What is the function of a Rathke pocket?
This anatomical structure originates in the initial stages of embryo development in the womb. Subsequently, it is transformed into the anterior lobe of the pituitary gland of the brain. Normally, a healthy newborn does not have a Rathke's pouch. In some people, particles of this structure remain. They form an independent cavity. It is located in close proximity to the pituitary gland and serves as the basis for the formation of cystic formation.
More about the disease
In fact, choroid plexus cysts in the fetus are not the most common problem. The probability of its manifestation occurs in 1 to 3% of cases among all observed pregnant women with a normal course of gestation. But it does not pose a particular threat to the life of the unborn baby.
Important! A diagnosed brain cyst in a fetus of this type cannot harm either a child or an adult if it remains with him for life (quite rare). Even in the presence of numerous cystic formations, the clinical prognosis is unchanged.
Cysts of the choroid plexus of the brain are an accumulation of cerebrospinal secretion inside the plexus of ducts itself, which is synthesized by it to feed the spinal cord and brain of the embryo. The vascular plexuses themselves arise in the early stages of the formation of the central nervous system in the fetus, and their paired numbers indicate the development of the two hemispheres of the brain. On ultrasound, these accumulations look like a cyst-like formation, therefore, in the reports, the pathology is positioned as a cyst of the choroid plexus of the brain.
What factors provoke pathology?
The exact causes of the occurrence and development of the neoplasm have not been established. Doctors identify a number of factors, the presence of which increases the likelihood of a cyst. These include:
- hereditary predisposition;
- viral diseases with aggravated course;
- inflammatory processes;
- hypoxia;
- intoxication of the body of a pregnant woman;
- irradiation, radiation;
- difficult childbirth;
- excessive exposure to UV rays.
The neoplasm is formed in the embryonic period. Doctors suggest that from its remains another structure is born - the adenohypophysis. Rathke's pouch cyst and endocrine gland cyst have the same origin. Therefore, doctors tend to believe that a pathological neoplasm and a pituitary adenoma can develop in parallel.
Why do they arise?
Cysts of the choroid plexus of the fetal brain are not equated to dangerous pathological processes, and are not considered a deviation. Often, this problem goes away on its own by the 28th week of pregnancy. But even if it does not resolve, this formation does not pose a threat to life. This type of pathology also includes a Blake's pouch cyst.
The formation of late cystic neoplasms is the result of the development of infectious diseases with enlarged lymph nodes, which provoke the appearance of a series of complications during gestation or during labor. The most common cause of this factor is the herpes virus. In infants, the pathology occurs with virtually no symptoms, but in adult life they can remind themselves, since the disease occurs against the background of a number of other factors.
Possible causative agents of cysts in a fetus of this type:
- injuries of various origins (including birth, concussions, etc.);
- micro-strokes;
- ischemic strokes;
- infections of various types;
- premature labor;
- deviations of the child in weight category, size, etc.;
- the presence of pronounced problems in the structure and dimensions of the head, the presence of pathologies in the anatomical characteristics of organs;
- aneurysm;
- hemorrhagic strokes.
Important! Research by specialists has shown that choroid plexus cysts can appear both in children with developmental problems and in children without any abnormalities.
A brain cyst in a child is diagnosed during neurosonography.
Who is at high risk?
The congenital pathology described in the article is a rare occurrence. It accounts for only 1% of cases among other benign neoplasms. Nevertheless, experts were able to identify a group of people whose representatives are more susceptible to developing the disease. It includes:
- Women of mature age. A tendency towards an increase in the size of the cyst and the appearance of its symptoms is observed after 40 years.
- Patients after meningitis or encephalitis of any etiology.
- Patients who have had a stroke.
- Workers of hazardous chemical production.
- People whose relatives have been diagnosed with a brain tumor.
A match on one or more points from the list above means an increased risk of developing a neoplasm. Such people should pay special attention to their own health and be sure to undergo a body examination.
Classification depending on location and degree of development
A choroid plexus cyst in a 20-week fetus or newborn is accepted by parents almost as a death sentence. But is everything so serious and dangerous?
Medical terms:
- A cystic neoplasm of the cerebral ventricle plexus on the right is a unilateral tumor. In the presence of genetic pathologies, the structure of the brain undergoes modifications. Abnormal processes can be detected during ultrasound. Cysts of the left choroid plexus (or right), accompanied by low levels of hCG and PAPP-A, are an indicator of congenital anomalies.
- Bilateral choroid plexus cysts of the brain are tumors with bilateral involvement. Structural indicators remain intact. The bases of the choroid plexuses of the lateral ventricles (left and right) are affected. Numerous pathological formations are diagnosed both in infancy and in adulthood.
A plexus cyst can remain with a patient all his life without causing problems if the tumor itself does not grow. But as it progresses, consequences may arise that worsen the patient’s quality of life:
- problems with coordination of movements (usually almost invisible);
- hypertonicity, which can be observed in newborns;
- pressure on the brain as the cystic formation increases in volume;
- minor hearing and vision disorders.
Even if the patient has such symptoms, the choroid plexus cyst is still very treatable.
The first manifestations of pathology
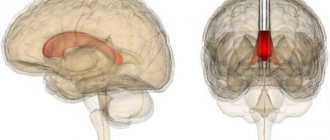
Rathke's pouch cyst is characterized by a long-term asymptomatic course. Often patients are unaware of the presence of such an insidious pathology in the brain. They usually find out about it after undergoing an MRI or other preventive examinations. The first symptoms of a neoplasm appear as its size increases. Rathke's pouch cyst begins to compress the optic nerve and the pituitary gland itself. As a result, pathological disturbances in the blood supply to the brain and disruption in the functioning of its main structures develop. In addition, the following disorders cannot be ruled out:
- dizziness;
- insomnia;
- hallucinations;
- nausea and vomiting;
- tinnitus;
- short-term memory lapses;
- violations of motor coordination.
In 80% of patients, the pathology is accompanied by diseases of the endocrine system. Many also note the appearance of mental disorders and confusion. The degree of manifestation of clinical symptoms largely depends on the size of the tumor, the force of pressure on neighboring nerve endings and blood vessels.
Symptoms
Like most cystic formations, this pathology often passes without obvious symptoms. The cyst begins to manifest itself only when it reaches a certain size. In this case, it begins to put pressure on neighboring areas. Due to the peculiarities of their location, the following may be affected by cysts: the pituitary gland, optic nerves, and cavernous sinus. The cavernous sinus is part of the dense membrane of the brain, which is involved in the regulation of blood circulation. As a result, the patient may exhibit the following symptoms and signs:
Possible complications
What consequences can a Rathke's pouch cyst cause? It is not the tumor itself that is dangerous, but the speed of its growth. Therefore, after identifying the pathology, the patient remains under the supervision of a doctor for some time. If it grows rapidly, urgent surgery is indicated. Lack of adequate therapy can lead to unpleasant consequences. First, the patient loses his vision. Then the clinical picture is complemented by mental disorders and destruction of the pituitary gland. In particularly serious cases, the cyst degenerates into a malignant tumor.
Variation of treatment
As already mentioned, cystic neoplasms of the choroid plexus extremely rarely provoke the development of degenerative disorders and symptoms. No specific measures are required to treat this disease; dynamic observation is sufficient if the cystic bodies do not resolve after the birth of the baby. Even if the previous forms of formation are preserved, this will not affect the health and development of the child.
Only with the active growth of a neoplasm or a predisposition to this factor, there is a need to reduce it. According to experts, an increase in pathology in volume occurs from the 24th week of embryo formation. But in the normal course of events, the cysts disappear by the 28th week of the fetus’s life.
The appearance of cysts in the plural is the result of an infectious disease suffered by a woman during pregnancy. In this case, all therapeutic manipulations are aimed at eliminating the consequences of the recently rampant disease.
In order to prevent the possibility of the formation of abnormalities at the genetic level after a diagnosed plexus cyst, the doctor prescribes a general examination for the child and a course of therapeutic manipulations to eliminate any anomalies for the further full development of the baby.
Diagnostic methods
If you suspect a Rathke's pouch cyst, the patient first needs to visit an endocrinologist. Sometimes additional consultation with a neurologist is required. To confirm the diagnosis and determine the size of the tumor, the following diagnostic methods are used:
- MRI. This research method is considered the most informative. From the images, the doctor can assess the size, location and anatomical characteristics of the cyst. All data is necessary for subsequent treatment.
- CT. A computed tomography scan can help identify calcification. The presence of this process usually points to the alternative diagnosis of craniopharyngioma.
- Angiographic examination of cerebral vessels.
To exclude the malignant nature of the neoplasm, additional examination by an oncologist may be required. Usually it involves taking a puncture for subsequent study of the material in the laboratory.
Surgical intervention
An increasing size of Rathke's pouch cyst requires a completely different approach. Treatment in this case also begins with hormonal drugs. If therapy is ineffective, the patient becomes worse and surgery is prescribed. Today, two types of surgical interventions are used in practice, each of which has its own characteristics.
- Classic transsphenoidal surgery. It comes down to removing the cyst through an incision in the nasal concha. Access to Rathke's pouch is possible only through the sphenoid sinus. To clearly see the surgical field, the surgeon uses a binocular microscope.
- Laparoscopic intervention is still the most popular. This is carried out using a special device - an endoscope. During surgery, the surgeon can easily remove the tumor without damaging the vessels and nerve endings near the pituitary gland. The doctor also enters the skull through the nasal passages.
After removal of the cyst, all its contents must be sent to the laboratory. Histological examination of the secretion allows us to exclude the malignant nature of the pathology. The surgical options described just above are the only effective methods of dealing with such a problem as Rathke's pouch cyst. Treatment with folk remedies is strictly contraindicated.
Reasons for development
Many medical experts argue about the reasons for the development of this pathology. There has not yet been a consensus on what to become the main reasons for its development. The most likely factors are:
- genetic predisposition;
- infectious diseases;
- pregnancy accompanied by viral diseases;
- inflammatory processes in the body;
- long-term use of medications;
- exposure to toxins on the mother’s body;
- radiation dose or exposure received while carrying a child;
- prolonged and constant exposure to sunlight;
- problems at the birth of a child.