Maxillary nerve branch
Rice.
1065. Connections of the nodes of the vagus and glossopharyngeal nerves with the sympathetic trunk and plexuses of the carotid arteries; right view (based on G. Oleinik’s preparations). Fig. 1054. Areas of distribution of cutaneous nerves of the lower limb, right (semi-schematic). (Anterior surface.) Maxillary nerve, n. maxillaris (see Fig. 972, 973, 974, 975, 976, 977, 1054, 1065), sensitive. After leaving the trigeminal ganglion and passing the cavernous sinus, the nerve leaves the cranial cavity through the foramen rotundum and enters the pterygopalatine fossa, where it divides into main branches.
Even before leaving the skull, the nerve gives off the (middle) meningeal branch, r. meningeus (medius), which branches in the dura mater of the brain along with the middle meningeal artery (see Fig. 972, 979).
In the pterygopalatine fossa the following branches arise from the maxillary nerve.
1. Infraorbital nerve, n. infraorbitalis (see Fig. 976, 977), is the most powerful of all branches of the maxillary nerve, which is, as it were, its direct continuation. From the pterygopalatine fossa, the nerve enters the orbital cavity through the inferior orbital fissure, runs in the infraorbital groove and, having passed the infraorbital canal, exits through the infraorbital foramen onto the anterior surface of the face in the area of the canine fossa and is divided into branches:
1) lower branches of the eyelids, rr. palpebrales inferiores, innervate the skin of the lower eyelid and the area of the corner of the eye;
2) external and internal nasal branches, rr. nasales externi et interni, numerous, innervate the skin of the lateral wall of the nose along its entire length, starting from the inner corner of the eye to the circumference of the opening of the nostril;
3) superior labial branches, rr. labiales superiores, directed to the skin and mucous membrane of the upper lip, gums and wings of the nose;
4) superior alveolar nerves, nn. alveolares superiores, along the path from the infraorbital nerve give branches to the teeth of the upper jaw:
- posterior superior alveolar branches, rr. aheolares superiores posteriores (see Fig. 974, 975), begin with 2-3 branches from the trunk of the infraorbital nerve even before it enters the lower orbital fissure, go to the tubercle of the upper jaw and, having entered the openings of the same name, pass through canals located in the thickness bones, to the roots of the three large molars of the upper jaw;
- middle superior alveolar branch, r. alveolaris superior medius, is a rather powerful trunk. It arises from the infraorbital nerve in the infraorbital groove. Heading down and forward, the nerve branches in the thickness of the outer wall of the maxillary sinus, anastomoses with the upper posterior and anterior alveolar nerves and approaches the small molars of the upper jaw;
- anterior superior alveolar branches, rr. aheolares superiores anteriores (see Fig. 973, 974), the most powerful. They arise in 1–3 branches from the infraorbital nerve almost before its exit through the infraorbital foramen. These branches pass through the anterior alveolar canals in the thickness of the anterior wall of the maxillary sinus and, heading slightly forward and downward, branch into several dental branches and the nasal branch. The first approach the incisors and canines of the upper jaw, and the second takes part in the innervation of the anterior section of the mucous membrane of the bottom of the nasal cavity.
The superior alveolar nerves connect with each other in the canaliculi of the alveolar process of the upper jaw and form the superior dental plexus, plexus dentalis superior. The branches of this plexus are called the superior dental and superior gingival rami, rr. dentales et gingivales superiores, are directed to the teeth and corresponding areas of the gums of the upper jaw.
2. Nodal branches, rr. ganglionares, are represented by 2-3 short thin nerves that approach the pterygopalatine ganglion, ganglion pterygopalatinum (see Fig. 979).
Some of the fibers of these nerves enter the node; others connect with branches extending from the pterygopalatine ganglion.
Branches of the pterygopalatine ganglion:
1) orbital branches, rr. orbitales;
2) medial and lateral superior posterior nasal branches, rr. nasales posteriores superiores mediales et laterales;
3) pharyngeal branch, r. pharyngeus;
4) greater palatine nerve, n. palatinus major;
5) small palatine nerves, nn. palatini minores (for a description of these nerves, see “Autonomic (autonomic) nervous system”).
3. Zygomatic nerve, n. zygomaticus, departs from the maxillary nerve in the region of the pterygopalatine fossa and, together with the infraorbital nerve, enters the orbit through the inferior orbital fissure, located on its outer wall. Along its course, the zygomatic nerve has a connecting branch with the lacrimal nerve (from the optic nerve), consisting of fibers extending from the pterygopalatine ganglion.
Subsequently, the zygomatic nerve enters the zygomatic orbital foramen and divides into two branches inside the zygomatic bone:
1) zygomaticofacial branch, r. zygomaticofacialis, emerges from the opening of the same name, ending in the skin of the cheek and lateral corner of the eye;
2) zygomaticotemporal branch, r. zygomaticotemporalis, also emerges from the opening of the same name and branches in the skin of the temple and lateral part of the forehead.
Both nerves are widely connected to the facial nerve by their terminal branches.
Anatomy of the nerves in the lower third of the face
The marginal mandibular nerve can be damaged during injection correction of the cheeks, jawline and neck. Caution must be exercised when injecting fillers into the midmandibular border, even with a cannula, as nerve damage may impair mobility.
In most cases, the marginal mandibular nerve passes anteriorly above the border of the mandible, but in 19% of cases it passes below this border. the cervical branch of the facial nerve is also at risk .
When correcting the neck, it is necessary to avoid introducing dermal fillers into the subplatysmal plane.
Chin augmentation requires a mental nerve . Care must be taken to avoid nerve damage, which can lead to loss of sensation in the front of the chin and lower lip. Equally careful injection of dermal fillers into the supraperiosteal plane is necessary.
Gasser Knot
GASSER KNOT
(ganglion Gasseri sg semilunare), gives rise to the sensitive root of n. trigemini; it is placed on the dorsal surface of the petrous part of the temporal bone, in a niche formed by the bifurcation of the durae matris (cavum Meckeli); on the bone there is a small depression in this place—impressio trigemini; the concave edge of the knot is facing backward, the convex edge is facing forward.
In G. u. there are a large number of round cells covered with a membrane formed from neuroglial cells, which passes directly into the Schwann sheath of the nerve fiber. Most of the cells of G. u. belongs to the pseudounipolar, equipped with only one process, which is divided in a T-shape; in some cells, before division, this process is very convoluted and forms a real glomerulus - glomerulus initialis, in others - a straight process; there are cells and multi-processed, fenestrated; some processes do not extend beyond the node.
The peripheral processes of the cells form three large branches: n. ophthalmicus (ophthalmic nerve), n. maxillaris (maxillary) and n. mandibularis (mandibular); these three branches emerge from the convex edge of the node (see figure).
The central process forms the root of n. trigemini, very large, consisting of 50 bundles, included with. motor root in the Varoliev bridge (peripheral branching, central course of fibers" and -induced gy-
Right Gasser knot (according to Spalteholz): 1—p.
opticus;
a
-art.
carotis int.; 3
- p.
oculomotorius; 4—
n. troehlearis;
5—p. abducens; e-n. trige-minus; 7
- p.
facialis and acusticus; a-n. ophthalmicus; 9
—p.
maxillaris; lo
-p. mandibularis; L—ganglion Gasseri.
Diagnostics
There are several strict criteria for diagnosing neuralgia in international practice:
- Paroxysmal attacks lasting from a fraction of a second to a minute affect one or more branches of the nerve.
- The pain is intense, sharp, stabbing or superficial, and begins from trigger zones - areas in the projection of the face.
- Attacks lead to stereotypical pain in a particular patient.
- There is no significant neurological deficit - motor or sensory.
- The patient has no history of other nervous system disorders.
Laboratory, electrophysiological or x-ray studies are rarely used for diagnosis, since examination and questioning of the patient is sufficient. An MRI is required to rule out other causes of pain, such as acoustic neuroma.
Branches of the trigeminal nerve: ophthalmic and maxillary nerves
Infraorbital nerve, n. infraorbitalis
, is the most powerful of all branches of the maxillary nerve, which is, as it were, its direct continuation. From the pterygopalatine fossa, the nerve enters the orbital cavity through the inferior orbital fissure, runs in the infraorbital groove and, having passed the infraorbital canal, exits through the infraorbital foramen onto the anterior surface of the face in the area of the canine fossa and divides into branches:
1) lower branches of the eyelids, rr.
palpebrales inferiores, innervate the skin of the lower eyelid and the area of the corner of the eye;
2) external and internal nasal branches, rr. nasales externi et interni
, numerous, innervate the skin of the lateral wall of the nose along its entire length, starting from the inner corner of the eye to the circumference of the opening of the nostril;
3) superior labial branches, rr. labiales superiores
, are directed to the skin and mucous membrane of the upper lip, gums and wings of the nose;
4) superior alveolar nerves, nn.
alveolares superiores, along the path from the infraorbital nerve give branches to the teeth of the upper jaw:
a) posterior superior alveolar branches, rr. alveolares superiores posteriores
, begin with 2-3 branches from the trunk of the infraorbital nerve even before it enters the lower orbital fissure, go to the tubercle of the upper jaw and, entering the openings of the same name, pass through canals located in the thickness of the bone to the roots of the three large molars of the upper jaw;
b) middle superior alveolar branch, r.
alveolaris superior medius, is a rather powerful trunk. It arises from the infraorbital nerve in the infraorbital groove. Heading down and forward, the nerve branches in the thickness of the outer wall of the maxillary sinus, anastomoses with the upper posterior and anterior alveolar nerves and approaches the small molars of the upper jaw;
c) anterior superior alveolar branches, rr.
alveolares superiores anteriores, the most powerful. They arise in 1-3 branches from the infraorbital nerve almost before its exit through the infraorbital foramen. These branches pass through the anterior alveolar canals in the thickness of the anterior wall of the maxillary sinus and, heading slightly forward and downward, branch into several dental branches and the nasal branch.
The first approach the incisors and canines of the upper jaw, and the second takes part in the innervation of the anterior section of the mucous membrane of the bottom of the nasal cavity.
Anatomy of the nerves in the cheek area
The location of the infraorbital foramen in the cheek area is critical to prevent neuropraxia. Damage may occur due to an infraorbital nerve . Fortunately, most fillers include lidocaine, which reduces the need for n. infaorbitalis in this zone. However, such anesthesia may be necessary for upper lip augmentation. Injecting an anesthetic into the eye socket, as well as too strong massage after injection of filler, can lead to:
- diplopia;
- dysesthesia;
- paresthesia.
There are known cases of Bell's palsy after injections of dermal fillers. In most patients, improvement occurs spontaneously (71%), but in a fairly large percentage of victims, residual weakness of one half of the face persists for life.
You may also be interested in: First aid for central retinal artery occlusion after filler injections
Emergency treatment for Bell's palsy is a short course of oral steroids. Surgical decompression and other treatments such as electrography, physical therapy and acupuncture are not supported by sufficient evidence.
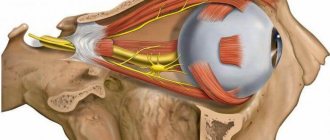
IV pair of cranial nerves - trochlear nerve (n. Trochlearis)
The superior alveolar nerves connect with each other in the canaliculi of the alveolar process of the upper jaw and form the superior dental plexus, plexus dentalis superior
.
The branches of this plexus are called the superior dental and superior gingival rami, rr. dentales et gingivales superiores,
are directed to the teeth and corresponding areas of the gums of the upper jaw.
Nodal branches, rr. ganglionares,
are represented by 2-3 short thin nerves that approach the pterygopalatine ganglion, ganglion pterygopalatinum.
Some of the fibers of these nerves enter the node; others connect with branches extending from the pterygopalatine ganglion.
Branches of the pterygopalatine ganglion:
1) orbital branches, rr. orbitales;
2) medial and lateral superior posterior nasal branches, rr. nasales posteriores superiores mediates et laterales;
3) pharyngeal branch, r.
pharyngeus;
4) greater palatine nerve, n. palatinus major;
5) small palatine nerves, nn. palatini minores
Zygomatic nerve, n. zygomaticus
, departs from the maxillary nerve in the region of the pterygopalatine fossa and, together with the infraorbital nerve, enters the orbit through the inferior orbital fissure, located on its outer wall.
Along its course, the zygomatic nerve has a connecting branch with the lacrimal nerve (from the optic nerve), consisting of fibers extending from the pterygopalatine ganglion.
Subsequently, the zygomatic nerve enters the zygomatic orbital foramen and divides into two branches inside the zygomatic bone:
1) zygomaticofacial branch, r.
zygomaticofacialis, emerges from the opening of the same name, ending in the skin of the cheek and lateral corner of the eye;
2) zygomaticotemporal branch, r. zygomaticotemporalis,
also emerges from the opening of the same name and branches in the skin of the temple and lateral part of the forehead.
Both nerves are widely connected to the facial nerve by their terminal branches.
Anatomy of nerves in the temporal region
In the context of injection facial correction, it is customary to distinguish several planes. For contouring, the technique most often used is to inject fillers into the space between the temporalis muscle and the bone of the temporal fossa . Injecting the drug into the specified plane in the superomedial area of the temple minimizes the risk of vascular complications, as well as damage to the zygomaticotemporal nerve.
Rice. 1: facial nerves and deep fat compartments
Fillers are also injected:
- between the superficial and deep layers of the deep temporal fascia.
- between the deep temporalis fascia and the temporalis muscle.
For patients with severe volume deficit in this area, filler is injected into the space between the superficial temporal fascia and the deep temporal fascia . Here the doctor works only with a cannula - this reduces the risk of damage:
- superficial temporal artery and vein;
- frontal branch of the facial nerve.
To prevent damage to neurovascular structures in this plane, the author uses a 22-gauge cannula.
Supraorbital neuralgia
Introduction to Supraorbital Neuralgia
The supraorbital nerve is the distal branch of the first branch of the trigeminal nerve, which is the smaller one. Supraorbital neuralgia refers to persistent or paroxysmal pain in the distribution of the supraorbital nerve (forehead).
Supraorbital neuralgia often presents as intermittent or bilateral posterior, periorbital, unexplained burning or dull pain.
There is obvious pain in the upper part of the incision, but the eyeball and its appendages do not have organic lesions, which are common diseases of ophthalmology.
The onset of the disease is more acute, manifesting as paroxysmal or persistent acupuncture pain or burning sensation on one or both sides of the forehead, and may also be accompanied by paroxysmal exacerbation in case of persistent pain. There is tenderness in the superior incision, and the area of distribution of the supraorbital nerve (forehead) has scaly hyperalgesia or is reduced.
Basic knowledge
Disease share: 0.01%
Susceptible people: no defined population
Mode of infection: non-infectious
Complications: muscle atrophy, bacterial infection
pathogen
Cause of supraorbital neuralgia
It is associated with colds, colds, trauma, etc. Since the supraorbital nerve is the distal branch of the first division of the trigeminal nerve, it is more superficial, so it is easy to affect. The onset is more acute, which manifests itself in the form of one or both sides of the paroxysmal forehead area.
Or persistent acupuncture-like pain or a burning sensation may also be accompanied by paroxysmal exacerbation in the case of persistent pain.
The body can see that there is tenderness in the superior sacral nerve at the exit of the supraorbital nerve, and the area of distribution of the supraorbital nerve (anterior edge) is scaly. Hyperalgesia or loss.
prevention
Prevention of supraorbital neuralgia
1. Mental stimulation. If mental stimulation can cause supraorbital neuralgia, then not all stimuli will cause the disease to occur. The most important cause of supraorbital neuralgia is mental stimulation.
Many patients suffer from emotions or moods. They are becoming more attractive every day.
Over time, they will develop liver congestion and anger, and the liver will become energetic, causing supraorbital neuralgia to occur.
2. The pain trigger point is not protected. Supraorbital neuralgia is a trigger point for pain. Patients should protect their body's trigger points. About 50% of patients have several or one sensitive trigger point around the eyelids.
To in turn cause a painful episode that is involved in the body.
These trigger points are mainly found on the lips, nose, face, mouth, tongue or corner of the eye, so the patient should try to protect the trigger point during the illness.
3, pay attention to avoid cold, overwork, mental stimulation. Antipyretic analgesics can be used for pain relief and Chinese medicine treatment.
complication
Complications of supraorbital neuropathy Complications, muscle atrophy, bacterial infection
Intracranial infection is a common complication in the treatment of supraorbital neuralgia, which causes severe intracranial infection during craniotomy or radiofrequency therapy.
Patients with supraorbital neuralgia have a mostly acute onset, and some symptoms of supraorbital neuralgia are insidious attacks. According to the medical history, the clinical manifestations are varied.
The onset of supraorbital neuralgia may cause the ipsilateral mastication muscle, masseter muscle, diaphragm, pterygoid muscle, and spermatozoon muscle to affect masticatory movements.
Eating does not deliberately fall on the affected side of supraorbital neuralgia and runny nose. And other phenomena, severe supraorbital neuralgia, can cause neuromuscular atrophy affecting appearance.
symptom
Symptoms of supraorbital neuralgia General symptoms Constant pain in the eyelids in the eyelids, ... facial pain, neuralgia, headache in the forehead, acupuncture in the forehead or burning sensation
//www.youtube.com/watch?v=Oqi9Kf4F6Oo
The onset is more acute, manifesting as paroxysmal or constant acupuncture pain or a burning sensation on one or both sides of the forehead, and may also be accompanied by a paroxysmal exacerbation in case of persistent pain. The notch is tender, and the area of distribution of the supraorbital nerve (forehead) has scaly hyperalgesia or is reduced.
research
Examination of supraorbital neuralgia
1. Laboratory examination is of auxiliary value for clinical diagnosis.
2. Evoked potentials.
3. Head CT and MRI.
diagnostics
Diagnosis and differentiation of supraorbital neuralgia
diagnostics
Based on symptoms and signs, a diagnosis can be made.
Differential diagnosis
It is necessary to pay attention to identifying sinusitis and trigeminal neuralgia.
Source: //www.healthfrom.com/ru/disease/h-2354.html