The first mention of blepharospasm and spasm of the lower part of the face was stated in a 16th century painting called “The Onlooker.” At that time, and for several centuries to follow, patients with such spasms were considered mentally unstable, and were often sent to insane asylums. Little progress in the diagnosis and treatment of blepharospasm was made until the early 20th century, when Henry Meige, a French neurologist, described a patient with eyelid and midface spasms and facial hemispasm, a condition now known as Meige's syndrome. Almost at the same time, the first medical procedures began to be used, including the injection of alcohol into the facial nerve, neurotomy and neurectomy.
Normally, an adult blinks 10 to 20 times per minute. The number of blinks tends to decrease when reading or working on a computer. An increase in the frequency and force of eyelid closure is known as blepharospasm. This is a focal dystonia that occurs in adults with repeated spasms of eye closure; the orbicularis oculi muscle contracts involuntarily and violently. Periods of spasms can last from a few seconds to several minutes and are often repeated. The severity of the condition varies from increased blinking with occasional spasms to severe with severe painful spasms. Sometimes the spasms can be so severe that they cause serious visual impairment.
Etiology
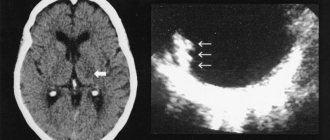
Blepharospasm is a subtype of focal dystonia. Most cases of blepharospasm are idiopathic and are called benign or primary blepharospasm. In the case of blepharospasm, involuntary closure of the eyelids occurs due to spasms in the orbicularis oculi muscle. This distinguishes blepharospasm from paresis of the levator palpebrae , in which apraxia occurs, and this condition occurs in Parkinson's disease. The etiology of blepharospasm is not yet known. It was thought that blepharospasm may be caused by pathology in the basal ganglia, but this has not been proven. At the same time, there is reason to believe that several cortical and subcortical structures may be involved in the development of blepharospasm. The circuitry that is involved in the blinking process includes the sensory peripheral part, the central control area in the brain, and the motor part. It is believed that a defect occurs in this circuit of neurons. The exact mechanism is not known, but it is likely that there is more than one defective locus, leading to overload of neurotransmission and the development of blepharospasm.
There have been cases of secondary blepharospasm due to a certain organic disease. Ocular causes of secondary blepharospasm include:
- Trauma to the eye (mechanical, chemical, or thermal)—particularly to the cornea—causes acute blepharospasm.
- Blepharitis.
- Conjunctivitis, iritis, keratitis.
- Dry eyes.
- Other chronic diseases of the eyelids or eyes
- Glaucoma or uveitis.
Blepharospasm can also occur with systemic conditions:
- Multiple sclerosis
- Focal brain injury or tumor
- Infections (viral encephalitis, Reye's syndrome, subacute sclerosing panencephalitis, Jakob-Creutzfeld disease, AIDS, tuberculosis, tetanus).
- Atypical form of Parkinson's disease / multiple system atrophy / progressive supranuclear palsy.
- Side effects of medications - for example, olanzapine, levodopa.
- Tardive dyskinesia.
- Tourette's syndrome.
- Cerebral paralysis
There is evidence of some genetic determination, although the likelihood of blepharospasm being inherited is only 5%.
Epidemiology
Prevalence estimates vary, with incidence rates ranging from 16 to 133 per million. Blepharospasm occurs more often in women than in men. This condition most often occurs over the age of 50.
Causes
The pathological mechanism for the development of blepharospasm is currently unknown. Most researchers believe that damage to the basal ganglia of the brain can lead to spastic contraction of the orbicularis oculi muscles.
Blepharospasm often occurs against the background of:
- Parkinson's disease;
- taking antipsychotic medications;
- trichiasis;
- supranuclear palsy;
- foreign body in the eye;
- dry eye syndrome;
- blepharitis.
Blepharospasm occurs against the background of many diseases, including Parkinson's disease
Prevention of blepharospasm consists of preventing eye injuries, timely detection and treatment of eye, dental, neurological and mental diseases.
Spasms of the orbicularis oculi muscles can also be provoked by:
- hypovitaminosis;
- working at the computer for many hours every day;
- exposure to stress;
- chronic lack of sleep, physical and mental fatigue.
Prevention of blepharospasm
In modern medicine there are no specific ways to prevent blepharospasm. If the pathology has developed secondary, then it is necessary to avoid irritating factors as much as possible. Wear dark sunglasses in bright light. It is recommended to treat blepharitis and dry eyes with medication, eliminate stress if possible and reduce the dosage of the provoking drug. Ophthalmologists recommend excluding drinks that provoke stimulation of the central nervous system (coffee and strong tea). After working at the computer for a long time, it is better to do eye exercises.
If you notice that for some reason the frequency of blinking is increasing or you need to make an effort to close your eyelids, you should seek help from a neurologist or ophthalmologist.
At the Fedorov Clinic in Moscow, doctors will help diagnose the disease in a timely manner and prescribe treatment. Make an appointment
Forms
There are two forms of blepharospasm, which can be considered as two stages of one process: clonic and tonic.
With clonic blepharospasm, frequent uncontrolled blinking occurs, initially of only one eye, but after some time the second one is also involved in the pathological process. Unilateral blepharospasm is extremely rare in clinical practice.
Slowly, over several years, the duration and intensity of episodic attacks of clonic blepharospasm increase. The squeezing becomes strong and prolonged. In this case, they talk about the transition of the pathological condition to the tonic form.
Tonic blepharospasm poses a serious problem for the patient. In severe cases, approximately 70% of patients develop mechanical blindness, that is, loss of vision due to the inability to open the eyelids.
Tonic blepharospasm is characterized by strong and prolonged squinting
In young women suffering from hysteria, bilateral blepharospasm may suddenly occur, disappearing on its own after a few hours. Characteristic of the hysterical form of blepharospasm is that pressing on the exit points of the branches of the trigeminal nerve leads to resolution of the attack.
Causes of pathology
In many cases, it is not possible to determine the exact nature of the development of muscle twitching. Since the disease is of neurogenic origin, it is customary to identify several factors that can lead to the development of the disease:
- Eye pathologies of both inflammatory and traumatic nature. Problems such as blepharitis, dryness, or foreign body penetration into the cornea and conjunctiva lead to constant irritation. The excitability of the nerve that provides the functions of the organ increases, which causes disruption of its normal functioning. The entire area around the eye becomes susceptible to environmental factors. Reflex blinking, which is a protective mechanism, develops into symptoms of blepharospasm. A similar etiology can cause tics in a child.
- Medications can also cause the disorder. The use of antipsychotics can cause side effects such as spasms of the facial muscles. These drugs are widely used in neurology to correct mental disorders and other problems.
- Long-term exposure to adverse environmental factors. These include constant eye strain while working with text or at the computer, lack of proper rest, as well as general psycho-emotional stress. Blepharospasm of the eyes is a common problem in people suffering from insomnia and chronic fatigue syndrome.
- Poor nutrition can also negatively affect the health of the nervous system. The lack of a sufficient amount of vitamins and microelements in the menu provokes a disturbance in the transmission of impulses, which leads to the manifestation of muscle twitching.
Diagnostics
Blepharospasm is determined by the presence of a characteristic clinical picture. It is important to establish the cause of its occurrence, since only by acting on it can a positive treatment effect be achieved. For this purpose, a complete ophthalmological examination is carried out. If blepharospasm is not explained by ophthalmological pathology, consultations are held with a neurologist, psychiatrist, or dentist.
A complete ophthalmological examination allows you to clarify the cause of blepharospasm.
What is blepharospasm
Blepharospasm is a disease of a neurological nature, a pathology associated with the formation in patients of a reflex contraction and closure of the eyelid. The facial periocular muscles involuntarily close and because of this, a person loses vision, because he simply cannot open his eyes without physical or medicinal assistance.
It occurs with unequal frequency in men and women aged 50-60 years. At the same time, women get sick 3 times more often; in some cases, blepharospasm was recorded in females who had barely reached 20 years of age. With blepharospasm in its initial stage (without complications and transition to a chronic form), only 1 eye twitches.
Treatment
Treatment of blepharospasm is aimed at eliminating the cause. For example, for dry eye syndrome, the use of moisturizing eye drops (“artificial tears”) is indicated. If there is a foreign body in the eye, it is removed followed by a course of anti-inflammatory and absorbable therapy.
If the cause of blepharospasm cannot be determined, Botox therapy is used: microdoses of botulinum toxin are injected into certain points of the round muscle of the eye, causing temporary paralysis of the muscle. As a result, blepharospasm stops. The effect of Botox injections lasts no more than three months, so injections must be repeated regularly.
Blepharospasm therapy with Botox is carried out for an unknown cause of the disease.
If treatment with botulinum toxin is ineffective, surgical correction of blepharospasm is performed, which consists of complete or partial removal of the orbicularis oculi muscle.
It is important to establish the cause of blepharospasm, since only by acting on it can a positive treatment effect be achieved.
Blepharospasm - symptoms and treatment
The main goal of treatment of blepharospasm is to achieve stable remission while maintaining the ability to work and social activity of patients.
The “gold standard” in the treatment of blepharospasm is botulinum therapy - local injections of botulinum toxin type A (BTA) [1]. Initially, this method was used by Californian ophthalmologist A. Scott in the treatment of people with strabismus. A little later, he used local injections of BTA to treat patients with blepharospasm and hemifacial spasm [16]. A year earlier, ophthalmologist B. Frueh and his colleagues first described the use of BTA for blepharospasm [17][18]. Since then, botulinum toxin has been used not only in ophthalmology, but also in the treatment of diseases of the nervous system.
Officially, botulinum therapy began to be carried out in 1989 after approval by the FDA (Food and Drug Administration, USA). One of the first indications for the use of BTA was blepharospasm [19]. According to the recommendations of the European Federation of Neurological Societies, BTA drugs are recommended as the first line of treatment for this disease [1][9]. Their safety and high effectiveness have been confirmed by numerous controlled studies and 35 years of clinical practice [9].
Botulinum toxin is injected into the target muscles: the eyelid muscles and the orbicularis oculi muscles. If the dosage is observed, the drug eliminates pathological muscle contractions without interfering with their function. BTA is recommended to patients immediately after diagnosis. Local injections must be performed regularly. The interval between procedures varies: it all depends on the patient’s well-being. On average, botulinum therapy is carried out every 3-4 months.
The effect usually occurs on the 3-4th day after the injection and gradually increases. Forced, uncontrolled squinting stops, which leads to improved vision, as voluntary control over opening and closing the eyes returns. The effect lasts 3-4 months, sometimes longer. Thanks to this, patients can lead a normal lifestyle [9].
Botulinum toxin is produced by the gram-positive bacterium Clostridium botulinum (botulinum). It affects nerve cells by blocking the release of acetylcholine, a neurotransmitter involved in the transmission of nerve impulses. This leads to a dose-dependent, reversible decrease in muscle strength [1][9].
The following BTA preparations are approved for use in Russia:
- 100-unit: Botox, Lantox, Xeomin, Relatox, Botulax (some drugs are available in bottles of 50 and 200 units);
- 300- and 500-unit: Dysport.
The dosage is calculated individually in accordance with the instructions for medical use. The conversion ratio of units of action between Dysport and 100-unit drugs for neurological indications is 3:1 or less, for aesthetic indications - 2.5:1 [20]. The final dosage calculation remains with the doctor.
Treatment with botulinum toxin should be performed by experienced professionals who have undergone appropriate training. The dose of administration at one point for 100-unit BTA preparations is 1.25-5 units. Injections are performed at 3-6 points on each side. The average total dose on each side is 15-30 units, respectively, 30-60 units of the drug are consumed per procedure. Botulinum toxin should not be injected into the middle zone of the upper eyelid, as this can lead to ptosis (drooping of the eyelid) [3][4][9].
Possible side effects of BTA:
- very often - ptosis;
- often - weakness of the facial muscles, diplopia (double vision), dry eyes, swelling of the eyelids, lacrimation;
- infrequently - paresis of facial muscles;
- rarely - ophthalmoplegia (damage to the oculomotor nerves), entropion of the eyelid [9].
To reduce the risk of side effects, it is important to maintain the dose of BTA and begin treatment with the minimum effective dosage. Drugs that affect the transmission of nerve impulses, such as antibiotics of the aminoglycoside group (amikacin, gentamicin, etc.), should be used with caution [9].
Before carrying out botulinum therapy, the doctor must obtain voluntary informed consent for injections. After BTA injections, it is recommended to actively contract the injected muscles for 20 minutes and to be under medical supervision for an hour to monitor the occurrence of immediate allergic reactions. To reduce the risk of intradermal hematomas on the face, it is recommended to cool the injection sites for 10-20 minutes [9].
Another effective way to relieve the symptoms of blepharospasm is pink sunglasses (with FL-41 filter). They are used to avoid provocation of squinting [1][3][4][9].
Drug therapy for blepharospasm is a thing of the past, however, if BTA is not possible, the following drugs can be prescribed: dopaminergic, cholinergic, serotonergic, catecholamines, GABA, anticonvulsants, benzodiazepines, antipsychotics. Their effectiveness does not exceed 20%, is often temporary, requiring a stepwise increase in dose and long-term use. The most commonly prescribed drugs are clonazepam and baclofen. However, you need to remember that many drugs have side effects, including addiction.
The least effective are muscle relaxants (tolperisone, tizanidine), benzamides (sulpiride, tiapride) and antidepressants (amitriptyline, fluoxetine, paroxetine, sertraline, fluvoxamine, trazodone) and anxiolytics (anti-anxiety drugs). They are prescribed as an addition to other drugs for the correction of concomitant pathologies (pain syndrome, emotional and/or somatoform disorders) [1][7][9].
Blepharoplasty , can be used as an additional treatment method . It improves the tolerability and results of BTA injections [3].
Deep brain stimulation (implantation of a special device into the body that sends electrical impulses to the desired part of the brain) has shown little effectiveness in treating blepharospasm. In addition, there is a possibility of postoperative side effects: speech impairment, paresthesia, development of hypokinesia, coordination disorders, infection, malfunction of the implanted generator, damage to the electrodes. The question of carrying out this procedure can be considered if there is no effect after 3-6 BTA procedures in a sufficient dose, i.e., with resistance to BTA, which is extremely rare [1][7]. Other surgical methods for correcting blepharospasm are not effective enough and are traumatic [23].
Separately, it is worth paying attention to the patient’s socialization and adaptation : include him in groups of psychological support, psychotherapy and cognitive behavioral therapy [1][4][9].
Possible complications of blepharospasm
Complications of chronic blapharospasm
At the initial stage of blepharospasm, the disease is manifested by rapid blinking and voluntary squinting. As the pathology develops, the symptoms become more and more pronounced; the closing of the eyelids can last for several minutes or hours.
Often the disease affects other muscles of the face, namely the neck, larynx, forehead, and tongue. The spasm affects the eyelids and lower part of the face. Chronic blepharospasm is accompanied by irritation of the membrane of the eyeball, a burning sensation, increased tearing, and a feeling of “sand in the eyes.”
Many patients develop mechanical blindness over time—the vision of the eye that is often closed decreases.
The consequences of the disease always make adjustments to the patient’s lifestyle. First of all, a person loses the ability to drive vehicles and perform work that requires visual concentration. In later stages, the patient may be completely unable to care for his own needs.
Signs of illness
Symptoms of blepharospasm usually affect both eyes. The unilateral form is considered rare and occurs in the initial stages of the disease.
Main features:
- unnaturally frequent blinking;
- involuntary squinting;
- twitching of eyelids;
- swelling in the eyelid area;
- tearfulness;
- moisture and loosening of the skin around the eyes.
A special type of disease is hysterical blepharospasm, which occurs in women during an emotional outburst. You can distinguish it from another nervous disorder by paying attention to the following signs:
- there was severe shock or stress before the attack;
- spasms affect only the eye area;
- with light pressure on the eyelid, the symptoms decrease;
- the muscles of the eyebrows and forehead are not subject to cramps.
If signs of blepharospasm occur, you should consult a doctor. With the participation of a therapist, neurologist, psychiatrist and dentist, a complete picture of the disease is drawn up and treatment is prescribed.
Diagnostic methods
The disease is diagnosed using several methods.
Ophthalmology and neurology
The disease is diagnosed by a neurologist and an ophthalmologist . Doctors conduct an initial examination of the patient, examine the organs of vision using a slit lamp and facial expressions using a special device. The cause of the disease determines which doctor is consulted for treatment: the primary form is treated by a neurologist or psychiatrist, while the secondary form requires the help of a dentist or ophthalmologist.
Taking an anamnesis
After reviewing the medical history, the doctor will find out whether the patient has undergone dental prosthetics in recent years, received facial injuries, or undergone plastic surgery.
Differential diagnosis
It is important to distinguish blepharospasm:
- from hemifacial spasm;
- from myokymia of the eyelid;
- from Tourette's syndrome;
- from painful tics;
- from apraxia of eyelid opening;
- from slow dyskinesia.
Is blinking a “mirror of the soul”?
It’s hard to disagree with the fact that the eyes are the “mirror of the soul.”
Here is a child, standing “under interrogation” in front of a parent and looking him straight in the face, and suddenly begins to “batt his eyelashes” frequently. Does this mean that something has gotten into his eyes and that something needs to be removed from there, causing frequent blinking to cause an increased secretion of tear fluid, which would wash and disinfect the surfaces of the eyes? No, he is simply guilty and for the sake of his own salvation, he openly lies at any cost.
This simple test indicates a deep connection between the state of the organ of vision - its ill health or health - and the state of the large brain. Or not so large, but no less important, its nervous structures, in the depths of which the roots of pathology often lie:
- facial nerve nuclei;
- brain stem;
- basal ganglia.
And depending on the height of the location of the affected structures, the forms of manifestation of blepharospasm and the degree of their severity will be different.
Prevention
To prevent exacerbation of the symptoms of blepharospasm, provoking factors should be avoided. To prevent and prevent the disease it is necessary:
- do not overload the eye muscles, limit the time spent in front of the computer and mobile phone screen;
- avoid overwork, maintain a sleep schedule;
- take vitamin complexes, especially in winter;
- try to avoid stressful situations and emotional outbursts;
- do eye exercises;
- reduce the consumption of coffee, alcohol and energy drinks.
Blepharospasm is a very common, but not the most dangerous disease. If you consult a doctor in a timely manner, the disease can be easily treated. At a young age, it is easier to avoid the development of muscle spasms by controlling visual stress and the state of the emotional background.
A strong immune system, physical activity and a healthy nervous system are simple and necessary factors to avoid attacks of blepharospasm.
Complaints before treatment of blepharospasm:
♦ Category: Diseases.
Treatment: goals and methods
There is no method for treating blepharospasm as such - the goal of therapy is to influence the causes that gave rise to it.
From here it logically follows that we follow several strategic directions in the treatment of ailments underlying the syndrome.
This is the principle of conservative therapy, including:
- drug therapy;
- acupuncture (acupuncture);
- psychotherapy.
And:
- the use of surgical methods of healing;
- treatment with injections of botulinum toxin A.
Drug therapy includes the use of several groups of drugs:
- anticholinergics (in particular, Clonazepam with a gradual – according to the scheme – dose increase);
- benzodiazepines;
- antidepressants;
- neuroleptics.
As a necessary measure, which also gives a time-limited effect, surgical methods are used:
- bilateral intersection of the branches of the facial nerves;
- thermolysis of the branches of the facial nerve (which can be replaced by a local injection of ethyl alcohol).
Treatment with botulinum toxin A consists of blocking cholinergic nerve endings with inhibition of the release of acetylcholine at the synaptic junction, leading to a weakening of muscle spasm.
Overcoming the dysfunction of the cholinergic and dopaminergic systems is another important task in the development of new methods of biochemical influence on the involved centers of the central nervous system.
It is possible to prevent the development of the disease!
To prevent the syndrome and its complications, healthcare workers should be as attentive as possible to the patient’s health - be careful when performing dental procedures and surgical operations on the face.
As for the patient himself, he should:
- avoid injuries to the face and head;
- provide measures designed to prevent the occurrence of diseases with the formation of foci of chronic infection that can subsequently lead to inflammatory eye diseases;
- promptly treat barely emerging neurological diseases (neuropathy of the facial nerve, facial tics);
- avoid overstraining the organs of vision and facial muscles when working on drawings, as well as with a computer and microscope;
- promptly select and change glasses when vision is weakened;
- Given that the activity of the basal ganglia ceases during sleep, due attention should be paid to night rest.
Of course, the patient can deceive himself for some time by delaying treatment with the help of “deceptive maneuvers” and corrective gestures (or drinking alcohol), but only timely help from specialists (neurologist, ophthalmologist, surgeon) can significantly improve the situation of a patient with blepharospasm syndrome .