Anatomy
The anatomy of the nervous system is quite complex and tortuous. The nerve trunk comes from processes covered with a special tissue - neuroglia. When neuroglia are damaged, the symptoms do not manifest themselves very acutely, compared to infringement or damage to the neuroglia itself.
The facial nerve consists of:
- areas of the cerebral cortex responsible for the work of facial muscles;
- Nuclei are located between the medulla oblongata and the bridge. There are three nuclei responsible for facial expressions; nucleus of the solitary tract regulatory
salivation endings giving taste sensations, corrects the salivary glands;
- directly the nerve trunk, or rather its processes;
- capillary network and lymph nodes, due to which the nerve cells are nourished.
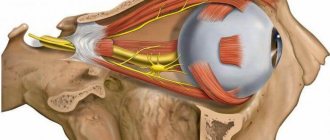
Also, facial sensitivity occurs due to the fact that the trigeminal nerve is located nearby. The ophthalmic branch is derived from the trigeminal. Basically, it serves as a sensory transmitter, that is, it transmits data from various receptors. Thinner nerve branches also diverge from the ophthalmic branch and innervate the orbit. Accordingly, the orbital fissure is supplied by the innervation of the trigeminal, and from it, in turn, branches extend to the frontal, lacrimal and nasociliary.
The maxillary branch also consists only of sensitive cells and transmits information from receptors. In the orbit itself, this branch branches, entering there through the lower palpebral fissure. The maxillary branch throws off the nerve maxillary plexus; its main task is the interaction of the nervous system with the receptors of the gums and teeth. As soon as the maxillary nerve fibers pass into the infraorbital region, innervation of the eyelid immediately occurs. And only one single branch regulates the sensitivity of the cheekbones and cheeks - this is the zygomatic nerve, which subsequently enters through the superior fissure into the orbit itself.
The mandibular branch, unlike those listed above, not only carries information between the central nervous system and nerve cells, but also carries out motor function. This is a large branch, starts from the oval foramen and immediately gives off three branches. Sensitivity is applied to the gums, dental nerve endings of the lower jaw and cheeks. The pterygoid, masticatory and temporal branches are responsible for motor functions.
Occipital neuralgia
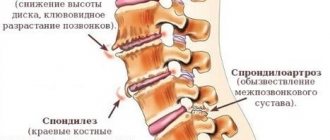
This disease is a complex of symptoms that include symptoms of damage to the nerves that form the cervical plexus. Occipital neuralgia can develop due to the influence of various etiological factors, which include:
- various intoxications and infections, pathological processes occurring in the cervical segment of the spine - spondyloarthrosis, spondylosis deformans;
- tuberculous spondylitis;
- ailments of the cardiac system - hypertensive disease and aneurysm of the vertebral artery in combination with circulatory disorders in the vertebrobasilar system;
- tumor formation localized in the cervical segment of the spinal cord, craniospinal zone, postcranial fossa;
- pachymeningitis of the cervical segment.
Treatment of occipital neuralgia includes the use of symptomatic medications. Also here you need to heal the basic ailment.
Functions
The most basic task of the facial nerve is motor function. Before branching into small parts, it is intertwined with the intermediate one, and performs some of the duties together with it. Through the internal auditory opening they tend to the tunnel of the facial nerve. After this, the genu begins to form, which provides sensory input to the intermediate nerve.
Coming from the parotid gland, the branches of the facial nerve are divided into powerful superior and more graceful inferior. They also branch into smaller processes. Which create the parotid plexuses, then the nerve provides motor activity to almost all facial muscles. But although this function is the main one, due to the intermediate nerve, it has secretory and taste fibers.
The intermediate one, located in the thickness of the temporal bone, throws off nerve processes: the large stony one, the stapedial one, the branches connecting it and the tympanic plexus, all of which ends with the chorda tympani.
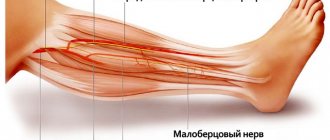
Cutaneous branches of the cervical plexus
It is known that the cervical plexus consists of:
- The occipital minor nerve, which arises from the third and second cervical nerves (CIII and CII), runs to the posterior border of the cleidosternomastoid muscle, and as it emerges from it, it often divides into a pair of branches. The latter follow upward and to the back of the head, then branch behind the auricle and above it in the area of the skin bordering at the back with the branching area of the large occipital nerve, and at the front with the segment of the large auricular nerve. The minor occipital nerve has connections with the greater occipital and auricular nerves and the facial nerve (its auricular posterior nerve).
- The auricular nerve (nervus auricularis magnus) is the largest cutaneous nerve of the cervical weave. It starts from CIII (CIV), follows the posterior border of the cleidosternomastoid muscle and, bypassing it below the tiny occipital nerve, moves to the outer surface of the muscle. Here the nerve trunk goes forward and upward to the auricle and is divided into posterior and anterior branches. What are the branches of the great auricular nerve? The anterior one is thinner, branches in the skin of the parotid gland segment, earlobe and in the skin of the sunken surface of the auricle. The dorsal branch branches in the skin behind the ear and in the skin of the protruding surface of the concha.
- The transverse nerve of the neck appears from CII (CIII), is directed, just like the large auricular nerve, to the posterior border of the cleidosternomastoid muscle, passes it and then follows in a perpendicular direction forward along the outer surface of this muscle, between it and the muscle neck subcutaneous. This nerve has connections with the cervical branch of the facial nerve, forming a cervical superficial loop with it.
- The supraclavicular nerves arise from CIII (CIV), follow the posterior border of the cleidosternal-mastoid muscle and emerge from behind it slightly below the perpendicular nerve of the neck, being located here in the area of the clavioscapular triangle, under the fascia. Then, piercing the fascia, the nerves travel down to the collarbone and fan out into three sets of branches: medial supraclavicular nerves, intermediate and lateral.
Clinical lesions
If a malfunction occurs or the facial nerve canal is pinched, this can lead to paralysis of the motor facial muscles. Facial asymmetry is visually diagnosed. The part of the face that is relaxed and motionless creates a mask effect, the eye does not close on the affected side, and lacrimation increases. It occurs due to irritation of the eye mucosa by air and dust, therefore leading to inflammation and conjunctivitis. Wrinkles on the forehead and nasolabial area are straightened. The corners of the mouth “look” down; the victim cannot wrinkle his forehead on his own. Paralysis of the orbicularis oculi muscle and the non-adjacent part of the eyelid to the eyeball lead to disruption of the formation of the capillary gap. Because of this, problems with tear production occur.

Peripheral lesions
If for some reason motor function is affected, then we can talk about peripheral paralysis. The clinical manifestations are as follows: complete asymmetry of the face, paralysis of facial muscles, limited intake of liquids, impaired speech apparatus. If damage to the nerve occurs when it is located in the pyramidal bone, then the following is observed: absence of taste symptoms, deafness and all of the above symptoms are observed.
Neuritis
A neurological disease characterized by inflammation. Neuritis can be located in the central part of the face and in the peripheral part. Symptoms depend on which part of the nerve is involved. As a rule, there are no erroneous diagnoses in differentiation and formulation. The development of the disease can be due to hypothermia, the so-called primary neuritis, and secondary, manifested due to some other diseases.
The clinical picture is described by an acute onset. The pain radiates behind the ear, and after a few days, facial asymmetry is noticeable. Symptoms may vary, depending on the affected part. If the nucleus of the facial nerve is affected, then the person suffers from facial muscle weakness. The process of infringement located in the area of the pons of the brain leads to strabismus and paralysis of almost all facial muscles. If infringement occurs at the exit, this can lead to impairment and short-term hearing loss.
Neuritis can be concomitant, for example, with chronic otitis media. And it arises due to the ongoing process of inflammation in the middle ear. Therefore, facial paresis occurs with accompanying “shooting” in the ear. When accompanied by mumps, general intoxication of the body occurs - fever, chills, body aches.
The treatment regimen for inflammation and injuries should be comprehensive and timely. Drug therapy necessarily includes:
- glucocorticosteroid drugs;
- diuretics that remove fluid from the capillary network;
- drugs that promote vasodilation;
- vitamin therapy, usually group B.
Further, complex treatment of this nerve includes exclusion and treatment of the underlying cause. Since neuralgia is the result of an illness or a secondary disease. Usually, nervous diseases are accompanied by quite painful sensations; analgesics are prescribed to reduce or stop them. For more effective and rapid treatment, the facial muscles should remain completely at rest. Physiotherapeutic measures are also adjacent to complex treatment. From the second week of the diagnosed disease, you can include facial massages and physical therapy. In this case, the load increases gradually.
Surgical intervention is performed in rare cases, if neuralgia is congenital or the nerve is severely damaged due to mechanical trauma. This operation involves stitching together torn or incorrectly fused ends. Another case that provokes surgical intervention is the ineffectiveness of drug therapy for 6-8 months. If you do not resort to such treatment methods or strongly start the disease process, this leads to complete atrophy of the facial muscles, which can no longer be restored. You can also resort to surgical facial plastic surgery; the material for this is taken from the leg of the person being operated on.

Therapy
The basis of therapy is anti-inflammatory drugs and analgesics. To relieve inflammation, medications containing ibuprofen or diclofenac are used. They also help relieve pain. In addition, to reduce pain, taking painkillers with ibuprofen or analgin is indicated. It is important to take antispasmodic medications. This relieves muscle spasm of the auditory tube, which increases discomfort and accompanies neuralgia.
To improve the patient's well-being and speed up recovery, the use of sedative medications is indicated. They normalize sleep and strengthen the nervous system, which speeds up recovery. Therapy is often supplemented with B vitamins and vasodilators (for example, nicotinic acid).
If medical treatment cannot be carried out for any reason, physiotherapy is used - electrophoresis, acupuncture, amplipulse.
Facial nerve: anatomy, diagram, structure, functions and features
The topographic anatomy of the facial nerve is quite confusing, due to the fact that it passes through the facial canal of the temporal bone, receiving and giving off processes.
Where does it start?
It arises from three nuclei at once: motor, secretory and sensory fibers. Then, through the auditory opening, the facial nerve passes into the thickness of the temporal bone into the internal auditory canal.
Here the intermediate nerve is added to it, and a knee is formed at the bend of the canal, which, taking the form of a node, gives the intermediate nerve the property of sensitivity.
The anatomy of the facial nerve and its diagram will be discussed in this article.
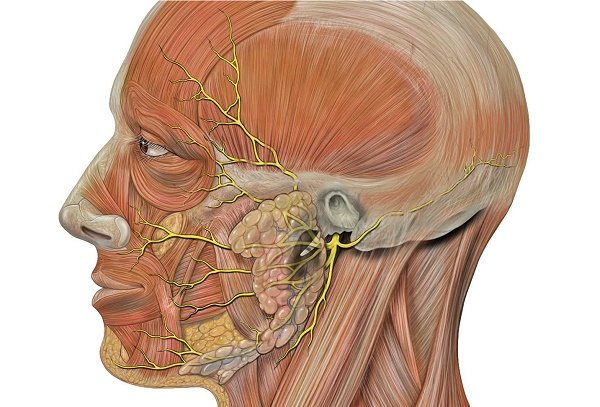
To enter the thickness of the parotid gland, the facial nerve is divided into separate processes: the lingual branch, the posterior auricular nerve, the digastric and stylohyoid branches. The intermediate gives off branches such as the stapedius and petrosal nerves, connective tissue with the tympanic weave and the vagus nerve, and the terminal branch (corda tympani). The anatomy of the facial nerve is unique.
Once again, the facial nerve diverges in the thickness of the parotid gland, giving two main branches - a small lower and powerful upper, which then also branch, moreover, radially: up, forward and down to the facial muscles. As a result, the parotid plexus is formed.
The facial nerve (the anatomy diagram will be presented in the photo) consists of the following parts:
- nerve trunk (more precisely, its processes);
- the spaces of the cerebral cortex, which are responsible for the work of facial muscles;
- nuclei located between the bridge and the medulla oblongata;
- lymph nodes and a network of capillaries that feed nerve cells.
Functions
The anatomy of the facial nerve (diagram posted above) is reviewed. Now let's talk about its functions.
The task of the facial nerve is to provide motor functions of the face. However, everything is complicated by the fact that before it branches into small parts, it is intertwined with the intermediate nerve and partially shares responsibilities with it. Through the internal auditory opening they move into the tunnel of the facial nerve, where it forms a genu that provides sensory input to the intermediate nerve.
The pattern of the fibers of the facial nerve is very interesting and requires careful consideration.
If the canal is malfunctioned or infringed, paralysis of the motor muscles of the face may occur.
Its asymmetry is visually observed: the relaxed part has a mask effect due to its immobility, the eye on the affected side does not close, and lacrimation increases due to the fact that the mucous membrane is irritated by dust and air, which, in turn, can cause conjunctivitis. Wrinkles on the forehead and the area around the nose and lips are straightened, the corners of the mouth are directed downward, the person cannot wrinkle his forehead.
In humans, the facial nerve is often affected (its branches, their anatomy and topography are presented in detail in the photo).
It is characterized by the following external signs: paralysis of the muscles responsible for facial expressions, complete asymmetry of the face, the speech apparatus is impaired, fluid intake can be limited.
If the nerve was affected at a time when it was located in the pyramidal bone, then in addition to the signs listed above, deafness and lack of taste are also noted.
Many have seen people with asymmetrical facial features or skewed in one direction. It’s hard to forget such a picture. Thus, neuritis of the facial nerve manifests itself.
Anatomy
The facial nerve is classified as the seventh pair of cranial nerves. The importance of its work for our body is difficult to overestimate. It innervates the muscles of the face; communication, which is based on the movement of the tongue muscles and facial expressions, depends on it. This nerve is also responsible for the sense of taste in the first third of the tongue.
The topography of the facial nerve is not simple and confusing. Its unique structure and blood supply have been studied for a long time. The nerve exits the brain into the cranial cavity, where it runs in the canal of the temporal bone. Next, it comes into contact with the auditory opening and passes onto the face.
Before entering the thickness of the parotid gland, the nerve fiber is divided into branches of the facial nerve: the lingual branch, the posterior auricular nerve, the digastric and stylohyoid branches.
In the thickness of the parotid gland, branching occurs again: into a small lower and much larger upper branch. And they, in turn, branch in three directions to the facial muscles: up, forward and down.
Structure of the facial nerve:
- nerve trunk;
- cerebral cortex (responsible for the work of facial muscles);
- nuclei between the medulla oblongata and the pons;
- networks of capillaries in lymph nodes (responsible for feeding cells).
Medicine has been dealing with colds of the facial nerve for a long time and today. This is mainly a seasonal illness associated with cold weather.
Diseases of the facial nerve usually manifest as problems with the movement of facial expressions. The symptoms of the disease may be similar to other ailments, which may be chronic and seem harmless in the early stages. Therefore, if you have alarming symptoms, you should not hesitate to go to the doctor.
The first signs may be mild pain in the ears. Then it is better to immediately contact an ENT doctor. If it does not go away and the face becomes distorted (the skin may also freeze in the mask), then most likely the facial nerve is damaged or inflamed.
A type of disease is paralysis of the motor muscles of the face. In this case, the person has visible facial asymmetry, one side resembles a mask, the eye on it does not close.
Paralysis usually develops due to injury to the tympanic portion of the facial nerve canal. This often happens during ear surgery. The disease also has associated problems:
- Getting dust and dirt onto the mucous membrane (with the eye open).
- The likelihood of conjunctivitis.
- With this type of disease, the patient cannot wrinkle his forehead himself.
Peripheral paralysis occurs when basic motor function is affected. Then complete asymmetry of the face occurs due to paralysis of the facial muscles. The movements of the speech apparatus are also impaired.
In addition to paralysis, there are paresis of the facial nerve. They are not always noticeable. With paresis, muscle movement functions are only partially impaired. The disease manifests itself most often when a person is talking. Paresis is classified into:
- Easy. Changes in facial expressions are minor.
- Heavy. The face turns into a mask. He is close to paralysis.
The cause of paresis and paralysis can be both compression of the fibers and nerve damage.
Symptoms of paresis and paralysis are as follows:
- difficulties with swallowing, speech;
- drooling, lacrimation;
- asymmetry of facial muscles;
- pain;
- eye twitching;
Signs may also include:
- bulging of the eyeball or turning it to the side;
- difficulty in pulling out the lips;
- hearing impairment, greater sensitivity;
- lacrimation.
The phase of the disease is also important. In its acute form, the symptoms appear most clearly.
Unlike paresis, neuritis is characterized by inflammation. The inflammatory process can occur in any part of the face.
There are secondary and primary neuritis. The first develops due to a cold. The second is a complication from other diseases. For example, the disease often develops with chronic otitis media, and neuritis of the facial nerve is also associated with otorhinolaryngology.
There may be many causes of the disease. It is important which part of the nerve is affected. Neuritis can also develop due to diseases:
- middle ear disease;
- stroke;
- ischemia;
- infection;
- oncology;
- multiple sclerosis;
- cerebral circulatory disorders and others;
The main reason is hypothermia.
For paresis and neuropathy, traditional methods of treatment are also effective. They are aimed at reducing pain and restoring nerve function. Various infusions and ointments are used. They use deltoid carnation, tricolor violet, sage, centaury, and creeping thyme. Each herb has its own method of brewing and infusion.
Also, when treating nerve colds, goat's milk with honey, flax seeds are used (they must first be steamed and then applied to the sore spot), rubbing fir oil helps a lot. Heated sand or salt is placed in bags and applied to the painful area. Doctors often advise drinking rose tea and other drinks that calm the central nervous system.
If the disease is detected early and all recommendations of a competent doctor are followed, the prognosis for cure is favorable. After proper regular therapy, the disease ends. Surgery is rarely resorted to.
The operation is resorted to in the following cases:
- if the injury is congenital;
- after a mechanical injury;
- when other therapy does not help;
During the operation, nerve endings that have grown together incorrectly or have been torn are stitched together. In case of additional treatment, devices are inserted into the facial nerve to reduce its sensitivity.
The facial nerve or nervus facialis is the seventh paired cranial nerve CN VII. In terms of anatomy, it performs motor, sensory and parasympathetic functions. According to evolutionary anatomy, the branches of the facial nerve, like itself, originate from the second branchial arch, which is present in the embryo.
The facial nerve innervates the muscles responsible for facial expression, the stylohyoid muscle, the posterior belly of the digastric muscle, and the stapedius muscle. It also recognizes the sense of taste in the tongue and transmits a signal to the corresponding part of the brain.
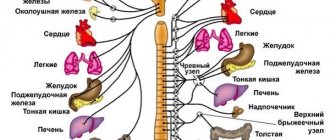
Nervus facialis performs a parasympathetic function. It lies in the fact that this nerve (nervus) can innervate many glands of the neck and head, including:
- lacrimal;
- salivary;
- producing mucus in the nasal cavity, palate and pharynx.
The topography of the facial nerve is quite complex. It has many branches, which consist of various combinations of sensory, motor and parasympathetic fibers.
From an anatomical point of view, the nervus facialis is divided into two parts. The first is intracranial, that is, it passes through the skull and its cavity. The second part is extracranial: it goes outside the skull, through the face and neck.
The nuclei of the facial nerve are located in the brainstem, which is called the pons. This is where the facial nerve begins. Its origin consists of two roots, large motor and small sensory. The part of the nervus facialis that originates from the small sensory root is called the intermediate nervus, in other words, the Wriesberg nerve.
When is surgery necessary?
The operation is resorted to in the following cases:
- if the injury is congenital,
- after a mechanical injury,
- when other therapy does not help,
During the operation, nerve endings that have grown together incorrectly or have been torn are stitched together. In case of additional treatment, devices are inserted into the facial nerve to reduce its sensitivity.
You should not resort to surgery if you can do without it.
Can complications occur? If the nerve is treated incorrectly or not treated, the following complications may occur:
- muscle contracture (when they tighten on one side),
- atrophy (decreased muscle volume),
- synkinesis (nervous excitement spreads across the face incorrectly),
- conjunctivitis,
- keratitis.
Prevention
Taking care of yourself is better than treating paresis or neuritis of the facial nerve. For this it is important: Do not chill the facial nerve, dress appropriately for the weather, and do not be near drafts.
- Eat right, exercise, toughen up.
- Avoid situations that could lead to pinching or other nerve damage.
- It is also important to promptly treat all colds and complications after them, for example, otitis media.
The facial nerve, whose anatomy is complex and unique, performs an important function in innervating the facial muscles.
Diseases of the facial nerve do not affect the overall health of the body. But those affected suffer in the social and psychological spheres of life. A person is embarrassed to appear in society, uncomfortable to communicate. His self-esteem drops.
During the treatment of the disease, it is important when the patient consults a doctor. The disease cannot be started. In difficult cases: if a person does not seek help from a doctor in the first 3 days, the face will remain immobilized forever or asymmetry may be observed.