In what part of the head are brain AVMs located?
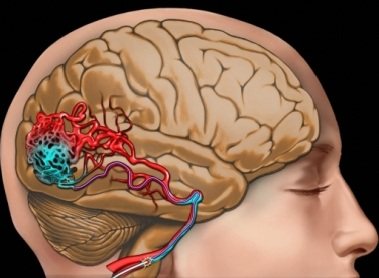
A common location for arteriovenous anomaly is the supratentorial space (upper brain) passing over the cerebellar tent.
To make it clearer, let's put it simply: a vascular defect in approximately 85% of cases is found in the cerebral hemispheres. Lesions of the vascular units of the parietal, frontal, occipital, and temporal lobes of the cerebral hemispheres predominate. In general, AVMs can be located in any pole of the brain, both in the superficial parts and in the deep layers (thalamus, etc.). It is possible to reliably determine the exact localization of the lesion only after undergoing a hardware examination with the ability to visualize soft tissues. The basic principles of diagnosis include MRI and angiography.
Classification of vascular malformations
In this pathological condition, additional formation of vessels occurs in the organ, which connect the arterial, venous and lymphatic parts of the blood supply system. The result of such deformation is the discharge of blood and disruption of the nutrition of the area located just below the affected area.
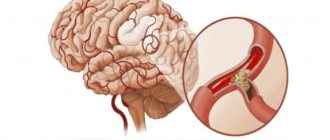
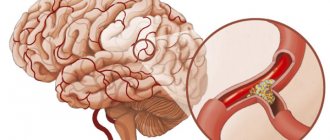
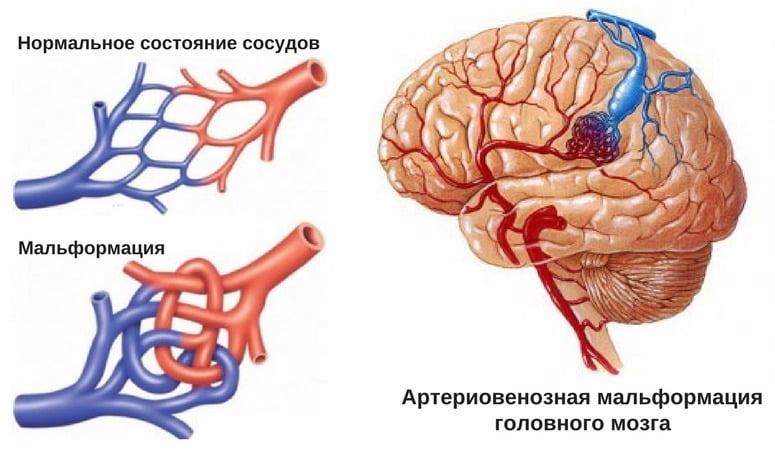
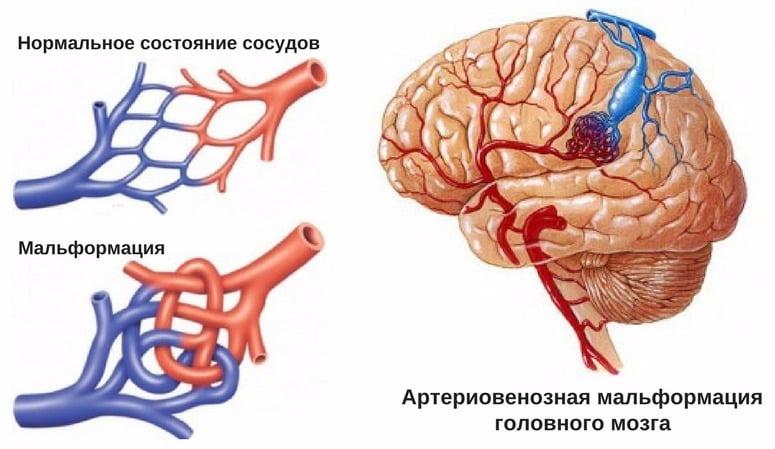
One of the most common diagnoses in medicine is AVM—arteriovenous malformation of cerebral vessels. This disease is characterized by disruption of the connections between arteries and veins, resulting in impaired blood flow. Additional connections look like saccular nodes, and capillaries are completely absent, which leads to accelerated blood supply.
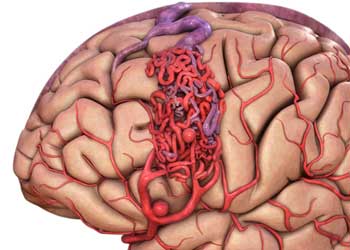
The disease has the appearance of large pulsating vessels. The size of the vascular malformation may vary in each individual case.
This pathology most often manifests itself in men over 30 years of age.
Modern medicine divides brain malformation into several forms:
- Arteriovenous malformation is a type of disease characterized by a complete absence of capillaries connecting the venous and arterial networks.
- Lymphatic pathologies are disorders in which the patient has problems with the lymph nodes. The peculiarity of this form is the frequent absence of a tumor.
- Arnold-Chiari malformation is characterized by displacement of the cerebellum towards the foramen of the occipital lobe, resulting in compression of the medulla oblongata.
Cerebral arteriovenous malformations can originate and develop in any part of the brain, both on its surface and in deep areas. In addition, the onset of pathology can occur between the pulmonary trunk and the aorta.
Spinal cord AVM
This disease most often originates in the lower parts of the spine. In the initial stages it is asymptomatic, but after a while it can result in severe loss of sensation in the back area. Can lead to hemorrhage in the spinal cord.
The pulmonary trunk is one of the largest blood vessels in humans, starting from the right ventricle, and the aorta is a large unpaired arterial vessel of the systemic circulation.
The embryo must have connections between the heart and blood vessels - the arterial flow. After birth, it begins to overgrow, and if this does not happen, then the unovergrown arterial flow is considered a congenital heart defect.
The disease, which originates and develops in this part of the body, provokes the most painful manifestations and complications.
Therapy consists of complete resection or complete surgical obliteration of the vascular defect. There are 3 types of high-tech operations that are used for these purposes: endovascular treatment, stereotactic radiosurgery, microsurgical intervention.
- Endovascular surgery. The method is suitable for the treatment of deeply located and large formations. The intervention is performed under X-ray control, anesthesia is provided by general anesthesia. This minimally invasive tactic is often the initial stage of treatment before the upcoming open surgery.
- A thin catheter tube is brought to the pathological part of the brain through the femoral artery through the vessels.
- Through an installed guide, a special adhesive biomaterial, similar to polyurethane foam, is supplied to the area of the malformation.
- The neurosurgeon uses a foam composition to cover the affected areas, that is, thromboses the abnormally developed vessels while maintaining healthy ones.
- Embolization allows you to “turn off” the pathological plexus from the general cerebral circulatory system.
- After the operation, the patient is usually under inpatient observation for 1-5 days.
- Stereotactic radiosurgery. The therapeutic tactics, although related to angioneurosurgery, are not traumatic. This means that there will be no incisions or insertion of intravascular probes at all. Suitable for the treatment of small vascular defects (up to 3.5 cm) or in cases where the lesion is located in an inoperable section of the brain.
- Radiosurgery involves the destruction of angiomas using systems such as CyberKnife or Gamma Knife.
- The devices operate on the principle of targeted exposure to radiation to an anomaly.
- The rays are emitted from different directions and converge at one point only in the defective zone; healthy structures are not affected. As a result, the AVM vessels grow together and the focus is suppressed.
- Cyber or Gamma Knife procedures are absolutely painless, and the patient remains conscious during treatment. The devices, on the couch of which you just need to lie motionless (from 30 minutes to 1.5 hours), resemble traditional tomographs.
- When treating with a Gamma Knife, a special helmet is put on the head and firmly fixed. To ensure that the patient receiving the helmet does not experience any discomfort, superficial local anesthesia is given to individual areas of the head. CyberKnife surgery does not require anesthesia or placing the head in a rigid structure.
- There is no need for hospitalization. But it may be necessary to undergo more than one radiosurgery session in order to finally eliminate the residual effects of AVM of the brain. Sometimes the obliteration process lasts 2-4 years.
- Direct microsurgical removal. Microsurgery for this diagnosis is the only method that gives the highest chance of radical cure of the pathology, minimizing the risk of relapse. It is the “gold standard” in the treatment of this disease with superficial localization and compact forms of the node.
- A microsurgical operation is not complete without a typical craniotomy; an economical opening of the skull is necessarily performed to carry out basic surgical manipulations on the brain.
- The intervention takes place under general endotracheal anesthesia, under the control of a high-power intraoperative microscope and ultrasound equipment.
- To prevent blood discharge through the supplying arterial vessel and vein, the bipolar coagulation method is used, that is, cauterization is performed.
- Next, in a single block through the trepanation window, a single-stage excision of the entire body of the malformation is performed with minimal blood loss.
- At the end of the surgical session, the hole in the skull is closed with a bone flap, and a suture is placed on the skin.
- Discharge is possible approximately 14 days after surgery. Next, you need to continue postoperative recovery in a specialized rehabilitation center. The duration of rehabilitation is determined individually.
There are several classifications of hereditary angiodysplasias, all of which are used in clinical practice as complementary to each other and allowing the development of an individual treatment plan.
Angiographic classification of arteriovenous malformations. Type 1 (arteriovenous fistula): bypass (letter W in the picture) of usually three separate arteries (letter A in the picture) and a single draining vein (letter B in the picture). Type 2 (arteriolovenous fistula): bypass (Sh) of multiple arterioles (A) and draining vein (B). Type 3 (arteriolovenous fistula): multiple shunts (III) between arterioles (A) and venules (B).
Evaluates the leading type of vascular disorders:
- Arterial.
- Venous.
- Shunt arteriovenous.
- Lymphatic.
- Microvascular (capillary).
- Combined.
Includes subclassification based on the type of connecting vessels and depth of location:
- stem and non-stem forms (single or scattered type of vascular connections);
- limited and diffuse forms (according to the type of tissue damage);
- deep and superficial forms.
| Type of angiodysplasia | Blood flow speed | Type of malformation according to the type of vessels involved |
| Vascular malformations | Fast | Arterial |
Arteriovenous fistula (fistula)
Combined
Reflects the stages of pathology development and is used to select optimal treatment.
| Slow | Capillary | |
| Vascular tumors | Different types of hemangiomas | |
| Stage | Clinical manifestations | |
| The first is peace | Redness and increased skin temperature over the formation | |
During ultrasound examination of blood vessels, there is a discharge of blood from the arterial into the venous bed
Vascular malformation looks like a benign vascular tumor
Vessels are increased in diameter
Veins are dilated and tortuous
Increased pulsation of the arteries is detected
Tissue malnutrition with ulceration and bleeding
Destruction of bone structures (if localized in bones)
Cardiovascular failure with left ventricular enlargement
Diagnostics begins with:
- careful determination of neurological status;
- blood pressure measurements;
- assessing the condition of the skin and gait;
- patient complaints;
- survey regarding the course of pregnancy.
Persons with this pathology are advised to:
- Doppler ultrasound. Allows you to evaluate the structure of veins and arteries, blood circulation in them;
- radiographic angiography. To visualize the vessels, a contrast agent is injected, which “illuminates” them;
- computed angiography. With its help, you can recreate a 3D picture of human blood vessels;
- magnetic resonance angiography. A high-precision method for determining arteriovenous malformation allows you to evaluate the shape, structure, and blood circulation in damaged vessels;
- ultrasound examination of the heart. For the diagnosis of patent ductus arteriosus. You can also evaluate the ejection fraction; if it is more than 70%, then this indirectly allows us to judge the presence of malformation.
It is a very dangerous and insidious disease, since its complications are always sudden and with a high probability can cause death or disability of a person. There are:
- intracerebral, intraventricular and subarachnoid (in the cavity between the arachnoid and soft membrane) hemorrhages. Occurs in 55 - 65% of cases. Symptoms are similar to those of a stroke: numbness of the limbs, difficulty speaking, impaired vision and coordination, sudden onset of severe headache;
- epileptic seizures in about 25 - 40% of cases;
- disruption of adequate blood supply to the brain leads to the death of a significant part of the neurons and, as a consequence, this leads to significant impairments in speech, intellectual abilities, and in some cases to paresis or paralysis of various parts of the body.
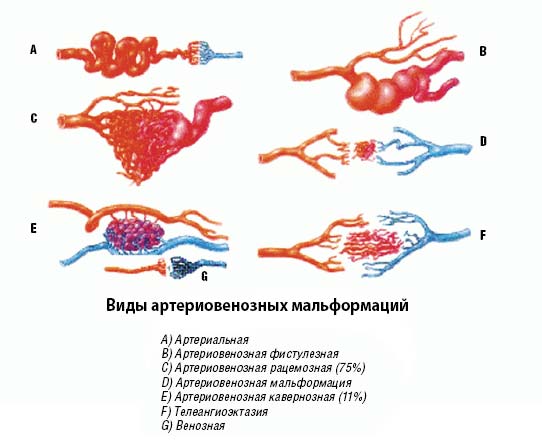
Classification and types of vascular malformation
Vascular malformation located in the brain can consist only of veins, arteries, or be a combination.
The last option, arteriovenous, is the most common. Based on the type of structure, cerebral AVMs are divided into:
- Racemose (account for ¾ of the total) - a branched vascular conglomerate.
- Fistulous - is a massive shunt between large vessels.
- Cavernous - a cluster of thin-walled cavities that externally resemble mulberries (diagnosed in 11% of AVM cases).
- Micromalformation is a small-sized formation.
Among the isolated ones, venous malformation, arterial, and telangiectasia are distinguished. Anomalies are also distinguished by size. The diameter of small ones does not exceed 30 mm, medium ones - 60 mm, and large ones are tangles larger than 6 cm. The localization of the defect is important for diagnosis and treatment: in mild cases they are located outside functionally significant areas, which include the brain stem, temporal and occipital lobes , thalamus, sensorimotor cortex, speech area, Broca's area. The nature of drainage is also important, that is, the presence of access to large veins.
The listed classification parameters are important for determining the risk in the event of surgery. Each of them (location, type of drainage, size) is assessed on a three-point scale, and depending on the amount of points scored, the operational risk is determined. Low is 1, and five means increased technical complexity of the intervention, a high probability of disability or death.
There are several classifications of hereditary angiodysplasias, all of which are used in clinical practice as complementary to each other and allowing the development of an individual treatment plan.
Angiographic classification of arteriovenous malformations. Type 1 (arteriovenous fistula): bypass (letter W in the picture) of usually three separate arteries (letter A in the picture) and a single draining vein (letter B in the picture). Type 2 (arteriolovenous fistula): bypass (Sh) of multiple arterioles (A) and draining vein (B). Type 3 (arteriolovenous fistula): multiple shunts (III) between arterioles (A) and venules (B).
Evaluates the leading type of vascular disorders:
- Arterial.
- Venous.
- Shunt arteriovenous.
- Lymphatic.
- Microvascular (capillary).
- Combined.
Includes subclassification based on the type of connecting vessels and depth of location:
- stem and non-stem forms (single or scattered type of vascular connections);
- limited and diffuse forms (according to the type of tissue damage);
- deep and superficial forms.
| Type of angiodysplasia | Blood flow speed | Type of malformation according to the type of vessels involved |
| Vascular malformations | Fast | Arterial |
Arteriovenous fistula (fistula)
Combined
Reflects the stages of pathology development and is used to select optimal treatment.
| Slow | Capillary | |
| Vascular tumors | Different types of hemangiomas | |
| Stage | Clinical manifestations | |
| The first is peace | Redness and increased skin temperature over the formation | |
During ultrasound examination of blood vessels, there is a discharge of blood from the arterial into the venous bed
Vascular malformation looks like a benign vascular tumor
Vessels are increased in diameter
Veins are dilated and tortuous
Increased pulsation of the arteries is detected
Tissue malnutrition with ulceration and bleeding
Destruction of bone structures (if localized in bones)
Cardiovascular failure with left ventricular enlargement
AVM with damage to cerebral vessels can be of the following types:
- Arteriovenous. The bundle is located between the feeding arteries and draining veins.
- Arterial. The conglomerate is represented exclusively by arteries.
- Venous malformation involving cerebral vessels. This pathology is characterized by a cluster of altered veins. Such isolated bundles are rare.
Depending on the size of the anomaly, it can be:
- Small – up to 3 cm.
- Average - no more than 6 cm.
- Large – more than 6 cm.
Most often, patients are diagnosed with racinous AVM. It occurs in 75% of cases. Less commonly, doctors detect fistulous and micromalformations.
Causes and mechanism of development of pathology
Pathology is divided depending on which vessels are affected:
- When the veins are connected abnormally, a venous malformation of the cerebral vessels is formed.
- If the problem lies in the arteries that directly turn into veins, then this is a cerebral arteriovenous malformation (AVM), which is most often found.
In AVM pathology, thin vessels connecting veins to arteries twist and pass into each other, forming a vascular weave. This plexus does not have a protective wall consisting of capillaries, so blood flow noticeably accelerates in the pathological area. As a result, the arterial walls hypertrophy and expand, and arterial blood enters the veins.
The weaves take blood and nutrients for themselves, robbing neurons. As a result of forced fasting, the functions of brain cells and metabolic processes are disrupted. The resulting malformations are quite vulnerable, since their vessels are under constant tension, which is dangerous due to their sudden rupture and hemorrhage.
Arteriovenous changes are:
- Racemonic.
- Fistulous.
- Cavernous.
As mentioned above, doctors call the reasons for the development of a pathological process in brain tissue:
- genetic mutations,
- infectious diseases suffered by the mother during pregnancy,
- bad habits (alcohol, drugs, uncontrolled use of medications during pregnancy),
- fetal injuries during pregnancy.
It is these factors that can lead to improper development of the capillary system, modification of vascular walls, and deformation of blood vessels.
Despite their rarity, vascular malformations can be very severe, significantly affecting the quality of life, so work to identify the causes is still underway.
Main causative factors:
- Genetic. Associated with the appearance of pathological changes in a number of genes, often of a hereditary nature. The most famous of these malformations is Osler syndrome (multiple “spider veins” on the skin and mucous membranes).
- Random. Vascular malformations that are not included in known syndromes are often isolated in nature.
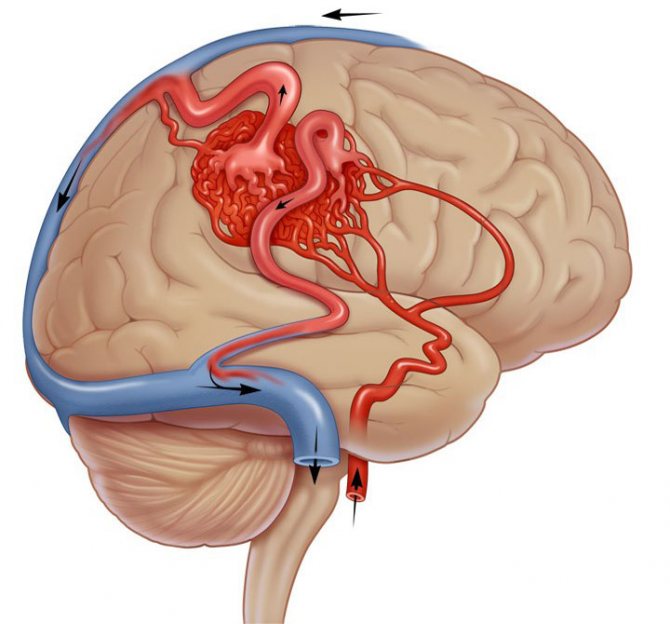
Regardless of the cause, the mechanism for the development of malformations is the same: during the intrauterine formation of the blood supply system, additional connections between the vessels develop with the formation of zones of pathological discharge of blood (“central zone”). Depending on the timing of the onset of the pathology, connections can be scattered (non-stem) in nature, if the defect arose in the first weeks after conception, or stem - this is the development of the defect at the end of the first - beginning of the second trimester.
The ability of angiodysplasia to increase over time or recur after treatment is associated with the preservation by the cells of the pathological vessel of the growth function characteristic of embryonic cells.
Arteriovenous malformation in general is not a very common congenital disease. Its reasons still remain unclear. Experts are inclined to believe that trauma to the mother during pregnancy and the presence of malformations in the embryo can affect the formation of blood vessels. The likelihood of the disease increases in men and in the presence of a hereditary predisposition.
By the way, some related pathologies may have the same reasons, for example, empty sella syndrome of the brain.
Some types of malformations are inherited, for example, hemorrhagic angiomatosis. But there are also isolated accidental violations. The tendency of malformations to grow and recur after treatment is due to the fact that the lesion consists of cells that have not lost their ability to grow.
Treatment
Arteriovenous malformations of the brain, if they rupture or if there is a danger of such a complication, must be removed. Preferably planned surgical treatment of AVM.
In case of rupture, it is carried out after the elimination of the acute period of hemorrhage and resorption of the hematoma. In the acute period, according to indications, surgical removal of the resulting hematoma is possible.
Simultaneous elimination of both hematoma and AVM is carried out only when the vascular malformation is located lobarly and has a small diameter. In case of hemorrhage into the ventricles, external ventricular drainage is primarily indicated.
Classic surgical removal of an AVM is performed by craniotomy. Coagulation of the afferent vessels, isolation of the AVM, ligation of the vessels extending from the malformation and excision of the AVM are performed. Such radical transcranial removal of an AVM is feasible when its volume is no more than 100 ml and is located outside functionally significant areas. For large AVMs, combined treatment is often used.
When transcranial removal of an AVM is difficult due to its location in functionally significant areas of the brain and deep structures, radiosurgical removal of the AVM is performed. However, this method is effective only for malformations no larger than 3 cm.
If the size of the AVM does not exceed 1 cm, then its complete obliteration occurs in 90% of cases, and for sizes over 3 cm - in 30%. The disadvantage of this method is the long period (from 1 to 3 years) required for complete obliteration of the AVM.
In some cases, gradual irradiation of the malformation over a number of years is required.
Methods for eliminating cerebral AVMs also include X-ray endovascular embolization of the arteries leading to AVMs. Its implementation is possible when there are afferent vessels available for catheterization. Embolization is carried out in stages, and its volume depends on the vascular structure of the AVM. Complete embolization can be achieved only in 30% of patients. Subtotal embolization occurs in another 30%. In other cases, embolization is only partially successful.
Combined staged treatment of AVM consists of the staged use of several of the methods listed above. For example, if the AVM is incompletely embolized, the next step is transcranial excision of its remaining part. In cases where complete removal of the AVM is not possible, radiosurgical treatment is additionally used. This multimodal approach to the treatment of cerebral vascular malformations has proven to be the most effective and justified for large AVMs.
Can vascular malformation be corrected? Treatment methods depend on the type of anomaly, its location, the size of the lesion, and a history of strokes.
There are three main methods of therapy:
- open surgery; - minimally invasive embolization; - non-invasive radiosurgical treatment.
For each of them there are indications, contraindications and a list of possible complications.
The most traumatic is open surgery. In order to get to the source, the skull is opened, the vessels are clipped and crossed. This option is possible if the malformation is located on the surface of the brain and is small in size. Attempts to reach a deep-lying source can result in damage to vital centers and death.
What can be done if the patient has a deep malformation. Treatment consists of endovascular embolization.
This is a fairly gentle procedure, during which a thin catheter is inserted into a large vessel feeding the abnormal conglomerate and, under X-ray control, the doctor gets to the malformation. Then a hypoallergenic drug is injected into the lumen of the vessels, which fills all the available space and blocks the blood flow in this area.
Unfortunately, this technique does not provide an absolute guarantee that the vessel is completely obliterated. Therefore, it is most often used as an additional treatment.
The most advanced method of treating vascular malformations is considered to be operations using a cyber knife (radiosurgery). The essence of the method is to treat the anomalous focus from different points with narrow radioactive beams.
This allows you to quickly destroy altered blood vessels without damaging healthy tissue. The process of vascular sclerosis takes on average several months.
The advantage is the complete absence of complications from the nervous system. But there are limitations to the use of this method.
1. The total diameter of the vessels should not exceed three centimeters.2. There should be no history of strokes or other hemorrhages. Since the thin wall may not withstand and rupture in the interval between the procedure and the final sclerosis of the malformation.
Treatment tactics are influenced by the following parameters:
- size of the lesion;
- type of disease;
- its localization;
- the presence of previous hemorrhages.
Surgical methods are used as treatment, both open interventions and minimally invasive operations, for example, radiosurgery or endovascular embolization. Each of these methods requires preparation and careful preliminary research.
Open surgery involves opening the skull and completely removing the source of pathology. This method is justified when the vascular malformation is located close to the surface and is easy to remove without risking damage to the brain, and also when its size is small.
If the pathology is located deep, this treatment method is contraindicated, since serious damage to vital brain structures can be caused.
Endovascular embolization is a minimally invasive procedure. A thin catheter is inserted under radiographic guidance.
A special drug is injected through a catheter, which clogs the vascular lumen in the area of the malformation. This method is considered one of the modern and innovative.
It is used when surgery is not recommended, most often when the pathology is deep in the brain tissue. There is no absolute guarantee of complete blockage of the vessel with this method, and therefore it is used as an auxiliary method after surgery or radiosurgery.
Radiosurgery is a modern method based on the use of radiation. It is successfully used to treat many brain diseases without compromising the integrity of the skull and possible complications in connection with this.
This treatment method uses thin beams of radiation that impact the pathological focus from different angles. This is the difference between this method and conventional radiotherapy.
Under this influence, healthy tissues remain practically unaffected, and the source of pathology is destroyed. All radiation beams emitted by the device converge at one point.
As a result of radiosurgical treatment, gradual occlusion of the vessels that form the malformation occurs. This process takes up to several months.
A popular technique called cyberknife is also a radiosurgical technique. The method is non-invasive, there are no contraindications to its use, and anesthesia is not required.
The disadvantage is that while complete embolization of the necessary vessels occurs, a hemorrhage in the brain may occur. After repeated application of the cyberknife method, the effectiveness of radiosurgery increases and the probability of complete embolization increases to 95%.
Treatment of such formations must be carried out in the early stages - in this case, the malformation is small in size, there are no dangerous bleeding and other associated symptoms. You need to understand that conservative treatment is inappropriate - it is carried out only in case of contraindications to surgical intervention.
Surgical treatment of malformations consists of their exclusion from the general bloodstream - this is carried out using endovascular embolization. It is also possible to completely remove them.
Endovascular embolization is considered a minimally invasive procedure and therefore has a minimal risk of complications. Before the procedure, angiography is performed to determine the exact location of the formation, after which the doctor begins embolization.
During this procedure, the surgeon has access to the surgical site through the vascular bed. The skull is not opened. In this situation, the surgeon uses a special technique that makes it possible to visualize the patient’s vascular network and perform an operation through the lumen of the vascular bed. This is done using a radiosurgical angiography system.
The embolization procedure begins with the introduction of a special catheter into the femoral artery, then it is passed through the artery into the brain vessels directly to the body of the malformation. After this, a thin platinum thread is inserted into the formation, which blocks the blood flow.
Malformation of cerebral vessels is a rather dangerous pathology that requires timely diagnosis and adequate treatment. Thanks to correctly performed procedures, a person can quickly return to normal life and avoid serious complications.
The choice of treatment method should be made by an experienced specialist. Treatment tactics depend on the location of the malformation, its size, the intensity of its symptoms, and the individual characteristics of the patient. If vascular anomalies are detected and do not manifest themselves in any way, then they do not require any treatment. Such individuals only need to periodically consult a doctor and monitor the condition of the malformations.
But if the patient has clinical signs of vascular malformation, then it is necessary to begin treatment of the disease.
It should be noted that conservative treatment does not produce any significant results, and is carried out only if surgery is contraindicated. Treatment of cerebral aneurysm in the early stages is more effective, since in this case the pathological area is small and easier to manipulate by the doctor.
Treatment of head vessels is carried out in three ways:
- Microsurgical removal.
- Stereotactic radiosurgery.
- Embolization.
Stereotactic radiosurgery is used only in cases where the size of the malformation is a maximum of 3.5 cm. Using microsurgical treatment, the affected area can be removed; more often, a combination of various methods and surgical intervention by vascular embolization are used.
During surgery, arteriovenous malformations of the brain are excluded from the general blood flow using endovascular embolization; it is a minimally invasive method of intervention, which reduces the risk of complications. Embolization is carried out only after identifying the location of the arteriovenous aneurysm using angiography.
The decision about which treatment tactics will be used in a particular case should be made only by an experienced surgeon after a detailed diagnosis. In most cases, surgical treatment is performed, but if the risk of spontaneous rupture is minimal, the tactic may be wait-and-see. Currently, three types of interventions are used for arteriovenous malformations of the brain, as well as various combinations of them:
- surgical (classical operations);
- radiosurgical;
- embolization (endovascular operations).
Endovascular embolization, or vascular fusion, is now the most commonly used method to prevent hemorrhage due to AVM. Radical exclusion of the malformation from the general bloodstream can be carried out in approximately 50% of patients, but in the rest, complete exclusion does not occur. Using a catheter, a special adhesive is applied to the AVM, which stops blood flow in this area (uncontrolled embolization). There are other types of endovascular operations:
- stationary balloon occlusion of the feeding arteries;
- combining balloon occlusion with vascular embolization;
- selective embolization or thrombosis of AVM.
Radiosurgical techniques can completely cure about 85% of patients whose malformation does not exceed 3 cm in diameter.
Radiosurgery is indicated when the location of the formation is inaccessible for classical surgery, as well as for residual malformations after surgery. Focused radiation is directed to the area where the anomaly is located, after which the procedure itself lasts approximately 1 hour. Then, over the course of 1-2 years, the vessels themselves sclerose and are replaced by connective tissue. The main disadvantage is the continued risk of hemorrhage until the vessels become hardened.
Surgical treatment is carried out if there is access to the location of the AVM and its volume is up to 100 ml. After craniotomy - opening the cranial cavity - the malformation is identified, then a laser or other instruments are used to completely cauterize it. After compression, the malformation is removed from the tissue. The operation, despite complete recovery if successful, may be complicated by stroke and other serious consequences. After the operation, a short course of rehabilitation of the patient is carried out. Typically, hospital stay does not exceed 5-7 days. In the future, the person is recommended to take nootropics and other vascular drugs, as well as undergo regular examinations (MRI) of the brain.
Cerebral vascular malformation is rarely treated with conventional therapy. Pathologies such as aneurysm of the vessels of the head require surgical treatment. The scale of such intervention and the method are determined based on four components:
- location;
- type of pathology;
- dimensions;
- the number of hemorrhages already suffered.
If open intervention is required, the skull is opened and standard excision of the lesion is performed. This method is acceptable if the aneurysm is on the surface and its removal will not affect brain tissue. Usually the malformations are small, excised and progress stops. However, with large aneurysms this is unacceptable due to the significant risk of damaging the structure and integrity of the brain.
For deep localization, another method is used - microsurgical removal. The operation is innovative and is carried out under the control of a monitor and equipment. A catheter with a substance is inserted through the hole, which should block the lumen of the vessels in the tangle itself. More often, this operation is used as an auxiliary to radiosurgery.
The most optimal method for treating malformations is radiosurgery. A method that does not require incisions and is safe for the body as a whole. Its essence is to direct a beam at the affected area from different angles. In this case, the underlying tissue is practically not affected and is not exposed to radiation.
Cavernous angioma or tumor?
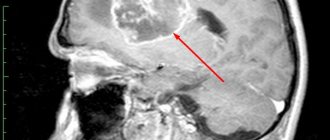
Brain scanning using CT and MRI in most cases allows one to clearly distinguish a cavernoma from other brain formations, including tumors of varying degrees of malignancy. However, in some cases, differentiation of these formations represents a diagnostic problem, the solution of which requires extensive experience.
In this regard, the ability to attract a highly qualified diagnostician is critical. In addition, high-quality interpretation of CT and MRI images provides a solution to other diagnostic problems: exclusion of surrounding cerebral edema, identification of the severity of hemorrhage, description of details affecting the operability of the cavernoma.
When using visualization methods, it is useful to separate the cavity into 3 components. These include (1) a peripheral pseudocapsule, consisting of glial tissue impregnated with hemosiderin, (2) an irregularly structured intermediate connective tissue separating the cavities, and (3) a central vascular part, consisting of vascular cavities with slow blood flow.
On CT images without contrast enhancement, a cavernoma appears as a focal formation of an oval or nodular shape, characterized by slightly or moderately increased X-ray density and does not have a volumetric effect on the surrounding parenchyma. Areas of calcification and hemosiderin deposition in the walls of fibrous septa, along with stagnation of blood in the cavities, contribute to increased x-ray density on non-contrast-enhanced images.
Contrast enhancement can be minimal or maximal, although 70-94% of cavernous malformations are weakly or moderately enhanced after intravenous contrast. In most cases, good contrast is the result of increased blood flow in the vascular component of the mass.
Mass effect is not typical for cavernomas, unless they are associated with recent hemorrhage. On CT images without contrast enhancement, cavernomas may not be detected at all. In hemorrhages and the formation of intracerebral hematoma, cavernomas are visualized as areas of focal signal enhancement in the area adjacent to the hematoma.
Any hemorrhage detected on CT in a relatively young patient should be carefully investigated, and cavernous angioma should always be considered as a possible cause. When evaluating a patient with a seizure disorder, cavernous angioma should also be considered as a likely etiological factor, especially if the patient is between 20 and 40 years of age.
Cavernous malformations identified by CT may also include other rare vascular malformations (thrombosis of arteriovenous malformation, capillary telangiectasia), glioma (poorly differentiated astrocytoma or oligodendroglioma), and metastatic melanoma.
D18 is a code according to ICD 10, which means any type of angioma by location and origin.
For successful treatment, it makes sense to distinguish between venous and cavernous angiomas. The first type occurs in the veins, as an expansion of one or more venous vessels. The pressure in the veins is low and the walls are quite strong, so the risk of rupture is low.
The cavernous type includes in its structure not only blood vessels, but also small cavities of the brain. The tumor completely fills the caverns, and its boundaries are thin membranes. With this type of disease, there remains a high risk of hemorrhagic stroke with profuse hemorrhage.
For treatment, the location of the tumor, the type of benign or malignant, and the activity of changes in size (constantly growing or has clear, unchanged boundaries) are important.
Clinical picture (symptoms)
The nature of the symptoms of malformation depends on:
- its size
- localization
- presence or absence of a gap
Large AVMs compress the chiasma (the intersection of the optic nerve fibers) and lead to visual impairment. It manifests itself as loss of visual fields, up to complete blindness.
The location of the vascular tangle near the cranial nerves (CN) or their nuclei is manifested by a disorder of the movement of the eyeballs (oculomotor disorders).
Migraine associated with this vascular anomaly is another clinical manifestation. In addition to headaches, it is manifested by transient and relatively persistent neurological disorders:
- decreased muscle strength (see hemiparesis)
- paresis of the external eye muscles (manifested by strabismus)
- impaired coordination of movements (including unsteady gait, nystagmus, changes in handwriting)
- mental disorders (psycho-emotional and behavioral areas suffer)
AVMs are characterized by repeated intracranial hemorrhage (ICH), epileptiform seizures and focal neurological disorders.
Intracranial hemorrhages occur among young people (usually under forty years of age) and lead to the formation of intracranial hematomas, which can compress the structures of the brain from the outside and lead to death.
A rupture of an AVM can manifest itself as multiple hemorrhages in the retina or large-focal hemorrhages in the vitreous body (the presence of Terson syndrome).
Rupture of the vessel wall and effusion of blood into the cranial cavity is manifested by meningeal signs (stiff neck, upper, middle and lower Brudzinski's symptoms, etc.).
Rarely, malformations are the cause of ischemic stroke (brain infarction). If this happens, it is manifested by neurological disorders, the nature of which depends on the location of the lesion.
Causes of pathology
This pathology is congenital, and the reliable and exact causes remain unknown to modern medicine. The main assumption is that trauma and intrauterine malformations of the fetus have a negative impact on the formation and structure of blood vessels.
Medical specialists were able to identify risk groups:
- male gender, since the vast majority of the disease affects men;
- genetic mutations;
- infectious diseases that the mother suffered during pregnancy;
- bad habits that a woman suffers from during pregnancy, such as smoking, excessive consumption of alcohol and medications;
- fetal injuries.
These are the main factors influencing the possibility of developing pathology.
Vascular anomalies of the brain are uncommon. There are 19 cases of pathology per 100 thousand people. The cause of its occurrence still remains unknown. It is assumed that injuries and intrauterine malformations of the fetus have a negative effect on the structure of blood vessels.
Experts identify two main risk groups:
- Male gender (the disease occurs more often in men).
- Genetic mutations.
This problem remains completely unexplored, so a variety of hypotheses about the nature of its occurrence appear. Some experts talk about the negative factors that the expectant mother was exposed to during pregnancy (alcohol, drugs, smoking, taking illegal drugs, chronic diseases).
Symptoms that should alert you
The size of the malformation can vary from small to large. The largest lesions can cause large hemorrhages and epileptic seizures in humans. If the lesions are small, then the symptoms do not manifest themselves and do not make themselves felt for a long time.
The most common symptoms of this disease:
- frequent attacks of headache;
- partial or complete loss of vision;
- loss of sensation in the limbs;
- muscle weakness;
- frequent convulsions, possible loss of consciousness;
- speech problems;
- lethargy, general malaise, inability to work.
Doctors distinguish the following groups of the disease according to the clinical picture:
- The torpid nature of the course is characterized by headaches, frequent dizziness, and nausea. Since such manifestations also apply to many other diseases, it is impossible to determine problems with the blood vessels of the brain from them. The affected area is located in the cortical areas of the brain.
- Hemorrhagic character is inherent in 75% of patients suffering from this pathology. The hemorrhage may be small, and in this case there will be no significant symptoms. However, if the hemorrhage turns out to be massive, then vital brain centers will be at great risk of disruption. Symptoms may include the following: impaired speech and coordination, impaired hearing and vision. The worst option is death.
- Neurological character occurs with spinal cord injuries. The vessels, expanding, compress the nerve roots and endings. The result is pain in the back and lumbar region, as well as numbness of all extremities and decreased sensitivity of the skin.
It is difficult to identify such a disease in young children, because at an early age it is practically asymptomatic, but there are some signs that may indicate the development of malformation in a child:
- speech defects, decline in intelligence, unstable gait, frequent convulsions;
- loss of coordination, shifty eyes, decreased muscle tone;
- partial visual impairment.
Symptoms of arteriovenous malformation may be practically invisible for a long time. That is why many people who have such damage to the vascular system find out about it by chance when they are scheduled for a brain examination. This is where the insidiousness of the disease lies: the anomaly gradually develops, can greatly increase in size, after which characteristic symptoms begin to appear. These include:
- frequent depression,
- apathy,
- constant lethargy,
- attacks of headaches,
- the occurrence of dizziness,
- visual impairment,
- disturbances in motor coordination and fine motor skills,
- increased intracranial pressure accompanied by throbbing pain,
- convulsive states,
- the appearance of visual, olfactory and auditory hallucinations.
With a congenital anomaly, such symptoms can appear from about ten years of age, when the child’s body begins to grow rapidly.
Possible complications
Even before the malformation manifests itself clinically, the person will latently develop irreversible pathomorphological phenomena. This occurs due to hypoxia of a section of brain tissue, its degeneration and death. Depending on the location of the affected area, characteristic focal symptoms are observed (impaired speech, gait, voluntary movements, intelligence, etc.), and there may be epileptic seizures.
Severe complications begin already in adulthood. Abnormal vessels have thin walls and are more susceptible to rupture, so ischemic strokes are more common in patients with malformations.
Large conglomerates of arteries and veins compress the tissue around them, causing hydrocephalus. The most dangerous is hemorrhage resulting from the rupture of several vessels at once.
This can either have fatal consequences or end with virtually no consequences. It all depends on the amount of blood shed.
Hemorrhagic stroke has a much poorer prognosis and may recur over time.
Ignoring the symptoms of vascular malformation increases the likelihood of developing complications of the disease. Abnormal vessels can lead to insufficient blood supply to certain areas of the brain, causing hypoxia.
Hypoxia, in turn, leads to degeneration and death of brain tissue. As a result, the clinical picture of ischemic stroke develops.
Compression of surrounding tissues can lead to the development of hydrocephalus of the brain, persistent movement disorders, and severe neurological disorders.
A very serious consequence of malformations is cerebral hemorrhage. Depending on the volume of hemorrhage and its location, the result can vary from headache to death.
Even before the rupture, when a vascular malformation exists, a person experiences insufficient blood supply to a certain area of the brain, that is, its hypoxia. As a result, dystrophy and gradual death of brain tissue occurs.
This phenomenon can provoke ischemic stroke, which is accompanied by loss of vision, memory, paresis and paralysis, speech impairment and other various and severe disorders. Large AVMs put pressure on surrounding tissues so that they cause dropsy (hydrocephalus).
How is diagnostics carried out?
If there is a suspicion of the presence of a formation in the patient’s brain, experts recommend conducting the following examinations to identify the malformation and determine its type:
- Magnetic resonance imaging of blood vessels. When conducting such a study, the specialist will be able to see in the image the pathological changes that have occurred in the vessels and detect the location of the anomaly.
- Duplex scanning. This modern non-invasive ultrasound test helps identify the area of the abnormality, its size and location. The study can be carried out repeatedly due to its complete safety for the human body.
- Computed tomography of the brain. This examination is usually prescribed with the introduction of a contrast agent, which allows you to clearly visualize the source of the disease.
- Cerebral angiography. The examination consists of the following: the patient is injected with a contrast agent, which is distributed through the arteries and veins of the head, after which a picture is taken using an X-ray machine. In the image you can clearly see the entire vascular network and pathological changes in it.
Diagnostics
Due to the frequent absence of characteristic symptoms, the malformation is discovered after a brain test that was ordered for some other reason. Such a study is most often a magnetic resonance imaging of the brain or computed tomography.
Contrast angiography is considered one of the most accurate methods for detecting vascular malformation. This is an x-ray examination, which is based on x-rays of the head with the preliminary administration of intravenous contrast agent.
Nowadays this method is used less and less, since its use is likely to cause complications.
Superselective angiography has become a good replacement for vascular angiography. This method involves injecting a contrast agent directly into the artery through a special catheter into the area of the malformation lesion. But computer and magnetic resonance imaging methods are now considered the most accurate and relatively safe. With their help, you can clearly determine the position of the object, its shape, size, outline and how the lesion interacts with surrounding tissues.
Often, cerebral vascular malformation is not associated with any neurological symptoms. As a rule, these formations can be detected during magnetic resonance or computed tomography of the brain, which are performed to diagnose other pathologies.
Contrast angiography is considered the most accurate method for identifying malformations. This technique belongs to the category of x-ray studies. The person is injected with a contrast agent intravenously, after which an X-ray of the head is taken. It is worth noting that this method is associated with the risk of complications, which is why it is not currently used.
Superselective angiography is used instead. This technique involves injecting a radiopaque contrast agent into the artery through a thin catheter directly into the area of the vascular malformation.
However, in most cases, magnetic resonance and computed tomography are used. These methods are considered relatively safe. In addition, they make it possible to determine the exact location of the pathological focus, its size, shape, and relationship to neighboring tissues.
Diagnosis of vascular anomalies is carried out by a neurologist, who collects the patient’s complaints, examines the patient, assesses the neurological status and prescribes additional examination.
For diagnostics the following are used:
- Arteriography makes it possible to detect abnormal cerebral vessels. Catheterization of the femoral artery is performed, with the help of which a contrast agent is injected into the vessels of the brain. This will show the condition of the brain vessels and the presence of malformations.
- Computed tomography is also used with the introduction of contrast. Subsequently, the radiologist takes a series of images, which shows whether there are vascular malformations or not.
- MRI can be considered the gold standard in the diagnosis of vascular malformations of the brain. It shows the exact location of the malformation, its size and the presence of complications.
- Doppler ultrasound shows the position of the affected vessel and allows for differential diagnosis of this pathology with other vascular diseases.
Arteriovenous malformation is usually detected using CT (computed tomography) or MRI (magnetic resonance imaging), which are also used to diagnose pathologies of neurological symptoms:
- Contrast angiography is the most accurate method for determining arteriovenous malformation (aneurysm) of cerebral vessels. A contrast agent is injected into the patient's vein, then X-rays of the head are taken. A significant disadvantage of this method is the risk of complications, which is why it is rarely used.
- Superselective angiography - the method involves the introduction of a contrast agent using a catheter directly into the area where the arteriovenous malformation is located.
Often, a CT or MRI scan is sufficient; these methods are distinguished by their safety, and they provide comprehensive information to the doctor about the patient’s condition - the exact location of the arteriovenous malformation, shape, size, and condition of adjacent tissues.
How is the disease treated?
When choosing treatment for an anomaly, a specialist must take into account many factors, including:
- Dimensions of the diagnosed pathology.
- Type of education.
- Location of the malformation (deep or close-lying).
- General health of the patient.
- Previous hemorrhages.
In medicine, there are several most common methods of treating pathology, all of them are aimed at completely eliminating the possibility of hemorrhages:
- surgical removal of the formation, the operation is performed on the open brain;
- endovascular intervention, this surgical method is recognized as less traumatic;
- radiosurgery;
- conservative treatment.
Arteriovenous malformation (with a superficial location) of cerebral vessels is most often removed using open intervention, the lesion is completely excised.
The second method is used when the formation is deep, when open intervention is simply impossible. A catheter filled with a drug that can stop the modified vessel is inserted into the brain. Such treatment is usually prescribed in combination with microsurgery or radiosurgery.
Conservative treatment is aimed at monitoring the condition of the anomaly and relieving painful symptoms.
Preventive measures
It is impossible to purposefully prevent the formation of vascular malformations, since they develop in utero. However, if an AVM has been diagnosed but treatment is not currently possible, you must take adequate precautions to prevent rupture of the malformation.
1. Control over the level of blood pressure, stopping attacks of its increase with the help of antihypertensive medications;
2. Elimination of psycho-emotional stress;
3. Refusal of heavy physical activity.
Treatment methods for cerebral vascular malformations
When there is improper fusion in the veins, the malformation is called venous. If changes are observed in the arteries, and the blood from them directly flows into the venous vessels, we are talking about a type of disease such as arteriovenous malformation. It is the latter type of pathology that most often occurs in patients. Due to the expansion of the arteries, the walls of the vessels become thinner, blood begins to flow through the efferent veins, increasing the blood output.
The veins increase in diameter, are overstrained and pulsate. Due to increased blood supply to the pathological area, brain cells do not receive enough oxygen and nutrients, and their functioning is impaired.
By type of morphology
From a morphological point of view, malformation of arteries and veins can be racemose, fistulous, or cavernous. Angiographic classification distinguishes 3 types of malformations:
- arteriovenous fistula: additional pathways connect three separate arteries and one draining vein;
- arteriolovenous fistula: multiple arterioles connected to the draining vein;
- multiple shunts, which represent a large number of connections between arterioles and venules.
Using the Hamburg classification, it is possible to identify which anomalies in which vessels are leading. They can be:
- arterial;
- venous;
- shunting arteriovenous;
- lymphatic;
- capillary;
- combined.
The forms of the disease are also distinguished based on which vessels are connected and how deep they are located. In the stem form, the additional connection is single; in the non-stem form, the incorrectly formed bonds are scattered in nature. Lesions may be limited or diffuse. They can be located deep in the brain tissue or closer to the surface.
According to the ISSVA method
Using the classification followed by the International Society for the Study of Vascular Anomalies (ISSVA), it is possible to describe the speed of blood flow in various angiodysplasias and find out whether they are benign.
If the blood circulation has accelerated, this indicates that an arterial, arteriovenous malformation or arteriovenous fistula is present. In the case of slow blood flow, we are talking about capillary, venous, lymphatic or combined malformation. Vascular tumors are represented by various hemangiomas.
Schobinger's classification describes the stages the disease goes through in its development. This has important diagnostic significance and helps to correctly navigate when choosing therapy. Highlight:
- the first stage (rest), in which hyperemia and hyperthermia are observed in the affected area, ultrasound shows the movement of blood from the arteries directly into the veins, the lesion is similar to a benign vascular tumor;
- the second stage (progression), in which the above-described manifestations are accompanied by an increase in the diameter of the vessels, dilation and curvature of the veins, and increased arterial pulsation;
- the third stage (destruction), during which the list of disorders is replenished with deterioration of blood supply to tissues, erosions, and hemorrhages;
- the last stage (decompensation) with the appearance of signs of cardiovascular failure, enlargement of the left ventricle of the heart.
Classification of brain AVMs
Based on their type, malformations of cerebral vessels are classified into arteriovenous, arterial and venous. Arteriovenous malformations consist of an adductor artery, draining veins and a conglomerate of altered vessels located between them.
There are fistulous AVM, racinous AVM and micromalformation. About 75% of cases are racinous AVMs.
Isolated arterial or venous malformations, in which there is tortuosity of only the arteries or only the veins, respectively, are quite rare.
There are several forms that vascular malformation can take. To systematize them, the American ISSVA classification adopted in 1996 is used. Its fundamental difference from other classifications is the division of all anomalies into tumors and malformations.
- Vascular tumors: - infantile hemangioma (appears in childhood); - congenital hemangioma; - fascicular hemangioma; - spindle-like hemangioendothelioma; - kaposiform hemangioendothelioma; - acquired tumors.
- Malformations: - capillary (telangiectasias, angiokeratomas); - venous (sporadic, glomangiomas, Mafucci syndrome); — lymphatic; - arterial; - arteriovenous; - combined.
Manifestation of the disease in a child
Abnormal development of the cerebral vascular system mainly occurs during the embryonic development of the fetus. If the pathology was not detected during pregnancy, it may not manifest itself for a long time. During the period of rapid development of the child’s body (puberty), specific manifestations of the disease are possible: causeless headaches, migraine attacks, convulsions. In severe cases, the child may have an epileptic seizure.
But sometimes the disease makes itself felt already in the first days of the baby’s life. A large area of deformed blood vessels in an infant can lead to congestive heart failure, which in turn leads to difficulty breathing. Congenital malformations are more likely to lead to hemorrhage than acquired anomalies.
How to live with this disease
If a patient is diagnosed with abnormal development of cerebral vessels, the following rules should be followed to avoid complications:
- eliminate stressful situations,
- do not lift heavy objects, reduce physical activity as much as possible,
- monitor blood pressure readings,
- create a menu in such a way that the products contain as much sodium as possible,
- do not drink alcohol, give up cigarettes,
- Visit your doctor regularly to monitor the development of the malformation.