kind of prevention is aimed at increasing protective forces and preventing contact with infected people. Hardening increases the body's resistance to the negative effects of external factors. It is better to start with dousing with cool water (+30 °C), gradually lowering the temperature to the lower limit - +10 °C. Remember, when scheduling procedures, it is important to take into account the individual characteristics of the body.
A balanced diet is an important condition for the prevention of meningitis. Active resistance of the body to bacteria and viruses is impossible without a sufficient supply of fats, proteins, carbohydrates and vitamins. In order to prevent the inflammatory process, it is necessary to include in the diet:
Plant and animal protein
Antibodies synthesized from proteins help the body resist infections.
Increases the body's endurance and supplies it with polyunsaturated fatty acids.
Complex carbohydrates, fiber
Provides the body with B vitamins.
They are natural antioxidants.
Natural immune stimulant.
Helps increase the number of immunocompetent cells.
Activates the synthesis of T-lymphocytes.
Ensure normal functioning of the circulatory system.
Magnesium, calcium, potassium
Necessary for strengthening the immune system.
Medicinal methods of preventing meningitis are also actively used. Taking adaptogens helps increase the body's nonspecific resistance to a wide range of harmful effects of a chemical, physical and biological nature. In addition, for the purpose of prevention, it is advisable to:
- use intranasal ointments during the off-season;
- take vitamin D;
- undergo a course of immunomodulatory therapy.
Maintaining good hygiene is an integral part of preventing viral meningitis.
Vegetables and fruits must be doused with boiling water before eating. Hands must be washed with soap before eating. You cannot use someone else’s personal hygiene products (towel, toothbrush).
Prevention of meningitis in contact with a sick person
Vaccination with polysaccharide or conjugated antigens helps prevent bacterial damage to the meninges. The first is used for vaccinating adults and older children. The immune system of a child under two years of age does not recognize polysaccharide antigens, which limits its use in young children. The conjugated antigen is recognized by the baby's immune system. The following vaccines are registered in Russia:
Against meningococcal infection
Against hemophilus influenzae
Against pneumococcal infection
Causes and risk factors
Meningococcal meningitis is caused by a bacterium known as Neisseria meningitidis. There are several types or serogroups of Neisseria meningitidis. The most common of these serogroups are A, B, C, D, X, Y, 29E and W135. Serogroups A, B, C and Y are responsible for the majority of meningococcal diseases.
The bacterium is spread through airborne transmission (i.e. droplets in the air) or through close contact with an infected person. It collects in the nasopharynx or postnasal space, connecting the nasal cavities with the throat. The bacterium is transported by the blood to the membranes around the brain (meninges) or spinal cord. It usually spreads from nearby infected areas such as the sinuses or from the cerebrospinal fluid.
Diagnostics
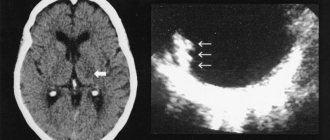
If meningitis is suspected, a spinal tap is first performed to make a diagnosis. Based on the nature of the released liquid, a preliminary conclusion is made. In a viral disease, the cerebrospinal fluid is clear and comes out under pressure. The meningococcal type of disease will produce discharge without pressure, whitish in color. Laboratory testing of the liquid is carried out to identify the pathogen.
At the same time, other types of diagnostics are carried out:
- examination of the cerebrospinal fluid regarding the presence of protein and glucose;
- general blood test, blood culture for sterility;
- to assess the functions of the urinary tract and kidneys - urine analysis;
- magnetic resonance and computed tomography;
- X-ray (if necessary) of the lungs and ENT organs;
- biopsy of the rash material to exclude skin diseases.
If there is a suspicion of purulent processes, infection in the cerebrospinal fluid, or characteristic symptoms, patients undergo electroencephalography, an X-ray of the head, and a fundus examination.
Affected Populations
Meningococcal meningitis mainly affects infants, children and young adults. Men are slightly more affected than women and account for 55% of all cases, with an incidence of 1.2 cases per 100,000 population, compared with 1 case per 100,000 population among women. Meningococcal meningitis can occur as an epidemic in subgroups, such as people in military service or students in dormitories. Vaccines can help control epidemics of meningitis caused by serogroups A, B, C, Y or W135.
The age-specific incidence of meningococcal disease is highest in young children, although the incidence of meningococcal disease in adolescents and college-age young adults appears to have increased. College students living in residence halls appear to be at higher risk. This occurs due to the close proximity of students in college dorms, which allows the infection to spread faster.
Diagnosis of meningococcal infection using general clinical research methods
- Meningococcal nasopharyngitis occurs with slight leukocytosis and normal or slightly increased ESR. When diagnosing meningococcal nasopharyngitis, epidemiological and bacteriological examination data are used. It is extremely difficult to diagnose this disease based on clinical data alone.
- Generalized forms of the disease occur with pronounced neutrophilic leukocytosis and a significant shift in the formula, eosinophils disappear from the peripheral blood, and ESR increases.
- The toxic form of meningococcemia occurs with thrombocytopenia and slight anemia. An increased hematocrit level indicates blood thickening in the vascular bed. Developed leukopenia indicates an increase in severe intoxication and is a poor prognostic sign. The platelet level in the blood drops and the coagulogram changes. Signs of metabolic acidosis and disturbances in the electrolyte composition of the blood appear.
- The appearance of traces of protein, casts and single red blood cells in the urine indicates toxic damage to the kidneys. A significant increase in protein, granular casts and red blood cells indicates the development of acute renal failure.
With the mass death of meningococci, endotoxins are released, the impact of which on the internal organs and systems of the body determines the clinical picture of the disease, the severity of which dictates the use of a certain amount of research.
Rice. 2. The photo shows meningococcemia in children.
Disorders with similar symptoms
Symptoms of the following disorders may resemble those of meningococcal meningitis. Comparisons can be useful for differential diagnosis:
- In general, meningitis is characterized by inflammation of the membranes around the brain or spinal cord. This inflammation can be caused by various types of bacteria, viruses, fungi, cancer, or reactions to certain injections into the spinal canal.
- Encephalitis is an infection of the brain. There are different types of this disorder, caused by different types of viruses. Encephalitis can also be caused by hypersensitivity caused by a virus or proteins foreign to the body. Symptoms may include headache, drowsiness, hyperactivity and/or general weakness. This disorder may have some symptoms similar to those of meningitis, such as a stiff neck, altered reflexes, confusion, speech problems, seizures, paralysis, and coma.
- Rocky Mountain spotted fever is an acute infectious disease transmitted to humans through the bite of an infected tick, usually in wooded areas of the midwestern, eastern, and southeastern United States. Fever and rash are some of the main symptoms. Not all cases may develop a rash, which can make diagnosis difficult. Swelling, headaches, chills, weakness and muscle pain may also occur. Severe headaches, lethargy, confusion, delirium, focal neurological deficits, increased pressure in the skull leading to compression and swelling of the optic disc, epilepsy and/or coma may occur in untreated cases as damage to the nervous system progresses. Some people may have a stiff neck due to muscle pain (myalgia) or irritation of the membranes surrounding the tissues of the brain and spinal cord (meningismus).
What are the predisposing factors and how to influence them?
The development of meningitis is due to a complex of reasons, including the high virulence of the pathogen, on the one hand, and reduced human immunity, on the other. The body's ability to protect against infections is reduced by overload at work, emotional stress, and exposure to physical factors (overheating, cooling, insolation). Consequently, just by harmoniously organizing the work-rest regime, it is already possible to reduce the risk of developing infectious diseases, including meningitis.
There are so-called risk groups for the incidence of meningitis
In some cases, such as the presence of concomitant pathology or chronic infectious processes in the body, the occurrence of viral or bacterial meningitis is more likely.
Factors determining risk groups:
- suffered traumatic brain injuries;
- history of neurosurgical interventions, including cerebrospinal fluid shunting;
- chronic sinusitis (frontal sinusitis, sinusitis);
- chronic purulent diseases of the chest organs:
- chronic pleural empyema,
- chronic purulent bronchitis,
- septic endocarditis and others;
- diseases of the blood system:
- Iron-deficiency anemia,
- B12 deficiency anemia;
- agammaglobulinemia,
- leukemia;
- diabetes;
- immunodeficiencies (congenital and acquired, including those provoked by taking immunosuppressive drugs);
- oncological diseases (lymphomas, brain tumors, etc.).
Of course, you cannot influence the presence of previous injuries and operations, but many chronic diseases can be cured. Regular visits to the doctor and strict adherence to his instructions will reduce the frequency of exacerbations of chronic diseases and increase the duration of periods of remission. This means that the body will be full of strength to produce an adequate immunological response in time to exposure to bacteria or viruses that can cause meningitis.
Prevention
Meningococcal vaccines protect against certain types (called serogroups) of meningococci that cause most meningococcal diseases: serogroups A, B, C, W and Y.
There are two types of proven vaccines against meningococcus:
- MenACWY Vaccine: This vaccine protects against meningococcal serogroups A, C, W, and Y. It can be given to children as young as 2 months.
- MenB vaccine: This vaccine protects against meningococcal serogroup B. It can be given to people 10 years of age and older.
Clinicians may also consider vaccinating all healthy adolescents and young adults aged 16–23 years with the MenB vaccine, preferably between ages 16–18 years, to provide short-term protection at ages when the risk of serogroup B infection is highest.
Children and adults who are at increased risk of getting meningococcal disease (including those who travel to countries in the meningitis belt) may receive one or both vaccines, depending on how old they are, what risk factors they have, and which meningococcal vaccines they take. already received.
MenACWY vaccine is recommended for the following:
- people living in an area where an epidemic may occur, including serogroups A, C, W or Y (for its control);
- conscripts;
- first-year students living in a residential building;
- tourists traveling to places where such infections are common, such as tropical Africa during the dry season from December to June and Saudi Arabia before visiting the Hajj;
- people who work with meningococcal bacteria in laboratories or in industry;
- children aged 2 months and older with certain immune system disorders;
- people whose spleen has been removed or damaged (for example, people with sickle cell disease);
- people who take eculizumab;
- HIV-infected.
Application of PCR for the diagnosis of meningococcal infection
Diagnosis of whooping cough using PCR (polymerase chain reaction) is the most promising technique in modern conditions. The high sensitivity of the test makes it possible to detect the DNA of bacteria, even if there are several dozen or even a few of them in the material under study. This method is highly specific. Its special value lies in the fact that the detection of meningococci in biological material becomes possible when other research methods give a negative result.
Rice. 8. The PCR technique is highly specific and allows you to detect the DNA of bacteria, even if there are several dozen or even a few of them in the material under study.
Standard Treatments
Until the results of a bacteriological study identifying the causative agent of the infection are obtained, the patient is usually placed in the intensive care unit and intravenous administration of antibiotics and fluids is started as soon as possible. If meningococcal infections are confirmed, antibiotics are replaced with the most effective drugs against these bacteria - usually ceftriaxone or intravenous penicillin.
Children and adults with meningitis may be given corticosteroids (such as dexamethasone). These drugs help prevent brain damage.
Drug therapy
The meningococcal inflammatory process does not tolerate delay; urgent hospitalization is necessary. The earlier treatment is started, the greater the chance of saving the patient's life. The main medicine is broad-spectrum antibiotics. You need to act immediately, and it takes some time to detect the pathogen and establish sensitivity.
The drugs are prescribed for at least ten days; if necessary, the course of therapy is extended for another week. Penicillin is used for treatment, as it copes well with the main pathogens of meningitis: staphylococcus, meningococcus, streptococcus, pneumococcus. Loading doses of the drug are used (300,000 units per kilogram of body weight per day) every four hours. If the pathogen is insensitive to penicillin, cephalosporin antibiotics are prescribed.
Meningitis of viral origin is treated symptomatically in accordance with the patient's condition. Antipyretic, painkillers, and anticonvulsants are used. Antiviral agents are widely used. Meningitis is a complex and dangerous disease; self-medication is unacceptable; consultation with a specialist is required.
Forecast
Before the introduction of sulfonamide drugs and penicillin into therapy, 30-70% of patients with meningococcal meningitis died. Survivors often had a decrease in intelligence, developed dropsy of the brain, deafness, blindness, persistent paralysis and epileptic seizures or necrosis, leading to amputation of limbs. With the introduction of sulfonamide drugs, mortality decreased to 8-28%. Mortality rate decreased even more thanks to the use of penicillin.
Currently, if treatment is started early, the prognosis is favorable. But despite this, meningococcal meningitis is even now one of the common causes of death from infectious diseases. The high mortality rate persists, despite the success of antibiotic treatment, due to the fact that in many cases the rapid progression of the disease is limited by the possibility of therapeutic intervention, and most of the deceased patients do not actually have time to receive treatment. From here it is clear that the main way to further reduce mortality from meningococcal infection lies in organizational and methodological measures.
Nonspecific prevention in adults and children
Simple measures to prevent meningitis
Issues of nonspecific prevention are especially relevant for viral meningitis, since today there are no other ways to prevent the development of an infectious process of viral etiology. Prevention of fungal meningitis can also be carried out only by nonspecific methods.
The main means of nonspecific prevention of any infectious diseases is a healthy lifestyle, which all family members should follow. This concept includes a balanced sleep and wakefulness regime, physical exercise, such as yoga or swimming, and restorative procedures (hardening, contrast shower). Strengthening the immune system, which is so important in the prevention of all types of meningitis, is impossible without a healthy diet, complete in minerals and vitamins.
As mentioned above, observation by a local physician (pediatrician) and specialists in the presence of various chronic diseases is an important component of a set of preventive measures aimed at preventing the development of infection of the meninges. Timely seeking medical help if an infectious disease is suspected will ensure that the diagnosis is made on time and treatment is carried out correctly, which will reduce the risk of complications, including meningitis.