Polyneuropathy is a disease that affects many peripheral nerves. Neurologists at the Yusupov Hospital determine the cause of the development of the pathological process, the localization and severity of damage to nerve fibers using modern diagnostic methods. Professors and doctors of the highest category take an individual approach to the treatment of each patient. Complex therapy of polyneuropathies is carried out with effective drugs registered in the Russian Federation. They have a minimal range of side effects.
The following types of neuropathies are registered in the International Classification of Diseases (ICD), depending on the cause and course of the disease:
- inflammatory polyneuropathy (ICD code 10 - G61) is an autoimmune process that is associated with a constant inflammatory reaction to various stimuli of a predominantly non-infectious nature (includes serum neuropathy, Guillain-Barré syndrome, a disease of an unspecified nature);
- ischemic polyneuropathy of the lower extremities (ICD code also G61) is diagnosed in patients with impaired blood supply to nerve fibers;
- drug-induced polyneuropathy (ICD code G.62.0) – the disease develops after long-term use of certain drugs or against the background of incorrectly selected doses of drugs;
- alcoholic polyneuropathy (ICD code G.62.1) – the pathological process is provoked by chronic alcohol intoxication;
- toxic polyneuropathy (ICD10 code – G62.2) is formed under the influence of other toxic substances, and is an occupational disease of workers in the chemical industry or those in contact with toxins in the laboratory.
Polyneuropathy, which develops after the spread of infection and parasites, has the code G0. The disease with the growth of benign and malignant neoplasms is encrypted in ICD 10 with code G63.1. Diabetic polyneuropathy of the lower extremities has an ICD 10 code G63.2. Complications of endocrine diseases and metabolic disorders in ICD-10 are assigned code G63.3. Dysmetabolic polyneuropathy (ICD 10 code - G63.3) is classified as polyneuropathies in other endocrine diseases and metabolic disorders.
Forms of neuropathy depending on the prevalence of symptoms
The classification of polyneuropathy according to ICD 10 is officially recognized, but it does not take into account the individual characteristics of the course of the disease and does not determine treatment tactics. Depending on the predominance of clinical manifestations of diseases, the following forms of polyneuropathies are distinguished:
- sensory – signs of involvement of sensory nerves in the process (numbness, burning, pain) predominate;
- motor – signs of damage to motor fibers prevail (muscle weakness, decrease in muscle volume);
- sensorimotor – symptoms of damage to motor and sensory fibers are simultaneously present;
- autonomic – there are signs of involvement of the autonomic nerves in the process: dry skin, rapid heartbeat, tendency to constipation;
- mixed - neurologists determine signs of damage to all types of nerves.
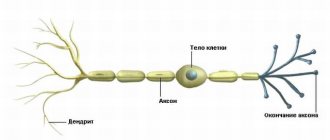
With primary damage to the axon or neuron body, axonal or neuronal polyneuropathy develops. If Schwann cells are affected first, demyelinating polyneuropathy occurs. In the case of damage to the connective tissue sheaths of the nerves, they speak of infiltrative polyneuropathy, and if the blood supply to the nerves is impaired, ischemic polyneuropathy is diagnosed.
Polyneuropathies have various clinical manifestations. The factors that cause polyneuropathy most often first irritate the nerve fibers, causing symptoms of irritation, and then lead to disruption of the function of these nerves, causing “prolapse symptoms.”
Folk remedies
The essence of pathology
All of the above conditions also affect the severity of the disease - older people experience pain much more severely than younger people. An important role is also played by where exactly the lichen was localized - if in the head area, then the pain will be much stronger than if the lichen had formed on the body.
With shingles, where viral cells get too close to the surface, a rash, itching and other symptoms of this disease appear. Skin rashes go away quite quickly, and the skin itself also quickly recovers, but the nerve cells at this time remain injured, which results in severe pain. These symptoms are symptoms of postherpetic neuralgia. Many people are interested in how long postherpetic neuralgia lasts.
This disease can last from several months to several years and, on the contrary, in many cases it was possible to overcome this disease in a very short time.
It has been established that most of those who suffered from chickenpox in childhood can subsequently develop shingles. But it is not a fact that all those who have had herpes zoster will subsequently develop postherpetic neuralgia. Here are a few circumstances that determine whether a person gets postherpetic neuralgia or not:
- Age. The reason is not only the weakening of the immune system in adulthood, but also the wear and tear of the nervous system. The risk of developing postherpetic neuralgia in older people is 35-40%, in young people - 10%.
- The existence of other diseases during the illness with herpes zoster. The immune system spends reserves to cure another disease, so the likelihood of developing postherpetic neuralgia increases several times.
- Places where shingles has manifested itself. If it is the face or neck, the likelihood of postherpetic neuralgia is predominantly higher than if the rash were on the ribs.
The main symptom of the pathology is a feeling of pain in the area where the rash was during shingles. Pain may last from several months to several years. The nature of the pain can be of several types:
- constant dull and pressing pain;
- periodic pain that occurs unexpectedly, resembles an electric shock;
- allodynic pain arising from any, even the slightest touch.
Some patients experience all of these types of pain simultaneously.
Even if the affected area is numb, it still does not lose its sensitivity and reacts to all touches.
Constant or periodic pain in a person negatively affects other areas of his life. This shows up:
- insomnia;
- prolonged fatigue;
- decline in physical activity;
- decreased need for food;
- feeling of hypochondria;
- inactivity and indifference to everything.
As is already known, the best prevention of postherpetic neuralgia is the prevention of herpes zoster.
To do this you need:
- prevent primary chickenpox infection by promptly vaccinating children.
- use drugs that increase immunity for people who have been in contact with those who have recently had chickenpox or shingles.
- Provide shingles vaccines to those over 60.
- the use of antiviral drugs such as acyclovir, valacyclovir, famciclovir, the use of these drugs during the first three days after the first rash of herpes zoster appears, will help to recover from this disease more quickly and reduce the risk of developing postherpetic neuralgia.
Features of therapy
Therapy for postherpetic neuralgia today is pain relief. For this purpose, drugs such as aspirin, Panadol, ibuprofen, naproxen, Celebrex are used. In those moments when the pain becomes especially severe, the use of medications such as tramadol and oxycodone is recommended. It is also possible to use such means as:
- Anticonvulsants - Topamax, Neurontin - these drugs should be taken when involuntary reactions develop due to damaged nerves.
- Antidepressants - Cymbalta, amitriptyline. Relieves symptoms of stress during severe pain.
- Various ointments, gels and tinctures. Used during mild pain.
- Blockades based on corticosteroids are dangerous, but at the same time very effective.
- Acupuncture. It often happens that after using acupuncture, the pain subsides and no additional medications are needed.
It often happens that after preventive measures, treatment may not even be required, since the disease recedes.
For somatic diseases
Diabetic polyneuropathy (ICD10 code G63.2.) is one of the most common and studied forms of somatic polyneuropathies. One of the manifestations of the disease is autonomic dysfunction, which has the following symptoms:
- orthostatic arterial hypotension (decrease in blood pressure when changing body position from horizontal to vertical);
- physiological fluctuations in heart rate;
- disorders of gastric and intestinal motility;
- bladder dysfunction;
- changes in sodium transport in the kidneys, diabetic edema, arrhythmias;
- erectile disfunction;
- skin changes, impaired sweating.
With alcoholic polyneuropathy, paresthesia in the distal limbs and pain in the calf muscles are noted. One of the early characteristic symptoms of the disease is pain, which intensifies with pressure on the nerve trunks and compression of the muscles. Later, weakness and paralysis of all extremities develop, which are more pronounced in the legs, with predominant damage to the extensors of the foot. Atrophy of paretic muscles develops rapidly, periosteal and tendon reflexes are strengthened.
In the later stages of development of the pathological process, muscle tone and muscle-joint sensation decrease, and the following symptoms develop:
- surface sensitivity disorder of the “gloves and socks” type;
- ataxia (instability) in combination with vasomotor, trophic, secretory disorders;
- hyperhidrosis (increased skin moisture);
- swelling and pallor of the distal extremities, decreased local temperature.
Hereditary and idiopathic polyneuropathy (code G60)
Hereditary polyneuropathy is an autosomal dominant disease with systemic damage to the nervous system and varied symptoms. At the onset of the disease, patients experience fasciculations (visible contractions of one or more muscles) and spasms in the muscles of the legs. Next, atrophy and weakness develop in the muscles of the feet and legs, a “hollow” foot and peroneal muscular atrophy are formed, the legs resemble the limbs of a stork.”
Later, movement disorders in the upper extremities develop and increase, and difficulties arise in performing small and routine movements. Achilles reflexes are lost. The preservation of other groups of reflexes varies. Vibration, tactile, pain and muscle-joint sensitivity decreases. In some patients, neurologists determine thickening of individual peripheral nerves.
The following types of hereditary neuropathies are distinguished:
- sensory radiculopathy with disorders of the functions of peripheral nerves and spinal ganglia;
- atactic chronic polyneuropathy - Refsum's disease.
- Bassen-Kornzweig disease is a hereditary acanthocytotic polyneuropathy caused by a genetic defect in lipoprotein metabolism;
- Guillain–Barré syndrome – unites a group of acute autoimmune polyradiculoneuropathies;
- Lhermitte syndrome, or serum polyneuropathy, develops as a complication of serum administration.
Neuropathologists also diagnose other inflammatory polyneuropathies that develop from insect bites, after administration of anti-rabies serum, rheumatism, systemic lupus erythematosus, periarteritis nodosa, as well as neuroallergic and collagenoses.
Drug-induced polyneuropathy (ICD code G.62.0)
Drug-induced polyneuropathy occurs as a result of metabolic disorders in myelin and feeding vessels as a result of taking various medications: antibacterial drugs (tetracycline, streptomycin, kanamycin, viomycin, dihydrostreptolysin, penicillin), chloramphenicol, isoniazid, hydralazine. Antibacterial polyneuropathies with symptoms of sensory neuropathy, night pain in the limbs and paresthesias, vegetative-trophic dysfunctions are detected not only in patients, but also in workers of factories that produce these medications.
At the initial stage of development of isoniazid polyneuropathy, patients are bothered by numbness of the fingers, then a burning sensation and a feeling of tightness appear in the muscles. In advanced cases of the disease, ataxia joins sensory disorders. Polyneuropathies are detected when taking contraceptives, antidiabetic and sulfa drugs, phenytoin, drugs of the cytotoxic group, and the furadonin series.
The essence of pathology
With shingles, where viral cells get too close to the surface, a rash, itching and other symptoms of this disease appear. Skin rashes go away quite quickly, and the skin itself also quickly recovers, but the nerve cells at this time remain injured, which results in severe pain. These symptoms are symptoms of postherpetic neuralgia. Many people are interested in how long postherpetic neuralgia lasts.
This disease can last from several months to several years and, on the contrary, in many cases it was possible to overcome this disease in a very short time.
Diagnostics
Neurologists make a diagnosis of polyneuropathy based on:
- analysis of complaints and how long ago symptoms appeared;
- clarification of possible causative factors;
- establishing the presence of diseases of internal organs;
- establishing the presence of similar symptoms in close relatives;
- identifying signs of neurological pathology during a neurological examination.
An obligatory component of the diagnostic program is an examination of the lower extremities in order to identify autonomic failure:
- thinning of the skin of the legs;
- dryness;
- hyperkeratosis;
- osteoarthropathy;
- trophic ulcers.
During a neurological examination, if the nature of the polyneuropathy is unclear, doctors palpate the available nerve trunks.
To clarify the cause of the disease and changes in the patient’s body, the Yusupov Hospital determines the levels of glucose, glycated hemoglobin, protein metabolic products (urea, creatinine), perform liver tests, rheumatic tests, and toxicological screening. Electroneuromyography allows one to evaluate the speed of impulse transmission along nerve fibers and determine signs of nerve damage. In some cases, a nerve biopsy is performed for examination under a microscope.
If there are indications, instrumental methods for studying the somatic status are used: radiography, ultrasound. Cardiointervalography allows identifying violations of autonomic function. A study of cerebrospinal fluid is carried out if demyelinating polyneuropathy is suspected, and when searching for infectious agents or an oncological process.
Vibration sensitivity is examined using a biotensiometer or a graduated tuning fork with a frequency of 128 Hz. The study of tactile sensitivity is carried out using hair monofilaments weighing 10 g. Determination of the threshold of pain and temperature sensitivity is carried out using a needle prick and a Tip-therma thermal tip in the skin of the dorsal surface of the big toe, dorsum of the foot, medial surface of the ankle and lower leg.
Causes
There are several groups of triggers that can initiate the development of peroneal neuropathy: nerve injury; compression of the nerve by the surrounding musculoskeletal structures; vascular disorders leading to nerve ischemia; infectious and toxic lesions. Neuropathy of the peroneal nerve of traumatic origin is possible with knee bruises and other injuries of the knee joint, tibia fracture, isolated fracture of the fibula, dislocation, tendon damage or sprain of the ankle joint, iatrogenic damage to the nerve during reposition of the leg bones, operations on the knee joint or ankle. Compressive neuropathy (so-called tunnel syndrome) n peroneus most often develops at the level of its passage at the head of the fibula - superior tunnel syndrome. It may be associated with professional activities, for example, among berry pickers, parquet floor workers, etc., people whose work involves squatting for a long time. Such neuropathy is possible after prolonged sitting with legs crossed. When the peroneal nerve is compressed where it exits the foot, inferior tunnel syndrome develops. It may be caused by wearing excessively tight shoes. Often the cause of peroneal compression neuropathy is compression of the nerve during immobilization. In addition, compression of the n peroneus may have a secondary vertebrogenic nature, i.e., develop in connection with changes in the musculoskeletal system and reflex muscular-tonic disorders caused by diseases and curvatures of the spine (osteochondrosis, scoliosis, spondyloarthrosis). Iatrogenic compression-ischemic neuropathy of the peroneal nerve is possible after its compression due to incorrect position of the leg during various surgical interventions. More rare causes of peroneal neuropathy include systemic diseases accompanied by proliferation of connective tissue (deforming osteoarthritis, scleroderma, gout, rheumatoid arthritis, polymyositis), metabolic disorders (dysproteinemia, diabetes mellitus), severe infections, intoxication (including alcoholism, drug addiction), local tumor processes.
Bibliography
- ICD-10 (International Classification of Diseases)
- Yusupov Hospital
- Batueva E.A., Kaygorodova N.B., Karakulova Yu.V. The influence of neurotrophic therapy on neuropathic pain and the psycho-vegetative status of patients with diabetic neuropathy // Russian Journal of Pain. 2011. No. 2. P. 46.
- Boyko A.N., Batysheva T.T., Kostenko E.V., Pivovarchik E.M., Ganzhula P.A., Ismailov A.M., Lisinker L.N., Khozova A.A., Otcheskaya O .V., Kamchatnov P.R. Neurodiclovit: possibility of use in patients with back pain // Farmateka. 2010. No. 7. pp. 63–68.
- Morozova O.G. Polyneuropathy in somatic practice // Internal medicine. 2007. No. 4 (4). pp. 37–39.