More and more patients are being diagnosed with stress urinary incontinence, in which a person is unable to control urination. The deviation appears both temporarily and permanently, causing discomfort to the patient. The disease develops for various reasons, one of which is stress. Women are especially at risk of getting the disease after childbirth. In men, involuntary urination appears after surgery for prostate diseases, in particular after removal of cancer.
Symptoms of stress urinary incontinence
The only symptom of this disease is leakage of urine during physical exertion, such as laughing, sneezing, coughing, running, sexual intercourse, etc. As a result of an increase in intra-abdominal pressure, anything from a few drops of urine to a fairly noticeable amount can leak out.
With regular use of sanitary pads, a few drops of urine may go unnoticed, but over time the disease progresses and becomes a real problem. Women refuse sexual activity and, trying to avoid situations that provoke urinary incontinence, are afraid to visit places of entertainment, public places, and go on visits. In this state of affairs, the development of neuroses and depressive states is possible.
Acute and then chronic cystitis often develops as a complication.
Diagnosis of the disease
The patient must share his complaints regarding his health condition. Thanks to this, the urologist can assess what stage the disease is at.
The set of diagnostic measures includes:
- Urinary incontinence in men. What types of this disease are there and how is it treated?
- Anamnesis collection. Information is collected about the patient's living conditions. It is important for the doctor to determine the frequency of hygiene procedures. Relatives may be asked about their urinary history.
- Filling out questionnaires. The most effective are ICIQ-SF, ICSmaleSF, UCLA PCI–incontinencesection, I-QOL, SEAPI-QMM. In them, the patient shares his impressions of life with the problem of urinary incontinence. Describes discomfort in detail.
- Inspection. First, a routine examination is carried out, followed by a urological examination.
- Keeping a urine diary. The patient records all trips to the toilet. Controlled processes are also taken into account. Thanks to the diary, the daily volume of urine is determined. The ratio of daytime and nighttime trips to the toilet is calculated.
- Daily PAD test. Another name is the insert test. Allows you to accurately determine the amount of urine loss per day. The mild form is defined as 3 pads in 24 hours, the moderate form is 4-6, the severe form is 7 or more.
- Urine and blood analysis. Makes it possible to identify a wide range of pathologies.
- Ultrasound. This is especially true for women. An examination of the pelvic organs and kidneys is carried out.
- X-ray studies. Urethrocystography is needed to identify urethral stricture. To see all the stages of urine passing through the organs of the urinary apparatus, cystography is used. Neighboring organs are also examined.
- Endoscopic examinations. Urethrocystoscopy is most effective. Mucus collects from the urethra and bladder. It is examined, after which an expert assessment of the vesicourethral junction is given.
- Urodynamic examination. Presented in the form of uroflowmetry, profilometry, cystometry, press-flow, sphincterometry. This study allows you to determine the capacity and distensibility of the bladder. The characteristics of uncontrolled contractions of the urinary organs in the phase of urine accumulation are provided. The speed and detrusive pressure are recorded.
Carrying out such a set of works will help to find out the nature of the disease and its current phase. The type of disease is determined, because patients often confuse the urgent form with the stressful form. After this, complex treatment is prescribed.
Causes of stress urinary incontinence in women
Urine leakage occurs as a result of intra-abdominal pressure, which normally does not occur. The reason lies in the weakening of the pelvic floor muscles and the ability of the urethra to resist the pressure of fluid in the bladder.
Factors leading to such a weakening may include:
- Difficult or multiple births;
- Heavy physical activity in sports or at work;
- Anomalies in the development of the pelvic muscles and urethra;
- Damage to the perineum as a result of trauma;
- Violation of the innervation of the pelvic floor muscles;
- Scars after operations on the pelvic organs.
As a result of “sagging” of the pelvic floor muscles, the relative position of the bladder and urethra changes, which disrupts the natural mechanisms of urinary continence.
Causes
Pathology occurs due to the fact that the urethra or neck of the bladder becomes mobile and takes an incorrect anatomical position during tension. This happens if there is prolapse of the pelvic organs. In addition, dysfunction of the sphincters leads to problems both in women and causes stress urinary incontinence in men.
It should be said that the problem is more common in women due to the following reasons:
- long complicated labor;
- labor too fast;
- operations;
- excessive physical labor;
- injuries to the perineal area.
Treatment of stress urinary incontinence
There is currently no drug treatment for this pathological condition, that is, stress urinary incontinence cannot be cured with injections and tablets.
Conservative treatment
However, conservative methods of treating mild degrees of incontinence exist, these are physiotherapeutic procedures (electrical stimulation of the pelvic floor muscles), special exercise therapy complexes, and the most modern method of treatment - the biofeedback method.
The pelvic floor muscles belong to the skeletal muscles, which means we can control their contractions at our discretion. At the same time, normally we do not think about when and with what force to strain these muscles, and if we draw an analogy, then while walking we also do not send mental commands to the muscle groups participating in it. We simply go in the right direction, and the motor centers of the brain take over control of the coordinated contraction of muscle fibers. This happens normally, but if a person recovers from an injury, then he has to learn to walk again, which means that conscious control and coordination of movements comes first.
The situation is similar with the pelvic muscles, which, as a result of disease, multiple births or injuries, are out of control of the nervous system, so the main goal of treatment is to regain this control. The biofeedback method copes with this task more effectively than physical therapy complexes.
The treatment is carried out using the Urostim device, which allows, while controlling the pelvic floor muscles, to simultaneously control visual images on a computer monitor, that is, it is very reminiscent of a computer game, but instead of a joystick or mouse, the perineal muscles are used. Ultimately, muscle contractions become automatic and volitional efforts are no longer required. The biofeedback method has proven itself well in combination with electrical stimulation.
What are the causes of the disease?
The main reason for the involuntary release of urine is weakness of the pelvic muscles. Problems with the bladder sphincter may also occur.
During pregnancy and childbirth, the pelvic floor muscles can weaken, leading to incontinence. Additional factors are hormonal imbalances, weight gain, and pressure from the baby on the pelvic floor.
Also, the development of pathology can be affected by the high weight of the child and the use of auxiliary instruments during childbirth. The disease often affects older women after menopause.
Stressful involuntary discharge can also occur under the influence of the following factors:
- presence of bad habits;
- excess weight;
- heredity;
- diseases of the nervous system;
- stomach upsets;
- anemia;
- persistent cough;
- surgeries and back injuries.
Any surgical intervention in the bladder area leads to the formation of adhesions, which puts pressure on the pelvis. The influence of several factors together gives a greater likelihood of developing incontinence. Usually, the development of pathology is influenced by several reasons at once.
The occurrence of involuntary urination affects a woman’s daily life. She is afraid to appear in public with a lot of people, as the fear of wetting herself is always present. A person cannot play sports, as physical activity leads to urine leakage.
The disease brings a lot of inconvenience, so it is better to get rid of it as soon as possible. There is no need to be embarrassed to consult a doctor, since a problem solved in time will help get rid of the patient’s psychological problems and nervous disorders.
Treatment of urinary incontinence syndrome at the Es Clinic MC
There are two main methods: surgical and non-surgical, from which treatment begins. The latter method of therapy includes the prescription of special exercises, the purpose of which is to strengthen the pelvic muscles. Achieving the same result is pursued by resorting to electrical stimulation, writing prescriptions for medications, and using vaginal cones. Only in case of failure should one turn to surgical treatment.
Treatment of involuntary urine leakage using a laser at Es Clinic
Unique European equipment, created in accordance with the latest technological developments, makes laser treatment the most effective, simple and reliable. The anterior wall of the vagina, together with the end of the urinary canal, is exposed to the laser.
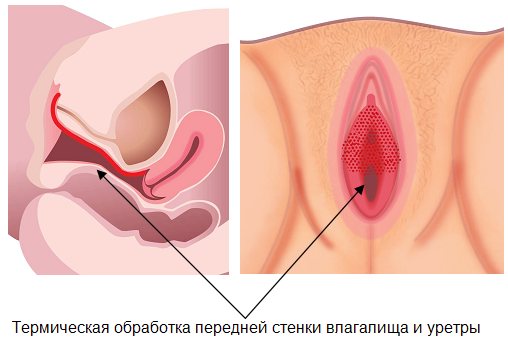
The impulses act gently on tissues without disturbing their structure. The heated tissues shrink, contract, and the active production of its own collagen starts. All this leads to increased firmness, elasticity, rejuvenation, and the result is a reduction in the symptoms of the syndrome.
Healing procedures
Treatment of stress urinary incontinence in women is carried out in different ways: conservative or surgical. The method by which therapy is carried out is chosen by the doctor. It depends on the results of the examination, the severity of the disease, and the individual characteristics of the body.
Conservative therapy consists of using medications (antispasmodics, antidepressants) in combination with performing a specially designed set of Kegel exercises. Exercise strengthens the pelvic muscles. The patient is advised to lead an active lifestyle; if he is obese, he is advised to lose weight.

In addition, the patient is advised to undergo bladder training. The principle of the procedure is for a person to gradually increase the time interval between urinations. Indeed, during the development of the disease, patients empty the bladder at the slightest load on it, fearing uncontrolled leakage of urine. During training, an individual urination plan is drawn up, and if the urge occurs outside of the routine, the patient must restrain it, squeezing the sphincter as much as possible.
Every six months, it is recommended to increase the interval between trips to the toilet by 30 minutes, bringing the time between urination to 3-4 hours.
The pelvic muscles are trained using the feedback method. Muscle training is carried out using the Urostym device 1–2 times a week. Systematic exercises on the simulator allow the patient to train the pelvic muscles and control urination. At the beginning of classes, patients mentally transmit the command to their muscles to contract, but after 2 months of training, the process occurs automatically. Along with biofeedback therapy, electrical stimulation of the muscles of the pelvic organs is performed. The technique restores the transmission of nerve impulses to muscle tissue.
If conservative treatment cannot help the patient, its effectiveness is low, surgery is performed. Collagen injections treat stress incontinence in the absence of a neurogenic factor. But the procedure cannot be performed when there is prolapse of the bladder or vagina.
Sling surgery is also often used. During the process, a synthetic loop is installed to prevent unwanted urination. The use of anterior colporrhaphy is considered ineffective in the treatment of incontinence. It is used for suturing the prolapsed vaginal wall.
Another type of operation is laparoscopic colposuspension. This is a low-traumatic surgical method aimed at restoring the normal position of the urethra and fixing it. This intervention does not cause complications and does not require long-term postoperative rehabilitation.
Contraindications
- Pregnancy, breastfeeding or immediately after childbirth
- Diabetes
- Oncology
- Age restrictions - up to 80 years
The procedure is performed on an outpatient basis. There is simply no rehabilitation period, which is undoubtedly a plus. Complete victory over the disease is noted in more than 70% of cases.
Mini-sling for the treatment of urinary incontinence at the Es Clinic MC
A type of surgery in which a braided tape (sling) is placed under the urethra. The material – prolene, which has excellent supporting properties, allows you to fix the urethra and eliminate excessive mobility. The tape is inserted after three small punctures (under the urethra, in the groin area). They are sutured with material that subsequently dissolves without leaving any traces.
Prolene, used in slings, does not dissolve over time and does not cause inflammation or allergies. The size of the pores in the weave of the tape allows connective tissue cells to pass through, the fibroblasts of which produce scaffold protein. Later, the implant will be overgrown with connective fibers that strengthen the urinary canal and retain urine even under strong pressure in the bladder. In this regard, final recovery may occur a maximum of six months after the procedure.
Professional specialists at Es Clinic will deal with your troubles and return you to your normal life!
With abbreviations(definition, factors, treatment)
Full version:
Trukhan D.I., Viktorova I.A. Diseases of the kidneys and urinary tract. – Omsk, 2009. – 104 p. – pp. 12-19.
Definition and epidemiology.
Stress urinary incontinence (SUI) is sudden urination due to activities that increase intra-abdominal pressure. Significant physical or psychological stress, coughing, are typical situations that can cause stress urinary incontinence. Urinary incontinence is a functional disorder that has a serious impact on the quality of life of patients. About 40% of women after 40 years of age and about half after 60 years of age suffer from stress urinary incontinence. Most people with urinary incontinence are embarrassed to seek medical help. According to studies, only 25% of women tell their doctor about their problem, and it often takes 9 to 12 years from the first symptoms to seek help.
In the Russian Federation, symptoms of urinary incontinence were noted by 36.8% of women surveyed (D.Yu. Pushkar, 1996).
The EPINCONT study (28,000 women over 20 years of age) showed an increase in the incidence of urinary incontinence among young women (20-30%), a clear increase in the incidence of urinary incontinence in middle age (30-40%), and a stable increase in the incidence of urinary incontinence in older women ( 30-50%). Etiology and pathogenesis
Function of urination in women
is under the control of estrogen. A decrease in estrogen levels during menopause leads to atrophy (thinning) of the submucosal layer of the bladder neck and urethra and its replacement with fibrous tissue. A decrease in estrogen is a risk factor for the development of urinary incontinence.
Other causes that lead to this are weakness of the pelvic floor muscles and prolapse of the pelvic organs (bladder, uterus and rectum), which occur after frequent childbirth or intense physical activity, and also associated with age-related changes. The weakening of the pelvic floor muscles can be caused by: trauma to the perineum; disorders of the nervous control of the pelvic floor muscles, often occurring in women who smoke, drink alcohol and have diabetes.
It is an undeniable fact that in most cases women who have given birth get sick. It has now been proven that in the development of the disease, the main role is played not by the number, but by the nature of childbirth. More often, urinary incontinence affects women who have undergone pathological childbirth, accompanied by ruptures of the pelvic floor muscles, perineum and genitourinary diaphragm.
Stress urinary incontinence can also be caused by injuries and congenital anomalies of the pelvis and urethra, as well as the consequences of surgical interventions on the pelvic organs. In general, there are four groups of risk factors
.
1. Predisposing factors increase the risk of developing urinary incontinence when precipitating factors exist. Sometimes, only predisposing factors are sufficient for the occurrence of SUI. These include family history, gender, race; anatomical, neurological and muscular disorders.
Family predisposition
– genetic factors play a role in the occurrence of urinary incontinence. Women whose mother or older sister complains of urinary incontinence are at high risk of developing stress or mixed urinary incontinence. The risk of developing urinary incontinence is even higher in women who know that their mother and grandmother had incontinence.
Floor.
The incidence of urinary incontinence, especially SUI, is significantly higher in women than in men. At the age of 60, urinary incontinence in women is 1.5-2 times more common than in men, and at a younger age it is 7 times more common. The main cause of SUI in men is removal of the prostate gland due to its hyperplasia or cancer.
2. Stimulating factors can cause SUI due to the fact that these factors lead to significant disturbances in the mechanism of urinary continence. These include pregnancy and childbirth, surgery on the pelvic organs (radical hysterectomy, radical surgery for rectal cancer, vaginal surgery with wide tissue dissection) and radiation therapy to this area.
3. Provoking factors contribute to the development of SUI, usually after prolonged exposure. These factors include urinary tract infection, obesity, constipation, respiratory diseases and smoking (chronic cough), neurological diseases, occupational factors and sports, menopause, certain groups of medications (diuretics, alpha-blockers, etc.).
4. Decompensating factors acting over a certain period of time or constantly can cause SUI, sometimes even without disruption of the mechanism of urinary continence. Decompensating factors can shift the “continence-incontinence” balance towards urinary incontinence in the presence of predisposing, stimulating and provoking factors. These factors include age, dementia and debility (mental disorders), concomitant diseases and motor dysfunction, and living conditions. The most studied and proven factors include age, pregnancy and childbirth, and obesity.
Normally, the maximum pressure in the urethra should exceed the pressure inside the bladder at all times, with the exception of the process of urination. With stress incontinence (during coughing, laughing, physical activity), intra-abdominal and intravesical pressure increases - it becomes higher than the pressure in the urethra, which remains open due to weakening of the sphincter, and urine loss occurs. In the pathogenesis of stress incontinence, displacement or dislocation of the proximal urethra and urethrovesical segment is important. In other words, the development of symptoms of this disease is impossible without the occurrence of disturbances in the anatomical relationships of the pelvic organs.
A number of authors divide SNM into two
main pathogenetic variants:
- the first, associated with dislocation and weakening of the ligamentous apparatus, unchanged urethra and urethrovesical segment, which refers to anatomical urinary incontinence;
- the second, associated with changes in the urethra itself and the sphincter system, leading to disruption of the function of the closure apparatus.
Clinic
Main complaint of patients
is the involuntary release of urine during physical exertion and the preserved physiological act of urination.
Depending on the degree of damage to the closing apparatus of the bladder, the degree of urinary incontinence can vary - from a few drops to almost complete emptying of the bladder at the slightest movement. This disease often brings severe suffering to the young contingent of patients. The constant smell of decomposing urine and concomitant skin diseases often affect the psyche of patients, leading to their social maladjustment. Differential diagnosis
Stress urinary incontinence can be considered when
Anamnesis data, complaints and identified symptoms indicate loss of urine during physical activity, without accompanying urgent symptoms (normal frequency of daytime and nighttime urination, lack of urgency due to provoking factors - “hand washing”).
The diagnosis is confirmed by a positive cough test, urodynamic confirmation of involuntary loss of urine with increased intra-abdominal pressure and the absence of involuntary detrusor contractions. Treatment
There are three types of treatment
stress urinary incontinence:
- conservative;
- pharmacological;
- surgical.
Conservative treatment
SNM consists of changing life patterns (weight loss, stopping smoking, limiting coffee consumption), regular bowel movements, treatment of pulmonary diseases, exercises for the perineal muscles and other types of treatment that can improve the functional state of the pelvic floor muscles.
Bladder training is necessary, which consists of gradually lengthening the time intervals between urinations. Conservative treatment methods should be preferred in elderly patients who have previously been operated without effect, as well as in young women with mild symptoms of SUI that arose after childbirth.
Gymnastic exercises
are aimed primarily at strengthening the sphincters of the bladder and rectum. They also have a stimulating effect on the abdominal muscles, pelvic organs and perineum, reducing the vesicourethral angle. As a result, normal anatomical relationships between the bladder neck, urethra and pubic symphysis are restored. There are a number of proprietary methods: physical therapy according to D.N. Atabekov, gymnastics according to F.A. Yunusov, N. Kegel exercises.
Mechanical methods.
Mechanical elimination of the anatomical cause supporting SUI. Previously, various types of pessaries, the action of which is based on mechanical compression of the urethra, were widely used to eliminate the symptoms of UIPN. Currently, special endourethral obturators are widely used, creating an obstacle to the involuntary release of urine. The patient is taught how to insert an obturator into the urethra, and subsequently, on an outpatient basis, she uses them independently, removing them before the next voluntary urination.
A special set of exercises has been developed using so-called vaginal cones of varying weights. The patient holds the cone with the vaginal muscles for a certain time, moving from lighter to heavier, thereby strengthening the muscles of the genitourinary diaphragm. The use of vaginal cones is limited due to possible side effects (discomfort, colpitis, vaginal bleeding).
Biofeedback method (BFB).
The principle of biofeedback is based on the effect of reflex inhibition of detrusor contractions during voluntary and sufficiently strong contractions of the perineum. The idea of biofeedback is to receive a visual or auditory signal from a sensor inserted into the vagina or rectum about the state of the pelvic floor muscles. With this method, the patient learns to contract and relax the muscles of the perineum and, thus, improve the mechanism of urinary continence.
Physiotherapy.
Various methods of physiotherapeutic influence normalize the function of the bladder closure apparatus: vibration massage, diadynamic and galvanic currents, amplipulse, electrophoresis.
Electrical stimulation of the pelvic floor muscles
indicated for patients who are unable to independently perform the above exercises. Several different types of electrical stimulation are known: perineal, vaginal, anal, sacral. The mechanism of action of this type of treatment includes indirect stimulation of the pelvic floor muscles through the branches of the pudendal nerve.
Pharmacological treatment.
Urinary incontinence that occurs during menopause or menopause is, in some cases, successfully treated with hormone replacement therapy.
[td]
Medicines can slow down the contraction of the bladder walls, cause the sphincter to contract, or reduce urine production. The greatest effect can be achieved when combined with hormonal therapy. It must be emphasized that of the large number of drugs proposed for the treatment of urinary incontinence, only the prescription of drugs with anticholinergic activity (trospium chloride, oxybutynin) is pathogenetically justified.
The remaining drugs belonging to various pharmacological groups have only an indirect effect on the lower urinary tract, and the effect of some of them is their side effect (picamilon, imipramine, baclofen, diclofenac, ephedrine, profenide).
Correction of drug therapy.
There are a number of medications that promote frequent urination by relaxing the muscles of the pelvic organs in such a way that a person ceases to control the act of urination. These may include diuretics, antidepressants, sedatives, some blood pressure medications, and antihistamines. In older people, these drugs are more likely to cause urinary incontinence.
Surgery.
The goal of surgical treatment of SUI is to restore normal anatomical relationships of the pelvis and lower urinary tract. In case of dislocation of the normal urethrovesical segment and the proximal part of the urethra, the main goal of surgical treatment is to restore altered topographic-anatomical relationships by moving and fixing the urethrovesical segment in a normal anatomical position (various options for urethrocystocervicopexy).
If the urethra and bladder neck do not function more like a sphincter and are often represented by a rigid tube and a scar-changed urethrovesical segment, then patients need to form additional support for the urethra and bladder neck, as well as to create passive urinary continence by compressing the urethra, since sphincter function in these patients is completely lost (various modifications of sling or loop operations). The technique of classic sling surgery involves passing a loop under the urethra or bladder neck and fixing it to the aponeurosis of the rectus abdominis muscles or to the pubic bones, which allows “stabilizing” the urethra.
Last time
So-called minimally invasive interventions aimed at correcting SUI and having certain advantages over traditional operations (local anesthesia, short duration of surgery, good tolerability, short rehabilitation period, better functional results) are becoming increasingly popular. These include: the Ulmsten operation (TVT technique), laparoscopic interventions, paraurethral collagen injections and implantation of microballoons, devices for bone fixation of the urethrovesical segment.
Most Popular
from this group of operations - the so-called free synthetic loop (TVT) - is indicated for women with stress urinary incontinence due to urethral hypermobility.
Surgical methods of treatment provide immediate results after surgery, however, there are possible complications that need to be discussed with the patient before surgical treatment. Assessment of various types of stress urinary incontinence should be based on subjective and objective data and include long-term follow-up (more than 2 years). Prognosis
The final criterion is positive
The result of surgical treatment of SUI is the restoration of adequate urination, the absence of residual urine and signs of relapse of the underlying disease.
Despite significant successes in the surgical treatment of stress urinary incontinence, from 10 to 30% of surgical interventions do not lead to the elimination of incontinence. Complications of operations include sexual dysfunction (in approximately 20% of cases after sling operations, patients experience discomfort during sexual activity during the first 4 months and in 5% of cases - within 1 year).
Tell/Share:
Overflow incontinence
Who does it happen to? Mainly in older men who have prostate adenoma or cancer. In women, this type of urinary incontinence is much less common.
How it manifests itself. In advanced cases of urinary incontinence, with frequent urges to go to the toilet, urine is released literally drop by drop. Residual urine begins to accumulate in the bladder, which is retained in the kidneys and provides a breeding ground for infection. And in especially severe cases, it can lead to kidney failure and even death of the patient.
Why does it arise? An annoying leak in this case is associated with overfilling and overstretching of the bladder due to long-term obstructions to the outflow of urine, for example due to prostate adenoma - a benign tumor of the prostate gland, which begins to compress the urethra, which prevents the outflow of urine from the bladder. In women, the cause of overflow incontinence usually remains unclear. Except for those cases when it comes to diabetes mellitus, in which there is a violation of the innervation of the bladder or neurological diseases (spinal injuries).
How to treat it. The main method of dealing with overflow incontinence is to eliminate the cause that led to it. The main thing is not to lead the situation to kidney failure.

The kidneys can't cope. What leads to disruption of their functions? More details