Basic rhythms of BEA brain
Bioelectrical activity is electrical vibrations. There is a huge network of neurons in the brain that operate on a specific wavelength. Waves are recorded on the electroencephalogram (EEG), and deciphering the graph helps doctors judge the state of a person’s biopotentials and psyche.
Biowaves, the so-called rhythms of brain activity, are divided by amplitude and frequency:
- alpha – 8-13 Hz (frequency), 5-100 µV (amplitude);
- beta – 14-40 Hz, up to 20 µV;
- gamma – more than 30 Hz (rarely up to 100 Hz), not higher than 15 μV;
- delta – 1-4 Hertz, 20-200 µV.
There are other types of biorhythmics, but medicine has not yet studied them enough.
Diffuse disturbances of bioelectrical activity
Normal bioelectrical activity is subject to changes due to trauma and organic diseases.
Dysrhythmic disruptions can be localized, that is, concentrated in a certain area of the brain (front, back, left or right). Or they can be diffuse, that is, spread throughout the brain, without a clear location, and disrupt the passage of electrical impulses due to increased ascending activating influences.
Depending on the symptoms and a number of specific EEG indicators, several types of BEA changes are distinguished.
Light (moderate) and pronounced
They do not cause any harm to the patient, at least not immediately. But the functions of the body and the mechanism of operation of the brain stem structures are already disrupted. Soon, if no steps are taken, these changes will develop into serious disruptions in the body.
If the BEA is somewhat disorganized, disturbances in the electrical activity of the main brain structures are observed, this means damage to the hypothalamus or thalamus. Such conditions cause disruptions in the nervous system, thyroid and pancreas.
Moderate and pronounced changes in BEA, manifested in the form of a slowdown in the frequency of background activity, are indicated by the onset of seizures. A person may experience convulsions that were not previously bothersome. Another symptom is blood pressure jumping for no reason.
Seizures are an alarming sign that can lead to the development of epilepsy.
Irritative
The term “irritation” refers to a large amount of brain damage. Irritative disorders manifest themselves in dysfunctions in the perception of one’s own body, speech, etc.
If the hypothalamus is affected, irritation of diencephalic structures is observed, and the mental phenomenon of depersonalization occurs - a feeling when one’s own body and one’s own “I” become alien.
Mild irritative disorders are characterized by a deterioration in general well-being and sudden changes in mood.
Changes in the cortex
When the fields of the cerebral cortex are damaged, disorders of consciousness and behavior occur. This area controls higher nervous activity. Sometimes one zone is damaged, in other cases several.
- if the occipital zone has undergone changes, this manifests itself as hallucinations;
- central gyrus - twitching of the arms or legs begins, developing into attacks of epilepsy;
- posterior central gyrus – a feeling of numbness and tingling occurs in the body;
- the adversive field is damaged – convulsive syndrome with loss of consciousness is observed.
During the study, it is not always possible to determine the localization of changes in the cortex and the level of disturbances. For example, EEG shows only rhythm deviations and diffuse changes in bioelectrical activity.
Damage to the cortex is also indicated by dysfunction of vision or hearing, olfactory hallucinations, attacks of twitching of different parts of the body, head due to a significant decrease in the convulsive threshold.
Etiology
There can be a large number of reasons for the development of symptoms of diencephalic syndrome.
Factors that have a negative impact on the functioning of the pituitary gland and hypothalamus:
- closed TBI,
- vascular diseases, in which the speed of blood flow decreases and brain hypoxia develops,
- degenerative-dystrophic processes in the cervical spine,
- stressful and conflict situations, psychological trauma, shock, excessive psycho-emotional stress,
- neoplasms in the brain - glioma, meningioma, craniopharyngioma,
- chronic intoxication with alcohol, drugs, nicotine,
- occupational hazards - gas pollution, dust, chemicals, toxins, volatile compounds,
- influence of environmentally harmful components,
- prolonged oxygen deprivation, as in suffocation or drowning,
- infection from chronic foci - caries, tonsillitis, sinusitis,
- viral and bacterial infections - influenza, malaria,
- pregnancy,
- hormonal disbalance,
- large blood loss,
- chronic somatic diseases - hypertension, peptic ulcer, bronchial asthma,
- birth trauma in children, intrauterine hypoxia and fetal malnutrition, pathology of the second half of pregnancy, FPN.
The main pathogenicity factor in the syndrome is increased vascular permeability. It ensures the penetration of microbes and their toxins circulating in the blood into the brain tissue. Patients develop meningoencephalitis or cystic arachnoiditis. The consequence of injuries and infections is often hydrocele of the brain, squeezing the hypothalamus from all sides. In addition to organic damage to the hypothalamic region by neoplasm or inflammation, a functional disorder of the organ due to endocrinopathies or mental trauma is possible.
The clinical signs of the disease are very diverse and diverse. They occur immediately after exposure to an etiopathogenetic factor or after some time. The polymorphism of symptoms is explained by the huge number of functions performed by the structures of the hypothalamic-pituitary region. First of all, patients have impaired thermoregulation, the functioning of vital organs and endocrine glands, water-electrolyte, lipid and protein metabolism.
Manifestations of pathology:
- Neuroendocrine syndrome is the basis of this disease and is manifested by symptoms of adiposogenital dystrophy, diabetes insipidus, sexual dysfunction, Itsenko-Cushing's disease, acromegaly, bulimia, anorexia, pituitary dwarfism, hypothalamic obesity. Patients complain of headache, insomnia, hysteria, nervousness, impotence and menstrual irregularities. Endocrine disorders are usually manifested by obesity, early puberty, excessive sexual desire or decreased libido, and heterosexuality.
- The neuromuscular form is manifested by dysfunction of the muscular system such as various myopathies, paroxysmal paralysis of an intermittent nature, and physical asthenia.
- Thermoregulation disorder is manifested by a change in body temperature - its increase to subfebrile levels and a sharp decrease, a state of chills, and muscle tremors.
- Vegetative-vascular manifestations of the syndrome - hyperhidrosis, dizziness, headache, nausea, cardialgia, rise and fall of blood pressure, rapid heartbeat, suffocation, mood swings from apathy to anger, decreased performance, insomnia, muscle weakness and hypotension, unstable gastrointestinal tract activity, pain in the solar plexus, emotional disorders. Vegetative-vascular crises are characteristic of this form of pathology. For some, they happen once every 2-3 months, while for others, several times a day.
- Neurodystrophic syndrome with impaired skin trophism - rash, itching, peeling, erosion, ulcers, swelling, bedsores; gastrointestinal mucosa - erosions and bleeding ulcers; bone tissue – demineralization, osteosclerosis.
- Diencephalic epilepsy is another manifestation of the syndrome, the main symptoms of which can be called convulsions, during which the patient often loses consciousness. These paroxysms clinically resemble attacks of ordinary epilepsy, but have a slightly different cause - dysfunction of the hypothalamus. Immediately before the attack, patients' mood changes, hunger and thirst, unreasonable fear, fever with chills, polyuria and profuse bowel movements appear. The attack ends with convulsions and fainting.
- Signs of salt metabolism disorders are: muscle ossification and interstitial edema.
- Psychasthenic and neurotic syndromes are caused by weakness of the cerebral cortex and hypothalamus and manifest themselves with symptoms characteristic of neuroses and psychoses.
These syndromes can occur in various combinations and determine the nature of the underlying pathology. But patients with diencephalic syndrome always have thirst, increased or decreased appetite, sleep disturbance, headache, stabbing or aching pain in the chest, palpitations, shortness of breath or suffocation, weight change, anxiety and panic attacks, digestive disorders, decreased mood, constant fatigue .
Classification of diencephalic syndrome:
- primary - caused by neuroinfection or trauma,
- secondary - associated with metabolic disorders.,
- mixed.
The following forms are distinguished according to severity:
- heavy,
- average,
- light.
According to the nature of the process, the syndrome is:
- progressive;
- regressing;
- recurrent.
In children with the syndrome, excitability and physical activity increase. Despite adequate nutrition and increased basal metabolism, patients become extremely exhausted. Autonomic symptoms in children are similar to those in adults. Their skin turns red, sweating, tachycardia and vomiting appear. External signs of pathology are large growth and excessively long limbs, a large head, optic nerve atrophy, nystagmus, and decreased visual acuity.
Diagnosis of diencephalic syndrome begins with the study of patient complaints, clinical signs of pathology and life history. At the same time, data regarding past infectious diseases and TBI deserve special attention. Because the syndrome manifests itself with many different symptoms, it can be difficult to diagnose.
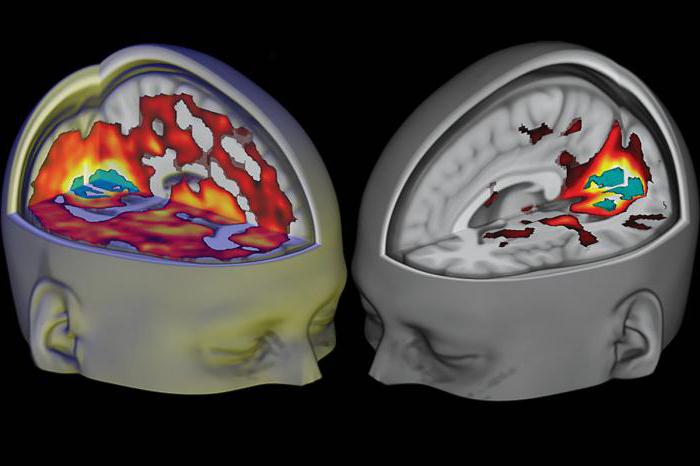
example of a child with a large tumor (astrocytoma) of the diencephalic zone
- Study of the sugar curve - glucose tolerance test: determining the level of glucose in the blood on an empty stomach and then with a load.
- A biochemical blood test can detect signs of metabolic disorders.
- Measuring body temperature in both armpits and rectum. Rectal temperature should be 1 degree higher than armpit temperature. With diencephalic syndrome, hypo- or hyperthermia develops.
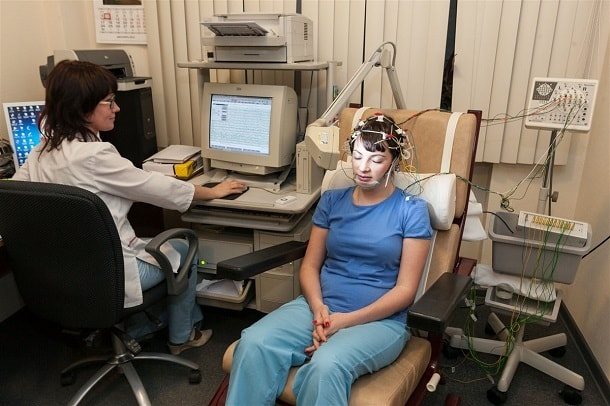
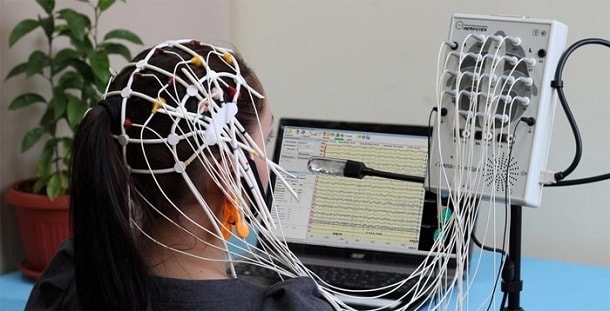
- EEG can detect damage to the deep structures of the brain.
- Urine examination according to Zimnitsky - determination of the basic concentration functional ability of the kidneys.
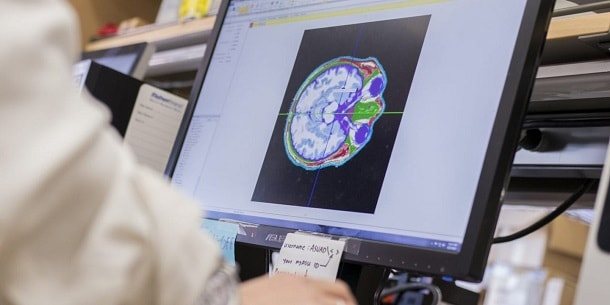
- Nuclear magnetic resonance of the brain - signs of increased intracranial pressure, consequences of injuries, hypoxia, neoplasms.
- Determination of hormone levels in the blood to identify endocrine disorders - LH, prolactin and cortisol.
- Additional techniques - ultrasound, CT or MRI of the adrenal glands, thyroid gland, pelvic organs and uterus.
- Ancillary methods include studies of the fundus, visual fields, radiography of the skull and adrenal glands.
- Dopplerography of cerebral vessels.
Causes of cerebral disorganization
Diffuse changes in BEA do not appear out of nowhere and are not genetically determined. These anomalies are formed due to disruption of certain processes and damage to neural connections. In particular, many diseases lead to disruption of the central nervous system.
Head injury
The intensity of diffuse changes in BEA completely depends on the severity of the injury. Moderate injuries cause discomfort in the patient and do not require long-term therapy.
Severe injuries can cause serious changes in the BEA, leading to severe dysfunction in the central nervous system.
Brain injuries include:
- concussion – occurs after a minor head injury;
- compression - occurs due to hematomas and reduction of intracerebral space in the cranial cavity;
- bruise - damage to the brain due to a blow to the head, often accompanied by hemorrhage;
- intracranial hemorrhage - destruction due to an impact on one of the blood vessels, which leads to local hemorrhage into the cranial cavity.
Inflammations affecting GM substance
Mild changes in BEA can occur due to inflammatory diseases affecting the brain substance.
Meningitis
This is an inflammatory process localized in the meningeal membranes. The main symptom of the pathology is intense headache, accompanied by nausea and repeated vomiting.
The disease is infectious or bacterial in nature, is very dangerous and can be fatal, especially if a child gets sick.
Arachnoiditis
The second name of the pathology is serous meningitis, since it involves serous inflammation of the arachnoid membrane of the brain. Its causes are injuries, intoxication of the body, acute and chronic infections. The disease can develop with slowly growing tumors and encephalitis.
With arachnoiditis, constant headache, nausea, and vomiting occur. Neurological disorders depend on the lesion.
Encephalitis
Encephalitis is a group of pathologies characterized by inflammation of the brain. They arise due to the action of pathogenic bacteria and viruses.
The most common is tick-borne encephalitis, carried by ticks. In addition to it, influenza, rheumatic, epidemic, and Japanese encephalitis are also distinguished.
The disease manifests itself with headaches, high fever and general weakness.
Anemia
This condition is characterized by a low hemoglobin content in the blood and a simultaneous decrease in red blood cells. Anemia is not an independent disease, but a symptom of various pathologies.
With anemia, little oxygen enters the brain, which causes starvation of brain cells (neurons), and as a result, complications in the form of wave dysrhythmia.
Irradiation (poisoning)
Radiological damage does not leave its mark on the body. It undergoes pathological changes, including the brain.
Signs of toxic damage are considered irreversible, can significantly affect the quality of life and a person’s ability to perform daily activities, and require a serious approach to treatment.
Atherosclerosis of cerebral vessels
A disease in which plaque builds up in blood vessels, impairing blood flow. The most common cause of BEA disorganization. At the beginning of the disease they are moderate in nature.
In the process of tissue death due to lack of blood supply, the deterioration of neuronal patency worsens, which is manifested by increased disturbances.
Associated abnormalities
Diffuse changes in BEA can be caused by dysfunctions of the lower part of the brain structure: the pituitary gland and hypothalamus. They can also occur in immunodeficiency states.
In newborns, dystrophic foci in the brain can be a consequence of hypoxic-ischemic lesions, which also manifests itself in a violation of BEA.
What kind of diagnosis is this?
The brain is a huge collection of cells. When pathology occurs in a specific area, it is called localized. When multiple pathological foci of different sizes appear in different areas, they speak of diffuse damage. That is, with this type of disease the entire organ is captured.
The brain, like any human organ, is characterized by certain pathological phenomena. With diffuse changes in the BEA of the brain, we can talk about:
- sclerosis (increasing tissue density);
- malaria (softening and loss of tissue structure);
- inflammatory reaction;
- tumor process.
Diffuse sclerosis
This is the most common pathology presented and is manifested by tissue compaction due to insufficient oxygen supply. The cause may be impaired blood circulation and the development of diseases due to which oxygen is delivered in insufficient quantities.
The most common provoking diseases are:
- hypertension;
- anemia;
- heart muscle failure;
- atherosclerosis of the carotid artery.
The listed pathologies are diagnosed mainly in elderly people; in the absence of timely and adequate treatment, they lead to the occurrence of diffuse sclerosis.
Provocateurs of sclerosis are pathologies not associated with oxygen deficiency: liver and kidney failure. They cause toxic damage to brain tissue, as a result, dead areas become denser or cysts form.
Another factor leading to diffuse sclerosis is improper functioning of the immune system. The myelin sheath, which covers the neuron, acts as a biological insulator. Immune agents attack the insulating layer, causing neurological symptoms. This is how multiple sclerosis develops, diagnosed in young patients.
Encephalomalacia
The brain tissue contains a large amount of fluid. When the cells die, wet necrosis is observed, the main symptom of which is the appearance of softened lesions. When the process affects multiple areas of the brain, they speak of diffuse encephalomalacia. At the final stage, sclerosis occurs or cysts form.
Diffuse softening is provoked by various factors that affect the entire brain. That is, they cannot be injuries and strokes that lead to focal changes. But there may be:
- infections;
- edema;
- suffered clinical death.
During an inflammatory reaction triggered by an infection, the immune system tries to block the spread of the pathogen. The result is the appearance in the inflamed brain of areas of dead tissue containing a purulent mass. Often the process ends in death, but with proper therapy, regeneration of brain structures is possible. Dead neurons are not restored, but their function is taken over by surrounding cells.
Diffuse tumors
A tumor is a pathology of focal type. Therefore, we can talk about diffuse damage only when metastases penetrate the brain.
Metastasis is the movement of malignant cells with lymph and blood. Most often, transfer to brain tissue occurs from the pulmonary system and prostate gland. When the supply of metastases is abundant, they speak of a cerebral extent of damage. Surgical intervention in this case is useless.
Consequences
Diffuse changes in BEA can cause a lot of inconvenience to a person. But if you quickly pay attention to the deterioration of the condition and carry out restorative treatment, the disorganization of the BEA is not critical for health.
Changes left without proper attention are dangerous, as they can cause irreversible complications. Depending on the location of the process, chronic impulse conduction causes motor skills disorders, psycho-emotional disorders, and developmental delays in children.

Serious consequences of BEA disorientation are the development of epilepsy and seizures.
Negative processes cause hardening and softening of brain tissue, inflammation and the production of new cells, which subsequently develop into a tumor. Against this background, a person may develop encephalomalacia, radiculopathy, diffuse sclerosis, oncological pathologies, and cerebral edema.
Diagnosis and treatment
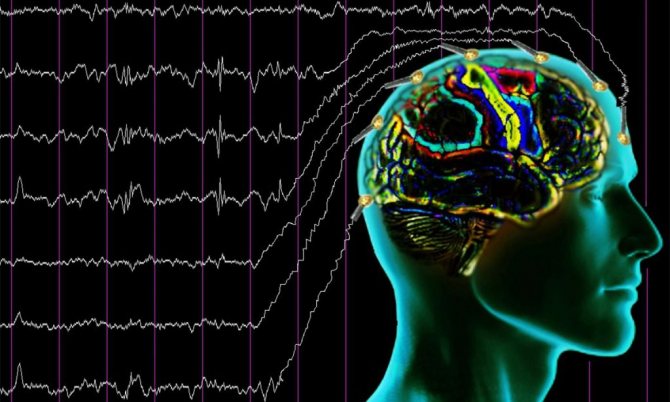
BEA dysrhythmia is diagnosed using several methods. The most informative is the electroencephalogram (EEG). Manipulation makes it possible to identify increased or, conversely, decreased bursts of electrical activity.
An EEG should not be confused with an ECG (electrocardiogram). The first method examines the brain, the second - the bioelectrical activity of the heart, its left or right ventricle, and myocardium. Both studies are highly significant for medicine, but have different implications.
A reliable diagnosis is made based on the following studies:
| Diagnostic method | Description |
| History taking | Determines the nature of symptoms in BEA disorders. The doctor conducts a full examination of the patient, paying attention to chronic ailments and head injuries. |
| Electroencephalography | Study of bioelectrical activity of the brain. The method identifies deviations from the norm and establishes the location of localization. The EEG shows abnormalities in BEA, but the cause is not determined. |
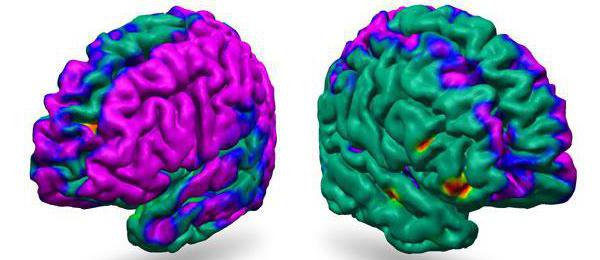
| MRI | Finds catalysts for accelerating or decelerating cortical rhythms. Shows irritative changes due to tumors, helps to establish the nature of neoplasms and study the structure of the cerebral hemispheres. |
| Angiogram | Necessary for diagnosing vascular atherosclerosis. |
How is dysrhythmia BEA treated? Therapy is prescribed only after a complete diagnosis of the patient and a control report. Without identifying the causes of the disorder, therapy is ineffective.
The rate of recovery of neural activity depends on how severely the brain tissue is damaged. If the changes are minor, treatment will be quick and effective.
Typically, a person diagnosed with BEA disorganization needs months, even years, to recover. It is easiest to restore brain activity at the initial stage of atherosclerosis; it is more difficult after radiation or chemical exposure, when irreversible changes have occurred in the tissues.
In exceptional cases, for example in the presence of tumors, surgery is required.
Decoding the electroencephalogram
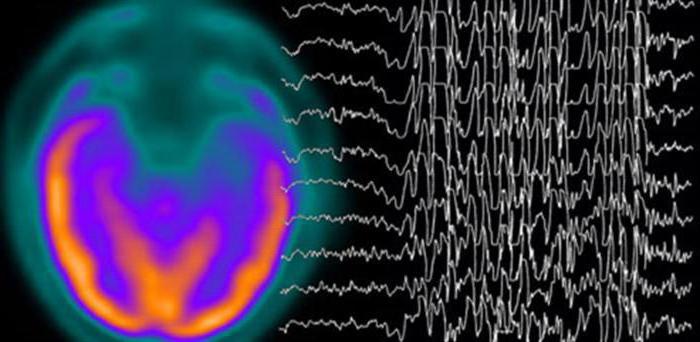
What does the EEG show when electrical conduction in the brain is not organized? The specialist sees BEA dysrhythms immediately, especially if the changes in rhythms are significant.
- rhythms manifest themselves in the form of wave asymmetry;
- disruptions in the distribution of alpha, beta, gamma waves are visible;
- their frequency and amplitude are outside the normal range;
- if the electroencephalograph registers a twofold increase in the beta rhythm, foci of epileptoid activity are visible, this may correspond to the onset of epilepsy.
During the EEG, photostimulation is performed. Normally, the rhythm of the waves should be equal to the frequency of the flashes. It is also considered normal to exceed the rhythm by 2 times. A low or repeatedly exceeded rhythm clearly indicates deviations.

Wave amplitude measures from one peak to another. The rhythm index is used to determine frequency.
In the EEG analysis they can write the following:
- mild regulatory changes, diffuse changes in the brain parenchyma;
- cerebral changes of a residual nature;
- bioelectrical disorientation of a general cerebral nature with the involvement of nonspecific midline structures of the hypothalamic level;
- relatively rhythmic BEA, dysfunction of mid-stem structures with foci of paroxysmal activity.
When deciphering EEG, specialists use a special database that contains normal indicators, as well as deviations, and what diseases they correspond to. Reading an encephalogram is not an easy task, requiring experience and dexterity.
Diffuse disorganization of cortical rhythms - what is it?
12 minutes Lyubov Dobretsova 24460
Electroencephalography or EEG is a highly informative study of the functional characteristics of the central nervous system. Through this diagnosis, possible disorders of the central nervous system and their causes are determined.
EEG interpretation in children and adults provides a detailed picture of the state of the brain and the presence of abnormalities. Allows you to identify individual affected areas.
Based on the results, the neurological or psychiatric nature of the pathologies is determined.
Prerogative aspects and disadvantages of the EEG method
Neurophysiologists and patients themselves prefer EEG diagnostics for several reasons:
- reliability of the results;
- no contraindications for medical reasons;
- the ability to perform research in a sleeping or even unconscious state of the patient;
- lack of gender and age boundaries for the procedure (EEG is performed on both newborns and elderly people);
- price and territorial accessibility (the examination is low cost and is carried out in almost every district hospital);
- insignificant time costs for conducting a conventional electroencephalogram;
- painlessness (during the procedure the child may be capricious, but not from pain, but from fear);
- harmlessness (electrodes attached to the head record the electrical activity of brain structures, but do not have any effect on the brain);
- the ability to conduct multiple examinations to track the dynamics of prescribed therapy;
- prompt interpretation of results for diagnosis.
In addition, no preliminary preparation is provided for conducting an EEG. The disadvantages of the method include possible distortion of indicators for the following reasons:
- unstable psycho-emotional state of the child at the time of the study;
- mobility (during the procedure it is necessary to keep the head and body static);
- the use of medications that affect the activity of the central nervous system;
- hungry state (a decrease in sugar levels due to hunger affects brain function);
- chronic diseases of the organs of vision.
In most cases, the listed reasons can be eliminated (conduct a study during sleep, stop taking medications, provide the child with a psychological mood). If the doctor has prescribed electroencephalography for your baby, the study cannot be ignored.
Indications for examination
Indications for functional diagnostics of a child’s nervous system can be of three types: control-therapeutic, confirming/refuting, symptomatic.
The first include mandatory research after neurosurgical operations and control and preventive procedures for previously diagnosed epilepsy, cerebral hydrocele or autism.
The second category is represented by medical assumptions about the presence of malignant neoplasms in the brain (EEG can detect an atypical lesion earlier than magnetic resonance imaging will show).
Alarming symptoms for which the procedure is prescribed:
- A child’s delay in speech development: impaired pronunciation due to a functional failure of the central nervous system (dysarthria), disorder, loss of speech activity due to organic damage to certain areas of the brain responsible for speech (aphasia), stuttering.
- Sudden, uncontrollable seizures in children (possibly epileptic seizures).
- Uncontrolled emptying of the bladder (enuresis).
- Excessive mobility and excitability of children (hyperactivity).
- Unconscious movement of the child during sleep (sleepwalking).
- Concussions, bruises and other head injuries.
- Systematic headaches, dizziness and fainting, of unknown origin.
- Involuntary muscle spasms at an accelerated pace (nervous tic).
- Inability to concentrate (distracted attention), decreased mental activity, memory impairment.
- Psycho-emotional disorders (unreasonable changes in mood, tendency to aggression, psychosis).
How to get correct results?
EEG of the brain in children of preschool and primary school age is most often carried out in the presence of parents (babies are held in their arms). No special training is required; parents should follow a few simple recommendations:
- Carefully examine the child's head. If there are minor scratches, wounds, scratches, inform your doctor. Electrodes are not attached to areas with damaged epidermis (skin).
- Feed the child. The study is carried out on a full stomach, so as not to blur the indicators. (Sweets containing chocolate, which excites the nervous system, should be excluded from the menu). As for infants, they must be fed immediately before the procedure in a medical facility. In this case, the baby will fall asleep peacefully and the study will be carried out during sleep.
It is important to stop taking medications (if the baby is receiving treatment on an ongoing basis, you need to notify the doctor about this). Children of school and preschool age need to be explained what they have to do and why. The right psychological attitude will help you avoid excessive emotionality. You are allowed to take toys with you (excluding digital gadgets).
You should remove hairpins and bows from your head, and remove earrings from your ears. Girls should not wear their hair in braids. If the EEG is repeated, it is necessary to take the protocol of the previous study.
Before the examination, the child's hair and scalp should be washed. One of the conditions is the good health of the little patient.
If the child has a cold or other health problems, it is better to postpone the procedure until complete recovery.
Methodology
According to the method of implementation, the electroencephalogram is close to cardiac electrocardiography (ECG). In this case, 12 electrodes are also used, which are symmetrically placed on the head in certain areas.
The application and attachment of sensors to the head is carried out in a strict order. The scalp in areas of contact with the electrodes is treated with gel. The installed sensors are fixed on top with a special medical cap.
Using clamps, the sensors are connected to an electroencephalograph - a device that records features of brain activity and reproduces the data on paper tape in the form of a graphic image. It is important that the little patient keeps his head upright throughout the entire examination. The time interval for the procedure, including mandatory testing, is about half an hour.
The ventilation test is carried out for children from 3 years of age. To control breathing, the child will be asked to inflate a balloon for 2-4 minutes.
This testing is necessary to identify possible neoplasms and diagnose latent epilepsy. Deviations in the development of the speech apparatus and mental reactions will help identify light irritation.
An in-depth version of the study is carried out on the principle of daily Holter monitoring in cardiology.
The baby wears the cap for 24 hours, and a small device located on the belt continuously records changes in the activity of the nervous system as a whole and individual brain structures.
After a day, the device and cap are removed and the doctor analyzes the results.
Such a study is of fundamental importance for identifying epilepsy in the initial period of its development, when symptoms do not yet appear often and clearly.
Decoding the results of the electroencephalogram
Only a highly qualified neurophysiologist or neuropathologist should decode the results obtained. It is quite difficult to determine deviations from the norm on a graph if they are not clearly defined. At the same time, standard indicators can be interpreted differently depending on the patient’s age category and health status at the time of the procedure.
It is almost impossible for a non-professional person to understand the indicators correctly. The process of deciphering the results may take several days due to the scale of the analyzed material. The doctor must evaluate the electrical activity of millions of neurons. The assessment of children's EEG is complicated by the fact that the nervous system is in a state of maturation and active growth.
The electroencephalograph records the main types of activity of the child’s brain, displaying them in the form of waves, which are assessed according to three parameters:
- Frequency of wave oscillations. The change in the state of waves over a second time interval (oscillations) is measured in Hz (hertz). In conclusion, the average indicator obtained by the average wave activity per second in several sections of the graph is recorded.
- The range of wave changes or amplitude. Reflects the distance between opposite peaks of wave activity. It is measured in µV (microvolts). The protocol describes the most characteristic (frequently occurring) indicators.
- Phase. This indicator (the number of phases per oscillation) determines the current state of the process or changes in its direction.
In addition, the rhythm of the heart and the symmetry of neutron activity in the hemispheres (right and left) are taken into account. The main assessment indicator of brain activity is the rhythm, which is generated and regulated by the most structurally complex part of the brain (thalamus). Rhythm is determined by the shape, amplitude, regularity and frequency of wave oscillations.
Types and norms of rhythms
Each of the rhythms is responsible for one or another brain activity. To decode the electroencephalogram, several types of rhythms are adopted, designated by the letters of the Greek alphabet:
- Alpha, Betta, Gamma, Kappa, Lambda, Mu - characteristic of an awake patient;
- Delta, Theta, Sigma - characteristic of the state of sleep or the presence of pathologies.
Manifestation of the first type:
- α-rhythm. It has an amplitude standard of up to 100 μV, frequency - from 8 Hz to 13. It is responsible for the calm state of the patient’s brain, in which its highest amplitude indicators are noted. When visual perception or brain activity is activated, the alpha rhythm is partially or completely inhibited (blocked).
- β rhythm. The normal frequency of oscillations is from 13 Hz to 19, the amplitude is symmetrical in both hemispheres - from 3 μV to 5. The manifestation of changes is observed in a state of psycho-emotional arousal.
- γ rhythm. Normally, it has a low amplitude of up to 10 μV, the oscillation frequency varies from 120 Hz to 180. On the EEG it is detected with increased concentration and mental stress.
- κ-rhythm. Digital vibration indicators range from 8 Hz to 12.
- λ rhythm. It is included in the general functioning of the brain when visual concentration is necessary in the dark or with eyes closed. Stopping the gaze at a certain point blocks the λ rhythm. Has a frequency from 4 Hz to 5.
- μ-rhythm. It is characterized by the same interval as the α rhythm. It appears when mental activity is activated.
Source: https://lechimsosudy.com/diffuznaja-dezorganizacija-korkovoj-ritmiki-chto/
Prevention
Many causes of changes in BEA are uncontrollable (irradiation, trauma, intoxication). But there are factors that can be eliminated by applying simple preventive measures.

Since the most common cause of BEA dysrhythmia is cerebral vascular atherosclerosis, it is necessary to monitor your lifestyle and take medications:
- increasing the elasticity of the vascular wall;
- reducing the degree of red blood cell aggregation;
- eliminating cholesterol plaques;
- preventing the proliferation of fibrous tissues;
- improving the functioning of the endothelium.
Preventive drugs include HeadBooster, Optimentis. What it is? These products are of plant origin and contain extract of the Ginkgo Biloba plant. They have a nootropic effect, enhance performance and improve cognitive functions of the brain, trigger the activation of neurons.
The medications should be taken in courses, adhering to the dose and recommendations for use. You can read reviews on the Internet.
General preventive measures that will help avoid changes in BEA:
- refusal of alcohol, tobacco, coffee, tea;
- moderation in food;
- avoiding hypothermia or overheating;
- frequent exposure to fresh air;
- performing a set of strengthening exercises;
- maintaining a gentle rest and work regime;
- no stress.

Normal bioelectrical activity of the brain (BEA) may be subject to changes caused by previous illnesses or injuries. These changes may appear localized in a particular area of the brain. Or they can be diffuse in nature - that is, spread to the entire brain as a whole without clearly identifying the source of the change, disrupting the passage of electrical impulses more or less evenly in all areas of the brain. In this case, they talk about disorganization of the bioelectrical activity of the brain. But in order to record diffuse changes in the bioelectrical activity of the brain, confirmation of a number of characteristic symptoms and specific electroencephalogram (EEG) indicators is necessary.
Electroencephalogram of the brain - definition and essence of the method
is a recording of the electrical activity of neurons in various brain structures, which is made on special paper using electrodes.
Electrodes are placed on different parts of the head and record the activity of a particular part of the brain. We can say that an electroencephalogram is a recording of the functional activity of the brain of a person of any age. The functional activity of the human brain depends on the activity of the median structures - the reticular formation and the forebrain, which determine the rhythm, general structure and dynamics of the electroencephalogram. A large number of connections of the reticular formation and forebrain with other structures and the cortex determine the symmetry of the EEG, and its relative “sameness” for the entire brain.
An EEG is taken to determine the activity of the brain in case of various lesions of the central nervous system, for example, with neuroinfections (poliomyelitis, etc.), meningitis, encephalitis, etc. Based on the results of the EEG, it is possible to assess the degree of brain damage due to various causes and clarify specific location that has been damaged.
The EEG is taken according to a standard protocol, which takes into account recordings in a state of wakefulness or sleep (infants), with special tests. Routine tests for EEG are:1. Photostimulation (exposure to flashes of bright light on closed eyes).2. Opening and closing the eyes.3. Hyperventilation (rare and deep breathing for 3 to 5 minutes).
These tests are performed on all adults and children when taking an EEG, regardless of age and pathology. In addition, additional tests may be used when taking an EEG, for example:
- clenching your fingers into a fist;
- sleep deprivation test;
- stay in the dark for 40 minutes;
- monitoring the entire period of night sleep;
- taking medications;
- performing psychological tests.
Additional tests for EEG are determined by the doctor–
who wishes to evaluate certain functions of the human brain.
Symptoms and diagnosis of diffuse changes
It is believed that the bioelectrical activity of the brain is disorganized if external signs appear, reflected in the behavior and reaction of the patient, and also if these changes are confirmed or preceded by hardware diagnostics. Often, the bioelectrical activity of the brain is first tested using a hardware method, after which suspicions arise, and only then do patients pay attention to behavioral and cognitive symptoms:
- sudden changes in mood from good to bad - and vice versa,
- decreased self-esteem,
- loss of interest in previous hobbies,
- slower performance of usual work,
- rapid onset of fatigue when performing even basic actions.
In general, the history of cerebral changes in BEA is also typical for other diseases of the central nervous system. A person describes his condition as a general malaise and may not correlate the symptoms with the first signs of diffuse changes in BEA (especially if the symptoms listed above are accompanied by dizziness and headaches, “jumping” blood pressure). Sometimes such changes are accompanied by signs of dysfunction of the diencephalic-trunk structures, which also manifests itself in complaints of poor health.
If diffuse changes are significant, and if a significant decrease in the threshold of convulsive readiness is recorded, then it is considered that the person is predisposed to epilepsy.
Common causes of changes - atherosclerosis, encephalitis, meningitis, toxic brain damage - are usually reflected in tissue necrosis, inflammation, edema, and scarring. And these pathologies, in turn, are recorded using EEG. In case of a general cerebral lesion, three types of pathological processes are recorded on the EEG, the most significant of which is considered the first, but the diagnosis is made in the presence of all three signs of the pathological process, namely:
- polymorphic polyrhythmic (multiplicity of rhythms) activity in the absence of regular dominant bioelectrical activity,
- disruption of the normal organization of the electroencephalogram, which is expressed in irregular asymmetry with simultaneous disturbances in the distribution of basic EEG rhythms, phase coincidence of waves in symmetrical parts of the brain, amplitude relationships,
- diffuse pathological oscillations (alpha, delta, theta, exceeding normal amplitudes).
Causes and consequences of changes
General cerebral changes in the bioelectrical activity of the brain can be caused by the following factors:
- Chemical toxic and radiation damage to the brain. Toxic poisonings that lead to disorganization are most often irreversible, affecting a person's ability to carry out daily activities. Such forms of lesions provoke severe forms of diffuse changes in the bioelectrical activity of the brain.

Head injuries and concussions. Here, the intensity of the changes depends on the severity of the damage caused: the stronger the damage, the more noticeable the result. With minor and moderate diffuse changes in the bioelectrical activity of the brain, the body feels slight discomfort, and impulse conductivity is restored without long-term treatment.- Inflammatory processes (including those caused by viral infection). Inflammations associated with meningitis and encephalitis are characterized by mild cerebral changes in BEA.
- Atherosclerotic vascular problems. The condition depends on the degree of vascular damage. The initial stage is characterized by mild diffuse changes in the bioelectrical activity of the brain. But with an increase in the area of vascular damage and tissue death, neuronal conduction disorders progress.
- Associated disorders. These include manifestations of regulatory pathologies. Cases associated with damage to the hypothalamus and pituitary gland are common. Changes can also be caused by incorrect functioning of the immune system.
Rough pronounced diffuse changes in the bioelectrical activity of the brain, as a rule, are the result of scarring, necrotic transformations, expansion of inflammatory processes and cerebral edema. Such signal conduction disturbances are heterogeneous, and instability of the BEA in complex cases is always accompanied by pathologies of the pituitary gland and hypothalamus.
Moderate changes in the bioelectrical activity of the brain are dangerous due to their complications. Subsequent stages, with softening or hardening of the brain tissue and the appearance of neoplasms, are transformed into cancer, diffuse sclerosis and other irreversible processes. To prevent them, treatment should be carried out at the stage of detecting slight changes in the bioelectrical activity of the brain. Moderate treatment and an attempt to reduce the consequences of the last stage of pathological changes are carried out only in specialized medical institutions.
Prevention and prognosis
The prognosis of diencephalic syndrome is ambiguous. It depends on the characteristics of the pathology that became its root cause. Persistent and irreversible changes in the hypothalamic-pituitary region cannot be eliminated with conservative therapy. In most cases, it only allows to reduce the negative manifestations of the syndrome. The course of the pathology is persistent and recurrent. Restoration of endocrine functions in women and men lasts an average of a year. Diencephalic syndrome caused by a tumor or severe neurotrophic disorders also has a poor prognosis. In other cases, a stationary state of the process or slow improvement is observed.
A certificate of incapacity for work is issued to persons with this disease for 2-3 weeks, during which they undergo inpatient treatment or intensive therapy on an outpatient basis.
Clinical recommendations from specialists:
- constant monitoring by the attending endocrinologist,
- implementation of all his recommendations,
- receiving maintenance therapy,
- compliance with the work and rest schedule,
- full sleep,
- balanced diet that normalizes body weight,
- optimal physical activity,
- timely sanitation of foci of infection,
- increasing the overall resistance of the body,
- preventive use of sedatives and tranquilizers.
Diencephalic syndrome is a serious disorder that affects the functioning of the entire body. This pathology is treated by specialists in the field of endocrinology, linking it with hypothalamic-pituitary hormonal disorders. Complex therapy allows you to eliminate various symptoms of the disease, activate the nervous and immune systems, and restore the functioning of the endocrine glands. If the syndrome is not treated correctly and in a timely manner, it will lead to disability of patients.
Prevention of increased diffuse changes in BEA
Some of the causes of cerebral changes in BEA are uncontrolled (injuries, poisonings, radiation). However, several causes are relatively easy to eliminate through preventive measures.
Since one of the most common causes of diffuse changes is vascular atherosclerosis, a preventive and therapeutic measure here will be correction of lifestyle, nutrition and the use of drugs that:
- improve the condition of the walls of large and small vessels, maintaining their elasticity,
- reduce the degree of red blood cell aggregation,
- eliminate cholesterol deposits and other lipid accumulations,
- prevent the proliferation of fibrous fibers,
- improve endothelial function.
The most popular preventive and therapeutic agents include herbal preparations HeadBooster, Optimentis with a nootropic effect of enhancing the performance and cognitive functions of the brain. Their popularity is explained by several factors, including a gentle, gentle effect on the vascular system of the brain and the presence of the relict plant Ginkgo Biloba in the extract. The effect of the drugs appears gradually, so they should be taken in courses. However, even in this case, one must adhere to the recommendations for a course of treatment, since an overdose of organic substances present in the Ginkgo extract increases the risk of developing strokes. When taken correctly, these drugs:
- reduce the permeability of the vascular wall, helping to strengthen it,
- normalize cholesterol levels,
- trigger antioxidant processes, preventing the destructive effects of free radicals on membranes,
- provide nutrition to brain cells by normalizing the transport of glucose and oxygen to tissues,
- facilitate the passage of impulses along nerve fibers.
In addition, in the drug treatment of atherosclerosis preceding diffuse changes, the following drugs are used:
- Nicotinic acid (its derivatives). Preparations based on it reduce cholesterol and triglycerides and increase the concentration of lipoproteins. All this improves antiatherogenic properties, but introduces a ban on these drugs for people with liver diseases.
- Fibrates. Miscleron, Gevilan, Atromide inhibit the synthesis of the body's own fats, but are fraught with side effects associated with the functioning of the liver and gall bladder.
- Bile acid sequestrants remove acids from the intestines, thereby reducing the amount of fat in cells, but can cause flatulence or constipation.
- Statins. They reduce the production of cholesterol by the body itself, which determines the time of taking them “at night,” when cholesterol synthesis increases. But their action can also destabilize the liver.
It is known that in the human brain there is an innumerable number of synaptic connections that provide our higher nervous activity. The number of neurons themselves - the main cells of the brain - is from 10 billion to 50 billion. Depending on various reasons, the neural network is damaged, and then various diffuse changes in the bioelectrical activity of the brain begin to progress.
Bioelectric activity of the brain: basic rhythms
Bioelectrical activity is literally the electrical vibrations of the brain. The neurons that create a huge network in it have their own electrical wave. These waves are recorded by EEG, and the data obtained through the study can tell a lot about the state of health and psyche of an individual.
Biowaves (or rhythms of brain activity) are divided depending on amplitude and frequency:
- beta waves - 14-40 Hertz, amplitude - up to 20 µV;
- alpha - 8-13 Hz, wave amplitude - 5-100 µV;
- gamma - above 30 Hz, occasionally up to 100 Hz, amplitude - up to 15 μV;
- delta - 1-4 Hz, amplitude - 20-200 µV.
Diffuse changes: symptoms
How do mild diffuse changes in the bioelectrical activity of the brain manifest themselves? Symptoms of changes will be noticeable even with the slightest changes in the normal activity of the biocomputer. As a rule, they are as follows:
- dizziness;
- slowness, weakness.
- With increasing changes, headaches and cramps appear.
The psyche also changes under the influence of changes in the brain. A person experiences sudden changes in mood, his behavior begins to seem hysterical to others. The circle of interests narrows, the motivation to act disappears. It becomes increasingly difficult for the patient to remember new information.
If these symptoms persist for a long time, you should urgently consult a doctor and get a diagnosis. Diffuse changes in the bioelectrical activity of the brain are a very serious disease. More precisely, its harbinger. If nothing is done, the condition worsens very quickly.
Diencephalic syndrome: causes, signs and manifestations, diagnosis, how to treat
Diencephalic syndrome is a complex symptom complex that indicates the development of serious disorders in the body and is manifested by signs of vegetative disorders, trophism and endocrinopathies. The disease develops as a result of damage to the structures of the hypothalamic-pituitary zone: thalamus, hypothalamus, epithalamus, pituitary gland. These organs actively interact with each other, are in close neurohumoral connection and regulate the functioning of the entire organism. When diencephalic structures are damaged, a syndrome develops, manifested by signs of endocrine and nervous dysfunction.
The hypothalamus plays a huge role in the functioning of the entire body. It secretes statins and liberins, which stimulate or inhibit the activity of hormone-producing cells of the pituitary gland. At the same time, the secretion of tropins, which realize their physiological effect by influencing the synthesis of hormones of the peripheral endocrine glands, decreases or increases. By influencing the thyroid gland, ovaries and testes, and adrenal glands, the pituitary gland regulates the functioning of internal organs. Elements of the hypothalamic-pituitary system exist in close interaction. Any malfunctions in the functioning of this system immediately affect the functioning of almost all organs.
Hypothalamic syndrome develops when there is dysfunction of the hypothalamus. Patients experience changes in body weight, headaches, mood changes often, hypertension develops, the menstrual cycle is disrupted, thirst occurs, and libido changes. The syndrome first appears in adolescents aged 13-15 years. Clinical signs become most pronounced at 30-40 years of age. The syndrome develops more often in women and affects their reproductive health. Patients are diagnosed with endocrine infertility, polycystic ovary syndrome, and perinatal pathologies.
Diencephalic syndrome has an ICD-10 code E23.3 and refers to “Dysfunctions of the hypothalamus, not classified elsewhere.” Pathology disrupts the process of normal development in children. In them, dysfunction of the hypothalamus also manifests itself as signs of damage to the endocrine glands and nervous system.
Pronounced and moderate changes
Moderate diffuse changes in the bioelectrical activity of the brain do not cause any harm, at least immediately. But the ultra-precise harmony of the universal system has already been disrupted, and soon these changes are likely to develop into more serious problems.
It happens that along with a disturbance in brain activity, disturbances in the functioning of its basic structures are revealed. This means that the thalamus or hypothalamus may be affected. As a result of such disorders, various endocrine or neurological syndromes arise.
The fact that pronounced diffuse changes in the bioelectrical activity of the brain begin is indicated by the onset of seizures. A person may develop a seizure disorder that has not previously bothered them. Or, more and more often, the pressure jumps for no reason. Seizures are a rather alarming symptom and can lead to the development of epilepsy.
Therapeutic measures
Endocrinologists, neurosurgeons, neuropathologists and gynecologists treat diencephalic syndrome. After conducting a thorough diagnosis, they select certain treatment methods individually for each patient.
Treatment of pathology is prescribed in accordance with the degree of metabolic, nervous and trophic processes disorders. Patients are prescribed etiological, symptomatic and pathogenetic therapy. Complex treatment of the syndrome is aimed at normalizing the functions of central regulatory mechanisms, metabolism and the regular menstrual cycle.
- Tumors, cysts and other neoplasms are surgically removed. Surgery is also used to eliminate the consequences of head injuries.
- Etiotropic treatment of infectious processes involves the use of antibiotics or sulfonamides.
- When intracranial pressure increases, patients are prescribed dehydration agents - diuretics "Furosemide", "Lasix".
- Regulation of the tone of the autonomic nervous system is carried out with the help of vegetotropic agents - calcium chloride, vitamin B1, Diphenhydramine, Novocaine, Ephedrine.
- To improve the bioelectrical activity of the brain, Carbamazepine or Diphenin are used.
- Angioprotectors that improve cerebral circulation - Vinpocetine, Cerebrolysin, Piracetam.
- General restoratives increase the activity of the sympathetic nervous system - calcium supplements, antioxidants, vitamin complexes.
- To suppress sympathetic activity, antipsychotics, antispasmodics, and ganglion blockers “Pentamine” and “Benzohexonium” are used.
- Hormone replacement therapy for the syndrome - Sinestrol, Premarin, Progesterone, Testoviron, Andriol.
- Detoxification - “Hemodez”, “Sodium thiosulfate”, “Ringer’s”, glucose, saline solution.
- Antidepressants for relieving exacerbations of the syndrome - Pirroxan, Grandaxin and neuroleptics - Phenothiazine, Sonapax.
- Antihistamines - Diphenhydramine, Suprastin.
- X-ray therapy on the hypothalamic region – 6-8 sessions.
Experts recommend that patients follow a diet and daily routine, normalize sleep, get proper rest, avoid stress, conflicts and nervous tension, and sanitize foci of infection. They are prescribed psychotherapeutic sessions and auto-training. Acupuncture, balneotherapy, therapeutic exercises, physiotherapy - calcium electrophoresis, galvanization of the collar area have a positive effect in the recovery period.
Irritative changes
The term “irritation” belongs to the science of neurology. Under this name lies a large number of potential damage to brain structures. Irritation itself is not a syndrome or a disease; it serves as an indication of irritation of certain brain structures.
Diffuse irritative changes in the bioelectrical activity of the brain lead to changes in the perception of one’s own body or to speech dysfunctions. Problems with the hypothalamus explain the mental phenomenon of depersonalization. This is a personality disorder in which a person perceives himself externally. However, these are complex irritative disorders. Mild deviations are characterized only by a deterioration in general well-being and some mood swings.
Symptoms
Changes in the BEA of the brain immediately affect the physical and mental state. A mild to moderate level of tissue biopotential impairment is manifested by:
- headaches;
- regular fluctuations in blood pressure;
- dizziness;
- sudden changes in emotional state, hysteria;
- problems with memory and performance;
- convulsive conditions.
Moderate and strong changes in BEA, expressed by a slowdown in the background frequency, signal the onset of epilepsy.
Reasons for changes
Diffuse changes in the bioelectrical activity of the brain are not inherited and do not arise out of nowhere. These anomalies are a consequence of disruption of certain brain processes, and sometimes damage to neural connections. What else leads to disturbances in the functioning of the central nervous system:
- Anemia (anemia). The brain receives little oxygen, and cells—neurons—starve.
- Atherosclerosis of cerebral vessels.
- Inflammation due to infection (meningitis, encephalitis, arachnoiditis).
- Associated disorders. Often the cause of this condition is a persistent metabolic disorder and lack of sleep.
In case of gross changes in brain activity, examination usually reveals:
- necrotic processes;
- scarring;
- brain swelling.
The causes of such serious conditions are injuries and bruises. A neurologist should strictly monitor all changes. Such a disease cannot be left to chance.
Changes in the cortex
Damage to the fields of the cerebral cortex leads to various disorders of behavior and consciousness. After all, this area is responsible for our higher nervous activity.
So, sometimes one zone is damaged, and sometimes several. Let's look at examples:
- If the occipital lobe is subject to any changes, attacks of hallucinations are observed.
- Central gyrus - there are epileptic seizures that begin with twitching of an arm or leg.
- Posterior central gyrus. The patient experiences numbness or tingling sensations throughout the body.
- Adversive field - convulsions with loss of consciousness.
These are local signs of bark irritation. When it is not possible to determine the localization of various attacks during the study, and the EEG shows deviations in rhythms, diffuse changes in the bioelectrical activity of the cerebral cortex are evident. This also results in hearing or vision impairment and olfactory hallucinations. Various attacks of twitching of the head or other parts of the body are also observed when the convulsive threshold is significantly reduced.
Diagnosis and treatment
To establish a diagnosis, the patient must undergo a set of diagnostic procedures and give the doctor a comprehensive anamnesis (history of symptoms that worry the person). The first study is an EEG, then rheoencephalography (REG) is needed. REG is an examination of the blood vessels of the brain, necessary to find out whether there is stagnation of blood. An MRI is also needed. Tomography will give the doctor an accurate answer to the question of the presence of a tumor. And if there is one, then what type.
As for the treatment of such patients, diffuse changes in the biological activity of the brain are treated only in the clinic under the supervision of an expert neurologist.
Immediate contact with a neurologist increases the chances of full recovery, even if parts such as the pituitary gland, pineal gland, thalamus or hypothalamus (diencephalic structures) are affected. It will take almost a year. Unexpressed changes are treated much faster - within just 2 or 3 months.
EEG interpretation
If something in the brain is abnormal, what does the EEG show? The specialist immediately sees diffuse changes in the bioelectrical activity of the brain. After all, disturbances in normal rhythms are significant:
- They manifest themselves in the form of wave asymmetry.
- Disturbances in the distribution of basic rhythms (alpha, beta, gamma) are visible. Their usual frequency and amplitude are beyond the normal range. When, for example, the EEG shows an increase in the beta rhythm by 2–3 times against the background of some foci of epileptoid activity, there is about a 50% chance of the onset of epileptic seizures.
- Brain activity is polymorphic and polyrhythmic.
All 3 pathological aspects must be present for the diagnosis to be confirmed.

During EEG, photostimulation is required. Signs of normality when stimulating the brain with light flashes include the appearance of a wave rhythm equal to the frequency of the flashes. An excess of 2 times is also considered normal. However, if the rhythm is lower than the initial frequency of flashes or is repeatedly exceeded, this is an unambiguous sign of deviations.
The amplitude of the waves is measured from one peak to another. In this case, the isoelectric line is not taken into account. The frequency of brain waves on the EEG is determined using the rhythm index. All normal indicators and those that characterize waves of people with various diseases (Parkinson, autism) are in a special database.
For specialists working with these brain problems, it is important to train for a long time in “reading” encephalograms, using such databases. After correlating the patient’s indicators with normal values, the doctor draws up a conclusion.
What are cerebral BEA disorders?
Unusual generalized BEAGM changes observed in comatose patients include alpha coma, beta coma, and spindle coma.
Three-phase waves are positive, high-amplitude sharp fluctuations of more than 70 microvolts. A positive wave is usually preceded by a slow negative wave. Typically, the first negative wave has a higher amplitude than the second. The standard clinical correlate of triphasic waves is metabolic or other type of encephalopathy.
Alpha, beta and spindle coma are less common in clinical practice, but the most dangerous. All patterns of coma usually indicate a severe degree of encephalopathy. It should be noted that the patient's psychomotor reaction is a good prognostic factor in these conditions.
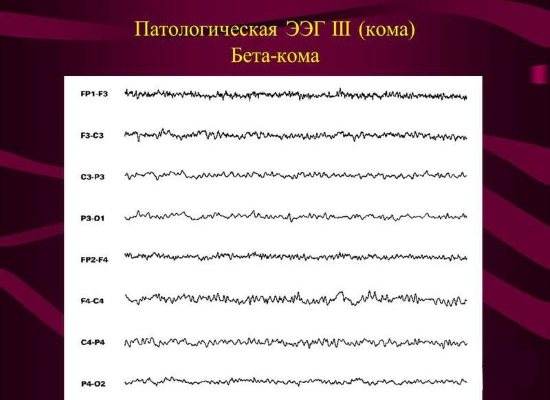
Beta coma is most often caused by intoxication
Triphasic waves are classically associated with hepatic encephalopathy. However, they are not specific and can be observed in uremic encephalopathy, as well as in other types of metabolic disorders. Many other diseases may have a triphasic morphology. Like regulatory changes in BEAGM, triphasic waves are quite often observed in the context of a pseudoepileptic seizure.
The human brain is a complex system in which the main role is played by electrical impulses generated and transmitted by neurons. The optimal scheme for such interaction is frequency, therefore nature and evolution implemented it in the brain much earlier than humans. In general, different parts of the brain generate and use up to nine frequency signals. For functional diagnostics, four main ones are sufficient - alpha, beta, theta and delta brain rhythms, which are recorded by an electroencephalograph.
The results of brain encephalography are presented as separate rhythm recording graphs. During analysis, they are combined into a single index that reflects BEA - the bioelectrical activity of the brain objectively, in a state convenient for study.
Any patient is interested in what [parameters of brain function are recorded by encephalography]. But not everyone, except neurophysiologists, understands that the result of the study is relative, but it does not lead to a final conclusion about the disease. Sometimes BEA rhythms may be altered. In such cases, they speak about the probability or absence of pathology.
Only epilepsy can be reliably diagnosed by EEG, but even this conclusion will require further research - you need to find the source of abnormal rhythms, a pronounced and localized thickening, scar or softening. The readiness for seizures and convulsions is indicated by the distribution and increased activity of delta and theta rhythms during wakefulness in an adult.
The brain is an electrochemical organ. Electrical activity in the brain manifests itself in the form of brain waves. Four types of waves are recorded on the EGG:
- beta waves (the fastest oscillations with large amplitude, the frequency of which is in the range of 15–40 Hz) are generated by the awake brain, actively involved in mental activity;
- alpha waves are the opposite of beta waves, their amplitude is larger and their frequency is 9-14 Hz;
- for theta waves, the amplitude is even greater, and the frequency is 5-8 Hz, they are generated by the brain of a person who is almost asleep;
- delta waves have a maximum amplitude and frequency of 1.5-4 Hz.
If the frequency of theta waves on the ECG drops to zero, this means that brain death has occurred. Deep, dreamless sleep is characterized by a theta wave frequency of 2-3 Hz. When a person lies down in bed and reads for a few minutes before going to sleep, he or she is in a “low beta” state. The moment we put down a book, turn off the light and close our eyes, the brain waves successively pass through the stages of beta, alpha, theta, and ultimately delta.
The four types of brain vibrations are common to all people, regardless of gender, age, nationality, culture and nationality. The results of EEG studies show that although one frequency always dominates in brain oscillations, the remaining three, depending on the level of activity of the person, are also always present.
Prevention
The most common cause of diffuse changes is circulatory disorders due to vascular atherosclerosis. Atherosclerosis develops against the background of poor nutrition. Some drugs can strengthen vascular walls, one of them is Ginkgo Biloba. And drugs of the statin class are now capable of lowering cholesterol levels. Fibrates reduce the ability to synthesize fats, thereby preventing the development of atherosclerosis.

And, of course, you need to take care of your head, since diffuse disorders after blows and head injuries take a long and difficult time to treat. But if you take care of the harmonious system of synaptic connections, monitor your diet and give yourself time for proper rest, your brain will function flawlessly and accurately for a long time.
Therapy
Diffuse brain activity disorder should be treated only in a medical facility. The therapeutic plan is organized taking into account the cause of the BEA distortion. It is most difficult to restore the brain of a patient who has suffered intoxication or radiation exposure. With atherosclerosis, normalization of brain activity is possible only at the initial stage.
Drug therapy involves taking medications aimed at eliminating both the provoking disease itself and its mental, neurological, metabolic, and autonomic symptoms. Are used:
- antioxidants;
- nootropics;
- drugs to normalize metabolism;
- vasoactive medications;
- calcium antagonists to normalize cerebral activity;
- the drug "Pentoxifylline" to improve blood circulation.
Physiotherapeutic measures give good results: magnetotherapy, electrotherapy, balneological procedures. For vascular diseases, hyperbaric oxygenation (saturation of tissues with oxygen under pressure of up to 1.5 atmospheres) and ozone therapy are used.
With atherosclerosis, a change in diet is required, eliminating foods that increase cholesterol levels in the blood. If the disease is advanced, the doctor prescribes a drug from the statin group. Medicines from the fibrate category inhibit lipid synthesis and prevent the development of atherosclerosis.
In case of severe diseases, the intervention of a neurosurgeon is necessary.