Under certain external influences, bioelectric signals appear in the brain, appearing at a constant time interval. Bioelectric signals are called “evoked potentials of the brain”; they arise as a result of exposure to an external stimulus or during mental activity, solving a cognitive task. The following are used as stimuli: visual, sound and electrical stimuli, which allow recording visual, auditory, and somatosensory evoked potentials.
At the Neurology Clinic of the Yusupov Hospital, a study is being conducted on the recording of electromagnetic signals emitted or potentiated in organs and tissues. The hospital performs visual, auditory, somatosensory evoked potentials of the brain and other diagnostic tests.
What are evoked potentials?
Evoked potentials (EP) are a method for studying brain functions by recording the response of various structures of the nervous system to internal or external stimuli (visual, sound, tactile).
The study came into practice in the late 50s of the last century. Since then, this method has become an important component of the comprehensive diagnosis of various pathologies of the central nervous system in the work of neurosurgeons, ophthalmologists, and otorhinolaryngologists (ENT doctors).
Obtaining the result is based on the biological activity of the cells of the human body, their reaction to irritation. The transmission of an information signal through each neuron (a cell is a functional unit of the nervous system) to the operating organ (muscles, eyes, skin, etc.) is ensured by the passage of an electrical impulse. In clinical practice, with the help of artificially evoked potentials, it becomes possible to determine the lesion.
The procedure is carried out using an electroencephalograph - an analyzer (a device that records changes in the electrical activity of the brain in the form of a curve). Data is collected from electrodes (similar to those used for electrocardiography) placed on the head.
Types of evoked potentials
Taking into account the patient’s pathology, the required type of stimuli is selected for the study. Depending on the type of stimulus, the following types of techniques are distinguished:
- Visual evoked potentials (VEPs).
- Auditory evoked potentials (AEPs) (acoustic).
- Somatosensory evoked potentials (SSEPs). The conduction of signals from sensitive receptors located on the skin to the brain is being studied.
- Cognitive evoked potentials (CEPs). To study disorders of higher cortical functions - speech, attention, memory, etc.
- Autonomic evoked potentials (EPPs). They are used to detect pathologies of the autonomic nervous system, which is responsible for the functioning of internal organs that are not subject to human will.
- Myogenic vestibular evoked potentials (MVEPs). They determine the state of the vestibular apparatus in the inner ear, which is responsible for balance, the sensation of gravity, vibration and acceleration.
The above types of research have their own narrow indications for the methodology and its implementation.
Indications for the study
The study of evoked potentials of the brain can serve not only for diagnostic purposes, but also to monitor the effectiveness of treatment. Or by the method of objective assessment of the dynamic state of the disease.
Pathologies for which the method is used:
- Multiple sclerosis.
- Acute and chronic cerebral circulatory disorders (stroke).
- Tumor processes.
- Neurodegenerative diseases (the process is accompanied by self-destruction of tissue): Huntington's chorea, or Huntington's disease, Parkinson's disease.
- Toxic and metabolic (metabolism-related) disorders.
- Traumatic brain injury and its consequences.
- Disturbances of consciousness: coma, vegetative state.
- Assessment of brain death.
- Monitoring evoked potentials during surgery and to monitor the effectiveness of resuscitation.
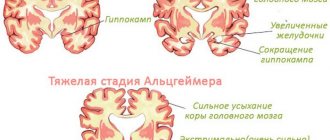
In addition, this method is used to determine the side effects of medications, early diagnosis of various dementias (dementia), assess the initial signs of cognitive impairment in parkinsonism, toxic brain damage, and diagnose disorders in children with deviant (deviating from generally accepted) behavior.
Using different types of potential recording, diseases of the peripheral parts of the analyzers (visual - eyes, auditory - inner ear) are diagnosed, so the method has become widely used in ophthalmological and ENT practice.
Contraindications for the study
Considering that during the research process, stimuli are applied to different sensitive systems with different intensities, there are conditions in which the use of the method is prohibited (described below).
- The presence of inflammatory or other pathological skin lesions at the site of electrode attachment.
- Epilepsy and other conditions accompanied by epileptic seizures.
- Mental illnesses with acute psychoses.
- Angina pectoris.
- High-risk hypertension.
- Presence of a pacemaker (when recording somatosensory potentials, pulses from the pacemaker may give false signals recorded on the potential curve).
Carrying out a diagnostic procedure does not pose a serious risk for the patient, however, in each individual case, the doctor himself decides on the advisability of the appointment.
How to prepare for research
There is no need for special preparation to record evoked potentials. However, in order to prevent false results, doctors recommend the following actions:
- The day before the procedure, stop taking sedatives and vascular medications.
- Rinse off hairspray or hair gel, if any, from your head.
- Get a good night's sleep the night before the test.
In addition, the patient must have the right attitude - excessive anxiety or fear can cause an incorrect conclusion.
How are evoked potentials recorded?
The study is carried out in a specially equipped room in a hospital or diagnostic clinic.
The general scheme looks like this:
- placement of electrodes on the area under study;
- supplying an external signal;
- registration and amplification of the brain response from electrodes on an encephalograph;
- A curve is displayed on the computer screen, which is subject to analysis.
However, each type has its own characteristics, presented in the table:
| Visual VPs | The main electrode is placed on the occipital region. The patient puts on special darkened glasses, which have a built-in LED system. At regular intervals, a flash of varying intensity appears in the glasses. The electrode records the response of the brain in the form of a rise in the curve. Most often, each eye is examined separately, while the other is closed with a shutter. |
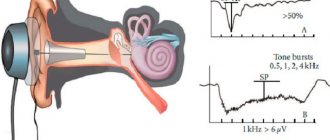
| Auditory VPs | The electrodes are placed symmetrically on the earlobe and in the temporal region of the head. The signal is supplied through headphones. The answer is registered on both sides at once on separate graphs |
| Somatosensory EPs | For this study, two groups of electrodes are required:
An impulse is sent from the stimulating electrodes, which is felt by the patient as a slight tingling sensation. Impulse conduction is studied for each nerve separately |
| Cognitive evoked potentials | This technique is based on a person’s ability to identify significant ones among many signals (visual, audio). The patient’s task is to count the number of significant ones. With their help, the doctor can determine which signals were not taken into account, in which area of the brain the pathology is located |
The duration of the study is from 30 minutes to an hour.
Advantages of this method
To evaluate the benefits of evoked potential testing, the table provides a comparison with other brain research methods.
| Criterion | Evoked potentials | Magnetic resonance imaging | Encephalography |
| Method for obtaining research results | Registration of an electrical impulse on external electrodes in response to stimulating signals | Using a strong electromagnetic field, microscopic movements of hydrogen atoms in tissues are recorded. The final result is layer-by-layer images of organs | Registration of electrical impulses that occur in the brain during normal patient activity |
| Diagnosis of organic changes | Possible | Possible | Functional state only |
| Mental state examination | The capabilities of memory, attention, and the adequacy of the reaction to the intensity of the stimulus are determined | No possibility | No possibility |
| Ability to assess functional status | No possibility | Throughout the study | |
| Duration of the study | 30 minutes - hour | From 30 minutes to 24 hours (for inpatients) | |
| Complications | None |
| None |
In addition, the study does not require access to blood vessels, administration of drugs or contrast agents, so the method can also be used for children.
Possible complications after the procedure
The absence of undesirable consequences is one of the main advantages of the method. However, their occurrence is possible if contraindications are neglected: an attack of epilepsy, angina pectoris, or hypertensive crisis may occur
Doctor's advice! Ignoring even relative contraindications to the study promises the development of serious consequences
How to decipher the result of an evoked potential study
The task that this method sets itself is to determine:
- Level and nature of damage.
- Process propagation.
- Severity.
- Prognosis in the development of the disease.
- Dynamics of the process.
- Monitoring the effectiveness of treatment.
The result of the study is an encephalogram (a curve consisting of peaks of different amplitudes and frequencies), the analysis of which serves as the basis for making a diagnosis.
The interpretation of the results is based on a comparison of the time required for the brain to respond to a stimulus and the magnitude (amplitude) of the reaction. For each type of study, there are peaks responsible for different parts of the brain.
For example, for auditory evoked potentials: registration of an altered peak I indicates brain death, II - pathology in the spinal cord, III - in the pons, IV - midbrain, V - cerebral cortex. This is how the localization and prevalence of the pathological process is determined.
The table shows diseases of the nervous system and corresponding changes in evoked potentials:
| Disease | Signs on the encephalogram |
| Auditory nerve tumor |
|
| Dementia (dementia) |
|
| Huntington's chorea, or Huntington's chorea |
|
| Multiple sclerosis |
|
Important! The test result may be affected by incorrect placement or malfunction of the electrodes, restlessness and poor vision (for recording visual evoked potentials) of the patient
It must be remembered that the evoked potential method is simple, fast and informative. However, deciphering research results is a difficult task that only an experienced specialist can handle.
Brain evoked potentials are a modern testing method
functions and performance of cerebral cortex analyzers. This method allows you to record the responses of higher analyzers to various external artificial stimuli. The most used and widespread stimuli are visual (for recording visual evoked potentials), auditory (for recording acoustic evoked potentials) and somatosensory, respectively.
The process of directly registering potentials
carried out using microelectrodes, which are brought close to the nerve cells of a certain area of the cerebral cortex. Microelectrodes got their name because their size and diameter do not exceed one micron. Such small devices are represented by straight rods, which consist of high-resistance insulated wire with a sharpened recording tip. The microelectrode itself is fixed and connected to the signal amplifier. Information about the latter is received on monitor screens and recorded on magnetic tape.
However, this is considered an invasive method. There is also a non-invasive one. Instead of bringing microelectrodes to the cells of the cortex, the electrodes under study are attached to the skin of the head, neck, torso or knees - depending on the purpose of the experiment.
The evoked potential technique is used to study the activity of the sensory systems of the brain; this method is also applicable in the field of cognitive (mental) processes. The essence of the technology is to register bioelectric potentials formed in the brain in response to an external artificial stimulus.
The response evoked by the brain is usually classified depending on the speed of reaction of the nervous tissue:
- Short latency – reaction speed up to 50 milliseconds.
- Medium latency - reaction speed from 50 to 100 milliseconds.
- Long-latency - a reaction of 100 milliseconds and above.
A variation of this method is motor evoked potentials. They are fixed and removed from the muscles of the body in response to the action of electrical or magnetic influence on the nervous tissue of the motor area of the cerebral cortex. This technique is called transcranial magnetic stimulation. This technology is applicable in the diagnosis of diseases of the corticospinal tract, that is, the pathways that conduct nerve impulses from the cortex to the spinal cord.
The main properties that evoked potentials have are latency, amplitude, polarity and signal shape.
Decoding the results of recording the brain reaction
The results of the study of somatosensory evoked potentials are expressed in the form of an encephalogram - a curve compiled from measurements of the electrical potential of nerve tissue signals. The curve, as a rule, consists of peaks and valleys of different frequencies and amplitudes, the shape and repeatability of which can be used to judge the nature of its lesions. Thus, for multiple sclerosis, characteristic signs are a reduced amplitude of response signals by more than 60%, as well as an extended absolute and interpeak latency. In dementia, the amplitude of all significant peaks is reduced, and the latency is prolonged. In general, the method of recording somatosensory evoked potentials allows the neurologist to judge:
- nature and level of damage;
- severity of the disease;
- the spread of the process or its localization in certain areas;
- dynamics of the pathological process.
In addition, this diagnosis allows making predictions about the development of the disease and monitoring the effectiveness of treatment procedures.
Kinds
Each type implies not only a general, but also a specific approach to the study of the activity of the cortex.
Visual VPs
Visual evoked potentials of the brain are a method that involves recording the responses of the cerebral cortex to external stimuli, such as a flash of light. The procedure is as follows:
- Active electrodes are attached to the skin of the parietal and occipital region, and the reference (relative to which the measurement is taken) electrode is attached to the skin of the forehead.
- The patient closes one eye, and the gaze of the second is directed to the monitor, from where light stimulation is supplied.
- Then they change eyes and carry out the same experiment.
Auditory VPs
Acoustic evoked potentials appear in response to stimulation of the auditory cortex by alternating sound clicks. The sound is presented to the patient first to the left ear, then to the right. The signal level is displayed on the monitor and the results obtained are interpreted.
Somatosensory EPs
This method involves recording peripheral nerves that arise in response to bioelectrical stimulation. The technique consists of several stages:
- Stimulating electrodes are attached to the skin of the patient in the places where sensory nerves pass. Typically, such places are located in the wrist, knee or ankle area. Recording electrodes are attached to the scalp above the sensory area of the cerebral cortex.
- Start of nerve stimulation. There should be at least 500 acts of nerve irritation.
- Computers average the speed indicator and display the result in the form of a graph.
Normal visual evoked potentials
The analysis of VEP is carried out by the amplitude of potentials, measured in microvolts, by the form of recording and the time period from exposure to light to the appearance of peaks of VEP waves (calculated in milliseconds). Also pay attention to the difference in potential amplitude and latency value during light stimulation in the right and left eyes alternately.
In the VEP (what this is in ophthalmology is of interest to many) of the phasic type, during reversal with a low frequency of a chess pattern or in response to a light flash, P 100, a positive component, is released with particular constancy. The duration of the latent period of this component normally ranges from ninety-five to one hundred and twenty milliseconds (cortical time). The preceding component, that is, N 70, is from sixty to eighty milliseconds, and N 150 is from one hundred fifty to two hundred. Late P 200 is not recorded in all cases. This is how a computer vision test works.
Since the VEP amplitude is characterized by its variability, when taking into account the results of the study, it has a relative significance. Normally, the values of its value in relation to P 100 fluctuate in an adult from fifteen to twenty-five μV, higher potential values in children - up to forty μV. In response to pattern stimulation, the amplitude value of VEP is slightly lower and is determined by the size of the pattern. If the squares are larger, then the potential is higher, and vice versa.
Thus, evoked visual potentials are a reflection of the functional state of the visual pathways and allow us to obtain quantitative information during the study. The results make it possible to diagnose pathologies of the visual pathway in patients in the neuro-ophthalmological field.
This is how a person sees.
Diagnostics
Somatosensory evoked potentials are used in the diagnosis of various diseases of the nervous system, including degenerative, demyelinating, and vascular pathologies of nervous tissue. This method is also confirmatory in the diagnosis of polyneuropathy in diabetes mellitus.
Evoked brain potentials are an instrumental research technique that allows you to record the response of certain areas of the brain to external stimuli. Stimuli arrive through a group of receptors associated with a specific area of the cerebral cortex.
In a healthy state, the brain reacts clearly and with a certain speed to certain external irritating signals. With various disorders, the reaction may be delayed or differ in nature from the normal response. Evoked potentials can show at what stage of the excitation pathway an inhibition or signal change occurs.
Each group of receptors has its own types of stimuli, which are converted into excitation, which is transmitted along the pathways of the peripheral and autonomic nervous system to the brain. The purpose of the examination is to elicit a response to the appropriate signal. Electrical, acoustic and light effects are used as stimuli.
In a simplified version, the essence of the study comes down to analyzing the entire path from the receipt of a signal through the main sensory organs and skin receptors to the brain and the feedback response to the stimulus. According to the examination, it is possible to find exactly that part of the nervous system where the transmission of excitation from the peripheral nerves through the spinal cord to the cerebral cortex is inhibited.
SSEP study indicators and interpretation
- Latent period is the time between the beginning of the irritating effect and the maximum intensity of the response impulse. There are short-latency EPs (0.05 seconds or less), medium-latency (0.05 - 0.1 seconds) and long-latency (0.1 seconds or more).
- Oscillation amplitude is the difference between the maximum and minimum impulse levels.
- Polarity is the diametrically opposed reactions of symmetrical parts of the brain to one irritating impulse.
- Aftercharge is the time required for the response signal pulse to decay. Starts 0.3 seconds after the irritating signal is given, lasts from 0.5 seconds to 1 second.
There are visual, brainstem auditory, motor and somatosensory SSEPs. Each of them requires a separate study, but in general they give a complete picture of the state of the patient’s nervous system.
Indications for evoked potential studies
Using this examination, pathologies are diagnosed:
- vascular diseases (stroke);
- lesions of the central, peripheral and autonomic nervous system;
- consequences of traumatic brain injuries;
- attention deficit hyperactivity disorder (ADHD) in children;
- sensory disorders, etc.
Using the study of evoked potentials, it is possible to study nervous and brain functions in completely healthy people. In this form, the method is in demand in sports, scientific research and in assessing the rate of development of children, especially in premature infants.
In medical practice, three types of brain evoked potential studies are most often used:
- Visual evoked potentials: make it possible to observe the visual pathway from the retina to the corresponding part of the cerebral cortex. This examination is one of the most informative methods for diagnosing patients with signs of pathologies such as multiple sclerosis, temporal arteritis, inflammatory and tumor diseases, diabetes mellitus, lesions of the autonomic nervous system, optic nerves and retina. Based on the results of the study, a specialist can make a forecast of visual impairment in a number of diseases of various etiologies (neurological, vascular, endocrine).
- Auditory evoked potentials are one of the ways of central, peripheral and autonomic lesions of the acoustic system. As a result of the examination, it is possible to quite accurately determine the nature, degree and localization of disorders of the human auditory and vestibular system. The result of the study is of high value in the study of multiple sclerosis (even in the absence of external symptoms), diseases of the facial and trigeminal nerve, acoustic neuritis, otitis media, otosclerosis, vascular pathologies of the brain, hidden and deep tumor pathologies.
- Somatosensory evoked potentials are the study of the path of a nerve signal from receptors in the skin of the hands and feet to the cerebral cortex. The purpose of the examination is to assess the sensory pathways, analyze the functioning and safety of the nervous structures of the spinal cord and brain, identify the degree of impairment and check the effects of medication. This technique is used to diagnose various pathologies of the spinal cord, multiple sclerosis, diseases of the peripheral and autonomic nervous system (neuropathies, traumatic lesions of nerve tissue, etc.) Somatosensory evoked potentials are one of the most informative methods for studying spinal cord diseases and the best way to monitor the effectiveness of treatment .
How does registration work?
Registration of evoked visual potentials is carried out in the form of oscillations of the electrical potential of a sequential nature or components that differ in polarity: the negative potential, or N, is directed upward, the positive potential, that is, P, is directed downward. The VEP characteristic contains a form and two quantitative indicators. VEP potentials are normally much smaller in magnitude (up to about 40 μV) in comparison with electroencephalogram waves (up to 100 μV). The determination of latency is carried out using the time period from the moment the light stimulus is turned on until the maximum potential indicator is reached by the cerebral cortex. Most often, the potential reaches its maximum value after 100 ms. If there are various kinds of pathologies of the visual pathway, then the shape of the VEP changes, the amplitude of the components decreases, the latency lengthens, that is, the time during which the impulse travels to the cerebral cortex along the visual pathway increases.
In which lobe is the visual area located? It is located in the occipital lobe of the brain.
Methodology for studying evoked potentials
The patient is explained the essence and process of the examination - they are told that during the procedure he will be in a lying or reclining position. Depending on the nature of the study, electrodes are attached to the head, arms, legs, neck or lower back, which will not cause any harm or discomfort to the patient.
Such psychological preparation is necessary so that the patient is as relaxed and calm as possible. Any physical activity can lead to distorted results. All data from the sensors on the speed of the brain’s reaction is recorded, after which the doctor can compare the patient’s indicators with the norm and identify the nature of the lesion.
Where to do a somatosensory evoked potential examination in St. Petersburg
The Center for Neurology of Professor Zhulev invites residents and guests of St. Petersburg to register SSEP using modern diagnostic equipment, followed by interpretation of the results. The examination is necessary for the diagnosis and further treatment of a number of serious pathologies associated with damage to the functions of the nervous system and its tissues. The readings are interpreted by Doctor of Medical Sciences, Professor of Neurology Zhulev. Sign up for registration of somasosensory evoked potentials by phone or on our website using the feedback form.
Complications of evoked potential testing
If all the rules of the technique are followed, complications are extremely rare. In the presence of relative contraindications (angina pectoris, epilepsy, psychosis), attacks of hypertension, a mental attack, and a sharp increase in blood pressure are possible.
The brain is the body's holy of holies. His work takes place in the field of ultra-weak electrical discharges and ultra-fast pulses.
Analysis of auditory evoked potentials is indispensable when searching for causes and hearing in children, because make it possible to determine at what stage of sound signal transmission the failure occurs: either it is a peripheral disorder or a lesion of the central nervous system.
Evoked potentials of the auditory analyzer are included in the standard for examining infants for early diagnosis of developmental disorders.
If visual and auditory evoked potentials concerned only parts of the brain and brain stem, then somatosensory evoked reactions in the peripheral parts of the central nervous system.
A stimulating impulse along its path irritates many nerve centers and makes it possible to diagnose their functioning. This method is able to give a general picture of disorders of the central nervous system.
SSEP is prescribed to clarify the diagnosis and severity of the disease; to monitor the effectiveness of treatment; making a prognosis for the development of the disease.
Most often, two nerve centers are selected for stimulation: on the arm and on the leg:
- The median nerve on the wrist joint
, receiving an impulse, transmits it to a point above the brachial plexus (the 1st recording electrode is placed here); followed by a point above the seventh cervical vertebra (2nd electrode); frontal region; symmetrical points on both sides of the crown project the control centers of the right and left hands in the cerebral cortex. The response of the recorded nerve centers on the graph will be indicated by the symbols: N9 (brachial plexus response) → N11 (cervical spinal cord) → N29 – P25 (cerebral cortex). - Tibial nerve at the ankle joint
→lumbar spine →cervical spine →frontal part →vertex (projection of the center of the cortex that controls the lower limbs). This is the 2nd SSEP pathway.
The corresponding reactions are isolated by the method of summation and averaging from the overall EEG picture based on 500 - 1000 electrical impulses.
A decrease in the amplitude of SSEP components indicates pathology of the nerve centers in this place or below its level; an increase in the latent period indicates damage to the nerve fibers transmitting the impulse (demyelinating process); the absence of a reaction in the cerebral cortex in the presence of SSEP components in the peripheral centers of the nervous system diagnoses brain death.
In conclusion, it should be noted that the method of evoked potentials should primarily work for the early diagnosis of childhood diseases and developmental disorders, when proper treatment can reduce negative phenomena to a minimum. Therefore, it is useful for parents to know about its capabilities and take it into service in the fight for the health of their children.
Evoked potentials
Evoked potentials
- a method for studying the bioelectric activity of nervous tissue using visual and sound stimulation for the brain, electrical stimulation for peripheral nerves (trigeminal, median, ulnar, peroneal, etc.) and the autonomic nervous system. Evoked potentials make it possible to assess the state of the visual and auditory nerve pathways, deep sensitivity pathways (vibration sensitivity, pressure sensation, muscle-articular sensation), and study the functioning of the autonomic nervous system. Depending on the object of examination, visual, auditory, somatosensory, and skin evoked potentials are used.
When is it worth doing a study of somatosensory potentials?
The procedure is recommended for the following diseases:
- Multiple sclerosis, to assess subclinical dysfunction of nerve fibers.
- Disorders in the peripheral nervous system, to determine the degree of damage to nerve tissue.
- Lesions of the spinal cord, to localize the damaged parts.
- Epilepsy, to clarify the diagnosis and condition of the nerve tissues.
- Ischemic stroke, to identify subclinical lesions of the examined tissues.
- Brain death, to diagnose the condition.
In addition, the SSEP examination is part of a set of procedures necessary for diagnosing a number of other diseases: sensitivity disorders, polyneuropathy, neuroinfections, tumors and vascular diseases of the brain.
Indications
A study of visual evoked potentials is indicated if pathology of the optic nerve is suspected (tumor, inflammation, etc.). It allows you to identify deviations in the passage of a nerve impulse at any part of the visual path from the eye to the visual zone of the cerebral cortex. Clinical neurology attaches great diagnostic importance to identifying such damage to the optic nerve as retrobulbar neuritis, which is a typical symptom of multiple sclerosis. In cases of demyelinating diseases, when the destruction of the myelin sheath of the optic nerve occurs without clinical manifestations and is not visible on MRI of the brain, only visual evoked potentials are able to recognize nerve damage. This examination can be used to assess and predict visual impairment in temporal arteritis, hypertension, and diabetes mellitus.
Auditory evoked potentials are used to diagnose damage to the auditory pathway from the ear receptors to the auditory cortex. Such a study is indicated if a tumor, inflammatory lesion or demyelination of the auditory nerve is suspected. In patients with complaints of hearing loss, dizziness, tinnitus, and coordination problems, it allows one to determine the nature and level of damage to the auditory and vestibular analyzer.
Somatosensory evoked potentials are used to study the state of the pathways of the brain and spinal cord responsible for deep sensitivity (somatosensory analyzer). They make it possible to identify the pathology of deep sensitivity anywhere from the skin receptors of the extremities to the corresponding area of the cerebral cortex. This is of great importance in the diagnosis of polyneuropathy, demyelinating diseases, amyotrophic lateral sclerosis, funicular myelosis, Strumpel's disease, and various spinal cord lesions. The examination is indicated for patients with sensitivity disorders (pain, tactile, vibration, etc.), a feeling of numbness in the limbs, unsteady walking and dizziness.
If there are complaints of pain in the face, shooting headaches, toothache in the absence of dental pathology; if trigeminal neuralgia of any origin is suspected, examination using trigeminal evoked potentials is indicated. Skin evoked potentials are used to study the functional state of the autonomic nervous system (heart rate and respiration, sweating, vascular tone - blood pressure). Such a study is indicated for the diagnosis of autonomic disorders, which are early manifestations of vegetative-vascular dystonia, Raynaud's disease, Parkinson's disease, myelopathy, and syringomyelia.
Indications for diagnosing the brain using the VP method
Readings from the device used to perform the study are taken by attaching electrodes to the patient’s skin in certain places and measuring the electrical potential when stimuli are received. The taken indicators are processed by a computer program, which isolates the nerve fiber signal from the general noise background and depicts it as a curve on a graph. Using the device readings, the following are assessed:
- the degree of demyelination when it is necessary to diagnose spinal cord injury;
- functional loss of sensory sensitivity and preservation of nerve pathways;
- circulatory disorders of the spinal cord and its general condition;
- level of spinal cord damage in diagnosed myelopathy.
The recorded signals are compared with standard indicators, which makes it possible to judge disorders in the nervous system.
Contraindications
Pathological processes on the skin in this area are considered an absolute contraindication for the application of electrodes. Relative contraindications to this study are the presence of epilepsy, mental disorders, severe angina or hypertension, and a pacemaker in the patient. Complications can only arise if the study was used in the presence of relative contraindications. This could be an epileptic or mental attack, an attack of angina or a hypertensive crisis.
Methodology
No preparation required. On the day of the procedure, it is necessary to stop taking vascular drugs and tranquilizers, as they can distort the results of the examination. Flat electrodes lubricated with gel are applied to the patient’s head. They are connected to a device that records bioelectrical activity. When conducting a study using visual ERPs, the patient is asked to look at a TV screen that shows pictures (for example, a chessboard) or at flashes of bright light.
When conducting a study of auditory EPs, clicks and other sharp sounds are used. When studying somatosensory EPs, transcutaneous electrical stimulation of peripheral nerves is used. To study the function of the autonomic nervous system, electrical stimulation of the skin is performed. The device records changes in the bioelectrical activity of the cerebral cortex. Data on the conduction of nerve impulses arising after stimulation are processed on a computer.
Cost of evoked potentials in Moscow
The price of the study may fluctuate depending on several factors. The form of ownership of the medical and diagnostic institution has the greatest influence on the cost of the procedure. In private clinics, the price of evoked potentials in Moscow is usually higher than in public medical organizations. Differences in cost may also be due to different scope of the study (registration of visual, somatosensory, auditory, cutaneous and trigeminal potentials). In private medical centers, pricing is often based on the qualifications of the functional diagnostics doctor.
How is VP analyzed by a neurologist?
No special preparation is required for the examination. Follow the neurologist's recommendations:
- Before the examination, the patient removes all jewelry, watches and other metal objects from his body, and then lies down on the couch, supine or in a semi-sitting position.
- The doctor attaches electrodes to the patient's skin in places determined by the study design. Typically, electrodes are placed on the wrists, ankles and knees, on the head and back, and in some cases on other parts of the body.
- Stimulating impulses are alternately applied to the electrodes, under the influence of which peripheral nerve fibers transmit a signal to the muscles to contract. To obtain enough information, stimulation is carried out 200 to 500 times or even more. The duration of registration depends on its goals and objectives.
- The computer processes information from electrical sensors and calculates the average time it takes for the signal to reach the brain.
- The study is repeated to obtain a repeatable result and collect statistics.
- The electrodes on the patient's body are moved to diagnose the next section of nerve fibers and the procedure is repeated the required number of times.