What is the provoking factor?
The main reason for the occurrence of epileptic seizures is the withdrawal of medications taken, the action of which is aimed at suppressing epileptic seizures.
However, status epilepticus can occur not only against the background of epilepsy, but also due to brain lesions, including:
- head injury;
- intoxication;
- intracranial malignant tumor;
- circulatory disorders in the brain;
- infection;
- dropsy of the brain (encephalopathy);
- withdrawal syndrome;
- complications of diabetes;
- hematoma.
The incidence of epistatus without a predisposing factor - epilepsy is approximately 50%.
Types and stages of epistatus
The variability of the types of epileptic seizures determines the formation of various clinical forms of epileptic seizures. They are divided into two main groups - convulsive and non-convulsive seizures.
According to the classification, the following types of status epilepticus are distinguished:
- Generalized SE - characterized by widespread tonic-clonic convulsions with an unconscious state.
- Not completely generalized ES - characterized by atypical muscle spasms with complete loss of consciousness. Tonic status is most common among children with Lennox-Gastaut syndrome. Can be observed at different ages. Clonic status is observed with epilepsy in infants, as well as with convulsions with high fever in young children. Myoclonic status is characterized by constant or episodic muscle twitching.
- The status of focal paroxysms proceeds according to the type of Jacksonian epilepsy with muscle contraction of a certain localization, for example, only the muscles of the face, one limb or half of the body. In this case, loss of consciousness may not occur.
- Absence or non-convulsive status is accompanied by a complete loss of consciousness without muscle contractions. Such attacks are characterized by the mildest course, however, due to the absence of seizures, diagnosis can be difficult.
- Partial status is characterized by unconscious and automatic actions with complete or incomplete loss of consciousness.
The stages of development of epistatus are also distinguished:
- pre-status - lasts 1-10 minutes;
- initial - lasts from 10 minutes to half an hour;
- expanded - lasts from half an hour to an hour;
- refractory - lasts more than an hour.
First aid
Providing assistance for status epilepticus can be carried out at several stages, one of which is pre-medical. Any person who sees the onset of a seizure can provide such assistance. The first thing you need to do is call an ambulance. Before her arrival, the patient in this condition should not be moved, only if he is near a cliff or other dangerous place. If it is on a hard surface, it is recommended to place something soft under the head, for example, rolled up clothing. To prevent injury, remove any nearby objects. And it is also recommended to turn the person on their side - this will help prevent possible aspiration of fluids (produced saliva or blood resulting from biting the tongue).
In such situations, you should not do the following:
- putting various objects into the patient’s mouth;
- unclench your teeth, as this can injure the person who is trying to provide first aid and damage the patient’s teeth;
- give the epileptic food or drink;
- fix the limbs, as this increases the likelihood of injury due to severe cramps involving the muscles;
- It is worth removing clothing that is constricting or has a suffocating effect.
Before the ambulance arrives, it is recommended to monitor the duration of seizures and their number. This will be important information to rule out other diseases.
What does it look like in real life
Symptoms of status epilepticus are determined by severe disorders in consciousness, respiratory system and hemodynamics, which are caused by a previous attack; the number of seizures during epileptic status can range from 3 to 20 per hour.
Consciousness by the time of the next attack does not clear up and the person is in a state of stupor, numbness or coma.
With prolonged ES, the comatose state worsens, becomes deeper, convulsions take on a tonic form, an increase in blood pressure is replaced by a sharp decrease, and increased reflexion is replaced by a lack of reactions. Hemodynamic and respiratory disorders become more pronounced.
The convulsions may disappear, and then the stage of epileptic prostration begins, which is characterized by external changes:
- pupil size changes;
- the gaze becomes unconscious;
- mouth slightly open.
It is very dangerous! In this condition, death can occur.
Epistatus necessarily lasts more than half an hour. This condition should be differentiated from episodic attacks, during the intervals between which there is a complete or almost complete clearing of consciousness, as well as a partial restoration of the patient’s physiological state.
The course of convulsive SE can be divided into two phases. At the first stage, compensatory changes occur to maintain blood circulation and the metabolic process.
This condition is characterized by:
- tachycardia;
- high blood pressure;
- vomit;
- involuntary urination;
- involuntary defecation.
The second phase occurs after half an hour or an hour and is characterized by a breakdown of compensatory changes. In this state, the following processes occur:
- lowering blood pressure;
- arrhythmia;
- respiratory dysfunction;
- thrombosis of the pulmonary artery and its branches;
- acute renal and liver failure.
Non-convulsive epistatus is characterized by various disorders of consciousness:
- feeling of detachment;
- immobilization.
In the case of ES of complex partial seizures, the following is observed:
- behavioral deviations;
- confusion;
- symptoms of psychosis.
Status epilepticus from A to Z:
First aid - rules and tips
The main goal when providing first emergency care in case of epistatus before the arrival of doctors is to prevent damage and trauma to the patient.
What to do during an attack:
- lay the person on a comfortable surface to reduce the risk of injury;
- remove those items of clothing that may cause discomfort (for example, a tie, a belt), unbutton the collar;
- place rolled clothing under your head;
- carefully turn your head to the side so that the patient does not choke on his saliva;
- if your mouth is slightly open, you need to put a handkerchief or some kind of cloth between your teeth, but in no case a sharp object, so as not to break your teeth;
- remove all dangerous objects that are in the immediate vicinity to avoid injury;
- do not hold the person too tightly, otherwise there is a high risk of broken bones;
- do not open your teeth if they are clenched.
Symptoms and first aid
Manifestations of seizures in adults include involuntary muscle contractions, which can be either generalized (over the whole body) or localized (local). There are also tonic, clonic and mixed (clonic-tonic) seizures. Tonic contractions are long, clonic contractions are short, but with a large interval.
First aid measures for convulsive syndrome should be aimed at preventing injuries. To do this, you need to make sure that the sick person does not fall or hit himself - lay him on a hard surface, place a pillow under his head. You cannot restrain the patient, as this increases the risk of bone fractures and tendon rupture, especially with tetanus.
Epilepsy
Generalized convulsive seizures followed by restoration of consciousness or short-term focal convulsive seizures.
Further actions
Relief of status epilepticus is carried out through the following measures:
- ensuring airway patency;
- use of oxygen therapy;
- intravenous injection of Diazepam (maximum daily dose - 40 mg), a side effect of this drug may be respiratory depression.
Further therapy is carried out by administering medications depending on the stage of status epilepticus.
At the initial stage, the following drugs are used to relieve status epilepticus:
- Diazepam;
- Lorazepam;
- Depakine;
- Feniton;
- Oxybutyrate.
Among the side effects of treatment, the following consequences can be identified: arterial hypotension, acute toxic hepatitis, phlebosclerosis, hypokalemia.
At the advanced stage of ES the following is used:
- Diazepam;
- Lorazepam;
- Phenobarbital;
- Sodium thiopental.
At the refractory stage of ES, the following measures are carried out:
- Intubation, correction of electrolyte disturbances, transfer to artificial ventilation of the lungs - to maintain vital functions of the body.
- Barbiturate anesthesia - intravenous injection of sodium thiopental for 20 seconds. 100-250 mg of the drug is administered. If the patient's condition does not improve, a dose of 50 mg is administered every few minutes until the seizure stops. Barbiturate anesthesia can last from 12 hours to a day.
- Dexamethasone and Mannitol injections are given to prevent cerebral edema.
- Infusion dehydration therapy is carried out to eliminate disorders of liquor dynamics and the metabolic process. For this purpose the following are used: Magenzia, Lasix, Cordiamin, Eufillin, Korglykon.
In the event that the epistatus is symptomatic, that is, it arose against the background of brain damage, a neurosurgical operation should be performed to compress the brain vessels.
How to cope with an attack?
The mechanism for the appearance of epistatus implies immediate assistance to the injured baby. The list of resuscitation measures includes:
- Monitoring the state of the respiratory system, respiratory rate and quality of blood circulation. The baby needs pure oxygen, you will have to determine your blood sugar level and prevent hypoglycemia.
- Fighting cramps. Diazepam can be administered intravenously.
- In a situation where a cramp lasts longer than 10 minutes, more powerful drugs are used, for example phenytonn, the dosage is determined by the doctor.
- Equipment for artificial lung ventilation is connected.
- Volume replacement is required to improve systemic blood pressure and perfusion pressure in the head.
- Use of inotropic agents, if necessary, provide children with general anesthesia.
Features of the condition in children
Very often, epistatus that occurs in children is a sign of the onset of epilepsy, but it happens that convulsive attacks appear already in the later stages of the course of this disease.
In newborns, a seizure occurs with partial loss of consciousness, while the reaction to external stimuli remains intact.
Generalized SE can manifest itself as tonic-clonic, clonic, myoclonic convulsions.
In nonconvulsive SE, electroencephalography is used to detect peak-wave stupor and slow waves, which reflect a state of epileptic stupefaction. Partial ES can be simple, somatomotor, or dysphasic.
In complex partial epistatus, stable preservation of epileptic twilight of consciousness is observed.
With generalized SE, the main property of an epileptic seizure is disrupted - it does not go away on its own.
The number of attacks can reach several tens or even hundreds per day. In this case, respiratory function and hemodynamics are disrupted, metabolic processes in the brain are disrupted, and the coma state can deepen until death occurs.
Diagnosis and treatment of status epilepticus
Since status epilepticus is an urgent condition, a minimum of time should be spent on its diagnosis. It is important to clarify the epileptic history and determine the type and doses of anticonvulsants previously taken by the patient. Basically, the diagnosis is established taking into account the medical history (trauma, intoxication, epilepsy, etc.) and the clinical picture. Additional examinations are necessary to clarify the etiology and assess the condition of the somatic systems of the body. It is possible to urgently carry out a biochemical blood test, urine test, and blood gas analysis; monitoring EEG and blood pressure. Diagnosis of non-convulsive forms of status is made using electroencephalography data. Accurate diagnosis of the cause of symptomatic epistatus can be carried out using MRI, MSCT or CT scan of the brain.
Treatment of status epilepticus is urgent and can be carried out by an epileptologist, neurologist, traumatologist, resuscitator, neurosurgeon and other specialists. If possible, the patient should be admitted to the intensive care unit. To protect it, it is necessary to fix the limbs. The primary task is to restore airway patency and relieve hypoxia, including the use of mechanical ventilation. Almost simultaneously, intravenous administration of diazepam is necessary. In most cases, a 1-2-fold administration allows, if not completely stopping, then at least interrupting the course of the epistatus.
In cases where status epilepticus cannot be stopped, they proceed to continuous administration of diazepam using an automatic dispenser or dropper. At the same time, they are fighting cerebral edema (mannitol is administered by drip, acetazolamide is administered orally or through a probe) and symptomatic therapy (corticosteroids, cardiovascular drugs, niketamide, heparin is administered for DIC syndrome). If status epilepticus occurs against the background of epilepsy, continue anticonvulsant therapy with the previously used drug, increasing its dose by 1.5 times.
The lack of effect of the treatment is an indication for the use of reserve methods: thiopental anesthesia, craniocerebral hypothermia, intravenous bolus administration of glucocorticosteroids, etc. If status epilepticus is caused by a large intracranial formation, urgent neurosurgical intervention is necessary: decompressive craniotomy, removal of intracerebral hematoma, stopping intracranial bleeding, etc. . P.
Clinical picture
Status epilepticus can occur in a situation where patients are not provided with proper care or when the patient neglects the advice of doctors. Status epilepticus does not have characteristic features in the clinical picture that could be used to distinguish the condition from a generalized seizure.

If it is nevertheless possible to differentiate the disorder, with status epilepticus the patient cannot return to a conscious state, but consistently experiences generalized seizures.
To correctly distinguish them, you will need a description of the classic symptoms that divide the seizure into 2 phases. The first, tonic, lasts 30 seconds and has complex consequences. Convulsion of all muscle tissues of the patient, including internal organs. Skeletal muscles may be damaged, the eyes roll back and open wide, and the mouth is held half open. First, the muscles of the torso experience spasms, then the arms and legs.
The second, clonic phase is characterized by contractions, the body, arms and legs bend and twitch. The duration of the phase is 3 minutes. Some seizures are preceded by a change in condition, headache. As an aura, stereotypical short-term defects may occur in the form of intense sweating, dizziness, and nausea.

During a generalized attack with two phases, symptoms appear in the form of mydriasis and areflexia, in which the pupils do not respond to external stimuli. Taking into account hypersalivation and increased clonic convulsions, foam appears near the mouth, and the possibility of biting the tongue increases. Muscle agony occurs while the patient is in a comatose state, resulting in uncontrolled bowel and bladder emptying.
Status epilepticus should be considered as a complex condition that threatens people's lives.
Prevention
Status epilepticus can most likely be prevented if you do not skip taking medications for epilepsy, promptly treat infectious diseases and head injuries, and avoid injuries and intoxications.
Adult patients should not drink alcohol, smoke, or take drugs. Patients with epilepsy need to be registered at a dispensary and regularly undergo examination by a neurologist and preventive treatment.
Is everything in the article correct from a medical point of view?Answer only if you have proven medical knowledgeYesNo
Share the article: Read us on Yandex.Zen
Diseases with similar symptoms: Anemia (matching symptoms: 6 out of 11)
... Absence (matching symptoms: 5 out of 11)
... Mechanical asphyxia (matching symptoms: 5 out of 11)
...Ventricular fibrillation (overlapping symptoms: 5 of 11)
... Asphyxia (matching symptoms: 4 out of 11)
...Which doctor should I contact?
If you suspect a disease such as status epilepticus, you should consult a doctor:
- A neurologist is a doctor who diagnoses and treats diseases associated with the central and peripheral nervous system. Read >
Best Neurologists in Ekaterinburg
Yuri Mikhailovich Nemchenko32 reviews Vladimir Vladimirovich Nevolin8 reviews Albina Amirovna Syunikova16 reviews Evgeniy Borisovich Ivanov26 reviews Tatyana Viktorovna Boreyko26 reviews All Neurologists of Yekaterinburg (49)
An epileptologist is a neurologist or a narrow-profile psychiatrist specializing in the diagnosis and treatment of epilepsy , as well as rehabilitation of patients, its transfer.Read >
Differential diagnosis
Status epilepticus requires differential diagnosis and distinction from psychogenic non-epileptic seizures. Pronounced seizure activity has been detected in several patients with psychogenic disorder. For differential diagnosis of psychogenic and real ES, you need to be aware of 4 main properties of the latter:

- Spread of motor activity during a seizure.
- Stereotypic condition.
- No pauses in convulsions during a seizure.
- During attacks, the eyes open.
Often, generalized symptoms appear in phases.
Clonic muscle contractions, during which tonic tension appears and subsequently cessation of the attack, are never detected during a real epileptic sign. Mild clonic contractions may occur before the tonic phase.
It would be useful to determine whether the patient has used any antiepileptic drugs, narcotic substances or alcohol. The examination is carried out to determine the symptoms of head injury, meningism, neurological deficit, and sites for insulin injections.
The need for intensive CT is determined if a TBI is suspected as a factor provoking a convulsive state. If there is a possibility of infection spreading in the nervous system, a lumbar puncture should be performed.
My husband has epilepsy
Girls, my husband has epilepsy. Congenital. Previously, he was treated until he was 14 years old... then he got tired of “swallowing pills” and quit. He drank a lot of beer, had attacks every 2 weeks, and his attacks occur when he sleeps at 2-3 am. When we decided to live together, he went to the doctor, she forbade him to drink beer in the first place and told him to start treatment again, now new drugs and treatment will be 1 month a year. He stopped drinking beer altogether, but doesn’t want to be treated... He says that he needs a lot of money for all the examinations. We are planning a child right now, but I’m very scared of the attacks, I’m afraid that because of this we can’t succeed... I get scared when he starts screaming at night, although now the attacks are already once every 2-3 months, but to be honest, I have enough impressions. It’s impossible to see this, but I jump out of bed and run into the bathroom, put headphones in my ears (the player is always in the bathroom, ready) and turn on the water. And I pray that the attack goes well. I am very afraid that he will pass this terrible disease on to his child. Girls! Who has the same problem? How can I get him to heal?
Symptoms
With the development of ES, the functioning of all organs and systems of the body is disrupted. ES occurs in two phases:
- Compensatory. Lasts 30–60 minutes, compensatory functions operate aimed at maintaining metabolism and hemodynamics. In this phase, blood flow increases, blood pressure rises, and the pulse quickens. During convulsions, involuntary urination, defecation, and vomiting occur.
- Failure of compensation. Blood pressure drops sharply, the pulse slows down, arrhythmia appears, and various forms of acute failure develop (respiratory, cardiac, renal, hepatic). Against the background of progressive disorders, epileptic prostration occurs: convulsions stop, the pupils dilate, the gaze becomes indifferent, the mouth is half open. At this stage, without emergency help for status epilepticus, the patient may die.
As an attack develops, breathing is disrupted and a complete short-term stop occurs (apnea). As the seizure ends, breathing becomes faster as a compensatory mechanism (hyperpnea).
Alternating apnea and hyperpnea significantly increases seizure activity in the brain. Thus, repeated electroactivity occurs, completing the circle. This causes long-term continuous circulation of electrical impulses through the nerve cells of the cerebral cortex, which leads to new attacks.
Under the influence of cramps, muscle fibers die, particles of which enter the bloodstream and enter the kidneys with the blood. The kidney tubules become clogged, and the formation and outflow of urine is disrupted.
Prolonged muscle activity during tonic-clonic convulsions leads to hyperthermia (overheating of the body), acidosis (increased acidity). Respiratory disorder causes hypoxia (oxygen starvation), cardiovascular disorders and, as a result, brain damage. The premotor areas of the brain are active and are responsible for muscle movements. This is an overload that the body cannot bear for a long time without emergency help.
The absence seizure state (without muscle activity) can last for hours and be invisible to others. With non-convulsive status epilepticus, consciousness is confused or switched off, no seizures are observed, the patient may fall into a coma. There is no convulsive focus in the brain, but high convulsive readiness. With moderate impairment of consciousness, patients can stay in the ES for a day or more, performing usual actions.
In most cases, from the outside, patients give the impression of adequate, but slightly inhibited people. With non-convulsive epistatus, inadequacy may manifest itself, for example, a high-ranking official, or just a wealthy person, can rummage through a trash can or wander. With severe impairment of consciousness, psychosis and schizoid states can develop. Nonconvulsive ES is not as life-threatening as convulsive ES.
Partial SE develops with continuously repeated high activity of the convulsive zone, and there is no convulsive readiness of the brain. Partial SE is not epileptic, but it is usually considered within the framework of epistatus.
The most life-threatening are tonic-clonic convulsions (tonic - tongue biting, jaw clenching, clonic - alternating contraction of muscle flexors and extensors). A seizure may begin with a strong scream, the jaws clenched (it is no longer possible to unclench them), the body bends in an arched manner, the limbs twitch, the patient hits his head on the surface on which he is lying, foam comes from the mouth, and blood may be released due to biting the tongue. The muscle contractions are so intense that arms or legs may be broken. The patient urinates on himself, possibly involuntary release of feces and vomiting. In the absence of consciousness, defensive reactions to bright light, loud sounds, and pain may persist.
Symptoms of status epilepticus
Between seizures, consciousness is not restored. The total duration of ES is 3–24 hours. During the first half hour of ES, compensatory mechanisms are activated. For the next half hour, the mechanisms are on the edge of what is possible. Duration of the status for more than an hour leads to irreversible consequences in the brain.
Complications of convulsive epilepsy, the development of which depends on the timeliness of care and treatment of status epilepticus:
- brain damage due to hypoxia and metabolic disorders;
- excitotoxicity (a pathological process in which nerve cells die under the influence of neurotransmitters - bioactive substances that carry out an electrical impulse);
- cerebral edema;
- intracranial hypertension;
- cerebral venous thrombosis;
- hemorrhagic stroke (hemorrhage) or ischemic stroke (necrosis);
- hyper- or hypotension, heart failure, cardiogenic shock, arrhythmia, cardiac arrest;
- respiratory failure and cessation;
- aspiration pneumonia, pulmonary hypertension, pulmonary edema, obstruction of bronchial branches due to hypersecretion;
- hyperpyrexia (febrile state);
- critical ischemia (damage to the peripheral arteries of the lower extremities);
- hyperhidrosis (excessive sweating);
- dehydration (dehydration);
- electrolyte imbalance;
- acute tubular necrosis in acute renal failure;
- acute liver failure;
- acute pancreatitis (inflammation of the pancreas);
- rhabdomyolysis (an extreme stage of myopathy in which muscle cells are destroyed);
- fractures;
- DIC syndrome (blood clotting disorder in small vessels with the formation of blood clots);
- secondary infections;
- skin damage.
With ES, multiple organ failure can develop - a stress reaction, a complex of failure of several systems, the terminal stage of the disease.
Treatment of seizure syndrome
Brief recommendations will help you react quickly if a person has a seizure disorder. Your actions are:
- Place the patient on a flat, non-hard surface if possible.
- Remove all sharp and hard objects from reach. This will help avoid injury due to uncontrolled limb movements.
- Unfasten or remove tight clothing that may impede breathing. If you're indoors, open the windows to let in fresh air.

First aid before doctors arrive is of great importance in this condition, and its absence can be fatal - Gently turn the victim's head to one side and hold it slightly to prevent the tongue from retracting and vomit from entering the respiratory tract.
- Remember that in no case should you hold the patient by force, you can only hold him a little, you should not try to open clenched jaws, and between the teeth (if they are not closed) place a non-solid object, for example, a tourniquet rolled up from fabric. In this condition, the victim’s muscles are very tense, and excess pressure can lead to a bone fracture.
- When the attack is over, do not leave the patient unobserved. Call an ambulance, briefly clarifying what happened to the victim.
Convulsive syndrome is the body’s reaction to external and internal stimuli, characterized by sudden attacks of involuntary muscle contractions
Convulsive syndrome in men, women and children is a nonspecific reaction of the body to internal and external stimuli. It is accompanied by involuntary contraction of muscle tissue.
The international classification of diseases includes convulsive syndrome. Its ICD-10 code is R56.8. This code is reserved for pathologies that do not relate to seizures of epilepsy or other etiology.
Convulsive syndrome often occurs in newborns. It affects adults of all ages. It is very important to find out the cause of the disorder in order to select an adequate course of therapy.
Reasons for violation
Convulsive syndrome is caused by various reasons. Quite often it develops due to congenital anomalies and pathologies of the central nervous system. Common factors also include genetic diseases, tumors in the body, and cardiovascular problems.
Common causes that lead to the appearance of the syndrome are presented in the table. They are divided by age groups.
| Age | Reasons for violation |
| Up to 10 years | Convulsions in childhood are caused by diseases of the central nervous system, fever, head injuries, congenital abnormalities in metabolism, cerebral palsy and epilepsy. |
| 11-25 years | The cause of the disease is head injuries, angioma, toxoplasmosis and neoplasms in the brain cavity. |
| 26-60 years | Pathology can be caused by neoplasms in the brain, inflammatory processes in the membranes of this organ, and abuse of alcoholic beverages. |
| From 61 years old | Seizures can be caused by kidney failure, drug overdose, Alzheimer's disease, and cerebrovascular disorders. |
Since convulsive syndrome in an adult or children has many causes, the methods of treating such a disorder differ. To achieve recovery, it is necessary to correctly determine the factor that led to the development of the disease.
Convulsive syndrome in children and adults has similar symptoms. Pathology appears suddenly.
A typical seizure is characterized by eye floaters, wandering eyes, and loss of contact with the outside world.
The tonic phase of the attack is characterized by short-term apnea and bradycardia. The clonic phase is characterized by twitching of facial areas on the face.
With alcoholic convulsive syndrome, which often occurs in adults and adolescents, severe intoxication, loss of consciousness, vomiting and foam from the mouth appear.
Convulsive syndrome in young children and adults is localized or generalized. In the first case, during an attack, individual muscle groups are involved. In the generalized course of the syndrome, the child may experience involuntary urination and loss of consciousness. Due to pathology, all muscle groups suffer.
Convulsions are characterized by an acute onset, agitation, and changes in consciousness
Spastic pathology, which is the state of convulsive syndrome, poses a danger to human health and life. If the attack is not suppressed in a timely manner and treatment of the disease is ignored, it will lead to dangerous consequences:
- Pulmonary edema, which threatens complete cessation of breathing.
- Cardiovascular pathologies that can lead to cardiac arrest.
Manifestations of an attack can overtake a person while he is performing actions that require maximum concentration of attention. We are talking about driving a vehicle. Even walking can cause serious injury if an adult or child is suddenly disturbed by the signs and symptoms of a seizure disorder.
To help the patient, it is necessary to urgently call an ambulance
Convulsive syndrome, which manifests itself in a child or an adult, cannot be ignored. Adequate treatment is required.
Before deciding on therapy, a specialist must find out the cause of the disease. It is for these purposes that diagnostics are used. The therapy offered by attending physicians is aimed at suppressing the symptoms of the pathological process and eliminating the negative factor that led to the development of the syndrome.
Urgent Care
First aid can be provided to a patient at the time of an attack by anyone. He must recognize the obvious symptoms of the disease and quickly respond to them. To avoid injury to the patient during seizures, it is necessary to act accurately and consistently.
First aid to a person with a convulsive syndrome helps him wait for the medical team to arrive and safely survive the painful condition. If infants, adolescents or adults experience symptoms characteristic of an attack, you should immediately call an ambulance. Next you need to do the following:
- It is necessary to provide the victim with access to fresh air. To do this, if possible, remove tight clothing or unbutton his shirt.
- It is necessary to place a small towel or scarf in the oral cavity so that the person does not accidentally bite his tongue or break his teeth.
- The patient's head should be turned to the side. The same must be done with his entire body. This action will prevent him from choking on vomit.
All these actions must be done very quickly. Afterwards, all that remains is to wait for the arrival of doctors who will help the person get rid of the attack.
Drugs
Taking sedatives helps the patient reduce the occurrence of seizures
Emergency care for a person with a seizure disorder may include taking medications. Drug therapy is aimed at eliminating the attack and further preventing this condition.
For convulsions, agitation and epileptic seizures, patients are prescribed GABA derivatives, barbiturates and benzodiazepines. Medicines help calm the nervous system and reduce muscle tone. For acute conditions, antipsychotics may be prescribed.
For cramps in the limbs, vitamin complexes can be prescribed. This therapy is effective if the attack is triggered by hypovitaminosis.
Providing assistance for convulsive syndrome includes the use of oral and external agents. For seizures, the following medications are recommended:
- Vitamins B and D.
- Magnistad.
- Magnerot.
It is strictly forbidden to give a baby or an adult medicine that has not been prescribed by a specialist. Medicines can be taken strictly on the recommendation of the attending physician. Otherwise, such therapy may lead to complications.
External remedies for the treatment of attacks include ointments. For leg cramps, it is customary to prescribe:
- Hermes.
- Troxevasin.
- Venitan.
Ointments and creams reduce the severity of seizures, stimulate blood circulation in the problem area and improve the saturation of tissues with nutrients.
Diet is of great importance in the treatment of convulsive syndrome. Patients are advised to adhere to a special diet that helps reduce the frequency of attacks to a minimum.
Patients with this diagnosis should exclude baked goods, carbonated drinks, sweets, strong coffee, alcohol and organ meats from their diet. If a person is overweight, then he needs to constantly monitor the number of calories consumed per day.
To cope with the painful condition, you need to include fresh vegetables and fruits, fermented milk products and whole grain cereals in your diet. It is imperative to monitor your drinking regime. Patients are recommended to drink 1.5-2 liters of clean water per day. Teas, compotes and drinks are not taken into account in this case.
If a person experiencing cramps is unable to create a menu for the week, he can seek help from a nutritionist. The doctor will select the optimal diet for the patient, which will allow the body to function normally.
Physiotherapy
Therapeutic exercises should be performed every day in conjunction with the prescribed treatment.
Therapeutic gymnastics helps to cope with convulsive syndrome. To achieve results from it, you need to practice regularly. Exercise therapy is also actively used in the prevention of attacks. Simple exercises will help you cope with the painful condition:
- Lifting small objects from the floor using only the toes.
- Rolling with your feet a rubber ball, which is equipped with spikes.
- Pulling your toes towards you while sitting with your legs extended.
Each exercise must be performed for 2-3 minutes. You can increase the duration of the training if the patient’s condition allows it.
If cramps bother you too often, the patient should take barefoot walks on sand or grass. If desired, you can use a special massage mat.
General information
Status epilepticus is a condition that can occur not only in patients with epilepsy, but also in other brain lesions (traumatic brain injury, intoxication, intracranial space-occupying formations, stroke, infections, hydrocephalus, etc.). Cases of status without a history of indications of epileptic paroxysms are approximately 50%. The incidence of epistatus does not exceed 20 cases per 100 thousand population. Young children are more likely to develop it, accounting for half of all cases. Among patients with epilepsy, status epilepticus is more often observed in children (10-25%), while among adult epileptics, status epilepticus is observed only in 5%. Status epilepticus is an urgent condition that can be encountered by specialists working in various fields of medicine: neurology, traumatology, oncology, resuscitation, narcology, psychiatry, and infectology.
Status epilepticus
Why is this condition dangerous?
Mortality in status epilepticus occurs in 5% of cases . For the symptomatic form, this figure corresponds to 30-50%. With the prolonged development of an emergency, the following consequences arise:
- Swelling of brain tissue.
- Oxygen starvation.
- Worsening blood pressure.
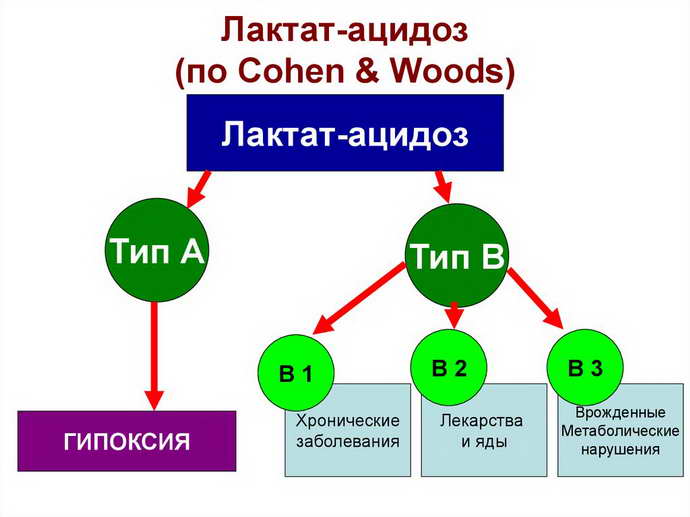
- Lactic acidosis, in which too much lactic acid accumulates.
- Electrolyte balance deteriorates.
- Mental retardation, problems with intellectual development, deterioration of mental functioning.
Classification
Status epilepticus is classified according to clinical forms (international classification):
- Generalized status: occurs with convulsions (tonic convulsions, clonic, tonic-clonic, myoclonic) and without convulsions (absence seizure).
- Partial: elementary type, dysphasic (with speech impairment), somato-motor.
- Partial complex.
- Unilateral.
- "Strange" (unclassified).
Traditional classification based on eclectic activity on EEG:
- Large (expanded) attacks.
- Peak-wave stupor: slow waves, peaks, spike-wave (peak) with a frequency of 3 in 1, small attacks, fleeting attacks, small long-term epiactivity, epileptic twilight (stupidity) of consciousness, low status.
- Focal motor epistatus: long-term epilepsy, focal (seizures are caused by electrical activity in a localized area of the brain), adverse (the head and torso are turned in any direction).
- State of twilight: prolonged stupor (lethargy), prolonged disorientation (loss of concept of space and time), temporolobar status, psychomotor status, persistent twilight.
- Hemiclonic status: hemiconvulsive (spastic), hemiplegic (with complete loss of mobility) epilepsy, large hemiconvulsions.
Classification depending on age:
- Neonatal status.
- ES of newborns.
- Status epilepticus in childhood: infantile seizures, febrile seizures (at high temperatures), seizures in myoclonic syndromes, partial episyndromes, status during slow-wave sleep, epileptic aphasia.
- In children and adults: tonic-clonic seizures, absence seizure, myoclonic ES in coma, specific types of intellectual retardation, non-convulsive form of simple partial seizures (when neurons are activated in a localized area of one hemisphere), ES of complex partial seizures (with impaired consciousness).
Classification by stages:
- Stage I - early status lasts 5-10 minutes.
- Stage II - extensive, duration 10–30 minutes.
- Stage III - refractory, duration 30–60 minutes.
- Stage IV - super refractory, lasting at least 24 hours.
By etiology:
- True status: for focal, generalized, symptomatic, idiopathic, cryptogenic epilepsy, including congenital malformations.
- Symptomatic status: with head injury, large brain tumors, inflammation of the brain and membranes, stroke, cicatricial adhesions, dysmetabolic disorders.
In medical practice, a simple classification is often used: convulsive ES (more common) and non-convulsive.
Causes
Let's list the provoking factors. Epilepsy, often a disorder caused by constant use of antiepileptic drugs, leads to this status. Skull injuries. Neoplasms of the nervous system. Inflammation of the brain and outer membranes. Problems with blood circulation in the head. Cicatricial spastic disorders of the liquorodynamic process. Dysmetabolic processes. Poisoning. Infectious processes and hyperthermia.

Status epilepticus occurs in 18-20 people out of 100,000. It is one of the most widespread neurological disorders. More often, epistatus manifests itself in newborns and elderly citizens. Approximately 5% of adults observed in epilepsy hospitals have encountered such symptoms at least once during the entire period of their struggle with the disease. When abnormal neuronal activity is localized in the frontal lobe, the largest number of status epilepticus is recorded.
Causes of status epilepticus
In half of the cases, status epilepticus occurs against the background of existing epilepsy. In such situations, the cause of the status, as a rule, is the abrupt withdrawal or irregularity of anticonvulsant (antiepileptic) therapy. The reason may be a relative reduction in the dose of the anticonvulsant used due to sudden weight gain or the occurrence of diseases with impaired intestinal absorption (malabsorption). Predisposing factors include: violation of the regime, somatic diseases, infections, pregnancy. Status epilepticus can occur as a manifestation of new-onset epilepsy.
Among the causes of symptomatic epistatus not associated with epilepsy are head injury, cerebrospinal fluid dynamics disorders (for example, occlusive hydrocephalus), brain tumors, cerebral cysts, hematomas, strokes, encephalitis, meningoencephalitis, infectious diseases occurring with severe hyperthermia and intoxication. This also includes poisoning and dysmetabolic disorders: acute renal failure and uremia, alcohol withdrawal syndrome, decompensated diabetes mellitus, hypothyroidism, hypoglycemia, porphyria, hyponatremia, eclampsia, lipoidosis, gangliosidosis. The status can be initiated by abrupt withdrawal of narcotic or sedative medications that have been taken by the patient for a long time. In young children, epistatus is possible as a consequence of brain developmental defects.
The pathogenetic substrate of status epilepticus is continuous or rapidly successive paroxysmal bioelectrical activity of cerebral neurons. It can cover different areas of the brain and have a variable degree of generalization. Epistatus, especially if it lasts for a long time, is an extremely dangerous condition, since it causes a number of pathological processes in the body: cerebral (brain hypoxia and neuronal death, cerebral edema), respiratory (hypoxia, aspiration pneumonia, airway obstruction, pulmonary edema), discirculatory (arterial hypertension or hypotension, arrhythmia, collapse), metabolic (acidosis, hypoglycemia, hypercapnia, hypoglucocorticemia), hemostatic (thrombosis, obligate DIC). The longer the duration of the status, the higher the likelihood of developing irreversible cerebral changes (death of some neurons) with the formation of a persistent neurological deficit.
Sources
- https://NeuroDoc.ru/bolezni/epilepsiya/epilepticheskij-status.html
- https://www.KrasotaiMedicina.ru/diseases/zabolevanija_neurology/status-epilepticus
- https://SimptoMer.ru/bolezni/nevrologiya/3457-epilepticheskij-status
- https://edemdarom.ru/lechenie-epilepsii/chto-delat-esli-u-moego-parnya-epilepsiya
[collapse]