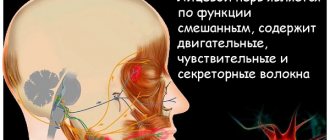
The peroneal nerve arises from the sciatic nerve at the level of the popliteal fossa. It runs in the outer part of the lower leg, foot, carries both sensory and motor fibers, that is, it is mixed in function. Its branches:
- External cutaneous nerve of the calf - provides sensitivity to the skin of the lower leg in the posterior outer region.
- Superficial peroneal – provides flexion and abduction of the foot, sensitivity of the skin on the dorsum of the foot.
- Deep peroneal – provides extension of the foot and toes, sensitivity of the skin of the foot.
With neuritis, these functions are disrupted.
Our expert in this field:
Kamyshev Lev Gennadievich
Manual therapy doctor, neurologist
Call the doctor
How to treat peroneal nerve neuropathy
Lack of mobility in the foot, numbness, and tingling indicate damage to the peroneal nerve. It emerges from the lumbar spine, branching from the sciatic nerve.
Damage can occur at the peripheral level - outside the spinal cord. Depending on the location and type of damage, treatment for peroneal nerve neuropathy is prescribed. Folk remedies can also support the body and stimulate the regeneration of nervous tissue.
What is peroneal nerve neuropathy?
Damage to the peroneal nerve is manifested by impaired extension and pronation of the foot. This is the most common mononeuropathy of the lower extremities.
The symptom of foot drop occurs after various injuries that result in muscle damage or compression or stretching of the nerve. Damage is possible due to metabolic disorders, such as diabetes.
Most often, the peroneal nerve is injured at the level of the knee. The common branch of the sciatic nerve is susceptible to damage in the pelvis and lower leg. It belongs to the sacral plexus and is formed by the roots of the last two lumbar and four sacral roots.
It exits the pelvic cavity through the greater sciatic foramen - in 90% of cases under the piriformis muscle and in 10% pierces its abdomen.
The sciatic nerve divides into the common peroneal and tibial nerves in the popliteal region. Next, the peroneal nerve descends along the lateral head of the gastrocnemius muscle and provides nerve signals to the outer side of the leg. The branch continues between the peroneus longus muscle and the fibula, where it again divides into two parts:
- The deep nerve provides movement to the tibialis anterior, extensor hallucis and extensor digitorum longus, and the tertiary peroneal nerve is responsible for extension of the foot. In the foot, it innervates the extensor digitorum brevis, the space between the second and first toes;
- the superficial nerve descends between the long and short peroneals to the main pronator muscles of the foot, as well as sensitivity of the outer part of the leg, foot and toes.
Neuropathy is manifested by dysfunction of one of the listed muscles, a decrease in the sensitive innervation of the skin, which receives impulses from this segment. This type of peripheral neuropathy develops in people of any age and is one of the common mononeuropathies.
Causes of occurrence and risk groups
Neuropathies develop when the myelin sheath covering the fiber is damaged. It is necessary for signal transmission. The axon or the body of the process - the neuron - can be injured, which leads to more serious symptoms.
The main causes of damage to the peroneal branch:
- knee injury;
- fracture of the fibula;
- use of a rigid orthosis or casting of the lower leg;
- habit of crossing legs;
- wearing high-top boots;
- pressure on the nerve during sleep, anesthesia;
- surgical damage.
People with a certain constitution are prone to developing mononeuropathy:
- excessively thin;
- suffering from autoimmune pathologies;
- drinking alcohol;
- patients with diabetes;
- people with hereditary lesions of nervous tissue (Charcot-Marie-Tooth syndrome).
The common peroneal nerve is most often injured at the level of the peroneus longus tendon, where it wraps around the head of the fibula and passes into the interosseous membrane.
The sciatic nerve is damaged at the level of the lateral branches, from which the common peroneal nerve arises. Compression-ischemic neuropathy is an occupational disease of people who spend long periods of time squatting.
Post-traumatic neuropathy is one of the complications of femoral osteotomy, which causes paresis of the peroneal nerve. Damage occurs when the femur is displaced without fracture. The causes of the lesion are a fracture of the femur, as well as surgery to restore the knee after injury.
With sharp plantar flexion of the foot, the peroneal nerve is stretched simultaneously with the muscle of the same name. Two weeks after injury, patients should be examined for nerve conduction.
Peripheral neuropathy occurs when the knee ligaments are damaged in almost 60% of sports injuries. Subluxations and dislocations of the ankle also affect its function, but more so – their treatment, which provokes long-term compression of the head of the fibula.
Active extension of the thumb indicates deep peroneal nerve function while the patient is in the cast. Swelling of the lower leg also contributes to dysfunction and impaired nerve conduction.
In osteoarthritis accompanied by knee varus deformity, the nerve is injured as a result of walking. With valgus, it is initially weakened along with the lateral branch of the sciatic, and inflammation of the tibial nerve often develops.
Symptoms
With compression and disruption of nerve conduction, the following symptoms occur:
- decreased sensitivity, numbness, tingling on the front or outside of the leg;
- foot drop or inability to straighten it;
- "splattering" gait;
- dangling fingers while walking;
- difficulty moving, lameness;
- weakness in the ankle or foot;
- muscle atrophy in the lower leg and foot.
Symptoms of tibial nerve damage may include cramps and burning pain. Deformities, corns and calluses are an indirect sign of decreased nerve conduction in the periphery or compression syndrome in the lumbar region.
Diagnostic methods
Patients who complain of pain along the outer leg and forefoot, as well as radiculopathy, should be evaluated for nerve conduction. Foot drop is the first sign of motor impairment.
If the injury occurs at the lumbar level, the patient cannot move the leg to the side, rotate the thigh outward, bend the knee, straighten the foot and big toe, or flex the foot. Similar disorders occur when damage occurs at the level of the piriformis muscle. At lower compression levels, only the foot is affected.
Sensitive conductivity – the area between the first and second fingers – must be studied. The patient is asked to extend the feet and toes under resistance, compared with the muscle strength of the other leg.
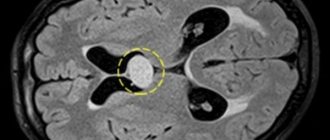
Hardware diagnostics clarifies the location and cause of the damage:
- X-ray excludes bone damage and dislocations.
- MRI is used in cases of suspected lumbar hernia or sacroiliitis.
- Ultrasound examination evaluates the integrity of the nerve at the level of the fibular head.
- Electromyography can determine the level of demyelination, a decrease in signal amplitude in the periphery, and also record a decrease in the impulse that the muscle receives.
Doctors test the strength of the muscles that flex and extend the thumb for peripheral neuropathy. The strength of the short head of the biceps femoris is tested to rule out radiculopathy or damage at the spinal level.
Treatment
It is important to eliminate the factor influencing the destruction of nerve tissue. If compression syndrome persists for a long time, it can only partially recover.
Medicines
Early signs of neuropathy are difficult to detect and treat. The following drugs are used: Diclofenac, Ibuprofen, serotonin reuptake inhibitors, opioid drugs for severe burning pain due to axonopathy. To reduce local pain, ointments with lidocaine, bee venom and red pepper are used.
In case of impaired blood supply to the lower leg, the drugs “Trental” and “Cavinton” are prescribed. Treatment is supplemented with B vitamins, vitamin C and leucine.
Folk remedies
Folk remedies cannot cure neuropathy, but they can eliminate its consequences. Compresses made from milk and honey improve the condition of tissues that have been deprived of nerve supply or blood flow.
It is necessary to moisten gauze in milk, apply liquid honey to the skin, and leave for 30 minutes. Compresses made from blue clay, which are diluted in water to a paste, help relieve inflammation. These recipes can be alternated every other day.
Surgery
For post-traumatic cases, microsurgical decompression is used . It is performed under general or local anesthesia, making an incision in the area of the head of the fibula. The fascia runs between the peroneus longus and gastrocnemius muscles. The nerve between the bands of connective tissue is released.
In this case, the peroneus longus tendon is not affected. It is this muscle that forms the peroneal tunnel. The operation does not require a cast or wearing a rigid orthosis. Symptoms are reduced in almost 50% of cases.
The second type of surgery is performed on the tarsal tunnel, where the tibial nerve divides into medial and lateral branches, controlling the adductor and abductor muscles.
Operation is necessary in three cases:
- ineffectiveness of conservative treatment;
- pinching affects walking;
- axonal damage was recorded.
The operation is performed if wearing an orthosis and physical therapy have not been able to restore the function of the foot muscles.
Source: https://VashyNogi.com/bolezni/kosti/nejropatiyu-malobertsovogo-nerva.html
Causes of the problem
The development of neuritis of the tibial nerve can be provoked by the influence of the following factors on the human body:
- the presence of a chronic source of infection in the body;
- degenerative diseases of the vertebrae;
- insufficient intake of B vitamins into the body;
- weakened immune defense;
- hypothermia;
- harmful working conditions;
- tissue trophism disorder;
- diabetes;
- history of nerve trunk injury;
- autoimmune diseases;
- vascular pathology.
The nerve is responsible for the motor activity of the posterior muscles of the leg.
Neuritis can be caused by a disorder of the trophism of nerve tissue due to mechanical compression of the ending itself or compression of the vessels feeding this formation. An important role in the development of the disease is played by hormonal disorders and damage to the body’s own cells as a result of autoaggression. A deficiency of vitamin-mineral complexes makes a person less resistant to damaging environmental factors.
Return to contents
Axonal neuropathy of the peroneal nerve
The medical term “peroneal nerve neuropathy” (FMN) is quite well known, but knowledge about this serious disease usually ends with the mentioned phrase.
A test for the presence of pathology can be carried out by standing on your heels: if you can easily stand on them, there is no reason for concern, otherwise you should learn more about SUI.
Note that the terms neuropathy, neuropathy, neuritis are different names for the same pathology.
Anatomical certificate
Neuropathy is a disease characterized by nerve damage that is non-inflammatory in nature. The disease is caused by degenerative processes, injuries or compression in the lower extremities. In addition to SUI, there is tibial nerve neuropathy. Depending on the damage to motor or sensory fibers, they are also divided into motor and sensory neuropathy.
Peroneal nerve neuropathy leads in prevalence among the listed pathologies.
Let's consider the anatomy of the peroneal nerve - the main part of the sacral plexus, the fibers of which are part of the sciatic nerve, departing from it at the level of the lower third of the femoral part of the leg.
The popliteal fossa is where these elements separate into the common peroneal nerve. It bends around the head of the fibula along a spiral trajectory. This part of the nerve's "path" runs along the surface.
Consequently, it is protected only by the skin, and therefore is under the influence of external negative factors that affect it.
Then the peroneal nerve divides, resulting in its superficial and deep branches. The “area of responsibility” of the first includes the innervation of muscle structures, rotation of the foot and sensitivity of its dorsal part.
The deep peroneal nerve serves to extend the fingers, thanks to which we are able to feel pain and touch. Compression of any of the branches disrupts the sensitivity of the foot and its toes; a person cannot straighten their phalanges. The task of the sural nerve is to innervate the posterolateral part of the lower third of the leg, the heel and the outer edge of the foot.
ICD-10 code
The term “ICD-10” is an abbreviation for the International Classification of Diseases, which was subjected to its tenth revision in 2010.
The document contains codes used to designate all diseases known to modern medical science. Neuropathy in it is represented by damage to various nerves of a non-inflammatory nature.
In ICD-10, NMN is classified in class 6 - diseases of the nervous system, and specifically - mononeuropathy, its code is G57.8.
Causes and varieties
The disease owes its occurrence and development to many reasons:
- various injuries: a fracture can lead to a pinched nerve;
- falls and blows;
- metabolic disorders;
- compression of the MN along its entire length;
- various infections against which SUI may develop;
- severe general diseases, for example, osteoarthritis, when inflamed joints compress the nerve, which leads to the development of neuropathy;
- malignant neoplasms of any localization that can compress the nerve trunks;
- incorrect position of the legs when a person is immobilized due to serious illness or prolonged surgery;
- toxic nerve damage caused by renal failure, severe forms of diabetes, alcoholism, drug addiction;
- lifestyle: representatives of certain professions - farmers, agricultural workers, floor and pipe layers, etc. - spend a lot of time in a half-bent state and risk getting compression (squeezing) of the nerve;
- disorders of the blood supply to the MN.
Neuropathy can develop if a person wears uncomfortable shoes and often sits with one leg crossed over the other.
Lesions of the peroneal nerve are primary and secondary.
- The primary type is characterized by an inflammatory reaction that occurs regardless of other pathological processes occurring in the body. The condition occurs in people who regularly load one leg, for example, when performing certain sports exercises.
- Secondary type lesions are complications of pre-existing diseases in a person. Most often, the peroneal nerve is affected as a result of compression caused by a number of pathologies: fractures and dislocations of the ankle joint, tendovaginitis, post-traumatic arthrosis, inflammation of the joint capsule, deforming osteoarthritis, etc. The secondary type includes neuropathy and MN neuralgia.
Symptoms and signs
The clinical picture of the disease is characterized by varying degrees of loss of sensitivity in the affected limb. Signs and symptoms of neuropathy appear:
- dysfunction of the limb - inability to normal flexion and extension of the fingers;
- slight concavity of the leg inward;
- inability to stand on your heels or walk on them;
- swelling;
- loss of sensitivity in parts of the legs - foot, calf, thigh, area between the thumb and index finger;
- pain that gets worse when a person tries to sit down;
- weakness in one or both legs;
- burning sensation in different parts of the foot - it could be the toes or calf muscles;
- a feeling of changing heat to cold in the lower body;
- atrophy of the muscles of the affected limb in the later stages of the disease, etc.
A characteristic symptom of SUI is a change in gait caused by the “dangling” of the leg, the inability to stand on it, and strong bending of the knees while walking.
Diagnostics
Identification of any disease, including neuropathy of the peroneal nerve, is the prerogative of a neurologist or traumatologist, if the development of the disease is provoked by a fracture. During the examination, the patient's injured leg is examined, then its sensation and functionality are tested to identify the area where the nerve is affected.
The diagnosis is confirmed and clarified through a number of examinations:
- ultrasonography;
- electromyography – to determine muscle activity;
- electroneurography - to check the speed of nerve impulses;
- radiography, which is carried out if there are appropriate indications;
- therapeutic and diagnostic blockade of trigenic points with the introduction of appropriate medications to identify affected areas of nerves;
- computed tomography and magnetic resonance imaging - these precise, highly informative techniques reveal pathological changes in controversial cases.
Medicines
Drug therapy involves the patient taking:
- nonsteroidal anti-inflammatory drugs: Diclofenac, Nimesulide, Xefocam, designed to reduce swelling, inflammation and pain. In most cases, they are prescribed for axonal neuropathy (axonopathy) of the peroneal nerve;
- B vitamins;
- antioxidants represented by the drugs Berlition, Tiogamma;
- medications designed to improve the conduction of impulses along the nerve: Proserin, Neuromidin;
- therapeutic agents that restore blood circulation in the affected area: Kaviton, Trental.
The constant use of painkillers is prohibited, as long-term use will aggravate the situation!
Physiotherapeutic procedures
Physiotherapy procedures that demonstrate high effectiveness in the treatment of neuropathy:
- massage, incl. Chinese dot;
- magnetic therapy;
- electrical stimulation;
- reflexology;
- Exercise therapy. The first classes should be conducted with the participation of an experienced trainer, after which the patient will be able to do therapeutic exercises independently at home;
- electrophoresis;
- heat therapy.
Massage for peroneal nerve neuropathy is the prerogative of a specialist, and therefore it is prohibited to do it yourself!
Surgical intervention
If conservative methods do not give the expected results, they resort to surgery. The operation is prescribed for traumatic rupture of the nerve fiber. Possible:
After surgery, a person needs a long recovery. During this period, his physical activity is limited, including the performance of physical therapy exercises.
A daily examination of the operated limb is carried out to identify wounds and cracks, if detected, the leg is provided with rest - the patient moves with special crutches. If there are wounds, they are treated using antiseptic agents.
Consequences and prevention
SUI is a serious disease that requires timely and adequate treatment, otherwise a person faces a bleak future.
A possible development of events is disability with partial loss of ability to work, since paresis, manifested by a decrease in the strength of the limbs, is often a complication of SUI.
However, if a person goes through all stages of treatment, the situation improves significantly.
Source: https://BoliGolovnie.ru/varikoz/aksonalnaja-nejropatija-malobercovogo-nerva.html
Diagnostics
Determining peroneal neuropathy begins with questioning.
A neurologist or traumatologist listens to complaints and examines the patient. If you suspect something is wrong, you can immediately use the “heel” test. It is not possible to stand on your heels normally - there is nerve damage.
The doctor tries to turn the foot towards the outside or straighten the toes. This is a simple test to detect neuropathy.
If this type of pathology is present, such an action will be extremely difficult (with effort) or not possible at all. Visually, you can also determine the “birdlike” gait, as well as muscle atrophy.
To determine the presence or absence of sensitivity, take a special needle and touch the desired limb.
After a preliminary diagnosis, the degree of nerve damage is clarified. To do this, electromyography is performed. They may prescribe an ultrasound of the nerve or vessels of the lower extremities, or an MRI.
If the disease arose as a result of grass, then an x-ray of the bone is taken. When the situation is not entirely clear, they resort to novocaine blockade for diagnosis.
It is important to correctly distinguish neuropathy from such pathologies as: polyneuropathy, neuropathy, PMA syndrome, as well as atrophy and tumors of the spine.
Among the problems faced by neurology, neuropathy of the lower extremities occupies a large place. Let us consider in detail the main types of therapy used in modern medicine.
Read about the symptoms and treatment of acoustic neuritis in the next topic.
What is vibration disease and who is at risk for this disease, we will consider further.
Peroneal nerve neuropathy: causes, symptoms and treatment
Peroneal nerve neuropathy is a disease that develops as a result of damage or compression of the peroneal nerve. There are several reasons for this condition.
Symptoms are associated with a violation of the conduction of impulses along the nerve to the innervated muscles and areas of the skin, primarily weakness of the muscles that extend the foot and its toes, as well as impaired sensitivity along the outer surface of the lower leg, the dorsum of the foot and its toes.
Treatment of this pathology can be conservative and surgical. From this article you can learn about what causes peroneal nerve neuropathy, how it manifests itself and how it is treated.
To understand where the disease comes from and what symptoms characterize it, you should familiarize yourself with some information about the anatomy of the peroneal nerve.
A small anatomical educational program
The peroneal nerve is part of the sacral plexus. The nerve fibers go as part of the sciatic nerve and are separated from it into a separate common peroneal nerve at the level of or slightly above the popliteal fossa.
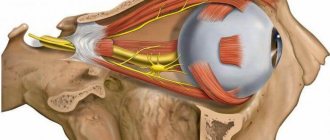
Here, the common trunk of the peroneal nerve is directed to the outer side of the popliteal fossa, spiraling around the head of the fibula. In this place it lies superficially, covered only by fascia and skin, which creates the preconditions for compression of the nerve from the outside.
The peroneal nerve then splits into superficial and deep branches. Somewhat higher than the division of the nerve, another branch departs - the external cutaneous nerve of the leg, which in the region of the lower third of the leg connects with the branch of the tibial nerve, forming the sural nerve.
The sural nerve innervates the posterolateral part of the lower third of the leg, the heel, and the outer edge of the foot.
The superficial and deep branches of the peroneal nerve are so named due to their course relative to the thickness of the lower leg muscles. The superficial peroneal nerve provides innervation to the muscles that provide elevation of the outer edge of the foot, as if rotating the foot, and also forms the sensitivity of the dorsum of the foot.
The deep peroneal nerve innervates the muscles that extend the foot and toes, and provides sensations of touch and pain in the first interdigital space.
Compression of one or another branch, accordingly, is accompanied by impaired abduction of the foot outward, the inability to straighten the toes and foot, and impaired sensitivity in various parts of the foot.
According to the course of the nerve fibers, the places of its division and the origin of the external cutaneous nerve of the leg, the symptoms of compression or damage will be slightly different. Sometimes knowledge of the characteristics of the innervation of individual muscles and skin areas by the peroneal nerve helps to establish the level of compression of the nerve before using additional research methods.
Causes of peroneal nerve neuropathy
The occurrence of peroneal nerve neuropathy can be associated with various situations. It can be:
- injuries (especially often this reason is relevant for injuries of the upper outer part of the leg, where the nerve lies superficially and next to the fibula. A fracture of the fibula in this area can provoke damage to the nerve from bone fragments. And even a plaster cast applied for this reason can cause peroneal nerve neuropathy. Fracture is not the only traumatic cause. Falls and blows to this area can also cause peroneal nerve neuropathy);
- compression of the peroneal nerve along any part of its course. These are the so-called tunnel syndromes - upper and lower. The upper syndrome develops when the common peroneal nerve is compressed as part of the neurovascular bundle with intense approach of the biceps femoris muscle to the head of the fibula. Typically, this situation develops in persons of certain professions who are forced to maintain a certain position for a long time (for example, harvesters of vegetables, berries, parquet and pipe layers - a “squatting” position) or make repeated movements that compress the neurovascular bundle in this area (seamstresses, fashion models). Compression can be caused by the “leg-to-leg” position, favored by many. Inferior tunnel syndrome develops when the deep peroneal nerve is compressed on the back of the ankle joint under the ligament or on the back of the foot at the base of the first metatarsal bone. Compression in this area is possible when wearing uncomfortable (tight) shoes and when applying a plaster cast;
- disturbances in the blood supply to the peroneal nerve (nerve ischemia, as if a “stroke” of the nerve);
- incorrect position of the legs (legs) during a long operation or a serious condition of the patient, accompanied by immobility. In this case, the nerve is compressed at its most superficial location;
- getting into the nerve fibers when performing an intramuscular injection in the gluteal region (where the peroneal nerve is an integral part of the sciatic nerve);
- severe infections accompanied by damage to many nerves, including the peroneal one;
- toxic damage to peripheral nerves (for example, with severe renal failure, severe diabetes mellitus, drug and alcohol use);
- oncological diseases with metastasis and compression of the nerve by tumor nodes.
Of course, the first two groups of reasons are the most common. The rest cause neuropathy of the peroneal nerve very rarely, but they cannot be discounted.
Consequences and prevention
SUI is a serious disease that requires timely and adequate treatment, otherwise a person faces a bleak future. A possible development of events is disability with partial loss of ability to work, since paresis, manifested by a decrease in the strength of the limbs, is often a complication of SUI. However, if a person goes through all stages of treatment, the situation improves significantly.
Tibial nerve neuropathy occurs for a variety of reasons, so it is best to prevent it.
- People actively involved in sports should regularly see a doctor for timely detection of pathology, incl. tunnel syndrome, also called compression-ischemic neuropathy. They call it compression because when the nerve trunks pass through a narrow tunnel, they are compressed, and ischemic - due to a disruption in the nutrition of the nerves.
- You need to train in special comfortable shoes.
- Reducing weight to reduce stress on the legs and feet to prevent deformation.
- Women who prefer high-heeled shoes should give their feet a break by removing them during the day and devoting time to therapeutic exercises to normalize blood circulation in the extremities.
An attentive and caring attitude towards your health is the key to ensuring that neuropathy of the peroneal nerve will bypass you.
Peroneal nerve palsy occurs most often as a result of traumatic injury. In this case, the muscles that are responsible for flexing the fingers and toes, as well as those that move the feet to the side, suffer.
If no measures are taken, the position of the leg with a dropped foot becomes fixed very quickly and this is associated with the development of contractures. This position of the foot also affects the patient’s gait - with each step he is forced to raise his leg high, which resembles the gait of a rooster.
Exercise therapy for peroneal nerve paresis should be carried out only after identifying the level of reducing muscle strength. This indicator is expressed in points and ranges from 0 to 5.
- Five points – normal muscle strength.
- Four – the patient can lift the limb with only slight resistance.
- Three – the patient can lift the limb if there is no additional resistance.
- Two – movements can only be performed in the horizontal plane.
- One - active leg movements are performed with a small amplitude.
- Zero – complete immobility.
Only after passing this test can you begin to perform one or another gymnastics, which, together with massage, medication and physiotherapy, will help restore your legs to their former strength.
It is very important to understand that exercise therapy is carried out not only for the sore leg, but also for the healthy one. This is done in order to minimize the difference in range of motion between the healthy and diseased legs.
Peroneal nerve neuropathy: symptoms and treatment
The appearance of pain in the lower leg or foot is often a symptom of peroneal nerve neuropathy. The pathology is not life-threatening if it is identified and treated in a timely manner. However, it can cause a lot of discomfort and limit physical activity. Especially in children. Therefore, you should not delay seeking medical help.
Anatomical parameters
To better understand peroneal nerve neuropathy, it is necessary to have a general understanding of its anatomical features.
In general, this structural unit of the peripheral nervous system is just a part of the sciatic nerve, which continues after leaving the sacral nerve plexus.
Towards the lower third of the thigh it will be divided into 2 segments - the peroneal nerve and also the tibial nerve.
After crossing the fossa below the knee, the fibular fiber reaches the head of the bony unit of the same name. Then it bifurcates again - into superficial and also deep branches. Therefore, by the localization of pathological symptoms, one can judge the level where the pathological lesion is located - to distinguish between neuropathy of the tibial nerve or the peroneal segment.
Thus, the deep peroneal nerve, moving through the anterior zone of the leg, reaches the back of the unilateral foot, where it bifurcates again. He is responsible for the dorsal movement of the foot in one plane, as well as raising its outer edge.
While the superficial branch, innervating the anterolateral part of the limb, is responsible for raising and simultaneous flexion of the foot.
The last division of the small tibial nerve is carried out in the area of the medial third of the leg - into two cutaneous dorsal nerves.
When examined by characteristic changes, a neurologist will differentiate neuropathy of the tibial nerve from neuritis of the peroneal nerve. Skin and muscle susceptibility, arbitrariness of movements and accuracy of reflexes are assessed - axonal damage will lead to neuritis of the tibial nerve, as well as the peroneal branch.
Causes
The development of a pathological focus in a nerve fiber can occur for many reasons. Most often, specialists diagnose the following:
- various injuries of the peroneal nerve - direct injury to the limb, or compression by colloid cords after surgical interventions, simultaneously with damage to the tibial nerve;
- compression of the nerve as a result of tunnel syndrome - typical for people whose profession requires them to be in a position for a long time that is uncomfortable for the lower extremities, for example, parquet layers, seamstresses;
- vascular pathologies and other blood supply disorders that lead to tissue hypoxia - a decrease in the number of oxygen molecules in them and, accordingly, a failure of metabolic processes;
- lesions of the peroneal nerve of a toxic nature - diabetic, renal, as a rule, have a symmetrical nature of the “golf” type;
- infections - involving one of the branches of the fibular fiber in the inflammatory process, or even simultaneously with inflammation of the tibial nerve;
- compression-ischemic neuropathy occurs with tumor neoplasms - as the tumor grows and metastasizes.
Less commonly, polyneuropathy of a traumatic nature is the result of systemic diseases. For example, gout, osteoarthritis or rheumatoid arthritis.
Symptoms
Since the peroneal nerve has a significant length, the clinical picture will directly depend on the level at which the pathological focus arose.
Thus, when the fiber is compressed in the area of the knee fossa, the sensitivity of the skin on the anterolateral surface of the leg, as well as the foot, will be impaired. People stop perceiving touch or temperature fluctuations in the air. Unpleasant symptoms intensify when trying to sit down.
Among the motor disorders, difficulty in straightening the foot is typical. It is impossible to lift exactly its outer edge.
At the same time, the ability to move on the heels is lost. Another typical sign is “horse foot”. It hangs directly down, and when walking you need to raise your leg too high.
Otherwise, your fingers will cling to the floor. Visually this appears as a “horse gait”.
With a prolonged and uncontrolled course, tunnel syndrome will be complicated by muscle atrophy - the limb is smaller in volume.
When the peroneal superficial branch is injured, the symptoms are somewhat different:
- burning and discomfort in the lower area of the leg, as well as the foot and fingers from I to IV;
- failure of sensitivity in these same structures;
- a person experiences difficulty in raising and abducting the outer edge of the foot.
When the deep peroneal branch of the nerve is involved in neuropathy, the muscles that are responsible for straightening the foot, as well as its toes, suffer from slight drooping. Sensitivity is impaired between fingers I and II on the back.
Treatment tactics
When identifying this disease in people, the efforts of specialists will be aimed at eliminating the factors that provoke it - the causes of compression and inflammation. Conservative therapy is the first step in correcting the pathological situation.
The doctor selects drugs from the following subgroups:
- NSAIDs – Nimesulide, or Ibuprofen, Airtal;
- drugs for correcting conductivity in the nerve fiber - Proserin or Neuromidin;
- vitamin therapy - Milgamma or Combilipen;
- means for correcting blood circulation - Trental, Curantil;
- antioxidants – Cerebralysin, Actovegin.
To restore movement function and skin sensitivity, specialists will select physical procedures:
- magnetic therapy and electrophoresis;
- ultrasound and electrical stimulation.
Massage has proven itself to be excellent for neuropathies of the peroneal nerve. It is carried out in courses, the duration of which depends on the severity of the lesion. The help of physical therapy is invaluable - the patient begins to perform exercises under the guidance of an employee of the exercise therapy room, and then continues independently at home.
In case of traumatic or tumoral nature of compression of the peroneal nerve, one type of surgical treatment is indicated. After which a course of rehabilitation therapy is required.
Treatment methods
Massage treatments for the treatment of neuritis stimulate blood circulation
Analgesic and antipyretic drug
1. Non-steroidal anti-inflammatory drugs - have a complex therapeutic effect. Aimed at suppressing pain, inflammation and swelling. Diclofenac, Nimesulide, Xefocam are effective.
Diclofenac is an effective drug that belongs to the NSAID group. It has a pronounced analgesic, antipyretic and anti-inflammatory effect. The drug is available in several forms: tablets, suppositories, solution, ointment and drops. Prescribed to children over 15 years of age and adults no more than 150 mg per day 2-3 times.
Nimesulide also belongs to non-steroidal anti-inflammatory drugs. The difference is that Nimesulide also has an antiplatelet effect - it prevents the formation of blood clots.
2. Antioxidants. For example, Berlition, Lipin. They have immunostimulating, neurotransmitter, hypotoxic and other properties. Thanks to such drugs, it is possible to strengthen the immune system, improve blood circulation and the functioning of internal organs.
Berlition is an effective remedy for neuropathy due to diabetes mellitus or alcoholism.
Lipin improves cellular respiration and metabolic processes.
3. B vitamins (B1, B2, B6, B12).
4. Medicines that normalize the conduction of nerve impulses are necessarily prescribed when neuritis develops, as they help restore sensitivity and muscle function. (Neuromidin, Proserin).
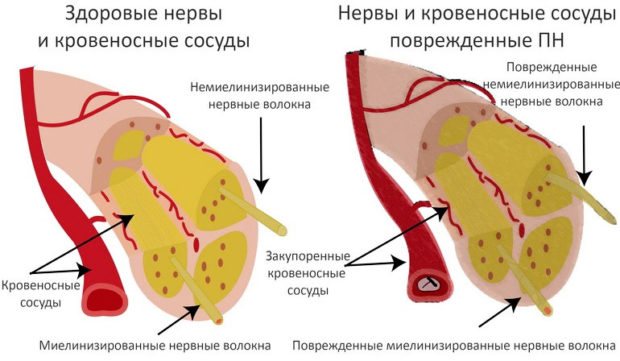
Prozerin is a synthetic drug that is widely used to treat diseases of the nervous system. Aimed at normalizing neuromuscular conduction, enhancing muscle tone and improving the functions of internal organs. The dosage and frequency of administration are determined by the doctor.
5. Drugs to improve blood flow - help eliminate blood clots and improve tissue trophism in the lower extremities. This group includes Caviton, Trental.
Kaviton is characterized by pronounced pharmacological properties. Its purpose is aimed at restoring blood circulation, reducing blood viscosity, and improving metabolic reactions.
The drug is contraindicated for persons under 18 years of age, pregnant and lactating women, as well as those with severe diseases of the cardiovascular system. Tablets start at 15 mg, gradually increasing the dose, but it should not be more than 30 mg per day.
Electrical stimulation of the lower extremities
Physiotherapy is aimed at reducing swelling of the lower extremities, accelerating blood circulation and metabolic reactions. As a result, soft tissue trophism is normalized and neuromuscular conduction is restored.
For treatment use:
- Reflexology.
- Magnetotherapy.
- Massage.
- Electrical stimulation.
The duration of physiotherapy is determined by the attending physician based on the severity and type of pathology. As a rule, physiotherapy methods are used comprehensively, in courses.
Massage has a good effect in treating neuropathy. It helps restore some atrophic areas.

Massage should only be done in a hospital setting by a specialized specialist. Massaging your legs yourself is contraindicated, as this can not only reduce the effectiveness of therapy, but also significantly harm your health.
Exercise therapy for damage to nerve endings
To maintain limb mobility, if nerve endings are damaged, the patient is prescribed exercise therapy. With regular exercise, it is possible not only to develop atrophied muscles, but also to speed up blood circulation.
For therapeutic purposes, gymnastics is selected by a doctor, based on the patient’s health condition, severity and form of pathology.
Some sets of exercises can be performed at home, but you should first consult with a specialist.
More effective for restoring motor activity of the limb are classes on special simulators and water sessions.
The load must be selected taking into account the physical fitness and condition of the patient. The first sessions should be carried out with minimal stress, gradually increasing the load and duration of the workout. All exercises are performed smoothly and measuredly; you should not rush or make sudden movements.
Folk remedies
Salt foot baths
You can treat neuritis in children and adults using traditional methods, but under the supervision of a doctor.
There are many universal recipes that help improve neuromuscular conduction, eliminate pain and swelling.
- Drink made from eggs and honey. To prepare such a medicine, you need to mix one raw yolk with two tablespoons of olive oil. Beat everything thoroughly with a fork, add 100 ml of carrot juice and 2 teaspoons of fresh liquid honey. It is better to drink the drink in the morning and evening before meals.
- Saline solution. For half a bucket of warm water, take a glass of table salt and 9% table vinegar in the amount of 2/3 cup. You need to keep your feet in the resulting mixture for 20 minutes every day. The course of therapy is a month.
- Infusion of fenugreek and bay leaf. It is especially effective for patients whose neuropathy is caused by diabetes mellitus. It is advisable to use a thermos to prepare the infusion. Mix 1 tbsp. l. chopped bay leaf and 3 tbsp. l. fenugreek seeds. Pour boiling water over everything, leave for 2-3 hours, then strain. You need to drink the product in small portions throughout the day.

Before using folk remedies, you should not neglect a preliminary consultation with your doctor, so as not to provoke allergic reactions and not worsen the existing condition.
Causes of pathology
Neuropathy of the nerve of the anterior group of the leg muscles occurs due to the fact that it is compressed or damaged in a certain area. Because of this, the sensitivity of the ankle may weaken or disappear, and a person may have problems bending his fingers.
With neuropathy of the nerve of the posterior group of muscles, similar difficulties can be observed in the femoral and knee areas, depending on which area is damaged. Very often, this damage can occur in the area of the tarsal tunnel (then tarsal tunnel syndrome occurs). All this leads to disruption of the innervation of a certain area (ankle, ankle, sole, etc.).
Sometimes different types of nerves are damaged, resulting in polyneuropathy, in which adverse symptoms can affect different areas of the legs. In this case, the disease develops without inflammation of the nerve, in other words, it is non-inflammatory in nature.
Compression of a bundle of nerve fibers or destruction of a nerve connection can occur for various reasons. This:
- Injuries. The likelihood of developing this disease is especially high with injuries to areas of the leg where the nerves are close to the bones or lie close to the surface. When a fracture occurs, the tibia bones can be crushed, and their fragments damage the nerve. Blows, dislocations, sprains and other traumatic circumstances are also considered risky.
- Compression of a nerve in any part of it. For this reason, neuropathy of the tibial nerve develops especially often in people who, due to their type of employment, are forced to occupy one position for a long time.
- Weakened blood supply. Because of this, the nerve fibers do not receive the necessary nutrients and their functioning is impaired. The result may be ischemic neuritis of the peroneal nerve.
- Keeping your legs in the wrong position for a long time. This is especially dangerous when there is no movement. In this case, compression of the major or minor nerve may occur.
- Infectious diseases in severe form. This can damage many nerve connections.
- Intoxication. It can be caused by a serious illness (diabetes or kidney failure), substance abuse or drug abuse. Long-term exposure can cause destruction of nerve connections.
- Oncological diseases. Tumors and metastases form, which can also put pressure on the nerves.
- Swelling of the tissue in the area of the tarsal canal. This provokes tarsal tunnel syndrome.