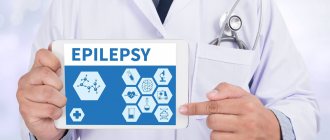
Epilepsy is a chronic neurological disease associated with damage or inflammation of the brain, externally manifested by seizures, mental disorders, personality changes and divided into two types: congenital and acquired.
Many people wonder whether epilepsy can be acquired, since in everyday life on the street or in other public places you can meet a person having an epileptic seizure, and therefore everyone wants to know the likelihood of contracting this type of disease.
The disease is a consequence of mechanical damage, in the form of a head injury or an infection that has entered the body. Often the cause is a brain tumor or a metabolic disorder, which can be congenital or acquired.
Acquired epilepsy is much less common than congenital epilepsy.
What causes and why do seizures occur?
What can cause an epilepsy attack? In 70% of cases, it is not possible to identify what exactly triggered the development of the disease.
The causes of an epileptic attack include the following factors:
- traumatic brain injury;
- degenerative changes after acute circulatory disorders;
- vertebrobasilar insufficiency, which causes difficulty in blood supply to the brain;
- stroke;
- malignant brain tumor, pathological changes in the structure of this organ;
- meningitis;
- viral diseases;
- brain abscess;
- hereditary predisposition;
- alcohol abuse, drug use.
Find out more about epilepsy seizures:
- what is status epilepticus and why is it dangerous?
- what are the features of a major and minor seizure;
- What is the algorithm for providing first aid during an epileptic attack?
Symptoms
The clinical picture among patients does not differ significantly. But partial seizures can be classified. During simple attacks the patient remains conscious. This condition can manifest itself as follows:
- Weak contractions of muscle tissue on the face and limbs, a feeling of tingling, numbness, and goose bumps occurs.
- The eyes turn with the head in the same direction.
- Intense salivation.
- The patient makes faces.
- Involuntary chewing movements occur.
- Speech defects.
- Disorders in the epigastric region, a feeling of heaviness in the abdomen, heartburn, intense peristalsis, flatulence.
- Hallucinations due to defects in the organs of vision, hearing, and smell.
Severe partial seizures occur in approximately 35-45% of the population.
At the same time, consciousness is lost. The patient is aware of what is happening, but cannot respond to the appeal to him. When the attack ends, amnesia occurs and the patient does not remember the events that occurred. Often there is a focal activation of the disorder, mirrored in the second hemisphere. In such a situation, a secondary generalized attack appears as convulsions.
Complex attacks are characterized by the following symptoms:
- Negative emotions, fear of death, and anxiety arise.
- Feelings or focus on events that have happened.
- When the patient is in a normal environment, there is a feeling as if he is in an unfamiliar place.
- A feeling of unreality of current events. The patient observes himself from the outside and can identify with the characters of the works or films he has read.
- Automatisms of behavior and some movements appear, the nature of which is determined by the affected area.
During the periods between attacks in the first stages of the disease, the patient will feel well. Over time, signs of the underlying disease or brain hypoxia develop. A sclerotic process occurs, migraines occur, behavior changes, and dementia begins.
What can trigger an epileptic stroke?
What most often provokes epileptic attacks?
Typically an epilepsy attack is caused by:
- flickering light (for example, when watching TV, working at a computer);
- lack of sleep;
- stress;
- intense anger or fear;
- taking certain medications;
- drinking alcohol;
- deep, too rapid breathing;
- electrotherapy, acupuncture, electrophoresis, active massage.
In women during menstruation, the frequency of attacks may increase.
Treatment
Partial seizures are complex. The main task of doctors is to reduce their number and achieve remission . In this case, the following are most often used: Carbamazeline (the medicine is the standard in the treatment of partial seizures. Use is carried out with a minimum dosage, after which, if necessary, the amount of medicine is increased), Depakine, Lamotrigine, Toliramate.
Often, combinations of several antiepileptic drugs are used to obtain good results. But recently, this tactic has been used infrequently due to the high likelihood of side effects.
Approximately 1/3 of patients do not experience any effect from the use of drugs, so surgery has to be performed.
Localization of the disorder in the brain area
The classification of partial epilepsy is based on identifying an area in the brain with increased activity during an attack. By the way, the picture of a particular seizure will largely be determined by the location of the focus of pathological excitability of neurons.
Possible localization of the outbreak:
- Temporal . This is the most common type of partial epilepsy (about 50% of all cases of the disease are provoked by the pathological activity of neurons in the temporal zone).
- Frontal . It deservedly ranks second in frequency of cases (24-27%).
- Occipital (about 10% of all patients with this form of epilepsy).
- Parietal . Occurs least often (1%).
How to determine the exact location of the outbreak? Now this is very easy to do. An EEG (electroencephalogram) will help.
Diagnosis is most often carried out while the patient is at rest or asleep (polysomnography). But the most accurate result is given by an EEG directly during the next attack. It is almost impossible to wait for it. Therefore, an attack is provoked by the introduction of special drugs.
First aid
If a person has a seizure, the following steps must be taken:
- Lay it down carefully.
- Raise your head slightly.
- If the person's mouth is open, insert a handkerchief or something tight to prevent him from biting his tongue.
- Turn your head slightly so that the person does not choke on saliva or vomit.
After the attack ends, help the person stand up and hold him until he is completely back to normal. Usually, immediately after an attack, complete normalization of the condition occurs.
Hemispherectomy
Hemispherectomy is a radical surgical procedure that removes the hemisphere of the brain. Similar procedures are performed for complex forms of epilepsy. This is necessary if the patient has more than 10 attacks per day. When the two hemispheres separate, several anatomically significant fragments remain.
This procedure is performed for patients under 13 years of age in a situation where one of the hemispheres is working with defects. If surgery is performed at this age, the chances of a favorable outcome increase. The patient is sent home after 10 days.
Prognosis and prevention
Partial epilepsy is difficult to treat. Most often, the patient is prescribed lifelong drug therapy.
During the stabilization of the condition, the doctor may prescribe a course of anticonvulsants for preventive purposes. This disease is characterized by relapses even with complex drug therapy.
Therefore it is important:
- carry out regular examinations;
- take prescribed medications;
- to refuse from bad habits;
- avoid places with flashing special effects;
- limit physical activity;
- avoid stress;
- limit fluid intake;
- monitor your diet.
Partial epilepsy is a serious disease that should not be treated with disdain. At the first signs of illness, it is important to consult a doctor in a timely manner to select adequate drug therapy. Self-medication is strictly prohibited.
Epilepsy, congenital or acquired
Acquired epilepsy is a neurological disease with a chronic course; it is characterized by the presence of repeated seizures due to excessive electrical activity of nerve cells in the brain.
This type of paroxysm accounts for 25% of cases. Symptoms of the disease are as follows: short-term memory loss, uttering inarticulate sounds, automatic actions, convulsive muscle twitching.
With a long course of the disease, patients experience personality disorders: increased sentimentality, suspicion, cruelty, outbursts of anger, and a tendency to take revenge.
Speech is stereotyped and slow; such people cannot quickly switch from one topic to another.
This type of disorder is always secondary; most often the causes of focal epilepsy are associated with:
- metabolic abnormalities;
- abnormal changes in blood vessels;
- volumetric processes in the cerebral cortex;
- congenital developmental defects;
- head injuries;
- infectious lesions;
- poisoning;
- hypoxia.
The acquired variety is diagnosed using instrumental and laboratory studies. The fundamental method for determining the focus of paroxysmal activity is computer imaging - MRI or CT.
Treatment is aimed at eliminating the cause of the abnormality, reducing or eliminating seizure activity, improving quality of life and preventing disability. Therapy includes taking medications or undergoing surgery.
Causes of acquired epilepsy
This pathology is secondary, formed under the influence of a large number of unfavorable factors associated with the transfer of a certain type of disease.
Acquired epilepsy manifests itself immediately or after some time.
Experts advise timely treatment of disruptions in metabolic processes, viral diseases, and in case of a head injury, seek professional help at a clinic.
The main causes of the symptomatic variety of the disease:
- head injuries, concussions, bruises and skull fractures, which violate the integrity of internal structures and can spur the onset of a seizure;
- infectious diseases such as meningitis, encephalitis and abscess;
- prolonged fever, when body temperature significantly exceeds acceptable levels;
- tumor-like neoplasms in the head;
- vascular disorders;
- presence of multiple sclerosis;
- intoxication with narcotic substances;
- alcoholism;
- drug overdose;
- birth injuries in a child associated with hypoxia, head contusion.
Researchers have proven that endogenous substances, more precisely amino acids, polypeptides, monoamines and acetylcholines, play an important role in the development of seizures. All of them perform mediator functions of various directions.
Glycine and taurine are responsible for the inhibitory function of the nervous system, and acetylcholine and glutamic acid are responsible for the excitatory function.
During the formation of a paroxysmal focus, the balance between these substances is disrupted, which leads to the appearance of corresponding symptoms.
Is acquired epilepsy inherited? Most scientists believe that it is not epilepsy itself that is inherited, but only a certain degree of convulsive readiness. That is, the predisposition itself, which, under the influence of a large number of (external or internal) unfavorable factors, can spur further growth of the paroxysmal focus.
Georgy Romanovich Popov
Neurologist, Candidate of Medical Sciences
Every year there is an increase in the number of people suffering from seizures. WHO provides the following data: 4-10 people per 1000 population have epilepsy. In Russia, the incidence rate accounts for 2.5% of cases. Epileptic seizures occupy one of the first places in the structure of disability.
In the absence of timely treatment, patients become disabled in groups 1 or 2. When studying the causes and factors leading to relapse of seizures, doctors established a certain pattern. Epilepsy is diagnosed several times more often in countries with low and middle levels of development.
According to statistics, 80% of patients live in such conditions.
Epilepsy is divided into several types. Acquired is not detected as often as compared to other forms of pathology. Doctors at the Yusupov Hospital are paying attention to finding out the possible causes of the disease. Thanks to this, it is possible to choose effective treatment.
It has been proven that if the rules of prevention are followed and anticonvulsants are taken, 70-80% of patients can live for a long time without relapse. An individual epilepsy treatment plan is developed for each patient at the Yusupov Hospital. The drugs used meet European quality and safety standards.
Personal preventive recommendations provided to all patients help minimize the risk of recurrence of epileptic seizures.
Clinical picture
During the occurrence of seizures, neurons work to the maximum, expending their energy. This enhances oxidative processes in brain cells. The consequence of this is relative hypoxia, when the organ does not receive enough oxygen; it is observed in different parts and is expressed unevenly.
As attacks progress, oxygen deficiency increases due to increased contractility of the muscular system. Generalized paroxysms that continue for a long time can lead to cerebral edema. Changes occur in vasomotor reactions, blood flow in the vessels is weakened. All this contributes to the appearance of acute disorders in neurons and cells of small vessels.
Seizures result in single or multiple damage to nerve fibers, which over time causes cell necrosis and hemorrhage. Subsequently, morphological changes in the brain contribute to a decrease in its volume.
Patients with severe disease are at risk with a high mortality rate. It is very important to provide timely assistance to such patients, since morphological changes during a prolonged attack may be incompatible with life.
Can epilepsy be acquired? Everything will depend on the cause of its occurrence; in adulthood, the development of symptomatic pathology is associated with the influence of unfavorable factors: numerous diseases, poisoning, drug overdose, head injuries.
The first signs of acquired epilepsy
Most acquired pathologies have symptoms that are precursors to an incipient seizure:
- headache;
- high irritability;
- feeling of fear;
- numbness or tingling in certain areas of the body;
- darkening of the eyes;
- noise in ears;
- changes in blood pressure;
- muscle twitching;
- detachment from reality;
- hallucinations: auditory, olfactory, visual.
The presence of such signs indicates a problem that should be given attention. For any head injuries, you should go to the clinic and undergo a comprehensive examination.
Initially, paroxysms may appear rarely and do not last long, but as they progress, the picture will worsen.
Symptoms of acquired epilepsy
The main symptom of the disease is the presence of epileptic seizures, which have a different course. A person may lose consciousness, freeze in a certain position, perform chaotic movements; with this type of disorder, convulsions do not always appear.
There are two main types of paroxysms:
- generalized;
- partial (focal).
For a symptomatic disorder, focal conditions are more characteristic, during which the focus of abnormal excitation in brain cells spreads to some areas of neighboring tissues.
In generalized forms, both hemispheres of the human brain are affected. There are two types of seizures:
- tonic-clonic - the muscles of the whole body tense, after which their rhythmic twitching occurs, with or without loss of consciousness, lasting no more than 5 minutes;
- absence - consciousness switches off for several seconds or minutes, there is no reaction to external stimuli, involuntary movements of the eyeballs often appear, twitching of the fingers or face is noted.
Partial attacks depend on the area of distribution of the pathological focus. The most common type of deviation is the temporal one, in which a person experiences visual and auditory hallucinations with loss of consciousness. If the lesion affects other parts of the brain, then problems are observed:
- with vision;
- with memory;
- with speech;
- with the perception of reality.
The patient's behavior may change dramatically; he becomes suspicious, overly suspicious, and vindictive. Acquired epilepsy due to alcoholism is quite common; it is characterized by loss of consciousness, convulsive syndrome, and automatic movements. The disease provokes the development of mental disorders, memory and thinking suffer.
Seizures can be single or multiple; when the condition worsens, there is seriality. The more frequent and intense the attack, the greater the likelihood of consequences.
Diagnosis of acquired epilepsy
Before making a diagnosis and prescribing treatment, the patient undergoes a full range of diagnostic procedures:
- A medical examination is carried out, an anamnesis is studied, and complaints are listened to. The interviews are conducted by a neurologist and a psychotherapist; these specialists are able to identify the presence of neuropsychiatric disorders at the first consultation.
- Instrumental diagnostics are prescribed, with its help you can find out about the nature of internal damage and see the area where the source of epiactivity is located. Hardware research includes:
- electroencephalography, it allows you to determine the degree of brain activity; with an artificially provoked attack, you can see the nature of the changes more clearly;
- magnetic resonance imaging - allows you to establish the cause of the deviation, identify the focus and find out the degree of its progression.
- Laboratory procedures are carried out to identify the presence of infectious, viral and bacterial complications.
Acquired epilepsy always has a cause of development associated with the influence of external or internal factors. Clarification of this circumstance will help in making a diagnosis and in selecting more effective therapy. It will also help in differentiating from similar ailments.
Treatment of acquired epilepsy
The main therapy is aimed at eliminating the cause of the disease, in some cases it is possible to achieve a complete cessation of negative paroxysmal activity. The main method of treatment is medication, which includes:
- anticonvulsants, which help relieve or prevent paroxysms; with their help, muscle spasms are relieved and pain during a seizure is reduced or completely eliminated;
- nootropics - stimulate mental activity, activate cognitive functions, improve memory and increase learning ability, and also increase the brain’s resistance to various harmful influences: hypoxia and excessive nervous stress;
- psychotropic drugs - have a beneficial effect on mental processes, they suppress excitement, eliminate depressed mood, improve thinking;
- vitamin complexes - are a good help for improving the body's resistance and enhancing immunity;
- tranquilizers - eliminate feelings of anxiety and stabilize the psycho-emotional background, they have a slight sedative effect, anticonvulsant effect, and help stabilize the autonomic nervous system.
In addition, intramuscular and intravenous administration of drugs is prescribed to stabilize brain activity.
Seriously?
Source: https://dingodesign.ru/jepilepsija-vrozhdennaja-ili-priobretennaja/
Forecast
When a patient is treated for simple partial seizures, the prognosis can vary. Often epilepsy is effectively treated or eliminated without intervention, sometimes it is necessary to monitor the patient's condition therapeutically.
Most forms of the disease are safe for the life and well-being of the carriers, excluding the possibility of accidents such as a fall, the initial stage of a seizure, or during swimming, while driving a vehicle, etc. Patients quickly learn to cope with their illness and avoid interaction with provoking factors or difficult situations.
The forecast always depends on the following factors:
- Location of abnormal bioelectrical activity of neurons.
- Limits of seizure activity.
- Reasons for appearance.
- The nature of transformations in the nervous system.
- Associated disorders.
- Types of seizures and features of their course.
- Age category of the patient.
- A type of epilepsy.
- There are other points that determine the condition of patients.
Seizures caused by severe brain damage are rare. They can cause complex organ dysfunction, changes in consciousness, loss of connection with the environment, or paralysis of the arms and legs.
Symptoms
There is a classification compiled by the International League Against Epilepsy, which distinguishes:
- partial or focal seizures, which in turn are divided into simple, complex and secondary generalized;
- generalized (these include absence, myoclonic, clonic, tonic, tonic-clonic and atonic);
- unclassified epileptic seizures.
Depending on the type of epilepsy, certain signs will appear. Partial epilepsy is characterized by the occurrence of a seizure focus in a specific area of the brain. Each separate area of the brain is responsible for a specific bodily function. Simple attacks occur without loss of consciousness and can manifest themselves as:
- motor signs: various twitching muscles of the face, arms and legs; chewing and smacking, licking lips; nystagmus; abduction and elevation of the head, arm, leg or half of the body; distortion of speech, involuntary sounds;
- sensory: sensation of numbness, tingling, decreased sensitivity or specific sensory symptoms - auditory, visual, taste and olfactory hallucinations, epileptic dizziness (feeling of flying or falling of the body and surrounding objects);
- vegetative: rumbling and pain in the abdomen, nausea, vomiting, flatulence, pallor of the skin, increased sweating, redness of the skin, dilated pupils, increased heart rate and breathing;
- mental symptoms.
Complex ones are accompanied by a change or loss of consciousness.
Generalized seizures initially involve both hemispheres of the brain and have the following features:
- Tonic attacks are characterized by spasms of the muscles of the entire body: head, face, limbs with their flexion and extension. The patient suddenly loses consciousness and falls. The attack begins suddenly, lasts a short time, and after completion the person remains in a confused state of consciousness for some time.
- Clonic seizures are repeated, irregular, bilateral jerking movements of the arms and legs. It also starts and ends suddenly, the frequency of contractions decreases towards the end.
- Myoclonic seizures are rapid and sharp muscle contractions (frequent blinking, head nodding to the sides) without loss of consciousness. They can be generalized (all muscles of the body are involved) or limited (muscles of one area are involved).
- Tonic-clonic seizures are the most frightening seizures for others. The patient screams and loses consciousness. In the first phase, all the muscles of his body contract; in the second, the spasm passes, but convulsions occur, with a gradually increasing amplitude and frequency. During this phase, patients often bite their tongue or cheek, and the foam released from the mouth becomes reddish. Autonomic symptoms also occur - facial flushing, tachycardia and increased blood pressure. Then comes a relaxation phase with involuntary urination and defecation. The duration is 2 minutes, but the unconscious state lasts up to 15 minutes. After a seizure, women feel unwell due to confusion, headache and nausea.
- Absence seizures are unlike any other. The patient at this moment looks as if he is deeply thinking about something, his consciousness is absent at the moment, his gaze becomes intent, small movements of the facial muscles are visible. This seizure is especially clearly visible if it occurs during a conversation - the dialogue immediately stops, and after it ends the person continues the thought. Absence seizures are most common in childhood.
- Atonic seizures also occur more often in children, but with the presence of Lennox-Gastaut syndrome. They are characterized by a sudden fall, as if the legs had given out, lasting several seconds without loss of consciousness. They are quite dangerous only because of the increased risk of injury when falling from their own height.
A partial seizure can transform into a secondary generalized one, characterized by the spread of neural discharges throughout the brain, as in the case of a primary generalized one. The symptoms are identical.
Lobectomy
During the procedure, the hemispheres are divided into 4 sections: occipital, frontal, temporal, parietal. If the epileptic focus is in the temporal lobe, it must be removed during surgery. The lesion is located in the frontal and mesial region. If it is necessary to remove a fragment of brain tissue not in the temporal lobe, extratemporal resection is performed.
Lobectomy is a common method of treating episyndrome. This type of surgery. In most examples, the initial seizure frequency is reduced by 95%.
Temporal resection is an open operation. To carry out this procedure, an operating microscope is used. The doctor opens the skull, removes the meninges, and removes the inflamed area. This method of combating pathology increases the chances of successfully preventing attacks by up to 80%. If no complications are observed, the patient is discharged.