Diseases of the visual organ and damage to the optic nerve are different. In the second case, there is a disruption in the generation and transmission of impulses to the brain. A feature of the disease of nerve fibers is the rapid onset and course of the acute period. The most common is retrobulbar optic neuritis. If it first affects one eye, then the inflammation spreads to the other.
Classification
Optic neuritis is classified according to the clinical picture that appears. The decisive points in dividing the disease into types are the causes of its occurrence and the source of inflammation.
Depending on the causes of optic neuritis, the following types are distinguished:
- Infectious.
- Parainfectious. Manifests itself as a consequence of viral diseases or the administration of vaccines.
- Demyelinating. The cause of the pathology is the destruction of the membrane of neurons.
- Ischemic. The result of disturbances in cerebral circulation.
- Toxic. Consequences after poisoning with methyl alcohol.
- Autoimmune. Occurs due to impaired immune functions.
If we take into account the area of damage to the optic nerve, then neuritis can be divided into intrabulbar and retrobulbar. The first of them extends to the optic nerve head. Most often, this deviation is observed in children. Retrobulbar neuritis is the result of untimely treatment. It manifests itself as inflammation of the nerve fibers located in the deeper layers of the eye.
In addition, the following types of neuritis are distinguished:
- Orbital. Inflammation penetrates into the eye socket.
- Transverse. All tissues of the optic nerve are affected.
- Papillitis. Damage to the optic nerve head in the early stages. Accompanied by hemorrhage.
- Neuroretinitis. The fibrous layer of the retina becomes inflamed.
- Interstitial. Accompanied by inflammation of auxiliary nerve cells and connective tissue.
- Axial. Those parts of the nervous system that are located directly behind the eyeball are affected.
As we see, optic neuritis has many varieties. Therefore, it is very difficult to establish an accurate diagnosis. The causes and symptoms of the pathology can provide significant assistance in diagnosing the disease. If neuritis is not treated in time, serious consequences are possible.
Causes of the disease
The number of disorders leading to the occurrence of optic neuritis is many. The prognosis of the disease depends on them. The following pathologies can cause optic neuritis:
- periostitis, phlegmon;
- iritis, iridocyclitis, panophthalmitis;
- meningitis, encephalitis, arachnoiditis;
- nasopharyngeal infection – pharyngitis, tonsillitis;
- common infectious diseases - tuberculosis, typhus, brucellosis, acute respiratory infections.
Promote the appearance of neuritis:
- pregnancy with complications;
- systemic diseases - gout, diffuse connective tissue disorders;
- diabetes;
- autoimmune pathologies;
- multiple sclerosis.
Inflammation affects the nerve sheath and its trunk. Due to the fact that n. The opticus swells and its fibers are compressed. This condition leads to degenerative changes and decreased vision.
After the end of the acute period, the affected nerve fibers are restored. A sick person notices an improvement in vision. However, with severe pathology, the nerve fibers are destroyed and disintegrate. The affected area is replaced by scar tissue. The optic nerve atrophies, causing vision loss irreversibly.
The occurrence of optic neuritis in multiple sclerosis is associated with demyelination of nerve fibers. The condition is accompanied by the occurrence of manifestations of retrobulbar neuritis.
Demyelination of nerve fibers
Reasons for development
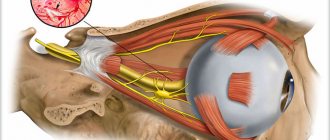
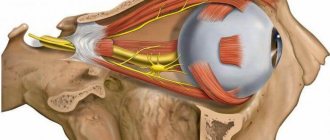
The optic nerve consists of axons that emerge from the retina and carry visual information to the primary visual nuclei. Most of the information is then sent to the occipital cortex where it is processed into an image.
Inflammation of the optic nerve causes vision loss, usually due to swelling and destruction of the myelin sheath covering the optic nerve.
Partial or temporary loss of vision (lasting less than one hour) may be a sign of early onset multiple sclerosis, causing neuritis. Multiple sclerosis is the most common cause of optic neuritis.
The disease can also be caused by ischemic optic neuropathy (blood clot). A thrombus is a blood clot that travels to the optic nerve. 50% of patients with multiple sclerosis develop optic neuritis, and in 20-30% of cases, optic neuritis is a sign of multiple sclerosis.
Other common causes of optic neuritis include infections (maxillary tooth abscess, syphilis, Lyme disease, herpes zoster), autoimmune diseases (lupus, neurosarcoidosis, neuromyelitis optica), alcohol poisoning, vitamin B12 deficiency, diabetes, and eye injuries.
Less common causes of the disease are:
- papilledema;
- meningitis, adhesions of the arachnoid membrane;
- traumatic brain injury or hemorrhage;
- brain tumors or abscess in the occipital region;
- thrombosis of the cavernous sinus, impaired liver or kidney function at a late stage of the disease.
Other possible causes include diabetes, low phosphorus levels in the body, or hyperkalemia.
Symptoms
The disease manifests itself quickly and unexpectedly. The disease is characterized by unilateral damage, so most often patients complain of symptoms appearing in only 1 eye. The manifestations of the disease largely depend on the amount of nerve damage: the more it is affected by inflammation, the brighter and stronger the symptoms.
Depending on what form of the disease has developed in the patient, its symptoms can manifest themselves to varying degrees: from the appearance of pain inside the eye to sudden loss of vision.
Symptoms of the intrabulbar form
The first manifestations appear already on days 1-2, after which their rapid progression is noted. Patients notice the appearance of visual field defects, in which blind spots form in the center of the image. Moreover, patients' visual acuity decreases in the form of myopia or even blindness occurs in 1 eye. In the latter case, it may become irreversible: the prognosis depends on the start of therapy and the aggressive properties of the pathogen.
A person most often begins to notice deterioration of vision in the dark: it takes at least 40 seconds to get used to the absence of light and begin to distinguish objects, and about 3 minutes on the affected side. Color perception changes, causing patients to be unable to distinguish certain colors.
On average, intrabulbar neuritis lasts about 3-6 weeks.
Symptoms of the retrobulbar form
Occurs much less frequently compared to the other form. Its main manifestation is considered to be loss of vision or its noticeable decrease. The disease is characterized by headaches, weakness, and increased body temperature.
In addition, central blind spots and decreased peripheral vision may occur. Patients often complain of pain “inside the eye,” in the eyebrow area.
On average, retrobulbar neuritis lasts about 5-6 weeks.
Diagnostics
Diagnosis of optic neuritis plays a key role in determining future therapeutic treatment. The main task is to differentiate neuritis from other pathologies of ocular structures. The main activities include:
- examination by an ophthalmologist;
- reaction of the pupils to light, bright radiation stimuli;
- examination of the fundus vessels of each eye;
- computer monitoring:
- MRI of the brain (if necessary);
- electrophysiological examination for various reactions.
If necessary, a comprehensive examination of the patient is carried out with consultations from specialists in various clinical areas. This is important for patients with a burdened neurological history, as well as when it is impossible to determine the true causes of the pathology. Usually a standard examination is sufficient to identify the diagnosis.
Diagnosis of pathology
Optic neuritis is a pathology that requires the joint participation of neurologists and ophthalmologists. The eye doctor checks visual acuity and prescribes instrumental research methods:
- perimetry;
- tonometry;
- study of direct and friendly reactions to light;
- biomicroscopy;
- ophthalmoscopy in conditions of mydriasis.
The main task of the eye doctor is to carry out a differential diagnosis with a congestive disc. The first pathology is supported by the appearance of edema and small bruises in the tissues of the optic disc. Fluorescein angiography of the fundus can more accurately confirm the diagnosis.
In difficult cases, the neurologist prescribes an EEG, brain tomography and lumbar puncture. Methods allow you to eliminate stagnant disks.
How to distinguish toxic neuropathy from neuritis
These two diseases are very similar in symptoms, but differ in treatment tactics and prognosis. To prescribe effective therapy, the correct diagnosis should be made as early as possible. To do this, you need to analyze the following nuances:
- The cause of the disease is that viruses or microbes always play a major role in the development of neuritis. Toxic neuropathy most often appears due to exposure to methyl alcohol or large amounts of 40-proof alcohol (more than 1.5 liters). Possible causes also include: Poisoning with heavy metals or their salts (lead, antimony, mercury);
- Overdose/individual intolerance to certain drugs: NSAIDs (Aspirin, Ibuprofen, Ketorolac, etc.), synthetic antibiotics (Sulfadimethoxine, Sulfacetemide) and cardiac glycosides (Digoxin, Strophanthin);
- Poisoning by vapors of phenol-formaldehyde resins (contained in regular cigarettes and smoking mixtures).
Using the above signs, toxic neuropathy can be identified. The main principle of its treatment is the elimination of the damaging factor (alcohol, metal, medicine) and its removal from the body. After this, the work of the nerve and its blood circulation are stimulated with the help of drugs such as Neuromidin, Trental, Actovegin, etc.
In most cases, vision changes become irreversible and the effect of treatment is to improve the general condition.
Retrobulbar neuritis in multiple sclerosis
Description
In multiple sclerosis,
the optic nerve is most often affected in the anterior part of the orbital part - from the point of entry of the vessels to the nipple - and in the intracranial part. Here changes are not only more common, but also more pronounced. The posterior part of the orbital part and the intracanalicular part of the optic nerve are less affected. In the anterior segment of the orbital part of the optic nerve, changes sometimes cover the entire area from the lamina cribrosa to the point of entry of the vessels and stop abruptly here. However, more often individual plaques are scattered in this area, with the maximum changes located in the circumference of the central vessels. In the posterior segment of the orbital part of the optic nerve, changes are less common and less pronounced. Sometimes, in the presence of large changes anteriorly, from the point of entry of the vessels, the posterior segment of the nerve remains completely normal. In other cases, there are separate pockets in it. As the nerve approaches the foramen opticum, the number of plaques and their size decrease. The intracanalicular part is always the least affected. The favorite location of plaques is the intracranial part of the optic nerve. Here, sclerosis begins near the connective tissue layers of the soft shell and spreads deep into the nerve trunk, gradually capturing its entire central part. Plaques from the intracranial portion of the optic nerve often extend posteriorly, where they merge with plaques on the chiasm.
A characteristic feature of multiple sclerosis is changes in the pulpy sheaths of nerve fibers
.
In fresh plaques, only the initial stages of myelin breakdown are visible; in old cases, the disintegration of the myelin sheaths goes so far that the nerve fibers lie completely naked among the sclerotic tissue. Multiple sclerosis is also characterized by the preservation of the axial cylinders
, despite the complete destruction of their myelin sheaths in one area or another. This explains the fact that ascending and descending degeneration is mostly absent. Despite their preservation, the axial cylinders in the area of the plaque still undergo some changes: the formation of round or spindle-shaped thickenings and the splitting of nerve fibers into fibrils. Some of these fibrils end up in the mass of protoplasmic decay. A certain amount of fibrils is retained and thus the continuity of the nerve fiber is ensured.
Changes in glia play a significant role in the formation of multiple sclerosis plaques
. Fresh plaques are characterized primarily by an increase in the number of glial cells. In old plaques, on the contrary, glial fibers predominantly grow. In the dense plexus of glial fibers, vessels with sharply sclerotic walls are sometimes visible. Between groups of glial fibers there are layers of connective tissue. In the area of plaques there is also an increase in the number of vessels. In fresh plaques, the walls of the vessels are slightly thickened, but they exhibit small cell infiltration of an inflammatory nature, which in some places is quite intense. In old plaques, there is a proliferation of connective tissue both in the walls of blood vessels and in their circumference. A small small cell infiltration is also observed in the connective tissue layers between the bundles of nerve fibers.
In general, pathological changes in the optic nerves in multiple sclerosis are identical to those observed in other parts of the central nervous system.
Retrobulbar neuritis in multiple sclerosis most often occurs acutely. His clinic corresponds to the one given in the previous section.
Additionally, it should be noted that in rare cases the disease is accompanied by slight swelling of the upper eyelid. Pain when moving the eyeball and exophthalmos last for several days.
Loss of vision
at the beginning of the disease it is very sharp. Vision is mostly reduced to light perception or movement of the hand in front of the eye. Sometimes visual acuity remains at several hundredths. The fundus picture in acute retrobulbar neuritis due to multiple sclerosis can be very diverse. This has already been mentioned earlier, when presenting general clinical data. According to our observations, among 13 patients, the fundus of the eye remained normal in 5, mild neuritis was noted in 4, and neuritis with edema was noted in 4.
The picture of neuritis is usually mild. With neuritis with edema, most often there is only a slight swelling of the nipple tissue. Much less often, an ophthalmoscopic picture resembling a congestive nipple is observed, as the following observation shows. Observation 11.
Patient M-vich, 36 years old, in mid-August 1946 felt pain in her left eye when moving the eyeball and a week later she noticed decreased vision in her left eye.
31/VIII visual acuity of the right eye 1.0; left 0.02. The optic nerve nipple of the left eye is hyperemic, enlarged in diameter, and the boundaries are blurred. There is tissue swelling throughout the nipple with protrusion into the vitreous body. The veins are sharply dilated and tortuous. The fundus of the right eye is unchanged. 10/IX visual acuity of the right eye 1.0; left 0.04. When examining the visual field with a white mark of 10 mm in the left eye, a central scotoma was determined within 10-20°, uniform in all meridians. The scotoma in the central part is absolute, in the periphery it is relative. In addition, there was a slight narrowing of the boundaries of the visual field. The field of vision of the right eye is unchanged.
A neurologist diagnosed an organic disease of the central nervous system; suspicion of multiple sclerosis.
The patient received a course of intravenous glucose infusions. Subsequently, vision began to improve rapidly. 17/IX visual acuity of the left eye 0.1, 21/IX - 0.4, 23/IX - 0.6. On 26/IX, in the left eye, the temporal half of the optic nerve papilla showed blanching, its boundaries were clear, the arteries were slightly narrowed. Field of vision of the left eye: a blurred narrowing of the boundaries to white, a small absolute paracentral scotoma.
Thus, the patient, along with non-inflammatory swelling of the optic nerve nipple, had a rapid and sharp decrease in vision in combination with a central scotoma
. The latter allows us to consider this disease as acute retrobulbar neuritis with localization of the focus of inflammation near the eyeball and collateral non-inflammatory swelling of the nipple. The correctness of this interpretation is confirmed by the fact that with the subsequent development of optic nerve atrophy, visual acuity rose to 0.6, which could not have happened if the atrophy had developed due to a stagnant nipple.
Pathological changes in neuritis with edema due to multiple sclerosis were first described by Chirkovsky. This observation is given below.
A 25-year-old patient was admitted on January 29, 1912 to the clinic of nervous diseases in serious condition, with symptoms of motor aphasia and paresis of the right hand. The pupils are evenly dilated, their reaction to light and close proximity is absent. On the left eye there is paresis of the internal rectus muscle. In the fundus of both eyes there is neuritis with edema, a slight protrusion of the nipples above the level of the surrounding retina. There are small hemorrhages in the retina of the left eye near the nipple. 13/II the patient died.
A pathological examination of the brain and spinal cord revealed scattered focal changes. Almost completely preserved axial cylinders
. Pathological diagnosis: acute multiple sclerosis.
A study of the optic nerves and chiasm found the following:
. The nipple tissue is swollen. The veins are greatly dilated and filled with blood. Infiltration of the walls of blood vessels in the nipple area is extremely insignificant. The highest protrusion of the nipple above the level of the surrounding retina is 2/3 mm. The nerve fibers of the optic nerves along almost the entire length from the lamina cribrosa to the chiasm are devoid of a pulpy membrane. The same thing is noted in the chiasmus. Only when moving into the optic tracts do the nerve fibers appear normal. The preserved axial cylinders appear swollen in places, sometimes fusiformly thickened. Along the entire length of the optic nerves and chiasm, a proliferation of glial fibers and an increase in the number of astrocytes are observed. The vessels are dilated and filled with blood. In the anterior part of the optic nerves, thickening of the connective tissue septa is noted. The changes found in the optic nerves and chiasm completely coincide with the changes in the spinal cord and brain.
Explaining the pathogenesis of nipple swelling, Chirkovsky notes the following. In the optic nerves throughout, the phenomena of stasis were striking: The vessels were dilated, in places filled with red blood cells. The perivascular lymphatic spaces are also greatly dilated. Difficulties in blood and lymph circulation in the optic nerve may have been the cause of nipple swelling.
In most patients, after the initial period of suppression of functions, a period of improvement begins, leading to a significant increase in visual acuity and improvement in the visual field. The duration of individual attacks of retrobulbar neuritis can vary widely. By the duration of the attack we mean the time from the first noted decrease in visual acuity to the maximum increase in visual acuity towards the end of the disease. An attack of retrobulbar neuritis most often lasts from 1 to 3 months.
In some cases, there is a sudden increase in visual acuity
: It stays low for a long period and then rises sharply over several days. Along with an increase in visual acuity, the central scotoma gradually undergoes reverse development.
The reverse development of central scotomas was described by us in the previous section.
Acute retrobulbar neuritis in multiple sclerosis often leads to the development of simple optic nerve atrophy
. The latter is most often expressed by blanching of the temporal half of the nipple. Along with this, complete blanching of the optic nerve nipple is observed. As already mentioned, sometimes the fundus of the eye remains normal after suffering retrobulbar neuritis. The final condition of the fundus in 13 of our patients was as follows. In 8 patients, simple atrophy of the optic nerve developed (in 6 - blanching of the temporal half of the nipple, in 2 - complete blanching of the optic nerve nipple). In the remaining 5 patients, the fundus remained normal by the end of the disease. Optic nerve atrophy mostly developed 1–3 months after the onset of the disease.
The prognosis for acute retrobulbar neuritis due to multiple sclerosis is usually favorable. For the most part, high or almost sufficient visual acuity is maintained. Long-term blindness occurs only as a rare exception.
Along with the general course of the disease described above, retrobulbar neuritis in multiple sclerosis is characterized by a number of features that distinguish it from retrobulbar neuritis of other etiologies. These include:
- remitting course with relapses,
- tendency to heal spontaneously
- and discrepancies between the fundus picture and the state of functions.
Remitting course
is as follows. After retrobulbar neuritis has resolved with significant or even complete restoration of function, after some time a new attack begins. The number of these attacks and the intervals of relative well-being between them may vary. Sometimes individual attacks follow each other with an interval of several days or weeks, in other cases - several months. Moreover, in the same patient, the intervals between individual attacks may also be unequal. The course of retrobulbar neuritis during repeated attacks can be very different. As a result of this course, the picture of the disease in such cases becomes very varied and peculiar.
Among the patients we observed, a relapsing course of the disease was observed in 4. Each of them had from 2 to 5 attacks, and the intervals between attacks lasted from 7 days to 13 months.
Such a remitting course with subsequent relapses is characteristic of the initial period of multiple sclerosis and is observed not only in relation to eye symptoms, but also in relation to other manifestations of the disease. It is caused by the fact that with multiple sclerosis, repeated eruption of plaques
and their partial reverse development in the same area of the central nervous system. Repeated eruption of plaques in the optic nerve is confirmed by pathological observations of Uthof, as well as Welter.
With the development of optic nerve atrophy after retrobulbar neuritis due to multiple sclerosis, there is often a sharp discrepancy between the condition of the fundus and the functions of the eye
. Despite the ophthalmoscopically clearly expressed picture of simple atrophy, visual acuity can be high. Among the 8 patients we observed with optic nerve atrophy after retrobulbar neuritis, visual acuity was 1.0 in 4 eyes and 0.9 in 2 eyes. In 1 case, despite a clear ophthalmoscopic picture of atrophy, not only visual acuity was high (1.0 in one eye and 0.9 in the other eye), but also the visual field was normal. In other cases, some changes were noted in the visual field. The latter consisted of a narrowing of the borders to red with normal borders to white and the presence of relative central scotomas to white and red.
A sharp discrepancy between the state of functions and the ophthalmoscopic picture was also observed by F. I. Yuzefova and F. L. Ravikovich.
Sometimes the discrepancy between the condition of the fundus and visual acuity occurs in a very peculiar way. The progressive development of optic atrophy coincides with a progressive and very significant increase in visual acuity. While the optic nerve becomes increasingly paler, visual acuity improves. We observed such a course of the disease in 3 patients.
This uniqueness can be explained by two points.
With retrobulbar neuritis, the focus of the disease is localized in the optic nerve at a certain distance from the eyeball. The atrophy that subsequently develops is descending atrophy. For the development of this descending atrophy, a certain period of time is required, the value of which is determined both by the distance of the source of inflammation from the eyeball and by the intensity of the process. During the time that descending atrophy descends to the nipple, the inflammatory process can be safely resolved, and then the function of the fibers that did not die in the process of inflammation is restored. Therefore, despite the development of optic nerve atrophy, visual acuity may improve.
High visual acuity in optic nerve atrophy
, developing with retrobulbar neuritis due to multiple sclerosis, can be explained by the characteristics of the pathological process itself. As already mentioned, within the plaques formed in the central nervous system, only the disintegration of the pulpy sheaths of nerve fibers occurs, while the axial cylinders are preserved. Only in outbreaks of great antiquity do the axial cylinders swell, lose the regularity of their contours and disintegrate. For the optic nerve, the preservation of axial cylinders in multiple sclerosis plaques was proven by studies by Utgof, Welter, as well as Wilbrand and Zenger. This preservation of the axial cylinders may explain the good visual acuity in ophthalmoscopically pronounced optic nerve atrophy. The paleness of the nipple in these cases is caused not so much by atrophy of the nerve fibers as by the desolation of the capillary network.
Below we present a case history that well illustrates the course and outcome of retrobulbar neuritis in multiple sclerosis.
Observation 12.
Patient S. L., 28 years old.
12/111 1946 was admitted to the hospital of the Leningrad Ophthalmological Institute with a complaint of blindness in the right eye. 25/II noticed swelling of the right upper eyelid and pain in the right eye, especially with eye movements. At the same time, she noted a decrease in vision in the right eye, which subsequently progressed rapidly, and by 28/2 the eye completely ceased to see. On admission, visual acuity of the right eye is equal to the movement of the hand in front of the face. Visual acuity of the left eye is 1.0. The optic nerve nipple of the right eye is swollen, somewhat embedded in the vitreous body, its borders are washed away; the veins are dilated, the arteries are somewhat narrowed. In the left eye there is a mild pallor of the temporal half of the nipple.
On general examination, RW in the blood was negative, urine and blood tests did not reveal anything pathological, and the x-ray of the skull showed no changes in the nasal cavities and sella turcica. No signs of organic disease of the central nervous system were found.
During her hospital stay, the patient received 10 intravenous glucose infusions. By 26/III, visual acuity of the right eye was 0.01. The boundaries of the visual field are normal. There was an absolute central white scotoma within 10-20°. Then the vision of the right eye began to rapidly increase: 6/IV - 0.04; 9/IV - 0.2; 11/IV - 0.4 and 24/IV it was 0.7 with correction. During this time, the following changes occurred in the fundus of the eye: 6/IV swelling of the nipple of the right optic nerve disappeared, then blanching of the nipple appeared, mainly in the temporal half, and the boundaries became distinct.
Due to the young age of the patient and the absence of other etiological factors, we suggested that retrobulbar neuritis was an early and so far the only sign of multiple sclerosis.
At the end of April, the patient was discharged for outpatient observation. 17/V marked blanching of the temporal halves of the nipples of the optic nerves of both eyes; the boundaries are distinct, the caliber of the vessels is not changed. Visual acuity of the right eye is 0.7, left 1.0. The boundaries of the visual field of the right eye for white (examination with 5 and 2 mm marks) are normal; to red - narrowed in all meridians to 10-20°. Within 3-5° there was a central relative scotoma in white and absolute scotoma in red.
25/V the patient felt pain in the left eye when moving the eyeball, 3/VI noticed that she saw worse with this eye. Then the patient had slight exophthalmos of the left eye. The pupils are uniform, their reaction to light and close proximity is lively. Movement of the eyeballs is not limited. The fundus of both eyes was unchanged compared to the data of previous studies. Visual acuity in both eyes was 0.7; glasses did not improve vision. The boundaries of the visual field of the left eye for white are normal, but for red they are sharply narrowed. There was a central relative scotoma of white color in different meridians from 5 to 10°. The neurologist did not find any symptoms of diseases of the central nervous system. The patient suffered from pneumonia from 15/VI to 25/VII and returned again only on 17/IX. During this time, no treatment was applied to the left eye. Upon inspection, the following was found. There is no exophthalmos. There was blanching of the temporal halves of the optic nerves of both eyes. Visual acuity wallpaper* eye 1.0. The boundaries of the visual fields for white (examination with marks of 5 and 2 mm) are normal, for red they are slightly narrowed. On the right eye there is a scotoma ranging from 3 to 5°, relative to white and absolute to red. There was a gap in the center of the scotoma within 1-2°.
5/X, based on neurological data, the initial stage of multiple sclerosis was diagnosed. 10/XI fundus and visual acuity of both eyes without changes. The boundaries of the visual fields for white are normal. On the right eye there is a relative central scotoma that is red in color with a small gap in the center. On the left eye there is a sharp narrowing of the borders to red.
Thus, there is reason to assert that in this case the patient suffered two attacks of retrobulbar neuritis
with an interval of 1.5 months. During the first attack, the vision in the right eye initially dropped to almost blindness, after two weeks it improved to 0.01 and then over the course of a month rose to 0.7. In the visual field, an absolute central scotoma of white color was noted in the initial period. Subsequently, the scotoma decreased, became relative, and a lumen appeared in its center. The second attack also involved the left eye, and here a central scotoma developed, which subsequently completely disappeared. During both attacks, pain was observed when moving the eyeball, as well as some inflammatory phenomena (swelling of the right upper eyelid, exophthalmos on the left). During the first attack, the patient was treated with intravenous glucose infusions; the second attack passed without treatment. Both attacks ended in the same way regarding visual acuity. By the end of the observation, visual acuity in both eyes was equal to 1.0, and in the fundus there was simple atrophy of the optic nerves (blanching of the temporal halves of the nipples). In this patient, retrobulbar neuritis was for a long time the only manifestation of the underlying disease. Other neurological symptoms of multiple sclerosis appeared only 7 months after the onset of the optic nerve disease.
In the majority of patients with retrobulbar neuritis in multiple sclerosis, changes in the visual field do not make it possible to establish the localization of the process in the optic nerve. Existing central scotomas with normal boundaries of the visual field indicate disease of the papillo-macular bundle. The latter, however, can be affected in any part of the optic nerve behind the eyeball. In these cases, the localization of the process can to a certain extent be judged by the state of the fundus.
The presence of neuritic changes in the fundus of the eye, especially in cases where they are accompanied by swelling of the nipple, suggests that the plaque is located in the orbital part of the optic nerve, not far from the eyeball.
Among the patients we observed, 13 had 23 attacks of retrobulbar neuritis, 6 attacks passed without any treatment. This indicates a greater tendency of the disease to heal itself.
, which coincides with the data available in the literature. Remissions are more often observed in the early period of the disease. Since retrobulbar neuritis is an early symptom of multiple sclerosis, their tendency to spontaneous healing becomes understandable in connection with the clinical picture of the underlying disease. Naturally, given this state of affairs, we must be very careful in assessing the effectiveness of the therapeutic measures we use. In the case of a favorable resolution of retrobulbar neuritis that has been treated, it is impossible to say with certainty whether this favorable outcome is due to the therapeutic effect, or whether we are dealing with another remission. At the same time, one should not completely abandon the treatment of retrobulbar neuritis in multiple sclerosis. In accordance with modern guidelines of neurologists, retrobulbar neuritis in multiple sclerosis is recommended to be treated with intravenous infusions of hexamine or glucose with nicotinic acid. In recent years, the Margulis-Shubladze vaccine has been used.
In conclusion, let us dwell on multiple sclerosis, which occurs monosymptomatically
. According to literature data, the first symptom of multiple sclerosis in 15% of cases was visual impairment. As many authors point out, sometimes retrobulbar neuritis can remain the only symptom for a long time, and other neurological symptoms of multiple sclerosis are revealed only much later. Among our 13 patients with retrobulbar neuritis, optic nerve disease as the only symptom of multiple sclerosis was observed for a long time in 6. Moreover, general neurological symptoms of multiple sclerosis were identified in the following periods after the onset of retrobulbar neuritis: from 3 to 7 months - in 2, from 1 to 2 years - in 2, after 2 years 7 months - in 1, after 4 years - in 1.
Wilbrand and Zenger provide the following data based on collected material from various authors. Among 29 patients with retrobulbar neuritis, who were subsequently diagnosed with multiple sclerosis, neurological symptoms of this disease were detected in the following periods: after a few weeks - in 2 patients, after a few months - in 2, from 1 to 3 years - in 7, from 4 to 6 years - in 4, from 7 to 9 years - in 6, after 10 or more years - in 8.
Fleischer, over a long period of time, found out the further fate of 30 patients who had suffered retrobulbar neuritis of unknown etiology. 14 of them were found to have multiple sclerosis on follow-up. Written data obtained from 7 patients who could not be examined also confirmed the presence of multiple sclerosis. Thus, in 21 out of 30 patients with retrobulbar neuritis of unknown etiology, symptoms of multiple sclerosis were discovered over a long period of time.
Based on the above, we believe that in case of acute retrobulbar neuritis of unknown etiology in young people, one should always presumably think about the possibility of multiple sclerosis
. In this regard, this group of patients should continue to remain under the supervision of an ophthalmologist and neurologist.
—-
Article from the book: Diseases of the visual pathway | E. J. Tron
Treatment and prognosis of optic neuritis
Urgent hospitalization is indicated for patients. Treatment of the disease is aimed at suppressing the inflammatory reaction and infection, desensitization, immunocorrection, dehydration, and activation of metabolism in the tissues of the central nervous system. In the first week of treatment, antibiotics, intravenous infusions of glucose, diacarb with potassium preparations (panangin), corticosteroids, administration of magnesium sulfate, B vitamins, nootropil, actovegin are prescribed.
In parallel with drug therapy, doctors find out the causes of the disease. After identifying the causes of optic neuritis, specific treatment is prescribed to eliminate them. This could be immunocorrective or antiviral therapy for herpes, specific treatment for tuberculosis, surgical treatment of sinusitis.
The patient may require emergency treatment, which includes detoxification measures. Prescribe oral administration of a 30% solution of ethyl alcohol in a dose of 100 ml, gastric lavage with a 4% solution of baking soda and other measures that are usually used for acute poisoning. If the patient has symptoms of optic nerve atrophy, he is additionally prescribed antispasmodics and medications that improve microcirculation (trental, nicotinamide, sermion, nicotinic acid).
The prognosis for the patient depends on the type of disease and severity. If you start treating the pathology on time and choose the most optimal tactics, you can achieve a complete recovery of the patient. However, often after the end of treatment, partial (in rare cases complete) atrophy of the optic nerve occurs.
Features of therapy
It is necessary to begin treatment of optic neuritis only after the cause of its development has been established. It is this that needs to be eliminated. Naturally, in the future the patient will be prescribed rehabilitation therapy. Treatment of the acute form of the disease is carried out strictly in a hospital neurological or ophthalmological department.
Initial therapy involves eliminating symptoms and maintaining the functionality of the optic nerve. As for medications, the patient will be prescribed the following medications:
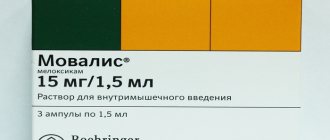
- Glucocorticosteroids: Dexamethasone, Methylprednisolone. These drugs help reduce the inflammatory process and swelling of the optic disc. For the treatment of intrabulbar lesions, general systemic steroid drugs are most often used. To treat retrobulbar neuritis, special injections are required, which are made into the tissue behind the eye. The duration of corticosteroid use is 5 days. Moreover, the dose should be maximum. After completion of therapy, the daily amount of steroids is gradually reduced. You cannot take them on your own, reduce the dosage or end the course.
- Preparations to eliminate intoxication of the body: “Hemodez”. These drugs are used intravenously, in the form of droppers. In some cases, these drugs need to be given to a person very quickly (in case of acute poisoning and a rapid deterioration in the person’s well-being).
Hemodez-N refers to a drug that has a detoxifying effect on the body. Price in pharmacies from 94 rubles.
- Vitamin preparations containing thiamine, pyridoxine, nicotinic acid. The tablet form of administration is suitable. They improve metabolic processes in nervous tissue. With the help of such drugs, the transmission of nerve impulses is stimulated. Sometimes vitamin supplements are used as intramuscular injections.
- Drugs used to restore normal microcirculation and nutrition of nervous tissue: Actovegin, Trental. They are used after the acute stage of the pathology has been relieved, if visual function is severely deteriorated.
- Means for improving impulse transmission: Nivalin.
If the nature of the pathology is viral, then you cannot do without antiviral drugs: “Amiksin”. Antibiotics are required to kill germs. However, specialists are not always able to establish the true cause of the pathology. Most often, combination antibiotics or cephalosporins are prescribed: Amoxiclav, Ceftriaxone.
Laser stimulation of the eye and retina not only relieves many of the negative effects of eye strain, but also produces long-lasting positive results.
The course of treatment with antibacterial drugs does not exceed 7 days. However, you should not use drugs that have an ototoxic effect on the nerves.
After using drug therapy, physiotherapeutic procedures are used to improve the result: magnetic and electrotherapy, eye stimulation with a laser beam.
Prevention
As you know, one disease often entails another, and inflammation of the optic nerve can develop as a result of other ailments. In order to reduce the risk of neuritis, you must follow several rules:
- avoid injuries associated with the skull, and in particular with the orbits and the eyes themselves;
- lead a healthy lifestyle, do not drink alcohol, especially in large quantities and often;
- Strengthen your immune system in every possible way, harden yourself and take enough vitamins;
- A healthy diet and compliance with all hygiene rules also play an important role;
- try to prevent infectious diseases, including sexually transmitted diseases;
- undergo regular preventive medical examinations.