It's no secret that alcohol abuse negatively affects the entire body, but brain and liver cells are especially sensitive to it. What happens to neurons, how they react to toxic alcohol damage, what diseases this can lead to, as well as what alcoholic encephalopathy is and how to deal with it, readers can learn from psychiatrist-narcologist, chief physician of multidisciplinary medical Vladislav Sipovich.
Acute forms of alcoholic encephalopathy
Modern medicine identifies only one acute form of alcoholic encephalopathy, which is called Gaye-Wernicke syndrome.
It manifests itself primarily as a significant deterioration in health. The time frame can be very different - for some this period can last months, for others - several weeks. The patient experiences an increase in the number of various disorders, ranging from nervous and somatic to mental. There is also an exacerbation of other diseases that are often present in people suffering from alcoholism (exacerbation of hepatitis, pancreatitis, gastritis and other diseases).
Symptoms that occur against the background of acute alcoholic encephalopathy:
- Severe weakness, shortness of breath and arrhythmia at the slightest exertion;
- Frequent headaches, as well as pain in the limbs and heart;
- Neurological changes intensify. Trembling in the limbs begins to appear more and more, movements become constrained, coordination is impaired;
- There may be a burning sensation in the chest, tightness, the patient’s limbs seem “alien” and very cold;
- Mental changes. The patient develops feelings of fear, panic, and frequent anxiety attacks;
- Sleep disturbances: the patient is accompanied by nightmares, unstable, intermittent sleep;
- Violation of muscle tone;
- Body temperature is most often elevated, increased sweating and peeling of the skin, bedsores may form;
- Voice contact is not possible;
- Stunning of consciousness, which, as it worsens, turns first into stupor and then into coma.
One of the main features of Gaye-Wernicke syndrome is the patient's lack of relief or pleasure from drinking alcohol.
Prevention
The best treatment for alcoholic encephalopathy is prevention. The most common preventive recommendations include:
- complete cessation of drinking alcohol and drinks containing it;
- maintaining proper nutrition that will replenish missing microelements and vitamins;
- sleep and wakefulness patterns;
- tracking blood sugar levels with insulin;
- monitoring blood pressure and, if necessary, taking medications to lower it;
- add physical exercises to your daily schedule, including walks in the fresh air and swimming.
What it is
Alcohol has a toxic effect on nerve cells, which leads to disruption of their functioning and death.
Before we begin to describe alcoholic encephalopathy, it is necessary to explain a number of syndromes that occur with the abuse of alcohol-containing substances.
Alcoholic brain disease is a pathological process in the brain, which manifests itself in a variety of psychopathological and neurological symptoms due to alcohol abuse.
Alcoholic brain disease is most often diagnosed in the form of withdrawal syndrome, alcoholic psychosis, alcoholic encephalopathy and dementia, and seizures. Some of these conditions are subject to treatment by a narcologist and/or a psychiatrist. In his practice, a neurologist often has to deal with encephalopathies and convulsive syndrome.
Alcoholic encephalopathy is a syndrome of damage to the brain substance, which develops as a result of oxygen starvation and impaired blood supply to nerve cells due to alcohol intake.
Brain damage from alcohol abuse occurs as a result of the toxic effect of alcohol on nerve cells and/or as a result of the harmful effects of substances that are formed during alcoholic liver damage.
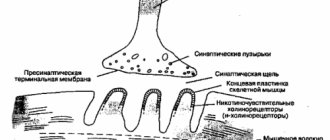
Ethanol in the body breaks down into a toxic metabolite - acetaldehyde, which freely penetrates the blood-brain barrier and affects all structures of the central nervous system. Liver damage leads to the accumulation of toxic waste products, which also affect the nervous system. At the same time, with alcoholism, a deficiency of B vitamins develops, leading to disruption of the conduction of excitation along the nerve fiber.
According to Shumsky’s classification, alcoholic encephalopathy occurs in the following nosological variants:
- Acute alcoholic Wernicke's encephalopathy.
- Korsakov psychosis.
- Mitigated encephalopathy.
- Fulminant encephalopathy.
- Alcoholic pseudoparalysis.
- Rare forms of alcoholic encephalopathy (alcoholic pellagra, alcoholic amblyopia, central pontine myelinosis, alcoholic cerebellar atrophy, etc.).
Diagnostics
Taking into account that alcoholic encephalopathy of the brain is quite fleeting, and the risk of complications in the form of heart failure and cerebral edema increases, doctors need to immediately carry out the diagnostic process and prescribe treatment.
A patient with suspected alcoholic encephalopathy is prescribed:
- electroencephalography (EEG);
- magnetic resonance imaging;
- computed tomography;
- ultrasound examination of the blood vessels of the brain;
- taking urine, blood and cerebral fluid tests.
Using EEG, disorganization of rhythms, which are a manifestation of epileptic activity, is detected. CT scans with MRI are necessary to detect atrophic changes in the brain. Using these diagnostic methods, the ventricles, subarachnoid space, and deepening of the sulcus of the brain are checked. To detect pathological abnormalities, a variant of nuclear MRI is used. Testing is necessary to identify toxic substances in them.
What are the forecasts
Forecasts that relate directly to alcoencephalopathy directly depend on the type and stage of the disease. Acute types of pathologies rarely go away completely without consequences. In the vast majority of diagnosed cases, they are fatal. Survivors develop various serious complications that significantly reduce the quality and length of life.
But timely, competent therapy using innovative therapy developments allows one to achieve better results. It must be remembered that treating encephalopathy at the stage of alcohol addiction is much more difficult than preventing its development. That is why you should reconsider your own lifestyle and give up alcohol abuse.
A tragedy happened in our family - our son buried both his wife and children. Died in a car accident. I've been drinking heavily since then. He was recently diagnosed with alcoholic encephalopathy of the brain. They say it can't be cured. How long do people with this diagnosis live?
The favorability of a disease such as alcoholic encephalopathy of the brain can be judged only after the appropriate diagnostic measures have been carried out. Of course, for those who have already been diagnosed with this pathology, the relevant question is how long you can live with it. In reality, no qualified doctor can give a specific answer. After all, everything depends on the disease that caused encephalopathy and the degree of brain damage. The general condition of the patient, as well as his internal mood, also affects.
Encephalopathy can be observed for a long time in its initial manifestations. On average, this period is about fifteen years
During this period, it is important to pay attention to your own health. After all, it is at this stage that it is easier to stop the pathological process. With adequate treatment of diseases in the medical history, as well as adherence to the principles of a healthy lifestyle, each patient can change their own future, improving the quality of life
With adequate treatment of diseases in the medical history, as well as adherence to the principles of a healthy lifestyle, each patient can change their own future, improving the quality of life.
Of course, if we are talking about acute conditions, the prognosis is less favorable. Such patients may live significantly shorter
In general, in order to improve the condition of encephalopathy, it is important to be regularly monitored by a doctor. Diagnosis and treatment are always mandatory
Therefore, you should not neglect them. Thanks to an appropriate lifestyle, you can improve and even restore your own health.
The group of alcoholic encephalopathies includes diseases included in the category of metal-alcohol psychoses, that is, complications of chronic alcoholism that occur with metabolic disorders, organ diseases and other problems. The term "encephalopathy" refers to diseases that are caused by damage to brain tissue.
The clinical signs of this group of diseases are very diverse. Patients experience hallucinatory experiences, delusions, neurological complaints, mental changes, and disorders of internal organs. Our task is to understand the types of encephalopathies in more detail.
Quick Facts
Encephalopathy of toxic origin is considered a severe form of intoxication. According to average statistical indicators, the largest incidence of deviations from the norm is caused by addiction to alcohol (up to 18%) and drugs (up to 13%). In third place are poisonings caused by inhalation of heavy metals (for example, lead, mercury, manganese) and affect 5 to 7% of individuals. Defeat strikes workers at manufacturing plants or mining companies. The highest frequency of TE diagnosis is found in the employed population in the age category from 25 to 55 years. By gender, the disease is observed more often in males.
Chronic alcoholic encephalopathies
Mostly (except for Korsakovsky) - rare forms of psychosis. Some of them are not found in every doctor’s practice.
Types of chronic alcoholic encephalopathies:
- Korsakov psychosis. In the specialized literature it is described, among other things, as alcoholic paralysis and polyneuritic psychosis. It develops more often in women 40-60 years old. In most cases, it is the result of acute encephalopathies. Mental manifestations consist of a symptomatic triad - amnesia (memory loss), disorientation, confabulation (memories of events that did not actually occur). Neurological complaints consist of the development of neuritis of the arms and legs, severe muscle atrophy. With treatment, the disease undergoes reverse development.
- Alcoholic pseudoparalysis. Very rare. More often in mature men after severe delirium and Gaye-Wernicke encephalopathy. Patients experience decreased judgment, loss of knowledge, flattened character, and lack of self-criticism. Rough and vulgar humor, rudeness, self-aggrandizement in conversation. The appearance of the patients is typical: tremors in the hands and facial muscles, speech impairment, weakened pupillary response to light. With active therapy, the condition improves. In the presence of concomitant diseases, the disease progresses.
Rare variants of chronic alcoholic encephalopathies:
Alcoholic encephalopathy due to stenosis of the superior vena cava. Occurs in alcoholics with liver cirrhosis. Often not recognized. With this form, a stunned state develops sharply with manifestations of yellowness of the skin and mucous membranes
Mental changes are characterized by a euphoric mood, stupid behavior, childish playfulness, and apathy. Please note: the fingers bend and straighten in a characteristic manner. The attacks are reversible and last no more than 1-2 days.
Alcoholic encephalopathy Marchiafava–Bignami
A disease of Italian peasants who consumed large quantities of red wine. The disease was also recorded in France, the USA, and Argentina. Mostly men suffer. Against the background of progressive degradation, delirium, stupor, and severe neurological problems (speech disorders, muscle tension, paralysis with sphincter disorders) develop.
Morel's disease. Develops against the background of wine alcoholism. Manifestations resemble Gaye-Wernicke encephalopathy. The outcome is unfavorable.
Alcoholic pellagra. The cause of this encephalopathy is a deficiency of vitamins B and PP, which often accompanies the course of alcoholism. The onset of manifestations is pellagronic neurasthenia - headache, fatigue, stomatitis, damage to the intestinal tract with severe diarrhea. Patients experience characteristic changes on the skin - red and brown spots on the hands, feet, neck and face.
Alcoholic cerebellar atrophy. In the clinic of this form, imbalance and unsteady walking are observed.
Among chronic alcoholic encephalopathies, there are variants with a beri-beri pattern (against the background of vitamin B1 deficiency), with retrobulbar neuritis (impaired central and lateral vision, normal color rendering), with central necrosis of the bridge (severe neurological manifestations with a distinctive feature - insensitivity to pain) .
Diagnosis of alcoholic encephalopathies is based on the manifestations of the disease, computed tomography, MRI, encephalography, rheography, angiography, and other methods.
Make an appointment with a neurologist
A multidisciplinary medical specialist suggests attending a consultation with a neurologist. Patients are offered diagnostics and treatment using the latest equipment, comfortable conditions, safety, individual approach and favorable service offers. You can make an appointment by phone or through the registration form on the website.
Moscow, st. Krasnodarskaya, house. 52, bldg. 2
+7
We work on weekdays and weekends from 8.00 to 21.00
Description of symptoms
Symptoms of alcoholic encephalopathy depend on the form of the disease. There are only two of them: chronic and acute. Acute encephalopathy is diagnosed less frequently; more often alcoholics suffer from a chronic form of the disease due to prolonged use of alcohol.
Gaye-Wernicke syndrome is an acute form of the disease and has the following symptoms:
- High body temperature (up to fever).
- Peeling of the skin and change in complexion.
- Swelling on the face and body.
- Lack of consciousness or impaired perception of information.
- Speech disturbance (muttering, delirium, screaming).
- Decreased reflexes.
Acute alcoholic encephalopathy occurs against the background of brain damage. The syndrome is most often diagnosed in men, much less often in women. The main and main symptom of the disease is weakness, in which a person is constantly in bed.
Alcoholic toxic encephalopathy can be fulminant in nature. When stupor occurs 3 to 5 days after the onset of the first symptoms, this is an alarming sign. Symptoms gradually increase, and after a short time the patient falls into a coma, followed by death.
Mitigated encephalopathy is considered another acute form. It develops with prolonged use of alcoholic beverages.
Main signs of the disease:
- decreased appetite (a person refuses food, experiencing disgust for it);
- sleep disturbance (the patient does not sleep well at night, he is tormented by nightmares);
- partial memory impairment (the patient can say his name, but at the same time forget basic things);
- inflammation of the optic nerve (ophthalmologists call this disease neuritis);
- a state of perpetual depression.
With alcoholic encephalopathy of the mitigated type, a person is in a special state. It is no secret that the disease has a negative effect on the nervous system. For this reason, the patient behaves inappropriately: sometimes he cries, sometimes he laughs, sometimes he shows outbursts of aggression for no particular reason.
Attention! Encephalopolyneuropathy is one of the signs of brain damage. Characterizes itself with numbness of the limbs, impaired motor function
Alcoholic encephalopathies come in not only acute but also chronic forms. Chronic ones include:
- Korsakov psychosis.
- Alcoholic pseudoparalysis.
Toxic encephalopathy of the brain of a chronic type, called Korsakoff psychosis. When making such a diagnosis, a triad of symptoms is taken into account. The first sign is considered to be a decrease in memory, or rather, its impairment. A person tells events that did not exist, but can describe them in detail. Often the story is fantastic.
In addition to memory impairment, there is spatial disorientation. The patient responds to his name, but does not understand where he is, what day and hour it is.
The third symptom is toxic (or toxic) damage to the body, which leads to the development of neuropathy, that is, the patient’s legs fail.
What is chronic alcoholic encephalopathy called alcoholic pseudoparalysis? This is a pathological human condition that develops against the background of prolonged consumption of alcohol-containing drinks. Despite the fact that the disease is chronic, it rarely leads to death, but can cause profound dementia.
Alcoholic pseudoparalysis has a characteristic clinical picture:
- memory function disorder;
- rude, inappropriate behavior (jokes, ridicule);
- signs of dementia;
- mental behavior disorder.
What is toxic encephalopathy? This is a disease that can occur due to the use of alcohol or medications. The disease is characterized by severe intoxication and can cause severe disability or death.
Many people argue that alcohol with low alcohol content cannot cause serious complications. Actually this is not true. Alcoholism can progress due to prolonged consumption of alcohol-containing drinks, even if we are talking about beer or cocktails. To become an alcoholic, it is not necessary to drink vodka or alcohol; it is enough to regularly consume a certain dose of ethyl, as a result of which addiction develops.
In turn, regular consumption of alcohol leads to changes in the human body. They mainly affect the nervous system and brain. Symptoms and treatment of the disease directly depend on the duration of alcohol intake and toxic damage to the patient’s body. Before starting therapy, it is necessary to conduct a number of diagnostic studies.
Symptoms
Depending on the form of the disease, alcoholic encephalopathy manifests itself through various unpleasant symptoms. But the most common ones include the following:
- cerebellar insufficiency, which manifests itself as imbalance with coordination, tremor of the upper extremities;
- feeling of chronic fatigue;
- decreased interest in something;
- dementia;
- weight loss due to loss of appetite;
- sudden mood swings;
- aggressiveness;
- anxiety;
- causeless fear;
- chills followed by fever and vice versa;
- decreased heart rate;
- insomnia;
- memory impairment;
- hallucinations, acute psychosis with delusions and other mental disorders.
Classification of the disease
This disease can occur in both acute and chronic forms.
The acute form develops very quickly. Treatment of acute forms of this disease is a rather complex process, and the consequences can be very severe, even fatal.
The development of chronic forms occurs more slowly, over several years, and the likelihood of a favorable outcome is much higher.
Acute forms include Gaye-Wernecke encephalopathy, and chronic forms include Korsakoff psychosis and alcoholic pseudoparalysis.
Gaye-Wernicke encephalopathy
The cause of the development of this form of alcoholic encephalopathy is thiamine deficiency. Gaye-Wernicke encephalopathy is more common than other forms of this disease.
MRI results of a patient with Gaye-Wernicke encephalopathy
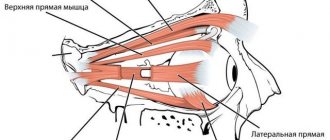
Mostly middle-aged men are susceptible to this form of the disease. The disease manifests itself as a sharp deterioration in the patient’s health: a person’s number of disorders of a different spectrum increases, and exacerbations of diseases characteristic of people suffering from alcoholism develop. Gaye-Wernicke encephalopathy is characterized by three main symptoms: ophthalmoplegia (paralysis of the eye muscles), ataxia and impaired consciousness.
The symptoms of Gaia-Wernicke are as follows:
- at the slightest physical exertion, a person becomes ill, he experiences weakness, arrhythmia and shortness of breath, and a feeling of constriction appears in the chest;
- the patient often complains of pain in the head, heart and limbs;
- the patient develops a feeling of causeless anxiety, fear, panic;
- there is a deterioration in muscle tone;
- body temperature is constantly elevated, the patient experiences increased sweating;
- the appearance and condition of the skin deteriorates;
- a person becomes unable to perceive someone else’s speech and speak himself;
- Stunning of consciousness is possible, leading to stupor, and in severe cases, coma.
A key feature of Gayet-Wernecke encephalopathy is that the patient's consumption of alcohol does not lead to either relief or pleasure.
Gaye-Wernecke is the most dangerous to health and life - in advanced cases, a person falls into a coma; in the absence of treatment, death is possible, occurring on average two weeks from the onset of the disease.
Korsakov psychosis
Korsakov's psychosis is more common among females.
It occurs due to a lack of vitamin B1. During this form of the disease, a person’s orientation in time and space is disturbed; he may confuse the location of rooms at home, forget the way home, or get lost while walking along his usual route.
Problems with memory appear, a person cannot correctly say his name or date of birth, repeats requests several times, addresses a familiar person as if he were a stranger.
The patient develops confabulations - the so-called. false memories. A person comes up with incredible events, stories and passes them off as actually happening. Thanks to this, the person suffering from Korsakov psychosis fills in the memory gaps that have appeared.
In victims of this disease, skin sensitivity is impaired and muscles atrophy. In elderly patients, a pronounced disturbance in facial expression appears; the face becomes like a mask.
With Korsakov psychosis, a person’s intellect does not suffer, his knowledge is preserved, and the patient thinks relatively sensibly.
Alcoholic pseudoparalysis
Middle-aged and older men are more susceptible to this form of the disease.
It is less common than Gayet-Wernecke encephalopathy and Korsakoff's psychosis. The patient's memory deteriorates, dementia develops, mood swings, causeless anxiety, manic states, and euphoria appear, often accompanied by delusions of grandeur.
The level of criticism towards yourself and your condition decreases. Neurological disorders soon make themselves felt, such as sluggish facial expressions, trembling of the limbs, twitching of the facial muscles, changes in tendon reflexes and impaired coordination.
With a timely course of treatment for alcoholic pseudoparalysis, the symptoms can regress and disappear, and the person can return to their normal life.
Consequences and forecasts
After discharge, patients are recommended to undergo sanatorium-resort treatment.
Acute neurotoxic processes are in most cases reversible and disappear completely within a few months. In some cases, the patient retains some symptoms of the disease: polyneuropathy, tremors, decreased mental abilities. The latter is most often noted in cases where toxic-hypoxic encephalopathy has occurred.
In turn, chronic intoxication with neurotoxic poisons is almost never completely cured. Experts manage to somewhat weaken the effects of the xenobiotic.
However, existing organic disorders in the structure of organs do not allow the symptoms to be eliminated completely. Such patients retain tremor, emotional instability, and psychoneurological disorders caused by changes in one or another structure of the brain.
Alcoholic encephalopathy
There are a number of pathological conditions that develop against the background of prolonged and uncontrolled drinking. Similar pathologies include encephalopathy. The occurrence of acute alcoholic encephalopathy indicates the presence of lesions in the brain with serious functional impairment.
If a person constantly abuses alcohol, then there is an imbalance of vitamins in his body. It’s just that, along with ethanol metabolites, a drinking person loses trace elements and minerals in huge quantities. necessary for a normal life. They are simply washed out en masse, but proper replenishment does not occur. And where do these vitamins and microelements come from if the food of an alcohol dependent person is always meager and consists of monotonous snacks, or there is no food at all. Often alcohol replaces food for an alcoholic, and alcohol itself is considered a very high-calorie product, but it does not contain the full range of essential nutrients, microelements and vitamins.
A particular deficiency is observed in vitamins P, B6 and B1. These vitamins are categorically incompatible with alcohol, but they are extremely necessary for health. For example, thiamine is necessary for the formation of new cells and normal absorption of carbohydrates. B1 also provides protection to the cardiovascular system, central nervous system and brain cells from all kinds of negative influences. With an acute complex deficiency of thiamine, pyridoxine and bioflavonoids, the human brain swells, and some parts of it even die. The blood vessels in the brain become thinner and edema forms. At times, damage affects only certain areas of the brain, but this is only for now.
The most suffering organ in people who drink is the brain. Although it cannot be unequivocally stated that alcohol is the only cause of encephalopathy. In fact, alcoholic encephalopathy is a consequence of disorders that affect the functionality of vital systems and organs.
Typically, the pathogenetic structure of encephalopathy of alcoholic origin includes factors such as exhaustion of the body, constant poisoning with ethanol metabolites. leading to the development of liver cirrhosis, hepatitis, digestive problems, etc. The body begins to experience an urgent need for vitamins and microelements, and against the background of these changes, serious disturbances occur in the cerebral cortex.
Alcoholic encephalopathy is inevitably accompanied by oxidative stress. When ethanol is metabolized, particularly dangerous substances are released - aldehydes, which poison brain neurons. This factor is fundamental in the development of pathology. But heredity also plays a certain role, although most often pathology is passed on to offspring only in terms of predisposition to alcohol addiction.
How is the treatment carried out?
The main goal of therapy is to completely rid the patient of the chemical element, reduce brain disorders, and correct neurological deficits. Based on the severity of the patient’s general condition, the treatment course can be carried out in the clinic of the neurological department, the intensive care unit or the intensive care unit. Treatment includes:
- To remove the toxic component of their body, doctors perform gastric lavage with distilled water or medical reagents, then prescribe enterosorbents.
- Detoxification procedures are aimed at binding or eliminating chemicals that have entered the blood. The patient is prescribed intravenous injections of plasma substitutes and clinical antidotes, hemodialysis, etc.
- Symptomatic and pathogenetic methods - use mask inhalations with oxygen, mechanical ventilation, the use of pharmacological drugs with antiepileptic and diuretic effects, tranquilizers, corticosteroids.