Convulsions, paralysis, paresis are signs of damage to the nervous system. Paresis is a decrease in muscle strength that is caused by damage to the nerve pathways connecting the brain to a muscle or group of muscles. The difference between paresis and paralysis is that with paralysis there is complete immobilization of a part of the body, and with paresis it is partial. Paresis can occur with any type of damage to the brain, spinal cord, or peripheral nerves.
Depending on the level of damage, neurologists distinguish between central and peripheral paresis. At the Yusupov Hospital, doctors use comprehensive treatment of paresis, an individual approach to the choice of method of therapy and rehabilitation of each patient.
Neurologists prescribe modern medications that are highly effective and have minimal side effects. The rehabilitation clinic is equipped with modern equipment for mechanotherapy. Exercise therapy instructors use innovative methods of physical therapy. Specialists at the Yusupov Hospital adhere to the principles of evidence-based medicine and use the best practices of their foreign colleagues. The hospital has created comfortable conditions for patients to stay, which help create a positive attitude toward recovery.
Types of paresis
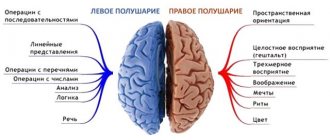
Central paresis occurs when the brain or spinal cord is damaged. Disorders develop below the site of damage. They capture the right or left half of the body. This condition is called right-sided or left-sided hemiparesis. Paresis of the left arm is called left-sided monoparesis.
If, as a result of central paresis, disturbances occur in both arms or both legs, we are talking about paraparesis, and if motor function is impaired in all four limbs, we are talking about tetraparesis.
Symptoms of facial neuritis
The clinical picture of damage to the facial nerve depends on the level of damage and the degree of conduction disturbance. It consists of symptoms of damage to the facial and intermediate nerves. As a result of damage to the facial nerve itself, paralysis or paresis of facial muscles occurs - prosoparesis or Bell's palsy. On the affected side, the eye is open and the patient cannot close it (lagophthalmos), or the eyelids do not close completely.
The severity of clinical manifestations of facial muscle paresis: according to a 5-point system for neuropathy of the facial nerve (proposed by Ya.S. Balaban)
NORMAL – 5 points;
MILD DISEASE
prosoparesis 4 points: the patient can close his eyes, frown and raise his eyebrows, wrinkle his forehead, but with less force than on the healthy side; when grinning, 4–5 teeth are visible, the mouth is barely noticeably pulled to the healthy side; the patient inflates his cheek, but with less force than on the opposite side; in electroneuromyographic studies, the latent time of the M-response is 4.5 – 5.0 ms;
prosoparesis 3 points: the patient can close his eyes, but the eyelashes protrude more than on the healthy side (eyelash symptom); may move the eyebrow towards the center and raise it, wrinkle the forehead, but to a lesser extent and with less force than on the healthy side; however, he cannot overcome the resistance of the researcher. When grinning, 3–4 teeth are visible; the patient does not form his lips well to whistle and can hardly whistle; puffs out his cheek, but does not overcome the resistance of the examiner; with electroneuromyography, the latent time of the M-response is 5.0 – 5.5 ms;
MODERATE DISEASE
prosoparesis 2 points: when grinning, 2–3 teeth are visible; cheek inflation is weak; the patient cannot whistle; does not close the eye completely - a strip of sclera 1-2 mm is visible (Bell's symptom); forehead wrinkles slightly; insignificant movements when trying to frown; with electroneuromyography, the latent time of the M-response is 5.5 – 6.0 ms;
SEVERE DISEASES
prosoparesis 1 point: the affected eye does not close – a strip of sclera 3–5 mm is visible (Bell’s symptom); cannot frown or raise an eyebrow, puff out his cheeks, or whistle; when grinning, 1-2 teeth are visible on the affected side; with electroneuromyography, the latent time of the M-response is more than 6 ms;
prozoparesis 0 points (prosoplegia): complete paralysis of facial muscles - the patient does not close his eyes (sclera strip more than 5 mm); cannot frown or raise an eyebrow, cannot bare his teeth; there is no movement of the corner of the mouth on the affected side; cannot move his lips to whistle; the mouth is sharply skewed to the healthy side; with stimulation electroneuromyography there is no M-response. degree of paresis of facial muscles according to K. Rosler’s classification
0 degree: no paresis;
I degree: mild paresis, no facial asymmetry at rest;
II degree: moderate paresis, squinting of the eyes is possible, but at rest the asymmetry of the face is clearly visible;
III degree: severe paresis, incomplete squinting of the eye, barely noticeable movements and low muscle tone;
IV degree: complete paralysis, lack of movement and low muscle tone (to the point of atony). House-Braakman scale
1st degree: norm (normal function of all branches);
Grade 2: mild dysfunction: A: mild weakness, detectable; upon detailed examination, minor synkinesis may be noted; B: symmetrical face at rest, normal expression; B: movements – 1. forehead: slight moderate movements; 2. eye: closes completely with force; 3. mouth: slight asymmetry;
Grade 3: moderate dysfunction: A: obvious, but not disfiguring asymmetry; detectable but not pronounced synkinesis; B: movements – 1. forehead: slight moderate movements; 2. eye: closes completely with force; 3. mouth: slight weakness with maximum effort;
Grade 4: moderate dysfunction – A: obvious weakness and/or disfiguring asymmetry; B: movements – 1. forehead: absent; 2. eye: does not close completely; 3. mouth: asymmetry at maximum force;
Grade 5: severe dysfunction: A: barely noticeable movements of the facial muscles; B: asymmetrical face at rest; B: movements – 1. forehead: absent; 2. eye: does not close completely;
Stage 6: total paralysis (no movements).
Due to insufficient pressure of the lower eyelid, a tear leaks out, and with damage above the level of origin of the greater superficial petrosal nerve, as well as the root (in the cerebellopontine angle), dry eye is characteristic. The patient cannot wrinkle his forehead or frown on the affected side. The nasolabial fold on the side of paralysis is smoothed, the mouth is pulled to the healthy side, motionless, and due to poor closure of the lips, liquid food and water flow out of this corner of the mouth. When the cheeks are puffed out, the sail sign is revealed (the cheek puffs out and fluctuates with the escaping air). The patient cannot blow out a candle or whistle. Bell's symptom is characteristic: when you close your eyes, the eyeball on the affected side rolls up and out. A strip of sclera is visible in the open palpebral fissure.
Early signs of developing prosoparesis or mild lesions are the symptom of rare blinking - asynchronous blinking of the eyes, less blinking on the affected side. A symptom of eyelashes is also noted - when squinting on the affected side, the eyelashes protrude more strongly, the patient cannot separately close the eye on the side of the paresis. In addition to the described symptoms of prosoplegia, autonomic-vascular disorders (dry eye or lacrimation) are usually detected; unilateral taste disturbance in the anterior 2/3 of the tongue (always occurs if the lesion is above the origin of the chorda tympani); hearing impairment (hyperacusis, especially in low tones). If the symptoms are manifested by prosoparalysis (paresis), as well as persistent and severe taste disorders in the area of the anterior 2/3 of the tongue on the affected side, the process is localized in the fallopian canal and is caused by a disease of the middle ear. The combination of prosoparesis (plegia) with pronounced and persistent symptoms of hyperacusis indicates a lesion at the level of the stapedius nerve. When the facial nerve is damaged in the internal auditory canal above the origin of the greater petrosal nerve, prosoplegia is combined with dry eye, taste disturbance in the anterior 2/3 of the tongue and deafness in one ear. This is particularly characteristic of tumors of the VIII cranial nerve.
In cases where prosoparesis (plegia) is a consequence of changes at the level of the cerebellopontine angle, patients also experience symptoms of dysfunction of the trigeminal and abducens nerves. This is most often characteristic of inflammatory processes in this area, as well as tumors of the vestibulocochlear nerve. In cases where the lower group of facial muscles is affected, it can be assumed that the central neuron (corticonuclear pathway) of the facial nerve is turned off.
To distinguish prosoparesis from neuropathy, one should take into account the preservation of the brow reflex (closing of the eyelids during percussion of the brow ridge), the presence of central paresis and hemiparesis phenomena. It is important for practitioners to know that most prosoparesis (plegia) is associated with the localization of the lesion in the facial nerve canal.
According to the course of the disease, there is an acute stage - up to 2 weeks, a subacute period - up to 4 weeks, a chronic stage - over 4 weeks. The course and prognosis of the disease depend on the depth of damage to the facial nerve, its etiology, the state of reactivity of the body, the timeliness and adequacy of the treatment started. Most lesions of the facial nerve of idiopathic origin, as a rule, have a favorable clinical prognosis, while with otogenic and traumatic neuropathies, recovery may not occur at all. This forces the neurologist and otorhinolaryngologist to carefully evaluate the influence of the etiological factor, the course of neuropathy, and most importantly, to look for new approaches to treatment.
Treatment should be comprehensive, including measures affecting the cause of the disease (if it can be established) and pathogenetic mechanisms (edema, ischemia). In the treatment of traumatic injuries, the main thing is to improve surgical options. Surgeries are performed to restore the integrity of the nerve (decompression of the intrapetrosal part of the facial nerve, isolation, movement and suturing of the trunk through anastomosis of the facial nerve with another donor nerve). The basis for intervention on the facial nerve is both a disease of the nerve itself (inflammation or tumor), and damage to it as a result of trauma (fracture of the base of the skull, iatrogenic trauma) or a tumor process in nearby structures.
Main causes of central paresis
Central paresis develops due to the following diseases:
- stroke;
- traumatic brain injuries, traumatic spinal cord injuries;
- encephalitis;
- neoplasms of the brain and spinal cord;
- osteochondrosis, intervertebral hernia.
The causes of central paresis are cerebral circulatory insufficiency due to atherosclerosis or arterial hypertension, multiple sclerosis, cerebral palsy, amyotrophic lateral sclerosis. Bladder paresis is a temporary or permanent loss of the ability of the muscular wall of the bladder to contract. It occurs with spinal trauma, spinal cord tumors.
Signs of central paresis
With central paresis, muscle strength decreases to varying degrees. In some cases, patients are worried about rapid fatigue and awkwardness, while in others there is an almost complete loss of movement. Since with central paresis the part of the spinal cord below the site of injury remains intact, it tries to compensate for motor disorders. This leads to an increase in muscle tone, strengthening of normal reflexes and the appearance of pathological ones, which do not occur in a healthy person. Due to spastic paresis, contractures can develop - restriction of movements in the joints.
Central paralysis: symptoms and treatment of the disorder
Central paralysis is a pathology in which there is a lack of muscle strength in a separate part of the body. The disease predominantly affects the upper and lower extremities.
With central (spastic) paralysis, muscle hypertension occurs. The peculiarity of the disease is that there is an increase in tendon reflexes and muscle tone.
In addition, there is involuntary motor activity. If characteristic symptoms of the disease occur, you will need to contact a medical specialist for diagnosis.
A treatment regimen is individually selected for each patient, thanks to which it will be possible to maintain and improve the condition of the body.
Characteristic
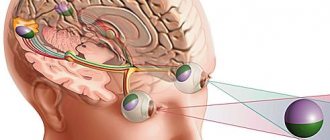
In healthy people, when irritants are applied to the skin, impulses are transmitted through the spinal cord to the cranial cavity. The process involves nerve fibers through which signals are sent.
With central paralysis, certain muscle groups are toned all the time. Reflexes do not pass through the tendons, and even the pain impulse does not enter the brain. The person experiences muscle spasms and uncontrolled movements.
Central paralysis prevents a person from assuming certain postures. If the face is affected, then the patient notes a deterioration in his emotional state. A temporary decrease in muscle tone is achieved through special massage, therapeutic exercises and warming up the problem area.
Over time, sick people learn to independently determine the nature of impulses, which are of external and internal types. Patients may feel discomfort and pain, depending on the degree of spasticity.
Those citizens who have a moderate level of spasticity have the opportunity to move with slow steps or independently change their body position.
When central paralysis occurs, a person often has problems with coordination and difficulty eating. Respiratory and digestive system disorders may occur.
Tactile sensitivity can become dull or worsen. Visual function may decline. Ballroom people require special care and must be handled with care.
Any change in body posture causes significant problems.
Main reasons
With central paralysis, a person loses the ability to control certain parts of the body. The causes are related to damage to the nervous system. Basically, pathology develops in disorders that arise in the motor centers.
Various provoking factors can lead to such a condition. Among them are dangerous diseases that humans have. In such a situation, you will need to identify them and, if possible, eliminate them.
Causes:
- Heredity. If close relatives have had central palsy, then the person will be significantly more likely to experience the disease. In most cases, the first signs of damage can be observed within 1 year of the child’s life.
- Infections. They can affect the spinal cord and brain. Because of this, various disturbances in the motor center are observed. It is important to treat all infections in a timely manner so that you do not have to deal with their complications.
- Developmental defects. In this situation, paralysis is diagnosed at an early age.
- Poor nutrition. Directly if you overuse fatty foods, a person may experience central paralysis.
- Metabolic disorders. Because of them, brain function significantly deteriorates.
- Malignant neoplasms in the brain. They compress the organ and lead to disruption of its functions. In particular, due to tumors, motor activity may deteriorate.
- Severe intoxication. When poisoned by toxic substances and drugs, a person may experience central paralysis.
- Congenital pathologies. In some children, even during intrauterine development, the central nervous system is formed incorrectly. This can happen due to hypoxia, infectious diseases, or difficult childbirth. In such a situation, a child is born with central paralysis.
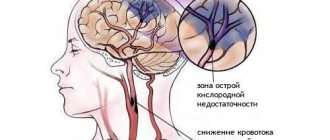
Central paralysis often occurs due to dysfunction of the circulatory system. Vascular stenosis, hemorrhage or blood clot formation leads to the destruction of neural connections.
The disease is often a complication after an ischemic or hemorrhagic stroke. When diagnosing, a medical specialist must determine the root cause of the disease. In this case, it will be easier to choose the right treatment regimen and improve the patient’s condition.
Symptoms
Central paralysis has characteristic manifestations by which pathology can be recognized. If several signs appear, you should visit a doctor. A medical specialist will be able to make an accurate diagnosis and determine the form of the disease.
Symptoms:
- Mobility abnormalities: Mobility may be decreased or increased.
- Speech disorders. A person may have difficulty pronouncing words and may completely lose the ability to speak.
- Muscle paresis. In this case, muscle strength and reflexes are significantly weakened, although they are preserved to some extent.
- Change in gait. It becomes much more difficult for a person to move. He may stop walking altogether.
- Muscle hardening. This condition occurs due to muscle hypertonicity.
- Tremor. The patient often experiences trembling of the limbs.
- Convulsive states. They can be temporary or permanent.
- Uncontrolled movement of limbs. A person can bend or straighten his arms and shrug his shoulders.
- Unnatural position of arms and legs. With central paralysis, it is impossible to keep the limbs in a relaxed and natural state.
- Uncontrolled downward abduction of the lower jaw.
It is important to take into account that symptoms depend on the affected area. With facial nerve paralysis, the pathology will affect the facial muscles. The person will experience distortion of facial expressions and unnatural muscle contraction. Speech function may deteriorate significantly due to the disease.
If characteristic symptoms occur, it is not allowed to make a diagnosis on your own. Negative manifestations may indicate other diseases, for example, synkinesis, hyperreflexia, clonus and other pathologies. Only a doctor, after conducting examinations, will be able to clearly say what we are dealing with.
If left untreated, further impairment of brain function will occur. New tissue will be affected and cannot be restored. For this reason, if you notice signs of central paralysis, it is important to go to the hospital immediately. In this situation, it will be possible to improve the condition of the body and prevent further spread of paralysis.
Diagnostics
If paralysis is suspected, a differentiated diagnostic method is used. In this case, the disease is determined by excluding other pathologies that do not relate to humans. Ultimately, one disease remains, which is the cause of spastic paralysis.
Diagnostics consists of three stages:
- First, the doctor finds out what diseases the patient has suffered. Some of them could cause complications in the form of impaired motor function.
- In the second stage, a medical specialist will examine the patient and find out the symptoms. It will be possible to roughly understand what you have to deal with.
- At the third stage, you will need to study all the laboratory tests on the basis of which the conclusion is made. Neuroimaging is used, for this purpose CT and MRI . The person is also sent for x-rays of the bones of the skull and spine. A cerebrospinal fluid tap may need to be performed. Based on the research results, it will be possible to generally judge the state of the body. If a person has any pathologies that provoked central paralysis, they will be identified.
If after diagnosis the disease is confirmed, the doctor will prescribe comprehensive treatment. You will need to simultaneously combat the symptoms of paralysis, improve the functioning of the central nervous system and eliminate the root cause. In this situation, it will be possible to achieve good results in treatment.
The prognosis depends on the degree of damage to the body, the person’s age and concomitant diseases. For this reason, it is impossible to say unambiguously how successful the chosen treatment regimen will be.
Treatment methods
Therapy is carried out exclusively under the supervision of a medical specialist. During treatment, it is necessary to relieve pain and spasms, and reduce muscle spasticity.
Therapy is necessarily aimed at improving the patient’s quality of life, as well as developing his abilities to perform everyday tasks. Doctors will need to make it easier for the citizen to perform controlled movements.
The desired result is achieved thanks to complex measures that are prescribed individually for the patient.
Drug treatment consists of at least two drugs. Drugs such as Baclofen, Dantrolene or Gabaleptin are often used.
A group of benzodiazepines is used, and Botox also provides good results. The latter remedy is injected into the damaged muscles, after which they relax. The pain disappears and the patient may feel relief.
One injection will last up to 16 weeks on average.
Surgical treatment may be required; in this situation, Baclofen is injected into the cerebrospinal fluid. The ampoule is implanted into the skin of the abdomen.
Additionally, the person will need physical therapy; specific procedures are prescribed depending on the patient’s condition. They give good results with regular use.
Doctors recommend that people with central palsy perform therapeutic exercises; specific options are selected depending on the patient's condition. Muscle condition can be improved with massage and water treatments.
Homeopathy may be prescribed as a supplement.
Exceptionally comprehensive measures can achieve good results. It is important to strictly follow the doctor’s recommendations, otherwise the desired effect will not be achieved.
The rehabilitation process is long and difficult, because it is not easy to restore motor activity. The rate of improvement is influenced by how advanced the disease is.
If a person is not treated for a long time, then muscle tissue atrophy will occur.
With timely treatment, there is a chance to completely restore brain activity and return a person to a full life. Naturally, we are talking about mild forms of central paralysis. In difficult situations, the main goal of therapy is to reduce the symptoms of the pathology and teach the person to live with movement disorders. A citizen will need to do therapeutic exercises throughout his life and, if necessary, take medications. To monitor the condition, you need to be observed by a doctor to prevent the progression of central paralysis.
Source: //nevrology.net/sindromy-i-zabolevaniya/perifericheskoj-nervnoj-sistemy/paralich/tsentralnyj.html
Peripheral paresis
Peripheral paresis develops when the nerve is directly damaged. In this case, disorders develop in one group of muscles that this nerve innervates. Muscle weakness may be present in only one leg or arm. The larger the nerve is damaged, the larger part of the body is affected by paresis or plegia (paralysis).
Peripheral paresis develops due to the following reasons:
- degenerative diseases of the spine, radiculitis;
- demyelinating diseases;
- nerve damage due to connective tissue diseases and vasculitis;
- compression of nerves (“tunnel syndromes”);
- nerve injuries;
- poisoning with alcohol and other toxic substances.
In the presence of peripheral paresis, muscle weakness, weakened reflexes, and decreased tone occur. Involuntary muscle twitching is noted. Over time, muscle atrophy develops (muscles decrease in volume) and contractures occur.
Facial paresis develops when the facial nerve is damaged. It is characterized by impaired functioning of facial muscles. Most patients have unilateral lesions, but total paresis also occurs. The main symptom indicating the progression of facial nerve paresis is facial asymmetry or the complete absence of motor activity of muscle structures on the side of the lesion.
Types of neuritis (neuropathy) of the facial nerve
- idiopathic neuropathy (Bell's palsy) is the most common (75%) form in which it is not possible to accurately determine the etiological factor; This form is characterized by seasonality, the development of the disease after cooling and colds;
- otogenic neuropathy accounts for up to 15% of facial nerve lesions; Most often, the trunk of the facial nerve is damaged in chronic inflammatory diseases of the middle ear and during surgical interventions (debridement operations, mastoidotomy, etc.);
- post-traumatic neuropathy of the facial nerve in injuries of the skull and brain with a fracture of the base of the skull, in wounds and closed injuries of the neck and face;
- infectious neuropathy is the rarest (10%) form of damage to the facial nerve, occurring when affected by the Herpes zoster virus (Hunt syndrome), polio virus, influenza, mumps, etc.
Edema and ischemia are currently considered to be the main factors in the pathogenesis of facial neuritis. The various etiological factors described above cause a violation of vascular tone with a tendency to spasms, mainly of arterioles, followed by their expansion and stasis of the capillaries of the perineurium, leading to a violation of their permeability. The resulting edema leads to compression of the veins and walls of the lymphatic vessels, which ultimately leads to ischemia of the nerve trunk with its swelling and hemorrhages, and destruction of the ischemic area of the nerve. This is especially pronounced in its vertical (distal) part, where the anatomical narrowing of the canal takes place.
Diagnosis of paresis
Neurologists at the Yusupov Hospital identify paresis and paralysis during an examination. The doctor asks the patient to make different movements, then tries to bend or straighten the affected limb and asks the patient to resist. The patient is asked to perform a test, which involves trying to hold both limbs of the same name suspended. If muscle strength is reduced in one of the limbs, then after 20 seconds it noticeably drops down.
After the examination, the doctor prescribes an examination that helps to identify the cause of paresis:
- computed or magnetic resonance imaging;
- neuromyography;
- clinical, biochemical and immunological blood tests;
- examination of cerebrospinal fluid obtained by lumbar puncture.
After analyzing the results of the study, the neurologist prescribes drug therapy. Professors and doctors of the highest category discuss severe cases of paresis at a meeting of the Expert Council and make a collegial decision regarding the tactics for further management of patients with paresis.
Treatment and rehabilitation for paresis
Neurologists at the Yusupov Hospital prescribe drug therapy depending on the cause and type of paresis. Rehabilitation treatment is of great importance for restoring movements and preventing contractures. The Yusupov Hospital is equipped with modern equipment from leading world manufacturers. The rehabilitation clinic employs exercise therapy instructors who improve their professional level in leading European and Russian rehabilitation centers.
Rehabilitation for paresis includes:
- therapeutic exercises;
- mechanotherapy on special simulators;
- massage;
- neuromuscular stimulation;
- use of orthoses;
- physiotherapeutic procedures.
For the convenience of patients, comprehensive rehabilitation programs have been developed that allow them to save the family budget and receive a full course of rehabilitation therapy at a stable, affordable price. In order to undergo a course of treatment and rehabilitation for paresis, call the Yusupov Hospital.
Author