- What is epilepsy and how often does it occur in children?
- Classification of the disease
- What causes epilepsy in children?
- Symptoms in newborns, infants and older children
- Examinations and tests
- First aid during an attack
- Basics and rules of treatment General recommendations and care
- Drug treatment
- Surgical intervention
What is epilepsy and how often does it occur in children?
Epilepsy is a serious psychological disorder that begins at a neurotic level when a pathological electrical voltage occurs in a part of the brain, causing seizures and short-term loss of consciousness. But if left untreated, the disease can progress to a psychotic level when a change in the patient’s personality occurs.
The disease occurs in most cases among children, but in children it is best treated. In almost ¾ of cases it is possible to completely recover from the disorder.
The onset of the disease mainly occurs in adolescents between 11 and 15 years of age. In almost 20% of cases, the onset occurs in schoolchildren aged 6 to 10 years. And the disease most rarely appears in children of primary school age, preschool age and infancy.
Did you know? Scientists have proven that listening to Mozart's compositions reduces the frequency and intensity of epileptic seizures in children.
The most interesting thing is that the works of other classics do not have the same effect.
Main manifestations
The key manifestation of epilepsy is a variety of seizures, which can be combined with each other or exist in isolation. They are convulsive (accompanied by uncontrolled paroxysmal activity of skeletal muscles) and non-convulsive, focal and generalized.
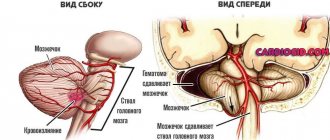
Often the development of an attack is preceded by an aura. And with a series of seizures following each other with generalization, they speak of the development of status epilepticus, which is fraught with the development of cerebral edema.

Seizures
With idiopathic epilepsy, seizures of any type may occur. But the predominance of one of them or the characteristic transformation of different species into each other makes it possible to differentiate the forms of the disease.
The main types of seizures include:
- Generalized classic “grand” tonic-clonic seizures and their variants, with a predominance of one of the phases.
- Absence seizures, which also belong to generalized seizures. They can be simple with autonomic disorders and freezing, or complex (with automatisms of various types, orofacial myoclonus, atony, eye rolling, etc.).
- Partial or focal seizures were previously called “minor” seizures. There are motor, viscero-vegetative, sensitive types, with mental epileptic automatisms, disturbances in the perception and sensation of the body diagram, etc.
Most idiopathic forms of the disease are not characterized by the development of neurological deficits and loss of higher cortical functions. Physical and intellectual development in children usually does not suffer if there are no concomitant diseases or previous perinatal harms complicating the situation.
Personality changes of the epileptic type occur infrequently, only in severe forms of the disease with frequent poorly controlled generalized seizures and epistatuses.
Classification of the disease
There are many types of disorders. Therefore, we will look at the main ones to understand how epilepsy begins in children.
Based on the nature of its origin, epilepsy is usually divided into:
- hereditary, which is transmitted genetically;
- traumatic, acquired as a result of any external brain-damaging injuries;
- functional, the causes of which may be unknown or may involve a functional disorder of the brain, for example, due to a tumor.

Did you know? In the 19th century, people with epilepsy were kept separate from other patients in mental hospitals because doctors at the time believed that seizures were contagious.
But according to the nature of its manifestation, the disease is divided into the following most common types:
- temporal lobe epilepsy - temporal lobe epilepsy is the most common, with convulsive seizures can be either so weak that they are invisible to others, or strong and accompanied by intense feelings;
- frontal or frontal epilepsy , in which there may be no symptoms for a long time or attacks have a very rapid onset and end just as quickly;
- reflex - a reaction in the form of seizures occurs to a certain stimulus (trigger), for example, to a bright light; juvenile myoclonic appears in adolescence and manifests itself in the form of myoclonic spasms;
- Rolandic occurs most often in preschool children and before puberty and does not lead to loss of consciousness, but the child experiences a feeling of numbness or tingling in one part of the head.

Find out how to treat in children: cystitis, dysarthria, enterovirus infection, intestinal infection, mononucleosis, stomatitis, scoliosis, atopic dermatitis, streptoderma, obstructive bronchitis, adenoids, colic and whooping cough.
Differences in symptoms for different forms of the disease
Epilepsy in infants, the symptoms of which differ depending on the form of the disease, can be identified by the nature of the seizures.
| General seizures | Seizures are focal | |
| Large | Small | |
| Sharp muscle tension for 10-30 seconds. | Blackout of consciousness for a short period. | Convulsions or immobilization of any part of the body. |
| Loss of consciousness | Decreased muscle tone. | Movement of the head and eyes left and right. |
| Rhythmic contraction of muscles and limbs for 2-5 minutes. | Brief tension of all muscles. | Behavioral disorders |
| Rough sleep | Motor seizures are repetition of the same actions. | |
| Loss of orientation in space. | ||
What causes epilepsy in children?
Parents faced with this problem often wonder whether epilepsy in children can be treated and what causes it? The disease, in fact, can have many causes, among them the main ones are:
- pathologies that arise during embryogenesis and manifest themselves in impaired brain development due to the bad habits of the mother - smoking, alcoholism, drug addiction, as well as due to viral infections suffered during pregnancy, toxicosis of the last trimester of pregnancy and due to late age;
- brain trauma during childbirth due to entanglement of the umbilical cord, lack of oxygen, obstetric forceps, long anhydrous period and compression of the head in the birth canal;
- brain injuries of a child at any age due to concussions, bruises and blows;
- genetic inheritance from a relative with the same disorder;
- a lack of magnesium and zinc sometimes also provokes the onset of the disease and seizures;
- brain tumors of any location;
- the cryptogenic nature of the disease, which suggests that the causes of the disease are not clear.

Important! In any case, the onset of the disease always has some provoking factor. Even with a hereditary predisposition, there must be some stimulus to the onset of the disease, for example, a severe infection with a significant increase in temperature or severe stress.
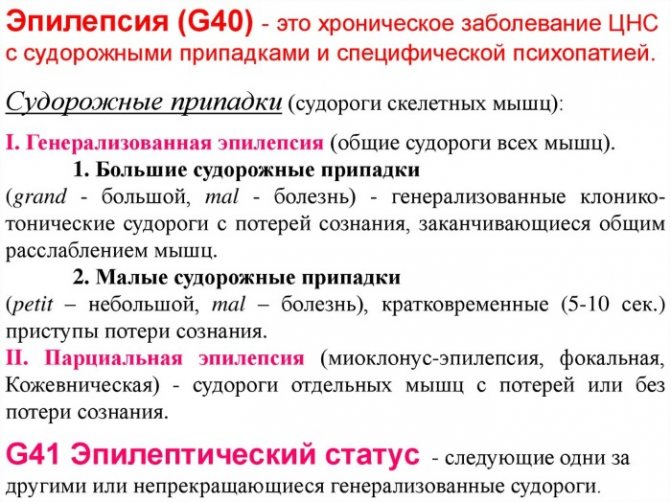
Classification of epilepsy according to the ICD
In accordance with the International Classification of Diseases, 10th revision, several etiological forms of epilepsy are distinguished.
They are presented in the table below:
| ICD-10 CODE | Form | Description |
| Epilepsy | ||
| Localized (focal) (partial) idiopathic epilepsy and epileptic syndromes with seizures with focal onset | Benign childhood epilepsy with EEG peaks in the central-temporal region Childhood, with paroxysmal EEG activity in the occipital region | |
| Localized (focal) (partial) symptomatic epilepsy and epileptic syndromes with simple partial seizures | Seizures without changes in consciousness Simple partial seizures developing into secondary generalized seizures | |
| Localized (focal) (partial) symptomatic epilepsy and epileptic syndromes with complex partial seizures | Seizures with changes in consciousness, often with epileptic automatism Complex partial seizures, developing into secondary generalized seizures | |
| Generalized idiopathic and epileptic syndromes | Benign: myoclonic - early childhood, neonatal seizures (familial), childhood epileptic absence seizures [pycnolepsy], Epilepsy with grand mal seizures on awakening Juvenile: absence epilepsy, myoclonic [impulsive petit mal] Nonspecific epileptic seizures: . atonic. clonic. myoclonic. tonic. tonic-clonic | |
| Other types of generalized epilepsy and epileptic syndromes | Epilepsy with: . myoclonic absences. myoclonic-astatic seizures Infantile spasms Lennox-Gastaut syndrome Salaam tic Symptomatic early myoclonic encephalopathy West syndrome | |
| Specific epileptic syndromes | Partial continuous: [Kozhevnikova] Epileptic seizures associated with: . drinking alcohol. use of medicines. hormonal changes. sleep deprivation. exposure to stress factors. If necessary, identify the drug, use an additional code for external causes (class XX). | |
| Grand mal seizures, unspecified [with or without petit mal seizures] | ||
| Minor seizures, unspecified, without grand mal seizures | ||
| Other specified forms | Epilepsy and epileptic syndromes not defined as focal or generalized | |
| Epilepsy, unspecified | Epileptic: . convulsions NOS. seizures NOS. seizures NOS |
Idiopathic, symptomatic or cryptogenic epilepsy
The international classification of epilepsies and epileptic syndromes, adopted in 1989 by the International League Against Epileptics, is based on 2 principles.
The first is to determine whether the epilepsy is focal or generalized.
According to the second principle, idiopathic, symptomatic or cryptogenic epilepsy is distinguished.
Localization-related (focal, local, partial) epilepsies:
- idiopathic;
- symptomatic (epilepsy of the frontal, temporal, parietal, occipital lobe);
- cryptogenic.
Generalized epilepsy:
- idiopathic (including childhood and juvenile absence epilepsy);
- symptomatic;
- cryptogenic.
Symptoms in newborns, infants and older children
In order to know how to recognize epilepsy in a child, parents must understand what symptoms they will encounter. Despite the fact that the symptoms of the disease in both children and adults are quite similar, children still have some manifestations characteristic of their age.
In newborns, epileptic seizures are not as obvious as in older children. Sometimes they are even difficult to notice. During a seizure, the baby may suddenly freeze and stop responding in any way to any irritating factors. The baby's gaze also changes - he begins to look intently and seems to freeze. And after the attack, the baby behaves as if nothing had happened.
In infants, the signs of epilepsy are not very different from newborns. The child also freezes, his swallowing reflex disappears, and he does not move his eyes. The attack usually lasts about 15 minutes, but no more. The baby can stretch out tense arms and legs and twitch them finely and symmetrically.

In children under one year of age, a seizure may be accompanied by an increase in body temperature, convulsive muscle tension, throwing the head back and a blank gaze.
Involuntary defecation and urination, as well as tongue biting and foaming at the mouth are not yet observed at this age.
It will be useful for you to read about vaccinations against: pneumococcal infection, diphtheria, meningitis and polio, and also familiarize yourself with the features of such vaccinations as: Mantoux, ADSM and DTP.
At an older age, during an epileptic attack, the above symptoms are also accompanied by throwing the hands behind the head and rolling the eyes. Also, the baby can tremble with the whole body or just muscle groups. The baby often has a headache, for no reason at all, and most often in the first half of the day. There is often loss of consciousness with muscle tension throughout the body.
It is difficult for the baby to speak; there is difficulty in speaking. Another sign may be the child’s hyperactivity, restlessness, excessive mobility, anxiety and absent-mindedness. The child can get up at night and perform any actions, while the child is not aware of anything.

What to do if your child has a seizure
Epilepsy, especially untreated, is bad because an attack can occur in a child at any time and in any place - including the most inappropriate or dangerous (for example, in the middle of the roadway). If the seizure is severe, adults will probably be required to provide first aid.
Its rules are as follows.
- It is better not to touch the patient unless necessary. That is, if there are no factors around him that threaten his health or life (cars, flow of people, objects that he can accidentally touch). If they are, you can take it to the side, to free space.
- The epileptic needs to place something soft under his head. Just don’t put him on the bed - it’s easy to roll off it, hitting him even harder.
- Don't put a spoon in your child's mouth. Fixing the limbs, jaws or tongue of an epileptic child, or trying to lay him on his side is also more harmful than beneficial. This will not stop the seizures, and in case of epilepsy in a child, the tongue and jaws are tense in the same way as other muscles of the body. That’s why he won’t swallow his tongue either—we’re not faced with a simple fainting spell, when such a thing is really possible. But the danger of breaking some of your teeth by biting a metal object during another spasm is quite real.
- The duration of the attack must be controlled. The longer it is, the higher the likelihood of additional damage to the cortex due to oxygen starvation (muscles consume a lot of oxygen during spasms, and the diaphragm itself works unevenly). Most epileptic seizures last less than three minutes, but up to five minutes is considered normal.
You should not expect your child to jump to his feet immediately after a seizure. On the contrary, the next day after it is characterized by weakness throughout the body, migraine and decreased concentration. No wonder: this surge of activity cost certain resources both to the cortex itself and to the muscles, which thanks to it were subjected to a short-term, but very intense load.

Examinations and tests
To identify the disease, the neurologist will first collect a detailed history, asking about the genetic predisposition of the little patient, the nature of the attacks and the conditions that precede them. The second necessary action is electroencephalography or EEG, where epileptic brain activity is determined.
To rule out brain damage, the baby may be prescribed an X-ray of the brain, MRI (magnetic resonance imaging), CT (computed tomography) and PET (positron emission tomography).
In order to exclude cardiac pathology that led to the disease, electrocardiography (ECG) is prescribed, possibly with daily monitoring.
It is also possible to study the biochemistry and immunology of the child’s blood and take a lumbar puncture to determine the causes of the disease.

Diagnosis of the disease

Diagnosis of idiopathic epilepsy should be carried out as early as possible. The later the disease is discovered, the more significant its consequences are, and treatment may become more difficult.
The main method for recording epileptic foci is the electroencephalogram. Electrodes are placed on the patient's head to record the difference in electrical potential between two points. This procedure helps to identify foci of the disease and detect the area of the brain that is susceptible to the disease. The type of disease and, accordingly, its treatment depend on the affected area.
Sometimes when carrying out this analysis it is necessary to provoke an attack, since excess brain activity is not always recorded in a calm state.
A careful collection of the overall picture of the disease also plays a special role. The specialist interviews not only the patient, but also his close circle. It is necessary to note and report the smallest details and oddities not only of physical condition, but also of behavior.
In addition to visiting an epileptologist, an examination by a neurologist is also necessary. This specialist notes changes in reflexes, mental and mental activity.
Sometimes an MRI and diagnostics of cerebral vessels may be required to rule out an acquired form of epilepsy.
First aid during an attack
When the first symptoms appear that indicate an approaching attack, you must:
- lay the baby on a flat surface without access to any objects and hold his head, avoiding bruises;
- free the toddler from tight clothes - unfasten the buttons or zipper;
- to prevent suffocation, you can turn the baby on its side and try to fix it like that;
- wait until the convulsions are over, protecting the child from blows;
- If the baby’s breathing does not recover on its own after the seizure ends, perform mouth-to-mouth artificial respiration.
Causes
According to medical statistics, epilepsy in infancy is much more common than in adults.
The positive point here is that in 70% of those affected during puberty, attacks disappear as the brain reaches its maturity.
The main causes of epilepsy in newborns:
- Hereditary factor. It has been proven that a child whose parents are sick has a higher risk of inheriting a tendency to pathology.
- Birth injury. The risk increases with prolonged labor, the use of vacuum extraction, and entanglement of the umbilical cord. If the mother has a narrow pelvis, the baby's head is compressed during birth and the brain may be damaged.
- Neuroinfections. Diseases such as meningitis, encephalitis, and influenza are very dangerous for a fragile child’s body. Seizures are often complications of these diseases.
- Head injuries. For a child, any bruise can become an impetus for the development of serious pathologies.
- Underdevelopment of the brain. Seizures occur especially often in premature babies.
- Genetic diseases in which chromosomal pathology is observed (Down's disease).
- Idiopathic causes. A baby is born with a lack of dopamine, which is responsible for regulating the processes of excitation and inhibition.

Basics and rules of treatment
How to treat epilepsy in children? The management of the disease, diagnosis and treatment is carried out by a neurologist or epileptologist.
General recommendations and care
The first thing treatment is aimed at is determining the root cause of the disease and alleviating the course of the disease.
The child requires a gentle regime with the absence of stress factors, overexertion, and fatigue. It is worth limiting mental and physical stress, as well as time watching television and spending time on the computer.
The baby should receive good nutrition, rich in all necessary microelements. You definitely need to give him vitamin complexes.

Vitamin deficiency can lead to weakening of the body and the development of various diseases in a child, so find out which vitamin complexes are best for your baby.
Compliance with all medical recommendations is not only desirable, but mandatory, due to the chronic course of the disease and due to the risk of the disease transitioning from a neurotic level to a psychotic level with personality changes.
The child can be helped through psychotherapy, immune support and hormonal therapy.
Drug treatment
To reduce the frequency and intensity of seizures, the child is prescribed anticonvulsants and antiepileptic drugs. At first the dose is given small, over time it increases until the baby can control the attacks.
These are drugs such as:
- Phenobarbital;
- Diazepam;
- Carbamazepine;
- Topiramate;
- Lamotrigine and others.

Important! Parents must give the baby all the medications prescribed by the doctor. Therapy is an urgent need and is often lifelong.
Surgical intervention
Treatment of the disease with surgical methods is not very common today. The treatment is dangerous and patients are selected with special care. Surgical intervention is allowed only if epilepsy does not respond to conservative treatment.
Surgery methods include:
- anterior temporal lobectomy;
- limitation of temporal resection;
- stimulation of the vagus nerve using implants;
- hemispherectomy;
- extratemporal neocortical resection.
Treatment of illness in children
Treatment of the disease in infants begins with normalizing the daily routine.
The baby should go to bed, wake up, and eat at approximately the same time.
The child should be protected from sharp sounds, flashes of light, and nervous shocks. You need to limit the amount of salt and carbohydrates in your diet.
Doctors are of the opinion that any form of epilepsy should be treated with anticonvulsants. The medicine is selected individually.
Without medication, the disease will progress, and the chances of recovery during adolescence will be significantly reduced.
The following drugs are approved for use in infants:
- Gluferal;
- Convulex;
- Depakine.
At the same time, nootropics (Pantogam) are prescribed. It improves cerebral circulation, eliminates the effects of hypoxia, and prevents cognitive impairment.
Surgical treatment is used if the cause of the attacks is a tumor in the brain.
Prognosis and prevention
Today there are many effective antiepileptic drugs, thanks to which it is possible to achieve significant success in most cases. If treatment begins immediately after the first signs of epilepsy appear in a child, then he will most likely be able to live a normal life. And if for several years the baby no longer has epileptic seizures, then the anticonvulsants can be removed. In more than half of the cases, seizures do not recur.
Important! The prognosis is unfavorable if the onset of the disease is early and is accompanied by a decrease in mental abilities, status epilepticus, and if there is no positive effect from taking medications.
Prevention of the disease should begin during the mother’s pregnancy and consist of a healthy lifestyle. If a child develops epilepsy, then treatment should begin from the very first symptoms, be sure to be regularly observed by a neurologist or epileptologist, strictly adhere to the prescribed treatment and notify school teachers about the child’s condition, familiarizing them with first aid methods for a seizure.

Despite the fact that epilepsy is a rather serious disease of a neurological nature, today it responds well to treatment and in many cases it is possible to achieve lifelong remission. The main thing is to pay attention to oddities in the child’s behavior in a timely manner, immediately seek qualified help and strictly follow the recommendations of the attending physician.
Children Children's diseases
Types and forms of epilepsy
Epilepsy in infants, the symptoms of which depend on the form of the disease, can have several manifestations. It is worth considering the most popular of them.
Dravet syndrome
Severe pathology leading to difficulties in psychomotor development and sometimes death. Appears at 2-10 months. Features: multiple attacks during the day.
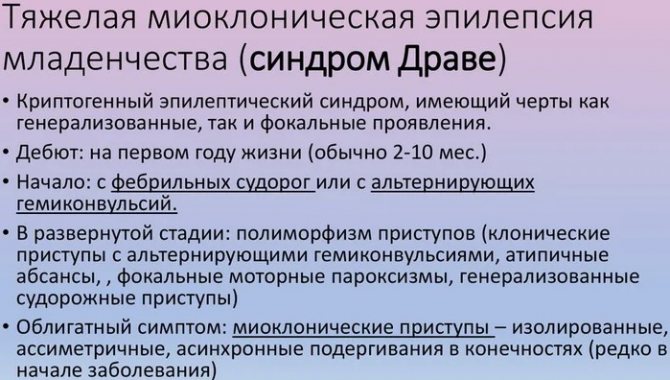
This condition can last for several days in a row (up to a week). Then a short break - 2-3 weeks, and everything repeats again. Convulsions may be present or everything can be done with muscle twitching and disturbances of consciousness.
Benign myoclonus epilepsy of infancy
Appears before the age of 3 years (early manifestations occur at 4-11 months). The disease is not preceded by psychomotor impairment. It is considered an idiopathic or symptomatic form of the disease and is milder than Dravet syndrome. Characteristic signs are short-term myoclinic (wobbly legs) attacks involving the head and arms.
Doose syndrome
Occurs in children aged 1-5 years. The disease is characterized by short-term convulsions, up to several times a minute, and nodding movements are common. Consciousness does not suffer in this case.
Epileptic seizures in this case are associated with diseases of the central nervous system, motor dysfunction, and mental retardation.
Benign familial seizures
Observed from the age of 3 days. Their appearance is associated with the presence of epileptic seizures in family members of the newborn. The attacks do not last long - 1-2 minutes, but their number can reach up to 30 per day. 1-3 weeks after the onset of seizures disappear.
Benign nonfamilial seizures
Observed on the 5th day after birth. Accompanied by muscle contractions in the limbs and on the face, sometimes on the right, sometimes on the left. Repeat throughout the day. Completely disappear after 2 weeks.
Ohtahara syndrome
A rare malignant disease. Appears in the first months of life. It is characterized by tonic attacks in the amount of 10-300 per day. The child has serious anomalies in the formation of the central nervous system.
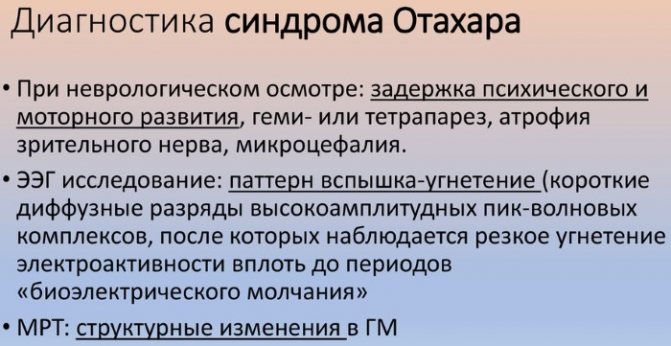
With age, the risk of mortality increases (up to 40-50%).
West syndrome
Catastrophic epilepsy, which becomes noticeable between the ages of 3 and 8 months. Accompanied by flexion and extension movements. It can develop with or without problems with the central nervous system. The consequences are delayed development of psychomotor functions, the appearance of signs of cerebral palsy. The prognosis of the disease is unfavorable.
Idiopathic benign partial epilepsies
Their collective name is “Watanabe syndrome”. They make themselves felt at the age of 3-20 months. They are characterized by complex partial seizures, moderate convulsions, cessation of motor activity, and bluish discoloration of the skin.
Early epileptic encephalopathy
Registered in the neonatal period of development. Characterized by a high degree of lethality. The genetic factor plays a significant role in the occurrence of the disease. Accompanied by myoclonic seizures, often fragmentary, but gaining intensity with age. Focal seizures, the center of occurrence of which is in the brain, are fundamental to the disease.
Vitamin B6 dependent epilepsy
The disease, which is inherited, may appear after 1 month of life. This is typical for children whose mothers took pyridoxine during pregnancy. Children remain restless between attacks and react to external irritants with muscle contractions.
The disease is not treated with conventional anticonvulsants and subsides when taking large doses of vitamin B6 (25 mg/kg per day).
Malignant wandering partial seizures
A very rare disease, only 50 cases are known in the world. Half of them occurred in the first days of life, the other half at the age of 1-3 months. It begins with the manifestation of one (focal) focus of seizures, and then turns into a multifocal (multifocal) form.

The disease demonstrates drug resistance and does not create metabolic problems.