In the first month of life, a newborn is required to undergo some health examinations, including neurosonography. What is neurosonography, how safe is it, what is it needed for, what results does it give - we will look at all this in the article.
- 2 Why and to whom is it prescribed?
- 3 Types of NSG
- 4 Are there similar research methods along with NSG?
- 5 Evaluation and interpretation of results
5.1 Standard indicators
What is neurosonography
Neurosonography (NSG, or ultrasound of the brain) is a method of studying the brain and other anatomical structures located in the cranial cavity using ultrasound. This examination is prescribed for children in the first year of life (and the earlier, the better), since the fontanel is still open, and ultrasound can penetrate the cranial cavity. This procedure has no contraindications and is therefore safe for the child’s health. Thus, all newborns under the age of 1 month are recommended to undergo neurosonography.
Reasons for the development of pathology
Agenesis of the septum pellucidum of the brain is a rare and abnormal disease of the central nervous system.
Each membrane of the brain performs a specific function. The septum pellucidum is the medulla and consists of two plates.
Agenesis is one of the components of most congenital brain defects. The absence of a septum is due to improper formation or underdevelopment of the corpus callosum.
Agenesis of the cavity of the transparent septum is classified as an anomaly of the central nervous system and is quite rare. This pathology is characterized by the complete or partial absence of the cavity of the transparent septum. This anomaly has not been sufficiently studied. The defect develops already in the second week after conception.
Predisposing factors to the development of agenesis:
- Heredity
- Mutations
- Intrauterine infections
- Insufficient supply of nutrients to the fetus
The development of pathology is also influenced by toxic substances and medications that the woman took during pregnancy. The use of drugs such as Trimethadione, Phenytoin, Isotretinoin and some others can contribute to congenital brain abnormalities. These drugs, used in the first trimester of pregnancy, affect the formation of the brain and can lead to developmental defects.
If the expectant mother drank alcohol, the child developed fatal alcohol syndrome. This also predisposes to congenital pathology. Infections in the mother or injuries sustained during the 12th to 22nd weeks of pregnancy can lead to disturbances in the development of the fetal brain.
Most often, this pathology is inherited or occurs due to spontaneous mutations.
Agenesis of the septum pellucidum does not occur in isolation. Typically, the pathology is part of various cerebral anomalies: agenesis of the corpus callosum, porencephaly, hydranencephaly, septo-optic dysplasia, holoprosencephaly, etc.
Clinical manifestations
Signs of pathology appear in the first years of a baby’s life
Severe symptoms appear in childhood during the first two years of life. At birth, children with agenesis appear healthy and develop normally until three months of age. At this stage of development, the first signs of pathology appear.
With agenesis, the following symptoms are observed:
- The appearance of porencephaly
- Microencephaly
- Insufficient formation of the gyrus
- Aicardi syndrome
- Atrophy of the optic and auditory nerves
Also, against the background of the pathology, early puberty, seizures and seizures can be observed. Pathology can manifest itself in different ways. With partial agenesis, these signs may not be observed in the child and may not affect development, but will need to be regularly monitored by a neurologist. Sometimes agenesis can occur without clinical manifestations for several years.
Why and to whom is it prescribed?
Neurosonography is indicated for all children, preferably in the first month of life, especially:
- premature;
- those born with low birth weight;
- with an unusual head shape;
- with suspicion of intrauterine infection;
- born with hypoxia;
- with birth trauma;
- in post-term pregnancy;
- during delivery by cesarean section;
- with neurological diseases or symptoms indicating them;
- with developmental anomalies of other organs or systems.
Using ultrasound, you can evaluate the structure of the brain, examine the structure of the soft tissues of the head, and see the presence or absence of deformations and tumors. Since this method is indicative, according to pediatric neurologists from the Russian Medical Server, it is proposed to use more accurate methods for identifying pathologies in case of suspicions identified during NSG (for example, a tomogram). An ultrasound of the brain can show the presence of serious problems in the child, which will need to be confirmed by other, more accurate studies.
The main misconceptions that accompany the NSG procedure are the common diagnoses of “increased intracranial pressure” and “perinatal encephalopathy”. Neurologists often make a diagnosis of increased intracranial pressure based on the results of an ultrasound of the brain and some behavioral characteristics of the child: dilated ventricles of the brain, sleep disturbances, hyperactivity, tiptoeing (or hypertonicity of the muscles of a child who cannot yet walk), tremor, developmental disorders, “marbled” color of the skin. The above diagnosis can only be made based on a combination of various factors that can be interpreted by an experienced medical specialist, taking into account the patient’s complaints: headaches, nausea, vomiting, regurgitation, blurred vision, consciousness, excessive growth of head circumference, bulging fontanelle, dehiscence of sutures between the bones of the skull. Of course, a small child will not be able to tell his parents about the listed symptoms, so it is necessary to notice changes in the baby’s behavior and find a competent specialist who, if necessary, will prescribe appropriate treatment. Thus, neurosonography does not allow one to assess whether the child really has increased intracranial pressure, but it can clarify the cause of the disease and its depth. As for the term “perinatal encephalopathy,” which characterizes disorders of brain function that occur during the period of intrauterine development, in accordance with the modern international classification of diseases, such a diagnosis does not exist. Be sure to monitor your child’s condition, his mood and behavior!
You can undergo neurosonography at the multidisciplinary medical holding "SM-Clinic": https://detskiy-medcentr-spb.ru/uslugi/uzi1/uzi-golovnogo-mozga-nejrosonografiya
neurosonography of the brain
Authors : Zaitsev S.V.
published 08/20/2015 14:00 in the categories Nervous, mental and psychological diseases, Neurology and psychiatry
Key words: perinatal encephalopathy (PEP) or perinatal damage to the central nervous system (PP CNS), hypertensive-hydrocephalic syndrome (HHS); dilatation of the cerebral ventricles, interhemispheric fissure and subarachnoid spaces, pseudocysts on neurosonography (NSG), muscular dystonia syndrome (MSD), hyperexcitability syndrome, perinatal convulsions.
It turns out... more than 70-80%! Children of the first year of life come for consultation to neurological centers about a non-existent diagnosis - perinatal encephalopathy (PEP):
Child neurology is a relatively new field, but is already going through difficult times. At the moment, many doctors practicing in the field of infant neurology, as well as parents of infants with any changes in the nervous system and mental sphere, find themselves “between two fires.” On the one hand, the school of “Soviet child neurology” is excessive diagnosis and incorrect assessment of functional and physiological changes in the nervous system of a child in the first year of life, combined with long-outdated recommendations for intensive treatment with a variety of medications. On the other hand, there is often an obvious underestimation of existing psychoneurological symptoms, ignorance of general pediatrics and the fundamentals of medical psychology, some therapeutic nihilism and fear of using the potential of modern drug therapy; and as a result - lost time and missed opportunities. At the same time, unfortunately, a certain (and sometimes significant) “formality” and “automaticity” of modern medical technologies lead, at a minimum, to the development of psychological problems in the child and his family members. The concept of “norm” in neurology at the end of the 20th century was sharply narrowed; now it is intensively and not always justifiably expanding. Probably the truth is somewhere in the middle...
According to data from the Perinatal Neurology Medical Clinic and other leading medical centers in Moscow (and probably in other places), so far, more than 80%!!! Children in their first year of life are referred by a pediatrician or neurologist from a district clinic for a consultation regarding a non-existent diagnosis - perinatal encephalopathy (PEP):
The diagnosis of “perinatal encephalopathy” (PEP) in Soviet child neurology very vaguely characterized almost any dysfunction (and even structure) of the brain in the perinatal period of a child’s life (from about 7 months of intrauterine development of the child and up to 1 month of life after childbirth), arising as a result pathologies of cerebral blood flow and oxygen deficiency.
Such a diagnosis was usually based on one or more sets of any signs (syndromes) of a possible disorder of the nervous system, for example, hypertensive-hydrocephalic syndrome (HHS), muscular dystonia syndrome (MDS), hyperexcitability syndrome.
After conducting an appropriate comprehensive examination: clinical examination in combination with analysis of data from additional research methods (ultrasound of the brain - neurosonography) and cerebral circulation (Dopplerography of cerebral vessels), fundus examination and other methods, the percentage of reliable diagnoses of perinatal brain damage (hypoxic, traumatic, toxic-metabolic, infectious) is reduced to 3-4% - this is more than 20 times!
The most bleak thing about these figures is not only a certain reluctance of individual doctors to use the knowledge of modern neurology and conscientious delusion, but also a clearly visible psychological (and not only) comfort in the pursuit of such “overdiagnosis.”
Hypertension-hydrocephalic syndrome (HHS): increased intracranial pressure (ICP) and hydrocephalus
Until now, the diagnosis of “intracranial hypertension” (increased intracranial pressure ( ICP) ) is one of the most commonly used and “favorite” medical terms among pediatric neurologists and pediatricians, which can explain almost everything! and at any age, complaints from parents.
For example, a child often cries and shudders, sleeps poorly, spits up a lot, eats poorly and gains little weight, eyes widen, walks on tiptoes, his arms and chin tremble, there are convulsions and there is a lag in psycho-speech and motor development: “it’s only his fault - increased intracranial pressure." Isn't that a convenient diagnosis?
Quite often, the main argument for parents is “heavy artillery” - data from instrumental diagnostic methods with mysterious scientific graphs and figures. Methods can be used either completely outdated and uninformative /echoencephalography ( ECHO-EG ) and rheoencephalography ( REG )/, or examinations “from the wrong opera” ( EEG ), or incorrect, in isolation from clinical manifestations, subjective interpretation of normal variants during neurosonodopplerography or tomography.
Unhappy mothers of such children unwittingly, at the suggestion of doctors (or voluntarily, feeding on their own anxiety and fears), pick up the flag of “intracranial hypertension” and for a long time end up in the system of monitoring and treatment of perinatal encephalopathy.
In fact, intracranial hypertension is a very serious and quite rare neurological and neurosurgical pathology. It accompanies severe neuroinfections and brain injuries, hydrocephalus, cerebrovascular accidents, brain tumors, etc.
Hospitalization is mandatory and urgent!!!
Intracranial hypertension (if it really exists) is not difficult for attentive parents to notice: it is characterized by constant or paroxysmal headaches (usually in the morning), nausea and vomiting not associated with food. The child is often lethargic and sad, is constantly capricious, refuses to eat, he always wants to lie down and cuddle with his mother.
A very serious symptom can be strabismus or difference in pupils, and, of course, disturbances of consciousness. In infants, bulging and tension of the fontanelle, divergence of the sutures between the bones of the skull, as well as excessive growth of the head circumference are very suspicious.
Without a doubt, in such cases the child must be shown to specialists as soon as possible. Quite often, one clinical examination is enough to exclude or preliminarily diagnose this pathology. Sometimes additional research methods are required (fundus examination, neurosonodopplerography, computed tomography or magnetic resonance imaging of the brain).
Of course, expansion of the interhemispheric fissure, cerebral ventricles, subarachnoid and other spaces of the cerebrospinal fluid system on neurosonography (NSG) images or brain tomograms (CT or MRI) cannot serve as evidence of intracranial hypertension. The same applies to cerebral blood flow disorders isolated from the clinic, identified by vascular Dopplerography, and “finger impressions” on a skull x-ray.
In addition, there is no connection between intracranial hypertension and translucent vessels on the face and scalp, walking on tiptoes, trembling hands and chin, hyperexcitability, developmental disorders, poor academic performance, nosebleeds, tics, stuttering, bad behavior, etc. and so on.
That’s why, if your baby has been diagnosed with “PEP, intracranial hypertension”, based on “goggle” eyes (Graefe’s symptom, “setting sun”) and walking on tiptoes, then you shouldn’t go crazy in advance. In fact, these reactions may be characteristic of easily excitable young children. They react very emotionally to everything that surrounds them and what happens. Attentive parents will easily notice these connections.
Thus, when diagnosing PEP and increased intracranial pressure, it is naturally best to contact a specialized neurological clinic. This is the only way to be sure of the correct diagnosis and treatment.
It is absolutely unreasonable to begin treatment of this serious pathology on the recommendations of one doctor based on the above “arguments”; in addition, such unreasonable treatment is not at all safe.
Just look at the diuretic drugs that are prescribed to children for a long time, which has an extremely adverse effect on the growing body, causing metabolic disorders.
There is another, no less important aspect of the problem that must be taken into account in this situation. Sometimes medications are necessary and the wrongful refusal of them, based only on the mother’s (and more often than not the father’s) own conviction that medications are harmful, can lead to serious troubles. In addition, if there really is a serious progressive increase in intracranial pressure and the development of hydrocephalus, then often incorrect drug therapy for intracranial hypertension entails the loss of a favorable moment for surgical intervention (shunt surgery) and the development of severe irreversible consequences for the child: hydrocephalus, developmental disorders, blindness , deafness, etc.
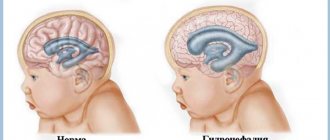
Now a few words about the equally “adored” hydrocephalus and hydrocephalic syndrome . In fact, we are talking about a progressive increase in intracranial and intracerebral spaces filled with cerebrospinal fluid (CSF) due to the existing! at that moment of intracranial hypertension. In this case, neurosonograms (NSG) or tomograms reveal dilations of the ventricles of the brain, interhemispheric fissure and other parts of the cerebrospinal fluid system that change over time. Everything depends on the severity and dynamics of the symptoms, and most importantly, on the correct assessment of the relationships between the increase in intracerebral spaces and other neural changes. This can be easily determined by a qualified neurologist. True hydrocephalus, which does require treatment, like intracranial hypertension, is relatively rare. Such children must be observed by neurologists and neurosurgeons at specialized medical centers.
Unfortunately, in ordinary life such an erroneous “diagnosis” occurs in almost every fourth or fifth baby. It turns out that some doctors often incorrectly call a stable (usually slight) increase in the ventricles and other cerebrospinal fluid spaces of the brain hydrocephalus (hydrocephalic syndrome). This does not manifest itself in any way through external signs or complaints and does not require treatment. Moreover, if the child is suspected of having hydrocephalus based on a “large” head, translucent vessels on the face and scalp, etc. - this should not cause panic among parents. The large size of the head in this case plays practically no role. However, the dynamics of head circumference growth is very important. In addition, you need to know that among modern children it is not uncommon to have so-called “tadpoles” whose heads are relatively large for their age (macrocephaly). In most of these cases, infants with large heads show signs of rickets, less often macrocephaly due to the family constitution. For example, dad or mom, or maybe grandpa has a big head, in a word, it’s a family matter and doesn’t require treatment.
Sometimes, when performing neurosonography, an ultrasound doctor finds pseudocysts - but this is not a reason to panic at all! Pseudocysts are single round tiny formations (cavities) containing cerebrospinal fluid and located in typical areas of the brain. The reasons for their appearance, as a rule, are not reliably known; they usually disappear by 8-12 months. life. It is important to know that the existence of such cysts in most children is not a risk factor for further neuropsychic development and does not require treatment. However, although quite rare, pseudocysts form at the site of subependymal hemorrhages, or are associated with perinatal cerebral ischemia or intrauterine infection. The number, size, structure and location of cysts provide specialists with very important information, taking into account which, based on a clinical examination, final conclusions are formed.
Description of NSG is not a diagnosis! and not necessarily a reason for treatment.
Most often, NSG data provide indirect and uncertain results, and are taken into account only in conjunction with the results of a clinical examination.
Once again, I remind you of the other extreme: in difficult cases, sometimes there is a clear underestimation on the part of parents (less often, doctors) of the child’s problems, which leads to a complete refusal of the necessary dynamic observation and examination, as a result of which the correct diagnosis is made late, and treatment does not lead to the desired result.
Undoubtedly, therefore, if increased intracranial pressure and hydrocephalus are suspected, diagnosis should be carried out at the highest professional level.
What is muscle tone and why is it so “loved”?
Look at your child’s medical record: is there no such diagnosis as “muscular dystonia”, “hypertension” and “hypotension”? — you probably just didn’t go with your baby to the neurologist’s clinic until he was a year old. This is, of course, a joke. However, the diagnosis of “muscular dystonia” is no less common (and perhaps more common) than hydrocephalic syndrome and increased intracranial pressure.
Changes in muscle tone can be, depending on the severity, either a variant of the norm (most often) or a serious neurological problem (this is much less common).
Briefly about external signs of changes in muscle tone.
Muscular hypotonia is characterized by a decrease in resistance to passive movements and an increase in their volume. Spontaneous and voluntary motor activity may be limited; palpation of the muscles is somewhat reminiscent of “jelly or very soft dough.” Severe muscle hypotonia can significantly affect the rate of motor development (for more details, see the chapter on movement disorders in children of the first year of life).
Muscular dystonia is characterized by a condition where muscle hypotonia alternates with hypertension, as well as a variant of disharmony and asymmetry of muscle tension in individual muscle groups (for example, more in the arms than in the legs, more on the right than on the left, etc.).
At rest, these children may experience some muscle hypotonia during passive movements. When trying to actively perform any movement, during emotional reactions, when the body changes in space, muscle tone increases sharply, pathological tonic reflexes become pronounced. Often, such disorders subsequently lead to improper development of motor skills and orthopedic problems (for example, torticollis, scoliosis).
Muscular hypertension is characterized by increased resistance to passive movements and limitation of spontaneous and voluntary motor activity. Severe muscle hypertension can also significantly affect the rate of motor development.
Violation of muscle tone (muscle tension at rest) can be limited to one limb or one muscle group (obstetric paresis of the arm, traumatic paresis of the leg) - and this is the most noticeable and very alarming sign, forcing parents to immediately consult a neurologist.
It is sometimes quite difficult for even a competent doctor to notice the difference between physiological changes and pathological symptoms in one consultation. The fact is that changes in muscle tone are not only associated with neurological disorders, but also strongly depend on the specific age period and other characteristics of the child’s condition (excited, crying, hungry, drowsy, cold, etc.). Thus, the presence of individual deviations in the characteristics of muscle tone does not always cause concern and require any treatment.
But even if functional disorders of muscle tone are confirmed, there is nothing to worry about. A good neurologist will most likely prescribe massage and physical therapy (exercises on large balls are very effective). Medicines are prescribed extremely rarely.
Hyperexcitability syndrome
(syndrome of increased neuro-reflex excitability)
Frequent crying and whims with or without cause, emotional instability and increased sensitivity to external stimuli, sleep and appetite disturbances, excessive frequent regurgitation, motor restlessness and shuddering, trembling of the chin and arms (etc.), often combined with poor growth weight and bowel dysfunction - do you recognize such a child?
All motor, sensitive and emotional reactions to external stimuli in a hyperexcitable child arise intensely and abruptly, and can fade away just as quickly. Having mastered certain motor skills, children constantly move, change positions, constantly reach for and grab objects. Children usually show a keen interest in their surroundings, but increased emotional lability often makes it difficult for them to communicate with others. They are very impressionable, emotional and vulnerable! They fall asleep extremely poorly, only with their mother, they constantly wake up and cry in their sleep. Many of them have a long-term reaction of fear when communicating with unfamiliar adults with active reactions of protest. Typically, hyperexcitability syndrome is combined with increased mental exhaustion.
The presence of such manifestations in a child is just a reason to contact a neurologist, but in no case is it a reason for parental panic, much less drug treatment.
Constant hyperexcitability is not causally specific and can most often be observed in children with temperamental characteristics (for example, the so-called choleric type of reaction).
Much less frequently, hyperexcitability can be associated and explained by perinatal pathology of the central nervous system. In addition, if a child’s behavior is suddenly disrupted unexpectedly and for a long time for virtually no apparent reason, and he or she develops hyperexcitability, the possibility of developing an adaptation disorder reaction (adaptation to external environmental conditions) due to stress cannot be ruled out. And the sooner the child is examined by specialists, the easier and faster it is possible to cope with the problem.
And, finally, most often, transient hyperexcitability is associated with pediatric problems (rickets, digestive disorders and intestinal colic, hernia, teething, etc.).
There are two extremes in the tactics of monitoring such children. Or an “explanation” of hyperexcitability using “intracranial hypertension” and intense drug treatment often using drugs with serious side effects (diacarb, phenobarbital, etc.). Or complete neglect of the problem, which can subsequently lead to the formation of persistent neurotic disorders (fears, tics, stuttering, anxiety disorders, obsessions, sleep disorders) in the child and his family members, and will require long-term psychological correction.
Of course, it is logical to assume that an adequate approach is somewhere in between...
Separately, I would like to draw the attention of parents to seizures - one of the few disorders of the nervous system that really deserves close attention and serious treatment. Epileptic seizures do not occur often in infancy, but they are sometimes severe, insidious and disguised, and immediate drug therapy is almost always necessary.
Such attacks can be hidden behind any stereotypical and repetitive episodes in the child’s behavior. Incomprehensible shudders, head nods, involuntary eye movements, “freezing,” “squeezing,” “limping,” especially with a fixed gaze and lack of response to external stimuli, should alert parents and force them to turn to specialists. Otherwise, a late diagnosis and untimely prescribed drug therapy significantly reduce the chances of treatment success.
All circumstances of the seizure episode must be accurately and completely remembered and, if possible, recorded on video for further detailed description at the consultation. If convulsions last a long time or are repeated, call “03” and urgently consult a doctor.
At an early age, the child’s condition is extremely changeable, so developmental deviations and other disorders of the nervous system can sometimes be detected only during long-term dynamic monitoring of the baby, with repeated consultations. For this purpose, specific dates for planned consultations with a pediatric neurologist in the first year of life have been determined: usually at 1, 3, 6 and 12 months. It is during these periods that most serious diseases of the nervous system of children in the first year of life can be detected (hydrocephalus, epilepsy, cerebral palsy, metabolic disorders, etc.). Thus, identifying a specific neurological pathology in the early stages of development makes it possible to begin complex therapy on time and achieve the maximum possible result.
And in conclusion, I would like to remind parents: be sensitive and attentive to your kids! First of all, it is your meaningful participation in the lives of children that is the basis for their future well-being. Do not treat them for “alleged illnesses,” but if something worries and worries you, find the opportunity to get independent advice from a qualified specialist. https://lib.komarovskiy.net/fakty-i-zabluzhdeniya-perinatalnoj-nevrologii.html
Types of NSG
There are 3 types of neurosonography:
- transfontanelle;
- transcranial;
- transcranial-transfontanelle.
Transfontanel NSG is the simplest way to visually examine the brain, in which it is examined using a sensor through the fontanelle. Transcranial NSG can be performed on both children and adults, due to the fact that the state of the brain can be viewed through the bones of the skull. Transcranial-transfontanelle NSG is a hybrid of the first two methods and provides a clearer assessment of the structure of the brain.

Transcranial method of performing NSG
Since a transfontanelle neurosonogram is possible only in the first year of a child’s life (while the fontanel is present), the time period for using this procedure is limited. The most informative method, as described above, is transcranial-transfontanelle NSG, which can also be used for up to a year. After the child’s fontanel has closed, the only possible way to assess the state of the brain is transcranial NSG (not counting other alternative methods). All types of neurosonography allow one to evaluate only the structure of the brain and tissues and detect possible formations.
Thus, to identify brain diseases, it is not enough to conduct neurosonography alone. Only in combination with complaints or behavioral characteristics different from the norm, does the NSG give some idea of the diagnosis and possible options for additional examinations.
Diagnostics
Pathology in a child can be detected during pregnancy
The pathology is diagnosed in the 2-3 trimester of pregnancy. During the prenatal period, it is quite difficult to identify brain abnormalities, since the fetus may assume a position that does not allow a clear view of all brain structures. The anomaly can be determined by ultrasound from the 18th week of pregnancy, not earlier. After birth, encephalography, ultrasound, CT, and MRI are prescribed to confirm the diagnosis.
The structures of the cranial cavity in children from birth with possible agenesis can be examined using neurosonography. The procedure is carried out through an open fontanel. Thanks to neurosonography, it is possible to examine the structures of the brain. Ultrasound can detect pathology in the brain even if it is not accompanied by symptoms. Thanks to computed tomography, it is possible to assess the condition in detail and identify possible disorders in the brain, as well as identify possible formations.
If agenesis of the septum pellucidum and corpus callosum is suspected, an MRI is performed.
This method complements neurosonography and makes it possible to detect the absence of a septum and changes in the structure of the ventricles of the brain. Magnetic resonance imaging helps determine the nature of the lesion, the absence of a transparent septum and other pathologies that cannot be determined by ultrasound. If agenesis is partial, then it is even more difficult to identify pathology.
Evaluation and interpretation of results
During NSG, the size and contours of the brain ventricles, the presence of cysts, enlargements, and tumors are assessed. The structures of the ventricles are normally symmetrical, not dilated, the contours are clear, and there are no formations.
Deviations of a few millimeters from the conventional norms on the NSG form should not frighten anyone. Often this is just an error in the method.
Normal indicators
| Part of the brain of a newborn baby (up to 1 month) | Norm, mm |
| Anterior horn of the lateral ventricle | 1–2 |
| Anterior horn body (depth) | 4 |
| Interhemispheric fissure | up to 2 |
| Third ventricle | until 6 |
| Large tank | 3–6 |
| Subarachnoid space | until 3 |
In case of significant deviation from the norms, it is recommended to redo the neurosonography in another place to exclude technical and human factors. The diagnosis should be made only by a competent doctor and on the basis of research.
Definition
Neurosonography is a method of ultrasound examination of the newborn’s brain. Allows you to obtain accurate information about the structure and functioning of structures in the cranium. Based on the results of an ultrasound, it is possible to identify the presence of dangerous abnormalities in the child’s body, which can ultimately save his health and life.

Procedure
Standard neurosonography includes the following steps:
- The child is placed in a place for examination : a couch or a special table. In this case, it is necessary to ensure that his body is fixed - a nurse or parents can handle this. The process itself lasts about 10-15 minutes , and during this time the baby should behave calmly, and his head should be motionless.
- A special gel is applied to the top of the small patient’s head in the area of the large fontanel . What is noteworthy is that the substance differs from its adult counterpart - it has hypoallergenic properties and improves the sensor signal, eliminating the presence of air between the skin and the device.
- installs a device on the treated surface of the head across the area, determining the necessary characteristics of the brain and surrounding structures.
- After the examination is completed, the gel is removed from the baby’s skin using a soft cloth.

This video shows what the doctor sees on the monitor:
How breast fibroma is treated at all stages. This article is all about throat cancer: symptoms and signs.
Here you can see what squamous cell carcinoma looks like in the photo.
Preparation and execution
As already mentioned, brain NSG is safe even for newborns. The procedure is no different from a standard ultrasound examination and does not require special preparation. It can also be carried out in the intensive care unit, and the doctor will not remove the baby from the incubator.
Doctors advise feeding the child so that he does not feel anxious. It is necessary to ensure that the baby's head is still, for which the mother or medical staff support the baby's head. If the baby falls asleep, the procedure will not be postponed; on the contrary, it will go faster and more calmly.

Access to the brain structures is gained through the large fontanel, which is easily palpable between the parietal and frontal bones in children up to 9-12 months. However, the bones of a newborn’s skull are thin and accessible to ultrasound, so the doctor can obtain additional information through the temporal bone, anterior and posterolateral fontanelles (closed at the time of birth), and the foramen magnum.
Before the procedure, a well-fed, dry baby is placed on the couch, holding his head. The fontanelle area and other areas of the skull are lubricated with a hypoallergenic gel, which will prevent friction between the ultrasound sensor and the child’s scalp. Next, a sensor is installed on the head, gradually changing its position and angle to obtain a more accurate picture.
The baby's NSG results are ready 1-2 minutes after the procedure. They must be deciphered by a specialist.