Axonopathy is a disorder in which the processes of nerve cells are affected. They are located throughout the body, so the symptoms of the disease can vary.
Axonal damage is classified as a group of polyneuropathies. The disease is considered a slowly developing degenerative process. A neurologist treats axonopathies.
Like all disorders of the peripheral nervous system, the disease is manifested by impaired movement and sensitivity, and autonomic symptoms. With adequate treatment, degeneration can be stopped, thereby improving the prognosis for life.
Axonopathy - characteristic signs and treatment methods
Axonopathy is a disorder in which the processes of nerve cells are affected.
They are located throughout the body, so the symptoms of the disease can vary. Axonal damage is classified as a group of polyneuropathies. The disease is considered a slowly developing degenerative process. A neurologist treats axonopathies. Like all disorders of the peripheral nervous system, the disease is manifested by impaired movement and sensitivity, and autonomic symptoms. With adequate treatment, degeneration can be stopped, thereby improving the prognosis for life.
Peroneal nerve neuropathy: symptoms and treatment
The appearance of pain in the lower leg or foot is often a symptom of peroneal nerve neuropathy. The pathology is not life-threatening if it is identified and treated in a timely manner. However, it can cause a lot of discomfort and limit physical activity. Especially in children. Therefore, you should not delay seeking medical help.
Anatomical parameters
To better understand peroneal nerve neuropathy, it is necessary to have a general understanding of its anatomical features.
In general, this structural unit of the peripheral nervous system is just a part of the sciatic nerve, which continues after leaving the sacral nerve plexus.
Towards the lower third of the thigh it will be divided into 2 segments - the peroneal nerve and also the tibial nerve.
After crossing the fossa below the knee, the fibular fiber reaches the head of the bony unit of the same name. Then it bifurcates again - into superficial and also deep branches. Therefore, by the localization of pathological symptoms, one can judge the level where the pathological lesion is located - to distinguish between neuropathy of the tibial nerve or the peroneal segment.
Thus, the deep peroneal nerve, moving through the anterior zone of the leg, reaches the back of the unilateral foot, where it bifurcates again. He is responsible for the dorsal movement of the foot in one plane, as well as raising its outer edge.
While the superficial branch, innervating the anterolateral part of the limb, is responsible for raising and simultaneous flexion of the foot.
The last division of the small tibial nerve is carried out in the area of the medial third of the leg - into two cutaneous dorsal nerves.
When examined by characteristic changes, a neurologist will differentiate neuropathy of the tibial nerve from neuritis of the peroneal nerve. Skin and muscle susceptibility, arbitrariness of movements and accuracy of reflexes are assessed - axonal damage will lead to neuritis of the tibial nerve, as well as the peroneal branch.
Causes
The development of a pathological focus in a nerve fiber can occur for many reasons. Most often, specialists diagnose the following:
- various injuries of the peroneal nerve - direct injury to the limb, or compression by colloid cords after surgical interventions, simultaneously with damage to the tibial nerve;
- compression of the nerve as a result of tunnel syndrome - typical for people whose profession requires them to be in a position for a long time that is uncomfortable for the lower extremities, for example, parquet layers, seamstresses;
- vascular pathologies and other blood supply disorders that lead to tissue hypoxia - a decrease in the number of oxygen molecules in them and, accordingly, a failure of metabolic processes;
- lesions of the peroneal nerve of a toxic nature - diabetic, renal, as a rule, have a symmetrical nature of the “golf” type;
- infections - involving one of the branches of the fibular fiber in the inflammatory process, or even simultaneously with inflammation of the tibial nerve;
- compression-ischemic neuropathy occurs with tumor neoplasms - as the tumor grows and metastasizes.
Less commonly, polyneuropathy of a traumatic nature is the result of systemic diseases. For example, gout, osteoarthritis or rheumatoid arthritis.
Symptoms
Since the peroneal nerve has a significant length, the clinical picture will directly depend on the level at which the pathological focus arose.
Thus, when the fiber is compressed in the area of the knee fossa, the sensitivity of the skin on the anterolateral surface of the leg, as well as the foot, will be impaired. People stop perceiving touch or temperature fluctuations in the air. Unpleasant symptoms intensify when trying to sit down.
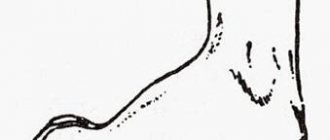
Among the motor disorders, difficulty in straightening the foot is typical. It is impossible to lift exactly its outer edge.
At the same time, the ability to move on the heels is lost. Another typical sign is “horse foot”. It hangs directly down, and when walking you need to raise your leg too high.
Otherwise, your fingers will cling to the floor. Visually this appears as a “horse gait”.
With a prolonged and uncontrolled course, tunnel syndrome will be complicated by muscle atrophy - the limb is smaller in volume.
When the peroneal superficial branch is injured, the symptoms are somewhat different:
- burning and discomfort in the lower area of the leg, as well as the foot and fingers from I to IV;
- failure of sensitivity in these same structures;
- a person experiences difficulty in raising and abducting the outer edge of the foot.
When the deep peroneal branch of the nerve is involved in neuropathy, the muscles that are responsible for straightening the foot, as well as its toes, suffer from slight drooping. Sensitivity is impaired between fingers I and II on the back.
Diagnostics
Early seeking medical help for neuropathy is the key to success in the fight against pathology. During the examination, the specialist determines the extent of sensory and motor disorders. In order to confirm a preliminary diagnosis, it is necessary to perform the following studies:
- electromyography – conduction of an impulse along a nerve fiber;
- Ultrasound – examination of soft tissues and choroid plexuses;
- magnetic resonance or computed tomography - study of images in which all structures of the lower extremities are depicted in different planes to clarify the localization of the pathological focus and its size;
- for injuries - radiography;
- various blood tests - general, biochemical, hormonal parameters and tumor markers.
The specialist will carry out differential diagnosis with infectious lesions and injuries, cancer formations and toxic effects on the human body. A thorough analysis of diagnostic information and identification of the causes of the pathology facilitates the selection of a treatment regimen.
Treatment tactics
When identifying this disease in people, the efforts of specialists will be aimed at eliminating the factors that provoke it - the causes of compression and inflammation. Conservative therapy is the first step in correcting the pathological situation.
The doctor selects drugs from the following subgroups:
- NSAIDs – Nimesulide, or Ibuprofen, Airtal;
- drugs for correcting conductivity in the nerve fiber - Proserin or Neuromidin;
- vitamin therapy - Milgamma or Combilipen;
- means for correcting blood circulation - Trental, Curantil;
- antioxidants – Cerebralysin, Actovegin.
To restore movement function and skin sensitivity, specialists will select physical procedures:
- magnetic therapy and electrophoresis;
- ultrasound and electrical stimulation.
Massage has proven itself to be excellent for neuropathies of the peroneal nerve. It is carried out in courses, the duration of which depends on the severity of the lesion. The help of physical therapy is invaluable - the patient begins to perform exercises under the guidance of an employee of the exercise therapy room, and then continues independently at home.
In case of traumatic or tumoral nature of compression of the peroneal nerve, one type of surgical treatment is indicated. After which a course of rehabilitation therapy is required.
Prognosis and prevention
In general, the prognosis for neuropathies is favorable - with their timely detection and comprehensive treatment, it is possible to completely restore both motor and sensory functions.
Complications appear only when a person contacts a neurologist late - at the stage of atrophy and severe pain syndrome. There is a loss of movement in the foot and ability to work. Disability sets in.
To prevent severe complications, experts recommend preventive measures:
- purchase and wear comfortable shoes;
- avoid staying in a position that is uncomfortable for the feet for a long time;
- When playing sports, follow safety rules to avoid injuries, even minor ones;
- reduce the load on the ankle joint if it is used throughout the entire working day - do warm-up and exercises;
- pamper your feet with baths with plant extracts - before bed;
- eat right - your diet contains more vegetables and fruits with B vitamins.
Damage to the peroneal nerve is not a death sentence. They can and should be fought. The health of every person is in his own hands.
Source: https://nerv-info.ru/perifericheskaya-nervnaya-sistema/nejropatiya-malobertsovogo-nerva-ee-prichiny-i-sposoby-lecheniya
Causes and pathogenesis of the disease
Damage to peripheral nerve processes can develop due to the following reasons:
- Chemical poisoning . With prolonged exposure to poison on the body, a disruption of the intracellular metabolism of neurons occurs, as a result of which a deficiency of essential nutrients develops and the tissue undergoes degeneration. Toxic substances include: methyl alcohol, carbon monoxide, arsenic.
- Endocrine disorders . Due to hormonal imbalance, metabolic processes in the body slow down. This affects all functions, including the transmission of nerve impulses along axons.
- Vitamin deficiency . Lack of nutrients leads to slowly progressive destruction of peripheral processes.
- Chronic intoxication with ethyl alcohol . Axonopathy often develops in individuals who have suffered from alcoholism for several years.
The mechanism of occurrence of disturbances in axons is considered at the cellular level. In the peripheral processes there are no organelles that produce protein compounds (EPS, ribosomes). Therefore, for the functioning of the peripheral parts, nutrients come from the cell body (neuron). They move to axons using special transport systems. Under the influence of toxic substances or hormonal changes, the flow of proteins to the periphery is disrupted.
The pathological condition can also arise due to insufficient energy production in the mitochondria, which leads to disruption of the anterograde transport of phospholipids and glycoproteins. Degeneration is especially pronounced in long axons. For this reason, the main symptoms of the disease are felt in the distal parts of the extremities.
Damage to the peripheral processes gradually leads to the death of the entire cell. In this case, it is impossible to restore functions. If the body of the neuron remains intact, then regression of the pathology is possible.
Axonal Polyneuropathy – chronic, motor, acute
20.03.2019
Axonal polyneuropathy is a pathology of the peripheral nervous system that develops as a result of damage to the peripheral nerves. The pathology is based on damage to axons, myelin sheaths or nerve cell bodies. Axonal polyneuropathy disables the patient and develops severe complications: diabetic foot syndrome, paralysis, anesthesia.
Polyneuropathy is manifested by a decrease in muscle strength, impaired sensitivity and local autonomic lesions in the area of neuropathy. Typically, nerves are affected symmetrically in distant parts of the body: arms or legs. As the lesion progresses, it smoothly moves to nearby areas: foot → ankle → lower leg → thigh → pelvis.
Causes
Polyneuropathy is caused by the following reasons:
- Chronic diseases: diabetes mellitus (50% of all cases of neuropathy), HIV infection (HIV-infected people develop polyneuropathy in 30% of cases), tuberculosis.
- Acute intoxication: arsenic, methyl alcohol, organophosphorus compounds, carbon monoxide, chronic alcohol consumption (develops in 50% of alcoholics).
- Metabolic conditions: deficiency of B vitamins, uremia.
- Long-term use of medications: Isoniazid, Metronidazole, Vincristine, Dapsone.
- Hereditary predisposition, autoimmune diseases.
The above factors cause endogenous and exogenous intoxication. Metabolic and ischemic disorders occur in the nerve. The nerve tissue and, secondarily, the myelin sheath are damaged.
Toxic compounds that come from the external environment affect the peripheral nerve with metabolites. More often this happens with liver failure, when unprocessed dangerous chemical compounds accumulate in the bloodstream, with lead, lithium and arsenic poisoning.
Among endogenous intoxications, metabolic disorders and accumulation of toxic substances in diabetes mellitus and renal failure are more common. As a result, the cylindrical axis of the axon is affected.
Damage to the peripheral nerve due to endogenous intoxication can reach the point where sensitivity is completely lost.
This is demonstrated in electroneuromyography when a stimulus is applied to the skin but there is no sensory response in the nerve.
With strong exposure to chemical agents, complex axonal demyelinating polyneuropathy develops.
Axonal demyelinating polyneuropathy occurs against the background of uremic intoxication, severe lead poisoning, and chronic use of Amiodarone in non-therapeutic doses.
The most severe lesions are observed in insulin-requiring diabetes mellitus, when malignant glucose levels are observed in the blood.
Symptoms
The clinical picture develops slowly. Signs are divided into groups:
- Autonomic disorders. Axonal polyneuropathy of the lower extremities is manifested by local sweating of the legs, hot flashes, and cold snaps.
- Sensory impairments. Manifested by a decrease in tactile and temperature sensitivity. The threshold for sensitivity to low temperatures increases: the patient can hold his foot in the cold for a long time and not feel it, which is why he gets frostbite. Paresthesia often occurs: numbness, crawling sensation, tingling.
- Pain syndrome. It is characterized by neuropathic aching or sharp, electric shock-like pain in the affected area.
- Motor disorders. Due to damage to the nerve and myelin sheaths, motor activity is disrupted: muscles weaken and atrophy, even to the point of paralysis.
Positive (productive) symptoms are identified: convulsions, fine tremors, twitching (fasciculations), restless legs syndrome.
Axonal sensorimotor polyneuropathy is manifested by systemic symptoms: increased blood pressure and heart rate, pain in the intestines, excessive sweating, frequent urination.
Axonopathies are acute, subacute and chronic. Acute axonal polyneuropathy develops against the background of heavy metal poisoning, and the clinical picture develops in 3-4 days.
Subacute neuropathies develop over 2-4 weeks. Subacute course is characteristic of metabolic disorders.
Chronic axonopathies develop over a period of 6 months to several years. Chronic axonal polyneuropathy is characteristic of alcoholism, diabetes mellitus, liver cirrhosis, cancer, uremia. A chronic course is also observed with uncontrolled use of Metronidazole, Isoniazid, Amiodarone.
Diagnosis and treatment
Diagnosis begins with collecting anamnesis. The circumstances of the disease are clarified: when the first symptoms appeared, how they manifested themselves, whether there was contact with heavy metals or poisoning, what medications the patient is taking.
Concomitant symptoms are examined: are there any coordination problems, mental disorders, decreased intelligence, what size are the lymph nodes, complexion.
Blood is collected and sent: the glucose level, the number of red blood cells and lymphocytes are examined. The level of calcium, glucose, urea and creatinine is examined in the urine.
Liver samples are collected through a biochemical blood test to determine whether the liver is affected.
The patient is prescribed instrumental diagnostics:
- Electromyography: the reaction of nerve fibers to a stimulus is studied, the activity of the autonomic nervous system is assessed.
- X-ray of the chest organs.
- Cutaneous nerve biopsy.
Treatment of axonal neuropathy:
- Etiological therapy. Aimed at eliminating the cause. If it is diabetes mellitus, normalize the blood glucose level; if it is alcoholism, stop drinking alcohol.
- Pathogenetic therapy. Aimed at restoring nerve function: B vitamins and alpha-lipolyic acid are introduced. If this is an autoimmune disease, corticosteroids are prescribed - they block the pathological effect on myelin and nerve fibers.
- Symptomatic therapy: pain syndrome is eliminated (antidepressants, opioid narcotic analgesics).
- Rehabilitation: physiotherapy, physical therapy, occupational therapy, massage.
The prognosis is conditionally favorable: when glucose levels are normalized, pathological mechanisms are eliminated and medical recommendations are followed, reinnervation occurs - sensitivity and movement are gradually restored and autonomic disorders go away.
Didn't find a suitable answer? Find a doctor and ask him a question!
Source: https://sortmozg.com/zabolevaniya/aksonalnaya-polinejropatiya
Risk factors
Disruption of cellular metabolism does not occur without a reason.
In some cases, it seems that there was no provoking factor, but this is not the case.
Thus, subacute and chronic variants of axonopathy develop. In these cases, degeneration occurs gradually.
Risk factors for the occurrence of a pathological process include:
- chronic intoxication, which is not always noticeable - it affects people who work in hazardous industries, take medications for a long time, and live in unfavorable conditions;
- the presence of inflammatory neurological diseases caused by infectious agents;
- oncological pathologies;
- chronic diseases of internal organs;
- alcohol abuse.
Types of pathological condition
There are 3 types of axonopathy, which differ in the mechanism of development, severity of the clinical picture and etiological factor.
- Type 1 disorder refers to acute degenerative processes; the disease occurs when the body is seriously poisoned.
- The subacute pathological process is characterized by type 2 , which is caused by metabolic disorders. Often, this is diabetes mellitus, gout, etc.
- Peripheral process degeneration type 3 develops more slowly than other variants of the disease. This type of disease is often observed in people with weakened immune systems and those suffering from alcoholism.
Clinical manifestations
The initial symptom of axonopathy is a decrease in sensitivity, which occurs gradually. Clinical picture
characterized by a feeling of pins and needles in the foot and hand, numbness of the fingers. Then there is a complete loss of deep sensitivity like “socks” and “gloves”. As the pathological condition progresses, a person may not feel pain and temperature stimuli.
A pronounced degenerative process is manifested by motor disorders. The patient is worried about weakness and lameness. In the terminal stage of the disease, peripheral paralysis and paresis develop. Tendon reflexes are weakened or not evoked at all.
Axons of the lower and upper extremities and cranial nerves undergo degeneration. Axonopathy of the peroneal nerve is expressed by the following symptoms:
- the motor activity of the leg suffers - the process of flexion and extension is disrupted;
- there is no pronation and supination;
- The strength in the calf muscles decreases, as a result of which a change in gait occurs.
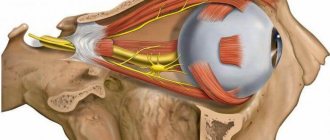
Damage to the oculomotor nerve leads to strabismus and ptosis. There may be a decrease in visual acuity and a narrowing of the field of view.
If the phrenic nerve is involved in the degenerative process, then a characteristic Horner's syndrome occurs, which is characterized by the development of ptosis, miosis and enophthalmos (retraction of the eyeball).
When the vagus nerve is damaged, the innervation of internal organs is disrupted, clinically this is manifested by tachycardia and increased respiratory rate.
Peroneal nerve axonopathy treatment
The deep peroneal nerve plays an important anatomical role; the health and sensitivity of the legs right down to the fingertips depends on its proper functioning. Since any violations in this area lead to problems, it is worth considering possible diseases of the peroneal nerve and methods of their treatment.
This segment of the nervous system originates in the area of the sciatic nerve, entering its composition with some of its fibers, and then separates into an independent branch. First, the peroneal nerve innervates the muscles up to the knee in the form of a single canal, passing to the fibula, and then divides into 3 fibers: superficial, external and internal.
Anatomy of the peroneal nerve
The superficial fiber is located above the lower leg. It is responsible for the functioning of the muscles in this area and the mobility of the foot.
The inner fiber is located under the shin. It allows for flexion and extension of the toes.
Pathologies of the peroneal nerve are associated with pinching of one or several fibers at once. Such a problem can lead to impaired functioning of the leg below the knee, including paralysis of the foot.
Causes of peroneal nerve diseases
Innervation may be disrupted for the following reasons:
- leg fractures with pinched nerve;
- compression of the canal or fiber;
- excessive physical activity;
- problems with blood circulation;
- disorders of the nervous system;
- complications of cancer;
- temperature violations;
- toxic poisoning of the body.
All types of diseases can be divided into two categories. Primary ailments are those disorders that do not depend on other processes occurring in the human body. These include injuries to the limbs or excessive physical activity, especially if it is carried out on only one leg.
Secondary diseases manifest themselves as complications of existing ailments, and therefore require complex treatment. First of all, this is the treatment of the underlying disease, and then the restoration of the functioning of the nerve.
Types of diseases
The main cause of problems with the peroneal nerve is compression or pinching; based on additional symptoms and circumstances of the lesion, a number of diseases associated with this condition are distinguished:
- osteopathy;
- benign bone tumors;
- synonymous inflammatory process in the area of the synovial membrane;
- fractures or dislocations in the ankle area;
- bruises of the legs below the knee;
- tenosynovitis;
- inflammation of the membrane located inside the joint;
- a complication of osteoarthritis - inflammation of joint tissue and cartilage;
- inflammation of the joint capsule (bursitis);
- arthrosis, manifested as a consequence of injury;
- neuropathy;
- neuralgia;
- Nerve damage during leg surgery.
Any disorder involving the peroneal nerve will cause similar symptoms. The limbs below the knee will be less sensitive and mobile than usual.
The patient will experience periodic sharp pain.
Like any other disease, such problems lead to a deterioration in the general condition of the body.
Diagnosis of dysfunction of the peroneal nerve
First of all, it is necessary to identify the specific point of compression of the nerve and the cause of the development of the pathology. A set of techniques is used for this.
- The doctor will conduct an examination, check sensitivity and evaluate the functionality of the limbs. After testing for reflexes, the approximate location of the lesion and the degree of development of the pathology will be clear.
- The specialist will prescribe an ultrasound of the peroneal nerve. This will help identify concomitant ailments and choose the optimal treatment method. In complex situations, MRI can provide an accurate clinical picture.
- Collect information about past injuries and existing chronic diseases. This will help determine whether problems with the nerve endings in the legs are due to another disorder.
Regardless of the cause and severity of symptoms, a visit to the doctor is necessary. If the disease is detected at an early stage, it is easier to stop the destructive process and prevent the appearance of new symptoms.
Symptoms and treatment of neuropathy
Neuropathy is an inflammatory process that deprives the limbs of sensitivity. First, a person ceases to feel temperature changes or mechanical influences, which under normal conditions cause discomfort or pain. In the future, this can lead to numbness of the limbs and impaired ability to control them.
Most often, neuropathy affects people who, due to their profession or type of activity, expose themselves to great physical stress. Professional athletes are at risk. A whole range of methods are used to treat the disease. Therapy is carried out mainly in a hospital, since most procedures cannot be performed at home.
- The patient is prescribed medication. Since neuropathy is primarily an inflammatory process, medications that relieve it are needed. And if the illness is accompanied not only by numbness of the limbs, but also by sharp pain, painkillers will also be prescribed.
- For such disorders, physiotherapy is effective.
- Restorative therapy aimed at overall strengthening of the body will be needed.
So, the patient is prescribed to take vitamins, and treatment is carried out aimed at reducing the level of toxins.
Features of neuralgia
Neuralgia occurs as a consequence of injury. This could be a severe bruise of the ankle joint, a dislocation or a fracture. Both adults and children are susceptible to pathology. Sometimes it can be a consequence of damage to the peroneal nerve during meniscus surgery.
The main symptoms of the disease:
- increasing the pain threshold, external influences are felt less in the damaged area.
- disturbances affect the functioning of muscles in the area of the nerve ending, and gait changes noticeably.
If the cause of a pinched nerve is injury, complex therapy is required. First, you need to immobilize the injured leg so that the tissues heal properly.
For this, plaster tape is used, which provides fixation and prevents possible re-injury.
If the injury site has already begun to become inflamed, the patient needs to take medications that can relieve pain and swelling. In addition, vitamins, physiotherapy and exercise therapy are needed for pinched peroneal nerves.
Signs and treatment of neuritis
Unlike the ailments described above, neuritis, although it is a type of inflammation, does not lead to loss of sensitivity. It manifests itself with spasms and a burning sensation. Pink-violet swelling appears, sometimes the effect of sagging limbs. General symptoms also develop:
- weakness;
- increase in body temperature.
Source: https://BoliGolovnie.ru/varikoz/aksonopatija-malobercovogo-nerva-lechenie.html
How does axonal degeneration occur?
The peripheral nervous system consists of nerve fibers consisting of axons (processes) of neurons, the bodies of which are located in the spinal cord and brain. Axons lack ribosomes and granular endoplasmic reticulum, therefore proteins synthesized in the cell body reach parts of the axons using axonal transport systems (axoplasmic current), which are divided into 3 types:
1) a slow axoplasmic current spreads along the axon at a speed of 1 mm per day and transports proteins - components of the cytoskeleton (the internal structure of the axon, consisting of oriented microtubules and neurofilaments);
2) fast anterograde current spreads at a speed of 200-400 mm per day and transports phospholipids, glycoprotectants and enzymes necessary for synaptic transmission;
3) fast retrograde current at a speed of 150-300 mm provides feedback between the cell body and its axon; with the help of retrograde current, substances are transferred that signal the need for changes in metabolic activity.
Axonal degeneration occurs if the synthesis of substances necessary for the axon is disrupted in the cell body or if energy production in the mitochondria is disrupted, as a result of which the fast anterograde axoplasmic current in the axon stops. With axonal degeneration, an increased level of calcium is observed in the neuron, which activates the calpain system, which can trigger various pathological processes.
With axonal degeneration, the thickened part of the axon is primarily affected, then the degeneration spreads in the proximal direction. The longest axons are damaged the most, so symptoms of axonal degeneration are felt primarily in the feet and hands.
The degenerative process that has spread to the cell body leads to its death. If the influence of the factors that led to axonal degeneration ceased before the cell died, then axonal restoration occurs. Regeneration occurs slowly and can take from several months to a year.
Toxic distal axonopathy
Distal axonopathy is the most common form of damage to the peripheral nervous system by toxicants. To date, this type of pathology, both experimentally and in clinical settings, has not been studied deeply enough.
A list of some substances that can cause toxic axonopathies in humans is presented in Table 25.
Table 25. Substances that cause toxic axonopathies in humans
| Medicines | Pesticides | Industrial toxicants |
| amitriptyline amphetamine dapsone diphenylhydanthione disulfiram vinblastine vincristine isoniazid nitrofuranthione penicillin chloramphenicol chloroquine cisplatin | DDT dieldrin dinitrophenol monobromomethane petachlorophenol barium polysulfide FOI (karbaphos, dichlorvos, leptophos, etc.) | acrylamide benzene hexane hydrazine dichlorobenzene methyl bromide methyl butyl ketone arsenic halogenated biphenyls lead carbon disulfide thallium TCCP tetrachloroethane trichlorethylene carbon tetrachloride ethylene oxide |
In most cases, the manifestations of poisoning are not very specific and are characterized by signs of symmetrical sensorimotor polyneuropathy. Electron microscopy of the affected nerves reveals an accumulation of neurofilaments in the areas of localization of the nodes of Ranvier.
Pathological changes initially form in the form of multifocal lesions of the distal sections of long myelinated axons of large diameter (motoneurons). The fibers of the sciatic nerve and, in particular, the conductors innervating the calf muscles are especially vulnerable.
Since initially only the distal parts of the nerve fibers are involved in the process, the victim can remain fully functional for some time. Degenerative changes in the axon gradually spread proximally towards the nerve cell body.
The weakness of the corresponding muscle groups increases. Since motor neurons are affected diffusely, and a large number of intact fibers remain in the structure of the nerve trunk, despite the pronounced clinical signs of intoxication, the speed of impulse transmission along the nerve changes little.
Axonal neuropathies are usually accompanied by secondary demyelination of nerve trunks.
Sensory impairment is also observed initially in the distal extremities. This is manifested by loss of sensation in the hands and feet (the “socks and gloves” symptom). Gradually, neurons of the sensory ganglia of the dorsal roots of the spinal cord may also be involved in the process.
Damages to vegetative fibers are extremely rare.
The sequence of events that develop during the formation of toxic neuropathies is quite typical.
Characteristic: periodically occurring feeling of numbness of the limbs; increased pain sensitivity of the skin of the distal extremities; pain along the nerves of the upper and lower extremities; paresthesia; weakness of muscle groups, developing from the periphery to the center, mainly extensors; ataxia; atrophy of the muscles of the limbs.
Axon regeneration (as opposed to remyelination) occurs slowly at a rate of about 1 mm per day. In this regard, the recovery process drags on for months and even years.
Many toxicants damage not only peripheral but also central nerve conductors. In the central nervous system, structures formed by long axons of large diameter are also affected: the corticospinal and spinocerebellar tracts.
Conducting pathways formed by short processes of small diameter (optic nerve) are the last to be involved in the pathological process, and, as a rule, only during chronic intoxication. Disturbances in the central nervous system and PNS can develop almost simultaneously, with central effects often masked by more pronounced peripheral effects.
However, after restoration of the functions of the peripheral nerve trunks, signs of damage to the central nervous system may appear: spasticity, ataxia, atrophy of the optic nerve, impaired mental abilities.
The intimate mechanisms of action of most toxicants are not known. It is noted that substances that can cause axonal degeneration inhibit the activity of enzymes such as neuresterase (see below), as well as glyceraldehyde-3-phosphate dehydrogenase, which are necessary to ensure energy and plastic processes in the nerve cell.
Tri-O-cresyl phosphate (TOCP)
A classic representative of substances that cause distal axonopathy is tri-O-cresyl phosphate (Figure 20). It is an oily liquid that is highly soluble in lipids and organic solvents.
The substance is widely used as a heat-stable additive to machine oils and a plasticizer in the production of plastics. TOCP belongs to the FOS group, but does not have an anticholinesterase effect.
Figure 20. Structure of the tri-O-cresyl phosphate molecule
A clear picture of intoxication develops when about 120 mg of TOCP is ingested (i.e., 2 mg/kg body weight). The analysis shows that pathology of varying severity can develop from significantly smaller doses of the substance (more than 0.5 mg).
In 1940, 89 Swedish army soldiers were poisoned by TOCP as a result of eating oil contaminated with the toxicant. The poisoning clinic for all victims was similar. After 1–12 hours, signs of gastroenteritis developed, characterized by vomiting (90%), abdominal pain, and diarrhea.
The phenomena continued for 24 – 36 hours. Then, after a latent period that lasted 13–27 days, paresthesia appeared, and then flaccid paresis of the distal muscle groups of the lower extremities (first the extensors). Later, the phenomena of weakness of the muscles of the upper extremities (46%), hips (41%), and pelvic area (43%) appeared.
Impaired tendon reflexes were noted in all victims (knee reflex, Achilles reflex). Sensory and cranial nerves were not involved in the pathological process. In 26% of victims, there was a violation of autonomic functions: bladder paresis, impotence. Manifestations of intoxication reached a maximum at 3–4 weeks of illness.
Then remission occurred, but three months after the onset of intoxication, signs of central nervous system disorders appeared: spasticity and ataxia. In 52 affected patients, complete recovery of functions did not occur.
The experiment established that the pathological process is based on pronounced morphological disturbances of individual nerve fibers. They are characterized by the appearance of areas of degeneration along the axons. Demyelination of fibers is not observed.
Electron microscopy of the affected areas of the nerve fiber reveals disintegration of neurofilaments, accumulation of membranous and granular pathological inclusions.
There are morphological abnormalities in the synapses of the anterior horns of the spinal cord, characterized by swelling and rupture of vesicular membranes.
It is believed that damage to the intracellular membranes of neurons is caused by the interaction of TOCP with membrane-bound neuresterase, which is involved in their formation. A necessary condition for the development of neuropathy is significant (about 80%), irreversible inhibition of the enzyme.
Didn't find what you were looking for? Use the search:
Source: https://studopedia.ru/10_304362_toksicheskaya-distalnaya-aksonopatiya.html
Causes of axonopathy
Axonal degeneration can result from:
- poisoning (food, alcohol, poisons);
- viral or bacterial infections;
- malignant neoplasms;
- diseases of the liver, kidneys or pancreas;
- administration of certain serums and vaccines, taking medications.
For axonopathy that has developed as a result of acute food poisoning, gastric lavage, the use of laxatives and activated charcoal are indicated. In case of lead poisoning, calcium thetacin or unithiol is administered intramuscularly. In case of poisoning with insecticides (organophosphorus compounds), treatment is carried out with atropine or proledoxime. Poisoning with thallium and arsenic is common (in cases of criminal or suicidal poisoning), which also results in rapid axonal degeneration. For any symptoms of poisoning, you should call an ambulance, since only doctors can administer the correct antidote.
Degeneration in nerve tissue can be caused by various viruses and bacteria (Epstein-Barr virus, herpes virus, human immunodeficiency virus).
Some cancer drugs, antivirals, anticonvulsants, and antibiotics can damage peripheral nerves with long-term use. Long-term use of amiodarone, metronidazole, and furadonin can lead to axonopathy. Therefore, you should not self-medicate and prescribe medications yourself: medication regimens should be developed by professionals.
Axonal polyneuropathies: pathogenesis and treatment
Polyneuropathy (PNP) is a disease of the peripheral nervous system that develops as a result of diffuse damage to peripheral nerves – their axons (axonal polyneuropathies), myelin sheath (demyelinating polyneuropathies) or neuron bodies (neuronopathies) [9]. The pathogenesis of axonal type polyneuropathies is based on generalized damage to the axial cylinders of peripheral nerves.
Pathogenesis
. Axonal degeneration (axonopathy) is the result of impaired neuron metabolism due to insufficient energy production in mitochondria and/or impaired axonal transport. In axonopathies, the myelin sheath suffers secondarily (secondary demylinization).
Myelin can be damaged as a result of nerve ischemia (damage to the vasa neurorum
), deposits of substances or immune complexes toxic to the nerve in the endoneurium (which is typical, for example, of diabetes mellitus, especially type 1 - with high hyperglycemia and autoimmune disorders) [4].
Accordingly, among the causes of axonopathy of peripheral nerves are metabolic disorders, toxic effects, ischemia of nerve trunks, hereditary predisposition and autoimmune mechanisms [5].
According to the etiological factor, the vast majority of axonal PNPs are metabolic and toxic, among which the first place is occupied by diabetic (up to 50% among patients with diabetes mellitus and up to 90% of damage to the nervous system in diabetes [9, 12]) and alcoholic (up to 50% among patients alcoholism [2, 9]).
The cause of toxic-metabolic PNP is exo- and endogenous intoxication. Substances coming from outside or their own metabolites that are toxic to peripheral nerves cause their damage.
The severity of this damage depends on the degree of toxicity of the agent (acute metabolic PSP is distinguished, developing against the background of severe general intoxication, for example, PSP with rapidly increasing liver failure or uremia, poisoning with organophosphorus substances, arsenic, lead, as an undesirable effect of treatment with lithium drugs, cytostatics ), the duration of its influence, the own genetic characteristics of the metabolism of nervous tissue, and the autoimmune factor also plays an important role [13].
Most of the metabolic ASPs frequently encountered in the clinic are the result of long-term exposure to endo- and exogenous toxic agents (diabetic, hepatic, uremic, alcoholic, occupational, medicinal). The result of such intoxication is damage to the axial cylinder of the axon.
Clinically, this is manifested not only by sensory disturbances and muscle weakness (which is also typical for demyelinating PSP), but also by muscle wasting and pronounced trophic disorders. All these signs indicate long-term suffering of peripheral nerve axons.
Electroneuromyography (ENMG) reveals a decrease (sometimes to the point of complete absence) in the amplitude of sensory potentials and M-responses of peripheral nerves.
In patients with axonal type PSP, motor functions are often sufficiently preserved (there are no pronounced paresis, patients retain the ability to walk, often without additional support), while sensory (pain and paresthesia) and trophic disorders are disabling.
Thus, axonal sensorimotor PSP is one of the important pathogenetic factors in the development of diabetic foot syndrome [3]. Axonal nerve damage develops slowly and gradually, but with proper treatment it is potentially reversible.
With massive exposure to an agent toxic to the peripheral nervous system, the participation of the ischemic component (due to the suffering of the vasa neurorum
), autoimmune influences develop PNP of the axonal demyelinating type, such as uremic, lead, amiodarone, caused by exposure to substances highly toxic to nerves [9].
In the most common diabetic PSP, the demyelinating component is maximally present in insulin-requiring diabetes mellitus (characterized by higher hyperglycemia), and the severity of demyelination of peripheral nerves increases with sharp increases in blood glucose levels [4, 7].
The presence of the demyelinating component in metabolic PSP is influenced by hereditary factors (genetically determined myelinopathy, which would proceed subclinically without additional exposure to a toxic agent), autoimmune damage (for example, myelinopathy is more pronounced in type 1 diabetes mellitus, in which immunocompetent cells damage pancreatic tissue ) [4, 14].
PSP of the axonal demyelinating type are more severe, with severe paresis, sensory ataxia, and neuropathic pain syndrome, but often, with timely elimination of the toxic factor, they quickly regress.
In case of a very severe and persistent course of the disease, given the role of the autoimmune mechanism in the development of this type of metabolic PSP, short-term administration of immunomodulatory therapy (usually glucocorticoids, sometimes cytostatics) is necessary [9, 11].
Clinical course of PSP.
As already mentioned, with prolonged exposure to an agent that is moderately toxic to nerves, axonopathy develops slowly, which is not always noticeable.
Predominant damage to poorly myelinated vegetative and sensory fibers causes paresthesia, increased cold sensitivity of the hands and feet, and mild trophic disorders.
With ENMG, it is not always possible to identify characteristic signs of sensory and motor axonopathy - a decrease in the amplitudes of sensory potentials and M-responses - if large, richly myelinated nerves are examined, the axons of which suffer later.
Signs of secondary myelinopathy are revealed more quickly, both clinical - the addition of neuropathic pain, paresis, and myographic - a decrease in the speed of propagation of excitation (SRV) along the nerves.
Subject to an adequate therapeutic strategy - eliminating the effect of the factor damaging peripheral nerves, prescribing drugs that affect the metabolism of nervous tissue - remyelination occurs, which is reflected both in ENMG in the form of an increase in SRV, and clinically - in the form of regression of paresis and neuropathic pain, improvement in sensitivity. However, if polyneuropathy developed under conditions of prolonged action of a toxic agent, damage to the axons of peripheral nerves, a decrease in the amplitudes of sensory potentials and M-responses to ENMG persists, since the axial cylinders of the nerves have a much lower ability to regenerate than myelin.
Thus, in a study [8] devoted to the treatment of alcoholic PSP, the leading ENMG sign of damage to peripheral nerves in most patients was a decrease in ERP.
Under conditions of elimination of the toxic factor (in this case, alcohol intake) and treatment with α-lipoic acid (berlithion in a daily dose of 600 mg), patients quickly, within 1 month, regressed ENMG and clinical signs of myelinopathy - the severity of paresis and pain syndrome (in points on a visual analogue scale from 5.2±1.0 to 2.6±0.5) significantly ( p
Source: https://www.mediasphera.ru/issues/zhurnal-nevrologii-i-psikhiatrii-im-ss-korsakova/2013/6/031997-7298201364
Types of axonopathies
Axonopathies are divided into acute, subacute, chronic and alcoholic.
Acute axonopathy develops in criminal or suicidal poisoning. The clinical picture of the disease develops within 2-4 days, and recovery with timely assistance occurs within several weeks.
Subacute axonopathy is caused by toxic and metabolic causes and occurs over several weeks or months.
The chronic form of axonopathy (the course of the disease is more than 6 months) develops with systemic diseases (cancer, diabetes mellitus, Lyme disease, etc.), with vitamin deficiencies, and with chronic intoxication.
Alcoholic axonopathy occurs in people who regularly abuse alcohol for a long time. As a result of prolonged exposure to alcohol in the body, metabolic processes in neurons are disrupted, changes occur in the spinal and cranial nerves, in the spinal cord and in the brain.
Axonopathy – Don’t get sick
Axonopathy is a disease of the nervous system associated with the involvement of neuron axons in the pathological process due to the influence of various factors.
It is believed that all axonopathies, in their clinical manifestations, are classified as polyneuropathies and require observation by a neurologist.
It is very important to begin timely treatment and conduct extensive diagnostic examinations in order to establish the true cause of the disease.
Causes of axonopathy
According to the causes, all types of axonopathies are divided into three large groups: acute, subacute, chronic axonopathies. What is it, type 1 axonopathy? Most often, this condition occurs during acute poisoning with various poisons (methanol, arsenic compounds, carbon monoxide) and is accompanied by the rapid development of clinical symptoms in a sick person.
What is type 2 axonopathy? This condition is associated with a subacute, gradually progressive onset of symptoms of neuronal axonal damage. Most often, such axonopathy occurs with various metabolic diseases (diabetes mellitus, other endocrine pathology).
It is important to note! If the damaging factor is excluded (giving up alcoholic beverages, fighting hypovitaminosis, etc.), the symptoms do not go away completely, since some of the damage to the axons remains irreversible.
With type 3 axonopathy, symptoms appear slowly and progress unnoticed by the patient for a long time. A similar picture is observed in persons with chronic alcohol intoxication and vitamin deficiencies.
Main symptoms of axonopathy
The manifestations of axonopathies are varied and depend mainly on the location of the affected neurons. The main symptoms of the disease: impaired skin sensitivity, crawling sensations, discomfort, excessive sweating or lack thereof, excessive pigmentation on the skin.
The development of symptoms, as a rule, occurs very slowly, unless we talk about the first type of axonopathies. The gradual involvement of a larger number of axon fibers and new axons in the pathological process leads to an increase in the intensity of symptoms and a decrease in the quality of life of sick people.
Axonopathy of the peroneal nerve is very often observed, associated with many damaging factors.
With the development of such a condition, the patient experiences a violation of not only sensitivity in the area of the lower leg and foot, but also disturbances in the motor sphere: weakness in the muscles of the foot leads to its inadequate flexion, extension, and also rotation to the side.
All this leads to the appearance of the so-called “horse” gait or steppage. As a result of damage to axons, movement may also be impaired in the fingers of the lower extremities.
Do you know the difference between the Milgamma vitamin complex and Kombilipen? Read about the effects of drugs on the nervous system.
How poisoning with toxic substances affects the nervous system can be found here.
Diagnosis of the disease
Making a diagnosis of axonopathy and determining the causes that caused it is a difficult task for any specialist.
Therefore, if any of the above symptoms appear, you must immediately contact a neurologist for examination and timely treatment.
The most important stage in the diagnosis of axonopathies is a neurological examination of the patient and collection of all complaints, taking into account the dynamics of their occurrence.
To make a diagnosis, they actively use:
- electroneuromyography (a method that allows you to determine the location of the lesion and evaluate the parameters of the nerve impulse along the axon);
- general blood and urine tests;
- biochemical study of blood glucose to exclude diabetes mellitus;
- X-ray examination of the chest organs;
- Ultrasound;
- tests for a number of infections (syphilis, HIV).
Treatment of axonopathy
Long-term treatment of axonopathies is based on the administration of vitamins B, C and E, as well as drugs that improve blood supply to the nerves (Actovegin, Cerebrolysin, Clopidogrel, etc.).
Very often, in addition to these medications, medications from the group of nootropics are used - Nootropil, Piracetam, Phenotropil, etc.
These products protect neurons from damaging effects and improve their recovery.
Do you know what Actovegin is used for? Indications and contraindications for use.
All about the side effects of Nootropil here.
Information about nootropics is available at this address: https://golmozg.ru/farmacevtika/nootropy-dlya-mozga.html. Nootropics for children and adults.
It is very important to treat the underlying disease, against which the axonopathy appeared. If this is due to infection, then first of all it is necessary to start antiviral or antibacterial therapy. In the case of diabetes mellitus, treatment must necessarily include hypoglycemic therapy to control blood glucose levels.
At the first stages of treatment, it is necessary to begin rehabilitation measures aimed at restoring damaged sensory and motor functions - therapeutic massage, physical therapy, physiotherapy. ( 35,00
Source: https://neboletall.ru/aksonopatiya.html
Symptoms of axonal degeneration
At the onset of the disease, sensory loss occurs in the feet and hands (like socks and gloves). Then weakness appears in the limbs, possible paralysis, swelling, changes in temperature and color of the skin. The oculomotor, optic and phrenic nerves may be affected, and the activity of the vagus nerve may be impaired, manifested by an acceleration of the pulse and impaired breathing.
Even at the initial stage of the disease, a person’s pain sensitivity is impaired: he may not feel needle pricks; temperature sensitivity decreases - the ability to distinguish between cold and hot; reflexes fade away: first of all, the Achilles reflex, then the knee reflex.
Diagnostics
When diagnosing axonopathy, the following methods are used:
- complete blood count, blood glucose test, blood test for HIV;
- Analysis of urine;
- ultrasound of the abdominal organs;
- spinal tap;
- nerve biopsy is a traumatic procedure that is used quite rarely; nerve tissue is most often taken from the lower leg;
- electromyography - insertion of a thin needle into the muscle in order to measure the electrical activity of the muscle during contraction and at rest (a sign of axonal degeneration is a decrease in the level of impulses along the nerve fibers).
To confirm the diagnosis of axonal degeneration, the following may be performed:
- research of the cardiovascular system;
- radiography of the lungs and abdominal organs;
- assessment of liver and kidney functions;
- muscle strength tests, which can detect motor neuron damage;
- computed tomography (to detect bone or vascular changes, tumors, cysts, hernias, etc.);
- magnetic resonance imaging - to study the condition of muscles that are affected due to axonal degeneration.
Treatment of axonal degeneration
Treatment of axonal degeneration is carried out depending on the reasons that caused it: antibacterial, antiviral, hypoglycemic and other drugs can be prescribed. Medicines that restore blood flow in small blood vessels and vitamin complexes, as well as drugs that support the nervous system, are also prescribed. Recovery from axonal degeneration takes a long time, and functions are not always restored in full.
To prevent axonal degeneration, it is necessary to lead a healthy lifestyle, eliminate the entry of toxins into the body, give up bad habits, and adhere to a properly balanced diet. At the first warning symptoms, it is necessary to undergo a full medical examination and identify the cause of the disease. Then undergo a course of treatment: with timely treatment, restoration of nerve cells is possible, albeit slow.