Stroke is a very dangerous disease and is becoming more and more “youthful”: if previously it was mainly older people who suffered from it, now it is not uncommon for young people to be hospitalized with this diagnosis. This happens most often due to overwork.
But older people with chronic diseases still need to take special care - some contribute to stroke, and also make it more difficult to recover.
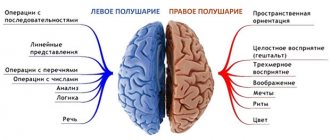
There are ischemic and hemorrhagic strokes. They differ in many respects and are treated differently, but it is not always easy to distinguish them - many of the symptoms are similar, because in both cases the problem is a violation of blood flow in the head, although its causes are different.
Ischemic and hemorrhagic stroke - differences
Ischemic stroke is an acute disorder of cerebral circulation that results in the death of a part of the brain.
This disease occupies a leading position among the causes of mortality and disability of the population. More often, the disease is diagnosed in men over 50 years of age who have bad habits. The prognosis of the disease ranges from complete recovery to death and depends on the location of the lesion and the timeliness of assistance. Ischemia is a deficiency of blood supply to a certain area of an organ or tissue.
A stroke is a disruption of blood flow to the brain.
Hemorrhagic stroke is an extremely dangerous disease, which is characterized by rupture of an artery with subsequent formation of a hematoma or penetration of brain tissue. After the first symptoms appear, the development of cell death occurs at lightning speed, so it is extremely important to provide assistance to the patient as quickly as possible, this can cost him not only the loss of health, but in most cases a person’s life is at stake. People over 40 years of age who have a history of diseases such as arterial hypertension, atherosclerosis, aneurysms, vasculitis and others are more susceptible to developing pathology.
The first significant difference between hemorrhagic and ischemic stroke is pathogenesis, so with a hemorrhagic stroke, a vessel ruptures with further hemorrhage, and with an ischemic stroke, there is a disruption in the flow of blood to a part of the brain.
Hemorrhagic and ischemic stroke also differ in the speed of development of pathology, the first is characterized by lightning-fast development. Cerebral ischemia is much more common and is different from cerebral hemorrhage.
Development mechanism
Translated, “hemorrhage” means hemorrhage. The pathogenesis of hemorrhagic stroke is based on a violation of the integrity of cerebral vessels with subsequent hemorrhage. In contrast, ischemic stroke occurs due to blockage of a blood vessel and cessation of blood circulation in its basin. In both cases, the delivery of oxygen and essential nutrients stops, and irreversible necrotic processes occur in the neurons. Outwardly, this manifests itself in a specific clinical picture.
Both pathologies arise due to pathologically altered blood vessels. The risk of developing the disease increases in the following situations:
- arterial hypertension;
- cerebral atherosclerosis;
- diabetes mellitus, impaired glucose tolerance;
- obesity;
- smoking, alcohol abuse;
- burdened heredity.
In addition, an ischemic attack can occur due to changes in the functioning of the blood coagulation system, a tendency to form blood clots, or a violation of the integrity of atherosclerotic plaques.
Hemorrhagic stroke occurs more often in patients with aneurysms - sac-like protrusions in the wall of the vessel. In rare cases, it is caused by hemophilia or an overdose of thrombolytics. As a rule, hemorrhage in the brain occurs at the height of a hypertensive crisis. In contrast, ischemic stroke can occur even with normal blood pressure.
There is also an age difference - hemorrhages are more common in young and middle-aged people, mainly in men. Ischemic stroke predominates in patients over 60 years of age and occurs equally often in men and women.
Causes of the disease
Causes of ischemic stroke
Development of ischemic stroke
The causes of ischemic stroke are divided into:
Cardioembolic - occurs as a result of blockage of the artery lumen by an embolus. A common cause of blockage is emboli that occur due to heart defects, endocarditis, and other heart pathologies accompanied by the formation of blood clots. A common cause is atrial fibrillation.
Atherothrombotic - usually manifests itself as a consequence of atherosclerosis of large and medium arteries. The plaque narrows the lumen of the vessel and is a catalyst for the formation of a blood clot. This type develops gradually and often culminates during sleep. Often the harbinger is a transient ischemic attack.
Hemodynamic – caused by a change in the normal speed of blood movement through the vessels. The onset of the hemodynamic type of the disease can be different and manifest itself both during sleep and during wakefulness.
Lacunar – damage to the small vessels of the brain. A common cause is prolonged high blood pressure.
Rheological - occurs due to changes in the properties of blood. Thrombophilia, leukemia, erythrocytosis, erythremia can lead to a rheological type of disease.
Causes of hemorrhagic stroke
- Most often develops against the background of hypertension of 2 and 3 degrees. If a patient with hypertension has endocrine pathologies in the form of a pituitary adenoma, changes in the thyroid gland, then the possibility of the disease doubles.
- Aneurysm rupture.
- Pathological processes of connective tissue, during which a violation of the elasticity and strength of blood vessels occurs.
- Hemophilia.
- Overweight.
- Bad habits.
- Changes in lipid metabolism.
- Diabetes.
- Heart diseases.
- Depressive states.
Based on the above reasons, it is clear that the difference between hemorrhagic and ischemic stroke is that most often ischemic stroke is caused by diseases accompanied by the formation of emboli and blood clots, and in hemorrhagic stroke, the main catalyst is a history of hypertension.
Stroke is a sudden disruption of blood circulation in the brain, blockage or rupture of a cerebral vessel. When a blood vessel is blocked, an ischemic stroke occurs, and when a blood vessel ruptures, a hemorrhagic stroke occurs. It is considered to be the most common brain disease in the adult population. Moreover, with age, the risk of stroke increases significantly. According to statistics, stroke affects 0.1 - 0.4% of the population per year, depending on the country of residence. Stroke is the leading cause of human disability and ranks third among the causes of mortality.
Contents: 1. Classification 2. Ischemic 3. Hemorrhagic 4. Extensive 5. Lacunar 6. Spinal 7. Acute 8. Micro 9. Repeated 10. Precursors 11. Degrees
You can often hear about various brain diseases. You can read about them in newspapers, hear on TV and even on the playground in your own yard. Common diseases such as heart attack and stroke spare no one. They hit you right in the head. And quite often very cruelly. In this article I would like to talk about stroke, namely, what types this disease is divided into.
So, let's begin. What is a stroke? As you already know, this is a brain disease. A stroke is the result of a blockage or rupture of a blood vessel in the brain. Most often, rupture of this vessel leads to hemorrhage in the lining of the brain. There are two types of stroke. One of them is hemorrhagic stroke, and the other is ischemic.
Let's talk first about hemorrhagic stroke. This type of stroke occurs due to the rupture of a blood vessel and its hemorrhage into the meninges. During such a stroke, blood under high pressure displaces brain tissue to the sides and fills the resulting void. This process leads to the appearance of a blood tumor in the brain. Doctors call this tumor an intracerebral hematoma.
There is another type of hemorrhagic stroke. It happens as follows. A person feels a blow of enormous force to the head. He starts having convulsions and has a very bad headache. At this moment, the aneurysm ruptures on the wall of the vessel. An aneurysm resembles a saccular formation located in the lining of the brain. A person with such a stroke constantly groans in pain, feels sick, and quite often loses consciousness. Despite this, this subtype of hemorrhagic stroke is easier, since the patient does not have paralysis.
With a hemorrhagic stroke, which occurs in the brain stem, a person does not live more than 48 hours. He dies without ever regaining consciousness.
Let's move on to ischemic stroke. This type of stroke occurs due to blockage of blood vessels in the brain. The causes of blockage are blood clots that form in areas of narrowing of blood vessels or pieces of plaque that appear as a result of separation from large vessels. Prolonged vascular spasms can also cause blockage.
Ischemic stroke is much more complex than hemorrhagic stroke. The reason for its complexity is the gradual impact on the human brain. First, the patient begins to have a headache. However, the pain is not very severe. Gradually the pain intensifies, the person loses consciousness and vomits. At the same time, his face becomes red and his breathing becomes hoarse. After a short period of time, the patient begins to become cowardly, his head, arms and legs refuse to work.
The scary thing is that after a few minutes the person almost completely comes to his senses. When the doctors arrive, he is already able to speak normally. The bad thing is that this condition is repeated several times. When a person wakes up in the morning, he may be half paralyzed.
Most often, these two types of stroke are the result of hypertension, various heart diseases, heart failure or cerebral atherosclerosis.
If you notice signs of a stroke in someone close to you or strangers, immediately place the person on a bed or on the ground and try to provide him with sufficient air flow. The patient's head should be raised at all times. It is also necessary to remove vomit from his mouth. Monitor the patient's condition until the ambulance arrives.
A stroke is a very dangerous disease, during which a person must be under the close attention of another person. Otherwise, a stroke attack can lead to the death of the patient.
What are the causes of epilepsy Diagnosis of cerebral aneurysm follow the link
Menu for cerebral stroke
Classification
There are several classifications of strokes, depending on the aspect that is chosen as a criterion. In the classification of strokes according to the pathomechanism that causes damage to brain tissue, the following types are distinguished:
1) atherothrombatic (85-90%):
- a. cardioembolic,
- b. lacunar,
- c. hemodynamic - as a result of a decrease in blood pressure and a critical decrease in local cerebral blood flow (without obstructions in the vessels).
2) hemorrhagic strokes (10-15%) - intracerebral hemorrhage. If we divide strokes taking into account their dynamics, we can distinguish:
- Transient ischemic attack (TIA) – symptoms disappear within 24 hours.
- Minor stroke (RIND) – symptoms disappear within 3 weeks.
- Completed stroke (CS) – symptoms remain constant or the strength is only partially reduced.
- Progressive stroke (PS) - symptoms appear suddenly and then intensify, gradually or in the form of another exacerbation.
- Strokes in the area of the blood supply to the cervical artery are observed in 85% of patients, and in the areas of blood supply to the vertebral arteries - in 15%.
Ischemic
This type of stroke is also called cerebral infarction. This disease most often occurs in people over 50-60 years of age. Ischemic stroke is more common than other types and occurs in 80% of cases.
The causes of ischemic stroke are associated with impaired blood flow through the arteries responsible for delivering oxygen to brain cells, the walls of which become narrowed or blocked. Ischemic stroke is caused by embolism (a pathology associated with blockage of blood vessels by dense accumulations of blood particles) or thrombosis of both extracranial and intracranial cerebral arteries.
A stroke caused by thrombosis usually occurs at night as a result of atherosclerosis of the cerebral arteries. In cases where the culprit of cerebrovascular accident is an embolism, the likelihood of a recurrent stroke is high. This is because blood clots that form in the heart as a result of irregular contractions can be transported through the cardiovascular system and clog small vessels in the brain that are responsible for feeding certain areas of the brain, resulting in necrosis (infarction) of this area of the brain.
Ischemic cerebral stroke is the most common form of stroke. According to various sources, up to 80% of all strokes are ischemic. AI has another name - cerebral infarction, that is, a focus of necrosis formed on the periphery of the area where blood flow is delayed. Necrosis in IS is the result of metabolic disorders in brain cells with phenomena of stagnation of blood in a region of nervous tissue. Causes of blood stagnation in the blood vessels of neuronal and glial brain tissues:
- stenosis (narrowing) or occlusion (blockage) of large arterial vessels of the brain;
- thrombosis - blockage of an arterial vessel with a thrombus (thrombus - a clot of blood cells);
- embolism - blockage of an arterial vessel by an embolus (an embolus is a clot of various cells that are not normally present in the bloodstream).
Hemorrhagic
Hemorrhagic stroke most often occurs after increased physical and emotional stress. If at the end of a busy day you feel severe headaches, your surroundings take on a reddish tint, and nausea creeps into your throat, you should immediately contact a medical specialist. Remember: symptoms can develop rapidly and lead to a stroke in a short time!
Orientation is lost, speech and sensitivity are distorted, the pulse becomes rare and intense, the temperature and pressure rise sharply, sweat appears on the forehead, a state of mild stupor appears, which can develop into a sudden loss of consciousness, even into a coma, suddenly a person feels a blow inside the head, loses consciousness and falls - this is a stroke itself. All blood pressure escapes through the ruptured vessel into the brain tissue. Just a few minutes is enough for blood to saturate a large area and lead to swelling or even death.
From the outside, a stroke can be identified by the following manifestations.
- Loud breathing with hoarseness
- Increased pulsation of cervical vessels
- Often, the eyeballs involuntarily deviate towards the lesion or, less commonly, in the opposite direction
- Vomiting may occur
- On the opposite side of the lesion, paralysis of the limbs is possible
- If extensive hemorrhage occurs, it is accompanied by involuntary movement of healthy limbs.
Extensive
Major stroke is a general term for massive strokes. In accordance with the classification of acute cerebral ischemia (E.I. Gusev, 1962) it corresponds to the signs of a severe stroke with pronounced:
- general cerebral symptoms:
- depression of consciousness;
- cerebral edema.
- focal symptoms:
- hemiparesis or hemiplegia on the side opposite to the lesion;
- paresis of gaze towards the paralyzed limbs;
- disorder of consciousness in the form of hemispheric damage (aphasia - speech disorder, heminopsia - loss of half the visual field, anosognosia - the patient does not understand his condition)
- autonomic disorders – a disorder of the nervous regulation of internal organs and systems of the body.
- trophic disorders - disturbances in nerve conduction, manifested by skin ulcers.
Massive strokes are complicated by secondary type brainstem syndrome in the form of impaired consciousness and oculomotor disorders:
- anisocoria – change in pupil size, enlarged on the side of the affected hemisphere;
- ophthalmoplegia – weakened or absent pupillary response to light;
- strabismus and strobism (pendulum-like movements of the eyeballs);
- hormetonia - generalized disorders in the form of muscle spasms of tonic muscles;
- decerebrate rigidity – increased tone of the extensor muscles,
By localization, extensive strokes correspond to lesions in the basins of large precerebral and cerebral main arteries (classification by E.V. Schmidt, 1985 and ICD-10).
No information was found comparing the incidence of major strokes in men or women. Major strokes are a common cause of death or long-term (lifelong) disability.
Lacunar
Lacunar stroke is a type of ischemic infarction (stroke) of the brain. LI is characterized by a limited lesion resulting from damage to one of the small perforating arteries. Perforating arteries are small vessels, ranging in size from lobes to 2 mm, up to 10 cm long, connecting larger deep and superficial arteries. The name was received in connection with the formation at the site of a heart attack of cavities (lacunae) of a round shape (less than 1.5 cm in diameter), filled with liquid contents - cerebrospinal fluid.
The incidence (occurrence) of LI is on average 20% of other ischemic strokes. Lacunar infarctions are not characterized by cerebral and meningeal symptoms. Characterized by focal symptoms:
- ataxic hemiparesis – impaired coordination of half the body;
- dysarthria – impairment of clear pronunciation of words;
- monoparesis - impairment of motor activity of one arm or leg.
Of the group of patients diagnosed with lacunar stroke, approximately 54% are women and 46% are men. The average age of patients diagnosed with LI ranges from 48 to 73 years.
The most common cause of lacunar stroke is atherosclerosis due to arterial hypertension. In some cases, an embolic cause of LI has been proven, which is more severe for patients due to the involvement of a larger area of the brain in the pathogenesis after blockage of a vessel by an embolus. The prognosis for the outcome of lacunar stroke depends on the location of the lesion and the time of initiation of treatment.
Spinal
Spinal stroke is an acute circulatory disorder in the spinal cord. The causes of spinal stroke can be ischemic or hemorrhagic stroke. The location of the spinal stroke is in the large arteries of the cervical and lumbar enlargement or small branches of the reticulo-medullary arteries.
It occurs more often in older and older people. The specific features of spinal strokes in men and women have not been identified.
There are no exact data on the prevalence of spinal strokes. This is probably due to the difficulty of differential diagnosis. More accurate diagnosis became possible after the widespread introduction of CT, MRI, and selective spinal angiography.
Some sources indicate the following precursors of spinal stroke:
- radicular syndrome – pain of different localization (neck, arms, legs, lower back);
- chronic cerebrovascular insufficiency (CSCI):
- periodic headaches,
- noise and heaviness in the head;
- short-term dizziness;
- increased fatigue and sleep disturbance;
- memory loss
- myelogenous intermittent claudication syndrome - a feeling of numbness in the legs during prolonged walking and rapid disappearance after rest, there is no pain in the legs.
The clinical picture is varied and depends on the location of the stroke in the spinal column.
Ten spinal ischemic syndromes:
- ventral half of the spinal cord or blockage of the anterior spinal artery or Preobrazhensky syndrome;
- anterior poliomyelopathy;
- Brown-Sequard;
- centromedullary stenosis;
- marginal zone of the anterior and lateral cords
- amyotrophic lateral sclerosis
- dorsal part of the diameter of the spinal cord (Williamson syndrome)
- diameter of the spinal cord
- occlusion of the artery of the cervical thickening
- turning off the artery of the lumbar enlargement.
Diagnosis and differential diagnosis using instrumental methods.
Spicy
This is the initial period of stroke development. It lasts on average twenty-one days, sometimes less. During this period, an increase in pathogenetic processes in brain tissue occurs, especially intense during the first six hours of the disease.
There are stages:
- formation of a nucleus from damaged brain cells – 5-8 minutes;
- enlargement of the penumbra (the area of metabolic changes around the core of the cerebral infarction):
- by 50% within 1 hour 30 minutes;
- by 80% within 6 hours.
Six hours is the “therapeutic window” time when therapeutic measures can be carried out with maximum effect. From the first minutes, a pathogenetic cascade is activated, which at the cellular level begins with the cessation of blood flow and ends with apoptosis (death) of the brain cell. Without treatment, cell apoptosis increases exponentially. On days 3-5, damaged brain cells undergo necrosis, and partial localization of the process occurs.
Next, the formation and/or increase of neurological disorders occurs in the form of general cerebral and focal symptoms.
Intensive therapy during the “therapeutic window” includes:
- improvement of hemodynamics of brain tissue due to drip administration of physiological solutions.
- neuroprotection (protection) of brain cells.
- improvement of rheological (viscosity) and coagulation (clotting) properties of blood.
- improvement of blood microcirculation.
- prevention of cerebral edema.
Micro
It is also called a minor stroke (Micro stroke). The name is given because of the relatively rapid (2-21 days) disappearance of symptoms of neurological deficit.
Neurological deficit syndrome: two or three or more of the following symptoms:
- unsteady gait
- muscle hypertonicity,
- mono-or hemiparesis,
- paralysis of the gaze or head,
- aphasia/anosmia
- seizures/epilepsy,
- causeless joy/rage
With a minor stroke, foci of cell necrosis form and persist in the brain. The symptoms of MI are similar to transient ischemic attacks (TIA).
The fundamental difference between a stroke and transient ischemic attacks is that with TIA:
- there are symptoms of neurological deficit;
- CT/MRI does not detect a focus of necrosis (ischemia) in the brain.
The development of minor stroke is observed in the age group from 25 to 45 years. Gender correlation has not been established.
The causes of a micro stroke are a combination of several of the following factors:
- arterial hypertension;
- regular use of oral contraceptives/other drugs that increase blood viscosity;
- venous thrombosis;
- systemic blood diseases;
- migraine;
- drugs, alcohol;
- head and neck injuries.
Microstroke is a risk factor for developing one of the types of completed stroke. Frequently recurring MI is a consequence of decreased intelligence and dementia.
Repeated
The main cause of recurrent strokes is previous cerebrovascular diseases (CVD). It should be considered that CVD means strokes and TIAs. During the first year, people who have suffered major strokes may develop:
- recurrent strokes;
- dementia disorders (acquired decrease in intelligence to varying degrees);
- lethal complications.
Impact on risk factors is a real chance of preventing recurrent strokes. Prevention must be consistent and continuous.
The standard algorithm for influencing risk factors in the secondary prevention of stroke is designated A-B-C therapy (A - antihypertensives, B - blockers, C - statins), namely the use for the prevention of recurrent strokes:
- antihypertensive drugs (Micardis, Agrenox and others);
- thrombus blockers (aspirin, warfarin, agrenox, clopidogrel and others),
- statins (counteracting the formation of cholesterol), drugs from the statin group are used to block the enzyme (HGM-CoA) involved in the production of cholesterol (lovostatin, fluvastatin, atorvastatin, rosuvastatin and others).
Harbingers
A small stroke can be a harbinger of circulatory disorders in the vessels of the brain. It occurs days, weeks or months before extensive brain damage occurs. With a minor stroke, brain function is suspended for a short time - only 15 minutes, and then completely restored. The symptoms are very similar to those of a real stroke, but the body can still cope with the circulatory disorder on its own. If this has already happened, you should not hesitate to seek medical help.
In the vast majority of cases, the disease occurs against the background of certain diseases:
- Arterial hypertension;
- Heart diseases;
- Atherosclerosis;
- Diabetes;
- Aneurysms on the cerebral arteries and arteries in the neck;
- Vasculitis;
- Thrombocytosis, erythremia.
Degrees
Periods of stroke:
- Acute stroke.
- Acute stroke.
- Early recovery period of stroke.
- Late recovery period of stroke.
- Period of complications and consequences of stroke.
- Residual period (long-term consequences of stroke).
Stroke severity:
- Minor stroke - the patient develops neurological disorders, while many symptoms may be erased and not noticed, or be classified as other diseases. Symptoms of a minor stroke usually resolve within 21 days.
- Stroke of mild to moderate severity - the patient experiences focal symptoms. There are no signs of impaired consciousness or cerebral edema.
- Severe stroke – the patient is most often unconscious, and neurological disorders rapidly progress. There are signs of cerebral edema. This degree of stroke most often leads to the death of the patient.
The dynamics of the development of neurological symptoms during stroke divides the disease into the following types:
Stroke in development, or stroke in progress. In this case, there is a progression, an increase in neurological disorders, and a deterioration in the patient’s condition. The stroke is complete. The patient's condition stabilizes, there is no progression of neurological disorders and even regression of disorders, and improvement in well-being.
Clinical picture
Symptoms of ischemic stroke
Ischemic stroke - symptoms
Symptoms of manifestation are very diverse and depend on the part of the brain in which ischemia occurred.
- Impaired consciousness;
- Strong headache;
- Nausea;
- Vomit;
- Increased sweating;
- Dry mouth;
- Gait disturbance;
- Visual disturbances in the form of double vision, decreased vision;
- Changes in hearing up to complete deafness;
- Dysarthria, aphasia;
- Memory loss.
Symptoms of hemorrhagic stroke
Hemorrhagic stroke - symptoms
Hemorrhage occurs with severe consequences and death occurs in 50–90%. It develops very quickly and the first harbinger of an upcoming brain catastrophe is a headache, a feeling of fullness in the head, vomiting, and impaired consciousness. After a few minutes, paresis and loss of consciousness may occur. The time during which medical workers can provide assistance and prevent the death of a patient is very short and ranges from 3 minutes to several hours.
- Confusion and loss of consciousness;
- Weakness;
- Vomit;
- Headache;
- Hemodynamic disorders.
- Paresis, paralysis of the limbs, a certain side of the body, facial muscles;
- When the left temporal lobe is damaged, speech impairment occurs;
- Visual and hearing disorders.
Hemorrhagic and ischemic stroke have fairly similar symptoms, the difference between them is that in the hemorrhagic form of the disease the symptoms are more pronounced and the patient’s condition is assessed more severely.
Symptoms
Following the warning signs, the first symptoms appear. Feeling can deteriorate very quickly after this, so the speed of response is one of the main factors that can ensure survival.
The first symptoms may appear several hours before an ischemic stroke: weakness, headaches and dizziness, fainting. Limbs may be lost on one side or vision may be impaired - in some cases only affecting one eye.
Other signs that can help identify ischemic stroke:
- the patient perceives reality incorrectly;
- his speech becomes unclear;
- pulse quickens;
- the pressure rises and falls;
- auditory perception deteriorates;
- he has difficulty swallowing;
- there is noise in the head;
- movements are not coordinated;
- nausea;
- heat;
- the face is distorted;
- pain appears that a person has not experienced before, for example, the chest or half of the face begins to ache.
The following symptoms indicate a hemorrhagic stroke:
- the head begins to hurt very badly;
- arrhythmia or tachycardia occurs;
- pressure rises;
- breathing becomes loud and hoarse;
- the patient may faint;
- photosensitivity increases;
- the face becomes asymmetrical, turns red or pale;
- convulsions begin;
- the gaze loses its meaning;
- nausea or even vomiting begins;
- limbs or the whole body are paralyzed;
- bowel movements involuntarily.
Ischemic and hemorrhagic stroke - treatment methods
Treatment of hemorrhagic stroke consists of strict bed rest, neurosurgical intervention, and antibacterial therapy (in case of traumatic brain injury). Most often, this type of disease is treated with surgical treatment; in some cases, the disease is treated conservatively.
The differences in the treatment of ischemic and hemorrhagic stroke lie in the treatment methods. When a cerebral hemorrhage occurs, in most cases, specialists resort to surgical intervention; cerebral ischemia is most often treated with conservative methods.
Repeated stroke
After an attack, there is a risk of relapse, so it is important to actively carry out prevention. It consists of regularly taking medications prescribed by a doctor: antihypertensives, statins, and anti-thrombosis.
Mostly recurrent stroke develops within a year after the first episode.
It is more difficult to treat, and the dynamics of recovery slow down significantly. Repeated pathology often provokes loss of intellectual and motor abilities and can cause the death of the patient.
Prognosis for patients
Ischemic and hemorrhagic stroke occupy leading positions in disability and mortality of the population. An important fact influencing the prognosis of the disease is the presence of concomitant pathologies. Up to 25% of people die in the first month after a cerebral infarction, 30% of people remain disabled. Only 25% of people who have suffered ischemia live more than 10 years.
The prognosis for hemorrhagic stroke is unfavorable, with death occurring in 60–70% of cases. The fate of a person is decided the first day after a hemorrhage; they are considered critical. The most significant difference between ischemic and hemorrhagic stroke is the survival rate. So, with a cerebral infarction, the survival rate is much higher than with a cerebral hemorrhage.
Spinal stroke
A rare disease is a violation of the blood supply to the spinal cord (1% of the total number of strokes). With pathology, blood flow through the spinal arteries stops or worsens.
The reasons are:
- atherosclerotic changes;
- physical impact (injury, surgery);
- embolism.
Spinal stroke is differentiated into ischemic and hemorrhagic. The second is rare, but requires emergency care. Often the hemorrhagic type is diagnosed already when hematomas form. Given their large size, it is extremely rare to achieve complete recovery.
Symptoms depend on the affected area, but paralysis of the legs or arms almost always occurs. There is loss of sensitivity, memory, pain in the head, muscle weakness, drooping head, urinary and fecal incontinence.
With the spinal form, the recovery period is long, and the disease often leads to irreversible consequences.
What is the difference between ischemic and hemorrhagic stroke? Which type of attack is more dangerous?

Hemorrhagic and ischemic strokes without proper medical care can cause the development of dangerous complications. That is why it is so important to be able to recognize the symptoms of these pathologies and the principles of their treatment.
The article will discuss the differences between these concepts, as well as which type of stroke is more dangerous for human health and life.
Causes and risk factors
The following reasons lead to the development of stroke:
- cardiovascular diseases (atherosclerosis, arterial hypertension);
- pathology of cerebral vessels (fibromuscular dysplasia, Moyamoya disease, cerebral arteritis, arteriovenous malformations, rupture of intracranial aneurysm);
- migraine with the presence of severe neurological deficit;
- traumatic injuries to the extracranial parts of the vertebral or carotid arteries with subsequent occlusion by an embolus or thrombus;
- systemic connective tissue lesions;
- homocystinuria;
- sickle cell anemia;
- thrombosis of the venous sinuses;
- leukemia.
Factors that increase the risk of stroke include:
- atrial fibrillation;
- arterial hypertension (high blood pressure);
- myxomatous degeneration of the mitral valve;
- smoking;
- hyperlipidemia.
How are these types different?
Reasons for development
Most often it develops:
- in the presence of hypertension of the second or third degree;
- due to a ruptured aneurysm;
- as a result of the proliferation of connective tissue, which impairs the strength of blood vessels;
- due to excess weight, bad habits, diabetes.

The main cause of ischemic stroke is insufficient oxygen supply to the brain. This condition occurs when:
- blood composition disorders;
- blockage of blood vessels or their damage;
- violation of the blood flow pattern.
Ischemic stroke can also develop as a result of atherosclerosis.
At-risk groups
Risk factors for developing ischemic stroke include:
- high blood pressure;
- heart diseases;
- diabetes;
- high blood cholesterol levels;
- congenital or acquired changes in the arteries;
- heredity (in the presence of strokes, heart attacks, arterial hypertension in relatives);
- bad habits, stress.
Provoking factors for the development of hemorrhagic stroke include:
- vasculitis;
- blood diseases;
- smoking, taking toxic substances;
- physical stress;
- chronic vascular pathologies;
- heart failure;
- poor nutrition;
- adherence to bad habits;
- regular stress;
- brain injuries;
- diabetes.
Course of the disease

The victim falls, losing consciousness, and a seizure may occur: convulsions, difficulty breathing, foaming at the mouth. The course of the disease in ischemic stroke is slower and smoother, while the symptoms of the disease can appear and disappear quickly. Sudden onset of symptoms is usually caused by vascular embolism (blockage of the aorta).
Symptoms
Let's consider how you can distinguish these two types of pathology by symptoms.
The main signs of hemorrhagic stroke:
- severe headaches;
- the appearance of vomiting and nausea;
- feeling of stupor, coma - in severe cases;
- memory impairment;
- speech disorders;
- convulsions.
If a person has an ischemic stroke, the following symptoms may indicate this:
- speech problems;
- drooping corners of the lips;
- facial asymmetry;
- loss of sensation;
- problems understanding other people's speech;
- nausea and vomiting;
- blindness, flashes before the eyes.
It is important to know not only the first symptoms of an ischemic stroke, but also the rules of first aid when it occurs.
Treatment methods

Treatment of ischemic stroke involves the use of drugs:
- to thin the blood;
- nootropics;
- calcium antagonists.
In the first 6 hours after an attack, thrombolytic treatment is considered the most effective: the administration of drugs that dissolve blood clots and normalize blood circulation in the brain. If the lumen of the carotid arteries is narrowed, surgical intervention may be prescribed.
Treatment of the gemmarogic form is aimed at stopping bleeding and stabilizing the functioning of all systems and organs. To do this, they prescribe (depending on the patient’s condition):
- cardiotonics;
- drugs to eliminate hyperemia;
- medications to lower blood pressure;
- antagonists;
- plasma substitutes.
In case of extensive hemorrhage, surgical intervention is prescribed to eliminate the resulting hematoma.
Rehabilitation period
Rehabilitation measures for stroke are prescribed after acute symptoms have been eliminated and the patient’s condition has stabilized.
Prevention
To never have a stroke, you need to take care of your health. To prevent it you need:
- to refuse from bad habits;
- eat right, in particular, do not eat fatty foods;
- watch your weight and do exercises.
Nothing complicated, but if you systematically follow these recommendations year after year - preferably from a very young age, the risk of not only a stroke, but also the occurrence of many other diseases will significantly decrease. A healthy lifestyle not only significantly prolongs it, but also allows you to stay in good shape for many years.
It is worth emphasizing several important nuances. The fight against excess weight is very important: every kilogram in excess of the norm leads to stress on the heart and blood vessels, and to the development of related diseases. Eating vegetables and fruits will help make blood vessels more elastic and get rid of high blood pressure.
Among physical activities, aerobic training is especially useful: swimming, cycling, running and walking. They will also help you get rid of excess weight. You need to exercise at least half an hour a day, but if your physical condition is advanced, you should first consult a doctor and monitor your blood pressure.
Interestingly, quitting drinking completely is not necessary. Of course, you should not abuse it, but small portions of alcohol can even be useful in preventing stroke, as they prevent the formation of blood clots. The daily portion is 17 ml of pure alcohol - this is, for example, about 150 ml of wine.
But in case of chronic diseases, drinking alcohol even in such moderate quantities should be discussed with your doctor.
Diagnostic methods

The main diagnostic methods include:
- MRI of the brain;
- performing spiral CT.
With their help, you can study the changes that have occurred that are characteristic of a certain type of pathology.
To determine the hemorrhagic type, CBC is used. With this pathology, an increase in the Krebs index is observed.
Table for a better understanding of the differences in stroke diagnostic methods:
| Diagnostic method | Stroke | |
| Hemorrhagic | Ischemic | |
| ECG | Indicates hypertrophy of the heart. | Allows you to identify changes in the myocardium and heart rhythm disturbances. |
| Fundus examination | The method is aimed at studying vascular damage and hemorrhage. | Indicates vasculitis, atherosclerosis. |
| MRI | Allows you to detect images of hemorrhage, hematomas, and cerebral edema. | The diagnostic method allows you to obtain images of infarct areas and identify signs of edema. |
| ECHO-encephaloscopy | The method provides information about the presence of edema and hematomas. | Allows you to detect interhemispheric asymmetry. |
Risk area
At risk of ischemia are people suffering from diabetes mellitus, hypertension, people with cardiac arrhythmias, low blood clotting and those with a hereditary predisposition. Overweight patients are also at risk. The last reason has become the most common in modern society.
In this case, the main risk group also includes hypertensive patients and obese people. This type of stroke affects people with congenital vascular pathology. Severe intoxication of the body can also cause the development of hemorrhagic stroke, as well as vitamin deficiency, vascular aneurysms and other inflammatory processes.
Bad habits such as smoking and alcohol also contribute to the development of stroke.