Brain tumors include all neoplasms localized in the central spinal canal and inside the skull. The development of brain tumors is associated with uncontrolled cell division, their classification depends on factors such as the primary factor and cellular composition.
A brain tumor can be benign or malignant. In addition, all brain tumors are classified according to certain criteria:
- by occurrence;
- by histological type;
- by localization;
- according to Smirnov.
Oncologists, neurosurgeons and radiologists at the Yusupov Hospital Oncology Center, when choosing an effective method for treating brain tumors, take into account not only the location and type of tumor, its features, the general condition and age of the patient, but also the likelihood of developing intraoperative and postoperative complications. The most advanced methods are used to treat brain cancer, providing maximum results.
Causes of symptoms
How to accurately and timely detect a brain tumor? This problem can be solved by relying on modern diagnostic methods that will identify the sources causing the symptoms. It could be:
- A tumor or inflammatory processes associated with its growth and penetration into other parts of the brain, which have the effect of pressing on its elements and preventing their normal functioning;
- Swelling of the tumor and the occurrence of inflammatory processes around the tumor;
- The manifestation of similar symptoms of primary brain cancer or metastatic, the most commonly observed type of tumor.
The appearance of symptoms depends on which area of the brain the disease begins to grow; sometimes they do not appear at all for a very long time inside the skull.
Duration of rehabilitation
Many people wonder how long it takes to recover. Unfortunately, no doctor can accurately answer this question. It all depends on the functions that were disrupted by the neoplasm and the procedures that will be performed.
For example, if the patient has impaired motor activity, then hand and foot massage, physiotherapy, and exercise therapy are performed.
If there are problems with the hearing aid, the patient needs to work with an audiologist. He also needs to take medications that improve communication between neurons in the brain.
Manifestation and development of tumors
How to identify the first signs of this terrible disease. The reason to contact a medical center is the appearance of the following symptoms:
- Headaches, mainly accompanying the development of a tumor inside the skull. Sometimes, besides this symptom, there is no other evidence of the disease. How to recognize a brain tumor if the nature of the pain is manifested by internal pressure bursting the skull, with a pressing sensation in the eye area? As a rule, in the presence of a tumor, such localization of pain is not observed, except in cases of focal neoplasms. Initially, the headache occurs at certain intervals and disappears with the use of painkillers. Over time, the pain becomes more severe and resistant to the effects of drugs aimed at reducing it. The nature of the pain can acquire varying degrees of strength during the day. Most often, patients experience severe pain in the morning, since the natural outflow of blood during sleep is hampered by the presence of a tumor. How to identify a brain tumor and distinguish it from ordinary poisoning? It will allow the use of a simple technique - changing the position of the human body. The vertical position of a waking person is accompanied by an outflow of cerebrospinal fluid and blood from the skull, which is accompanied by a decrease in intracranial pressure in general and headaches decrease;
- Symptoms of brain tumor disorders include nausea and vomiting. These symptoms are not related to food intake; they may appear early in the day, before meals. Nausea and vomiting characteristic of poisoning are usually accompanied by upset stool and abdominal pain, which is impossible with cerebral spasms.
Psychological state of a woman
When patients are diagnosed with cancer, it negatively affects the psyche of each of them. All people are aware that the presence of a malignant neoplasm often leads to death. The body is difficult to tolerate treatment. Not all municipal clinics do all tests and procedures for free. The patient may not have the resources for the necessary treatment.
Oncologists recommend that in addition to therapy for the underlying pathology, you should consult a psychotherapist. This is associated with a high suicide rate after diagnosis. He conducts sessions, discusses the problem, prescribes antidepressants.
Explains that not every case of malignant neoplasm leads to death.
A timely visit to a psychotherapist will help not only the woman, but also her relatives, cope and accept the emerging illness.
If the patient’s mental state is severe, this negatively affects the signs of the underlying disease. Neurological symptoms worsen. This is associated with constant depression, depression, and nervous disorders. Headaches, nausea, and seizures increase. She is in a state of panic. Timely control of this condition will help improve your well-being.
Focal tumors
Focal growths may also be accompanied by nausea and vomiting, which can be alleviated to some extent by changing head position. Such manifestations are accompanied by vegetative responses from the body: unexpected sweating, respiratory rhythm disturbances, hiccups, changes in skin color, and loss of consciousness.
- Increased pressure inside the skull may be accompanied by dizziness. Neoplasms inside the brain compress the vessels of the circulatory system of the head. The symptom does not have any specific features, but this sign should not be overlooked in the presence of other symptoms;
- Pressure of tumor inflammation on the congestive optic disc. In most cases it causes swelling in the eye area and blurred vision. In medicine, this pathology is considered an obligatory sign of tumors in the brain. The process of visual acuity impairment progresses and cannot be corrected with optical lenses;
- Constant intracranial pressure in most cases causes mental disorders in patients. Primary signs of impaired concentration or memory cause emotional instability. Progression of tumor growth can provoke aggression and inappropriate behavior;
- A type of epileptic seizures of the generalized category, which accompany patients in most cases of cancer. They are unpredictable and occur when the patient is absolutely calm and well-being. This is a very serious symptom that requires mandatory medical monitoring.
The appearance of a tumor in the brain is not always indicated by certain symptoms, and their manifestation during the course of the disease has its own characteristics. It all depends on the location of the tumors inside the skull.
Risk factors
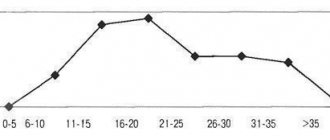
Primary malignancies in the head account for only a small percentage of all cancers. However, this disease is extremely common in children and comes second after leukemia.
- This disease is more often found in males, but some of its forms, for example, meningiomas, are more often detected in women.
- A huge number of tumors in the head occur in people aged 60-80 years, as well as in preschool children.
- This disease is diagnosed more often in white people than in other races.
- Poor environment and harmful working conditions.
- Exposure to radiation.
- Study of chemicals, other substances and metals.
- People with immune system disorders also have a high risk of developing central nervous system lymphoma.
- Genetic predisposition.
It should be noted that at the moment the exact causes of this pathology are unknown.
Establishing a diagnosis of a brain tumor
If persistent health problems appear, it is imperative to consult a doctor, who will prescribe a number of diagnostic procedures to check the head for the presence of oncological manifestations.
Symptomatic detection of brain cancer
Identified abnormalities in the patient’s nervous system provide grounds for clarifying the diagnosis. For this purpose, modern diagnostic methods are used. Since X-ray readings provide insufficient information, computer techniques are used for a more accurate diagnosis of a tumor, one of them is CT - computed tomography or another version of MRI - magnetic resonance imaging. With their help, it is possible to determine the exact location of the tumor and its size. How to check if there is a brain tumor? Currently, computer methods are used.
The diagnosis of pituitary adenoma is confirmed by MRI or CT techniques only when the process of compression of the nerve endings of the eye begins. A blood test confirms the presence of pituitary hormones.
- The type of tumor is determined by examining part of the affected tissue using a microscope. The method in medicine is called biopsy;
- Cerebral fluid is subjected to microscopic examination if the development of a malignant tumor is suspected. Cerebral fluid is obtained using a lumbar puncture. This procedure is used only if there is no increase in intracranial pressure. Otherwise, a serious complication called herniation may occur. The consequence may be disruption of the respiratory process, heart contractions, and a sharp change in blood pressure;
- A biopsy is performed during surgery to remove the entire tumor. To identify oncology located in remote areas of the brain that are difficult to reach with a surgeon’s instrument, modern equipment is used to scan the required area. With the help of the latest devices, the surgeon is able to monitor the manipulations of the needle designed to select the affected tissue.
Existing methods help doctors both recognize a brain tumor and prescribe the correct treatment in the early stages of the disease.
Treatment methods for brain tumors
Studies performed in the diagnostic department make it possible to prescribe individual treatment to the patient, since the treatment regimen is determined by several factors: age, general condition of the patient, the size of the tumor formation, its type and location in the skull. As a rule, treatment involves the participation of specialists in various fields: oncologist, neurologist, neurosurgeon, radiologist, physiotherapist and rehabilitation specialist.
There are newer techniques used to treat patients diagnosed with a brain tumor.
Surgical method
Surgery is the most commonly used treatment procedure. This method is used to remove the tumor and identify it.
If the tumor is difficult to access, surgeons perform a biopsy to obtain a portion of the tissue necessary to determine the type of tumor. Removing benign tumors often allows one to obtain satisfactory results and improve the patient’s condition. During surgery, the neurosurgeon tries to remove the entire growth.
Brain tumor - treatment methods
Surgery is advisable for brain tumors, since in this case the surgeon has the opportunity to remove part of the healthy tissue, which will provide a greater guarantee against the recurrence of a harmful tumor.
However, in the case of brain surgery, the neurosurgeon's capabilities are greatly limited due to the characteristics of the tissues that are responsible for certain body functions. At the present stage, the section of surgery has been replenished with new non-surgical methods for removing harmful formations. This is the so-called stereotactic (radiosurgery) method. This category includes gamma knives, cyber knives and proton beam surgery.
The use of modern methods creates undeniable advantages over the surgeon’s usual tool – a scalpel. However, the use of these methods is limited due to the longer recovery procedure and the higher risk of possible complications.
As a rule, before the upcoming surgical intervention, the patient undergoes conservative treatment, which consists of the following:
- undergoing an anti-inflammatory steroid course to reduce swelling in the area of the tumor;
- prophylactic administration of drugs that reduce the possibility of involuntary seizures during surgery;
- the use of a shunt method to reduce the patient’s hypertensive state by removing excess cerebral fluid.
After carrying out the necessary preliminary procedures, neurosurgeons use the optimal method for removing oncology.
International histological classification of tumors of the central nervous system (WHO, 2020).
| Tumor type | Grade | ICD-O code |
| Diffuse astrocytic and oligodendroglial tumors | ||
| Diffuse astrocytoma NOS (not otherwise specified) | II | 9400/3 |
| Diffuse astrocytoma with a mutation in the IDH gene | II | 9400/3 |
| Gemistocytic astrocytoma | II | 9411/3 |
| Diffuse astrocytoma without mutations in the IDH gene | II | 9400/3 |
| Anaplastic astrocytoma NOS | III | 9401/3 |
| Anaplastic astrocytoma with a mutation in the IDH gene | III | 9401/3 |
| Anaplastic astrocytoma, without mutations in the IDH gene | III | 9401/3 |
| Glioblastoma NOS | IV | 9440/3 |
| Glioblastoma without mutations in the IDH gene | IV | 9440/3 |
| Gliosarcoma | IV | 9442/3 |
| Giant cell glioblastoma | IV | 9440/3 |
| Epithelioid glioblastoma | IV | 9440/3 |
| Glioblastoma with a mutation in the IDH gene | IV | 9445/3 |
| Diffuse midline glioma | IV | 9385/3 |
| Oligodendroglioma NOS | II | 9450/3 |
| Oligodendroglioma with a mutation in the IDH gene and 1p/19q codeletion | II | 9450/3 |
| Anaplastic oligodendroglioma NOS | III | 9451/3 |
| Anaplastic oligodendroglioma, with a mutation in the IDH gene and 1p/19q codeletion | III | 9451/3 |
| Oligoastrocytoma | II | 9382/3 |
| Anaplastic oligoastrocytoma | III | 9382/3 |
| Other astrocytic tumors | ||
| Pilocytic/piloid astrocytoma | I | 9421/1 |
| Pilomyxoid astrocytoma | IV | 9425/3 |
| Subependymal giant cell astrocytoma | I | 9425/3 |
| Pleomorphic xanthoastrocytoma | II | 9424/3 |
| Anaplastic pleomorphic xanthoastrocytoma | III | 9424/3 |
| Ependymal tumors | ||
| Subependymoma | I | 9383/1 |
| Myxopapillary ependymoma | II | 9394/1 |
| Ependymoma | II | 9391/3 |
| Papillary ependymoma | 9393/3 | |
| Clear cell ependymoma | 9391/3 | |
| Tanycytic ependymoma | 9391/3 | |
| Anaplastic ependymoma | III | 9392/3 |
| Ependymoma with RELA chimera | 9396/3 | |
| Other gliomas | ||
| Chordoid glioma of the third ventricle | II | 9444/1 |
| Angiocentric glioma | 9431/1 | |
| Astroblastoma | IV | 9430/3 |
| Tumors of the choroid plexus | ||
| Choroid plexus papilloma | I | 9390/0 |
| Atypical papilloma of the choroid plexus | II | 9390/1 |
| Choroid plexus carcinoma | III | 9390/3 |
| Neuronal and mixed neuronal-glial tumors | ||
| Dysembryoplastic neuroepithelial tumor | I | 9413/0 |
| Gangliocytoma | I | 9492/0 |
| Ganglioglioma | I | 9505/1 |
| Anaplastic ganglioglioma | III | 9505/3 |
| Dysplastic cerebellar gangliocytoma (Lhermitte–Duclos disease) | I | 9493/0 |
| Desmoplastic astrocytoma and ganglioglioma in children | I | 9412/1 |
| Papillary glioneuronal tumor | I | 9509/1 |
| Rosette-forming glioneuronal tumor | I | 9509/1 |
| Diffuse leptomeningeal glioneuronal tumor | Not determined | No |
| Central neurocytoma | II | 9506/1 |
| Extraventricular neurocytoma | II | 9506/1 |
| Cerebellar liponeurocytoma | II | 9506/1 |
| Paraganglioma | I | 8693/1 |
| Tumors of the pineal region | ||
| Pineocytoma | I | 9361/1 |
| Parenchymal tumor of the pineal gland of intermediate differentiation | II or III | 9362/3 |
| Pineoblastoma | IV | 9362/3 |
| Papillary tumor of the pineal region | II or III | 9395/3 |
| Fetal tumors | ||
| Medulloblastoma NOS | IV | 9470/3 |
| Medulloblastoma classic | IV | 9470/3 |
| Medulloblastoma, desmoplastic/nodular | IV | 9471/3 |
| Medulloblastoma with pronounced nodularity | IV | 9471/3 |
| Medulloblastoma, large cell/anaplastic | IV | 9474/3 |
| Medulloblastoma with activation of the WNT signaling cascade | IV | 9475/3 |
| Medulloblastoma with activation of the SHH signaling cascade and mutation in the TP53 gene | IV | 9476/3 |
| Medulloblastoma with activation of the SHH signaling cascade without mutations in the TP53 gene | IV | 9471/3 |
| Medulloblastoma without activation of the WNT/SHH signaling cascades | IV | 9477/3 |
| Medulloblastoma, group 3 | IV | No |
| Medulloblastoma, group 4 | IV | No |
| Embryonic tumor with multilayered rosettes, with damage to the C19MC gene | IV | 9478/3 |
| Embryonic tumor with multilayered rosettes NOS | IV | 9478/3 |
| Medulloepithelioma | IV | 9501/3 |
| Neuroblastoma of the central nervous system | IV | 9500/3 |
| Ganglioneuroblastoma of the central nervous system | IV | 9490/3 |
| Embryonic tumor of the central nervous system NOS | IV | 9473/3 |
| Atypical teratoid/rhabdoid tumor | IV | 9508/3 |
| Embryonic tumor of the central nervous system with rhabdoid features of the central nervous system | IV | 9508/3 |
| Tumors of the cranial and spinal nerves | ||
| Schwannoma | I | 9560/0 |
| Plexiform schwannoma | I (this and the next 2 are subtypes of schwannoma) | 9560/0 |
| Cellular schwannoma | I | 9560/0 |
| Melanocytic schwannoma | I | 9560/1 |
| Neurofibroma | I | |
| Atypical neurofibroma | I | 9540/0 |
| Plexiform neurofibroma | I | 9550/0 |
| Perineurioma | I-III | 9571/0 |
| Malignant peripheral nerve sheath tumor (MNTS) | There are both benign and malignant, but according to ICD - malignant | 9540/3 |
| Epithelioid PVD | IV | 9540/3 |
| PVD with perineural differentiation | IV | 9540/3 |
| Meningiomas | ||
| Meningioma | I | 9530/0 |
| Meningothelial meningioma | I | 9531/0 |
| Fibrous meningioma | I | 9532/0 |
| Transitional meningioma | I | 9537/0 |
| Psammomatous meningioma | I | 9533/0 |
| Angiomatous meningioma | I | 9534/0 |
| Microcystic meningioma | I | 9530/0 |
| Secretory meningioma | I | 9530/0 |
| Meningioma with pronounced lymphoplasmacytic infiltration | I | 9530/0 |
| Metaplastic meningioma | I | 9530/0 |
| Chordoid meningioma | II | 9538/1 |
| Clear cell meningioma | II | 9538/1 |
| Atypical meningioma | II | 9539/1 |
| Papillary meningioma | III | 9538/3 |
| Rhabdoid meningioma | III | 9538/3 |
| Anaplastic (malignant) meningioma | III | 9530/3 |
| Mesenchymal, non-meningothelial tumors | ||
| Solitary fibrous tumor/hemangiopericytoma Grade 1 | I | 8815/0 |
| Solitary fibrous tumor/hemangiopericytoma Grade 2 | II | 8815/1 |
| Solitary fibrous tumor/hemangiopericytoma Grade 3 | III | 8815/3 |
| Hemangioblastoma | I | 9161/1 |
| Hemangioma | I | 9120/0 |
| Epithelioid hemangioendothelioma | 9133/3 | |
| Angiosarcoma | IV | 9120/3 |
| Kaposi's sarcoma | IV | 9140/3 |
| Ewing's sarcoma/simple neuroectodermal tumors | IV | 9364/3 |
| Lipoma | I | 8850/0 |
| Angiolipoma | I | 8861/0 |
| Hibernoma | I | 8880/0 |
| Liposarcoma | IV | 8850/3 |
| Fibromatosis desmoid type | Unknown | 8821/1 |
| Myofibroblastoma | I | 8825/0 |
| Inflammatory myofibroblastic tumor | Unknown | 8825/1 |
| Benign fibrous histiocytoma | I | 8830/0 |
| Fibrosarcoma | IV | 8810/3 |
| Undifferentiated pleomorphic sarcoma/malignant fibrous histiocytoma | IV | 8802/3 |
| Leiomyoma | I | 8890/0 |
| Leiomyosarcoma | IV | 8890/3 |
| Rhabdomyoma | I | 8900/0 |
| Rhabdomyosarcoma | IV | 8900/3 |
| Chondroma | I | 9220/0 |
| Chondrosarcoma | IV | 9220/3 |
| Osteoma | I | 9180/0 |
| Osteochondroma | I | 9210/0 |
| Osteosarcoma | IV | 9180/3 |
| Melanocytic tumors | ||
| Meningeal melanocytosis | I | 8728/0 |
| Meningeal melanocytoma | II | 8728/1 |
| Meningeal melanoma | IV | 8720/3 |
| Meningeal melanomatosis | IV | 8728/3 |
| Lymphomas | ||
| Diffuse large B-cell lymphoma of the central nervous system | IV | 9680/3 |
| Diffuse large B-cell lymphoma in AIDS | IV | No |
| EBV-positive diffuse large B-cell lymphoma, NOS | IV | No |
| Lymphomatoid granulomatosis | II | 9766/1 |
| Intravascular large B-cell lymphoma | IV | 9712/3 |
| Low-grade CNS B-cell lymphomas | No | No |
| T-cell and NK/T-cell lymphomas of the central nervous system | IV | No |
| Anaplastic large cell, ALK-positive lymphoma | IV | 9714/3 |
| Anaplastic large cell, ALK-negative lymphoma | IV | 9702/3 |
| MALT lymphoma of the dura mater | IV | 9699/3 |
| Histiocytic tumors | ||
| Langerhans cell histiocytosis | IV | 9751/3 |
| Erdheim-Chester disease | II | 9750/1 |
| Rosai-Dorfman disease | No | No |
| Juvenile xanthogranuloma | No | No |
| Histiocytic sarcoma | IV | 9755/3 |
| Germ cell tumors | ||
| Germinoma | IV | 9064/3 |
| Embryonic cancer | IV | 9070/3 |
| Yolk sac tumor | IV | 9071/3 |
| Chorionic carcinoma | IV | 9100/3 |
| Teratoma | II | 9080/1 |
| Mature teratoma | I | 9080/0 |
| Immature teratoma | IV | 9080/3 |
| Teratoma with malignant transformation | IV | 9084/3 |
| Mixed germ cell tumor | IV | 9085/3 |
| Tumors of the sella turcica area | ||
| Craniopharyngioma | 9350/1 | |
| Adamantine-like craniopharyngioma | II | 9351/1 |
| Papillary craniopharyngioma | II | 9352/1 |
| Granulocellular tumor of the sella region | I | 9582/0 |
| Pitucytoma | II | 9432/1 |
| Spindle cell oncocytoma | I | 8290/0 |
ICD-O (ICD-O) – Morphological code of the International Classification of Diseases in Oncology. The grade of malignancy is coded as follows: /0 for benign tumors, /3 for malignant tumors and /1 for transitional forms or unspecified malignancy.
Method of radiation therapy for brain tumors
Radiation therapy is a popular method of treating cancer. It is resorted to if surgical intervention is unacceptable.
This method is also used after surgical removal of a harmful formation. This is necessary to prevent relapse of the disease. The radiation method is used to locally remove the affected cells. In this case, only part of the brain is exposed to radiation, a certain dose calculated by the doctor individually, taking into account all factors.
Cancer chemotherapy method
In medicine, this method is classified as a systemic course of treatment. The effect is exerted on the patient’s entire body, that is, during the treatment process, both affected and healthy cells are affected.
One or more drugs are used for treatment. The entire course of treatment is selected by oncologists according to a specific scheme, taking into account all factors: age, concomitant diseases, degree of risk. The drugs are designed for oral and intravenous administration.
Treatment of patients with chemotherapy in combination with radiation increases the effect of fighting cancer. However, this type of treatment is characterized by side effects that are caused by the toxic effects of drugs on the gastrointestinal tract and the circulatory system of the brain.
Condition of a woman in advanced stages of cancer
When the tumor has developed so much that it puts excessive pressure on the nervous tissue, its cells are transferred throughout the body through the circulatory system, and the patient’s well-being deteriorates greatly. Due to the extensive destruction of the myelin sheath of nerve tissue, a decrease in motor function is formed. Gradually the person becomes bedridden. Only some patients retain the ability to walk.
Food can only be consumed parenterally, as the swallowing reflex is impaired. When urinary function is eliminated, the patient is given a catheter through which urine flows. There is often an admixture of blood in it. This indicates an extensive inflammatory process and damage to the walls of the mucous membrane.
Infertility in a woman develops not only due to illness, but also due to chemotherapy or radiation.
The person loses consciousness and often falls into a coma. At this stage, doctors consult with relatives about the use of artificial ventilation or its elimination.
These actions may be discussed in advance with the cancer patient before she falls into a coma. If mechanical ventilation is not used, death occurs because the respiratory system cannot cope on its own.
In later stages, therapy is not recommended. The tumor is extensive and cannot be removed. Chemotherapy will make you feel worse.
Endoscopic treatment method
The method of endoscopic treatment of brain tumors involves penetration of the tumor through small incisions. This process is carried out using special endoscopic devices. This technique achieves accurate access to the tumor lesion in the brain. In this case, there are no disturbances in the blood vessel system. . Promising treatment methods cannot yet guarantee complete recovery of patients with cancer in the naked eye. Only certain types of tumors do not resume their development within five years after undergoing a course of treatment or surgery.